Abstract
Purpose of Review
Orthopaedic surgeries are occurring at an increasing frequency in the elderly patient. The goal of this review was to provide exposure to risk stratification scores to help identify high-risk elderly orthopaedic patients.
Recent Findings
New guidelines have been developed to assess the risk of cardiopulmonary and other perioperative complications. Older scoring systems, such as the American Society of Anesthesiologists (ASA) score and revised cardiac index, are still of importance as they have strong correlation with risks of cardiac and other complications. Other scoring systems, such as the Estimation of Physiologic Ability and Surgical Stress (E-PASS) score and Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity (POSSUM) score, have recently been shown to stratify high-risk elderly patients undergoing hip fracture surgery and other orthopaedic surgeries.
Summary
The elderly orthopaedic patient has higher risks of perioperative complications than the younger patient. Scoring systems have been developed to help identify those patients at higher risk. Familiarity with these scoring systems will help the practitioner to appropriately select patients for surgery and guide patient counseling on risks on complications and protocols to optimize preoperative care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Fifty percent of Americans will undergo a surgery when they are over the age of 65 years old. Often these surgeries are unplanned, unexpected, and carry significant risks [1]. In patients over the age of 75 years old, low-energy trauma causes 80% of operatively treated fractures [2]. These injuries are often accompanied by a high rate of morbidity and often mortality [2]. The incidence of orthopaedic issues amongst the super or very elderly is increasing, with a 114% increase in hip fractures in patients 90 years of age or older in 2001–2005 compared to 1993–1996 [3]. More elective interventions, such as total joint arthroplasty and spinal surgery, are also frequently performed in the elderly due to the prevalence of degenerative joint disease in this population [4]. These elective cases often offer time for adequate preoperative planning and optimization by the orthopaedic surgeon, medical team, and anesthesiologists. Such optimization requires careful attention to patient comorbidities, as well as the physiologic changes associated with aging, to ensure safe surgery. This review will serve to highlight several preoperative risk scoring systems as well as review system-specific risk modification strategies.
Cardiopulmonary Risk Scores
American Society of Anesthesiologists Score
The American Society of Anesthesiologists (ASA) first reported its physical status classification system in 1941 [5]. Originally designed to estimate overall mortality risk in patients undergoing surgery, the ASA score has been shown to more specifically predict cardiac and pulmonary complications [6,7,8]. An ASA score of greater than 2 is associated with a two- to threefold increase in the risk of perioperative pulmonary complications [9]. In geriatric orthopaedic patients, increasing ASA score is also associated with an increased risk of developing a variety of perioperative complications [10, 11]. Higher ASA scores are associated with longer times to surgery [12], increased length of stay [11, 12], and higher 30-day mortality rates in the geriatric orthopaedic population [12]. While no specific interventions have been described to mitigate the risks associated with higher ASA scores, it is a readily available tool that has utility in risk screening and will be further discussed later.
Goldman Cardiac Risk Index
The first cardiac risk index was originally reported by Goldman and colleagues in 1977 [13]. This prospective cohort study included data from general surgery, orthopaedic and urological patients. The authors identified nine variables that were associated with poor cardiac outcomes, specifically life-threatening cardiac events and cardiac-related mortality (Table 1). Each variable was then given a numerical risk score, and these scores were summed to stratify the patients into one of four risk classes. The two major cardiac outcomes reported were life-threatening cardiac events (including pulmonary edema, myocardial infarction, and ventricular tachycardia) and cardiac mortality. While not all the variables are modifiable, they concluded that 28 of the total of 53 points are potentially controllable and modifiable preoperatively [13].
The authors recommended that surgical interventions in class IV patients be limited to true life-saving procedures. In addition, all patients qualifying for classes III and IV should receive a preoperative medical consultation [13]. This system has been subsequently validated, though its sensitivity has been called into question [8, 14, 15]. The original Goldman’s classification is the basis of many of the more common cardiac risk indices.
Detsky Modified Cardiac Index
In 1986, Detsky et al. modified Goldman’s original multifactorial index [14]. Major changes to Goldman’s original index included the simplification of the point system as well as the addition of several other variables. Surgical procedures were classified as either major (e.g., hip replacement) or minor (e.g., arthroscopy). Both the original Goldman index and this modified index were calculated for 455 consecutive patients who received a preoperative medical consultation. This differed from the patient population used in Goldman’s original article [13], as only surgical patients with a documented concern for cardiac status were included in this study. The original outcomes defined by Goldman et al. were used, with the addition of new or worsening congestive heart failure and coronary insufficiency. Severe events were defined as cardiac death, myocardial infarction, and alveolar pulmonary edema. Serious complications were defined as any severe complication and the addition of coronary insufficiency, as well as congestive heart failure without alveolar pulmonary edema [14].
The authors concluded that this modified index added a statistically significant amount of predictive information over the original Goldman index. Results showed a strong correlation between the derived index and the likelihood ratio of cardiac event for both major and minor surgeries. This modified index, however, was plagued with the poor sensitivity demonstrated by Goldman’s original index [8, 14] and is not routinely used today.
Lee’s Revised Cardiac Index
In 1999, Lee et al. assessed the validity of both the Goldman’s and Detsky’s cardiac indices and devised a more simplified version (Table 1) [8]. Though previous risk schemas were able to stratify patients into subsets with increased rates of adverse outcomes, few patients fell into the highest risk groups [8]. In Lee et al.’s prospective cohort of 2893 patients, of which 1026 were orthopaedic patients, six factors were identified that were associated with perioperative cardiac complications. The authors concluded that this index stratified more patients into the higher classes, had an increased ease of use, and demonstrated equivalent correlation with risk of cardiac events (Table 1).
In addition to having an increased risk of immediate postoperative cardiac complication, patients with a history of ischemic heart disease, congestive heart failure, and diabetes mellitus maintained this elevated risk during the next 6 months, even if they did not have major immediate perioperative cardiac complications [16]. In particular to hip and knee arthroplasty, a revised index score of greater than or equal to three has been shown to be significantly associated with an increased risk of a myriad of complications beyond cardiac issues, including those related to neurological, renal, and wound complications [17]. Lee’s revised cardiac index is easy to use, shows a strong correlation with cardiac events, and is one of the more commonly used cardiac indices today.
American College of Cardiology and American Heart Association Guidelines
The ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery was published in 2014 [18••]. This was developed based on the review of published research, and the report presents a stepwise approach to preoperative evaluation of the surgical patient with risks for cardiac disease (Table 1). Unlike the original cardiac indices, which focused mainly on evaluating risk factors for cardiac complications, this guideline provides a stepwise approach to guide need for cardiovascular testing, perioperative pharmacological management, and perioperative monitoring.
Pulmonary Risk
Postoperative pulmonary complications are known to have a longer hospital stay than patients who develop postoperative cardiac complications [19, 20]. In 2006, the American College of Physicians (ACP) published guidelines to help predict perioperative complications before non-cardiac surgery and recommend strategies to reduce the risk for postoperative pulmonary complications [21]. Notably, any patient undergoing general anesthesia was classified as high risk [21]. A meta-analysis performed by Rogers et al. concluded that the use of neuraxial blockade, spinal and epidural anesthesias, significantly decreases the risk of perioperative pulmonary complications, among other complications, when used alone or combined with general anesthesia [22]. Use of these types of anesthesia may help to lower the risks of pulmonary and other complications in the geriatric orthopaedic patient.
The prevalence of chronic obstructive pulmonary disease (COPD) has been estimated to be 14.2% (11–18%) in those over age 65 [23], and there is a twofold increase in prevalence for every 10-year increment in age [24]. There have been several preoperative strategies which have been proposed for COPD management, as its presence doubles the risk of postoperative pulmonary complications [6, 25]. These include the use of ipratropium and tiotropium for all symptomatic patients, symptomatic use of inhaled beta agonists, liberal use of corticosteroids, and reserving antibiotic administration only when a change in the character of sputum is present [26]. The 2006 ACP guidelines also recommended against the routine use of spirometry and chest radiographs for the assessment of pulmonary-specific risk. The exception to this is select patients with COPD and uncontrolled severe asthma. [21].
While the ACP guidelines recommend for the use of incentive spirometry or deep breathing exercises [21], there is mixed evidence on their effectiveness in preventing pulmonary complications [27]. Given the possible benefit and low risk of incentive spirometry, it is still routinely used today. Elderly patients are at increased risks of pulmonary complications, especially those with preexisting lung disease. Appropriate preoperative and postoperative optimization of preexisting pulmonary conditions should be considered in all patients.
American Society of Anesthesiologists Score
Paksima et al. evaluated predictors for mortality after hip fracture and identified advanced age, male gender, high ASA classification, the presence of a major postoperative complication, history of cancer, chronic obstructive pulmonary disorder, history of congestive heart failure, ambulating with an assistive device, or being a household ambulator prior to hip fracture as risk factors [28]. Additionally, he found that while the mortality rate is increased to approximately 30% within the first year, it normalizes within the first 3 years after fracture [28].
Several scoring tools are available to help provide risk stratification based on patient factors. Goals of scoring tools are to provide objectivity in predicting patient outcomes, guide clinical decision making, improve informed consent when patients are considering non-operative versus operative treatment, and help to optimize treatment plans based on known risk factors and predilection for certain outcomes [29, 30].
The ASA score is used by anesthesiologists for preoperative risk stratification but has recently been suggested as a predictive score for perioperative complications and for readmissions after hip fracture repair [11]. Donegan et al. evaluated patients using their ASA classification and found that ASA 3 and 4 had the highest rates of medical complications. Patients with an ASA 3 had a 3.78 times higher rate of any medical complication compared to ASA class 2, while patients with ASA class 4 had a 7.39 times higher rate of medical complications compared to ASA class 2 [30].
Radcliff et al. performed a study of 5683 male veterans over 65 years old who sustained a hip fracture using the National Surgical Quality Improvement Program (NSQIP) database. They found that patients with ASA 3 and 4 had an increased mortality within the first 30 days, with an odds ratio of 2.10 and 3.83, respectively [31]. Furthermore, an ASA classification of 3 or 4 can portend a poor prognosis after sustaining a hip fracture. A ninefold increase in mortality rate has been reported in patients with an ASA of 3 or 4 compared to patients with an ASA of 1 or 2 [32]. ASA classification is widely used perioperatively and can thus be used easily. It is a well-accepted and understood classification scheme that can help guide clinicians and patients in understanding specific perioperative risks.
Estimation of Physiologic Ability and Surgical Stress Score
The Estimation of Physiologic Ability and Surgical Stress (E-PASS) is a score that has been found to correlate with morbidity and mortality in gastrointestinal and pulmonary surgery and incorporates preoperative and intraoperative patient data. Recently, E-PASS has been used in the orthopaedic population, specifically for patients undergoing hip fracture fixation or arthroplasty [33, 34]. The E-PASS score is determined from an algorithm in which patient variables are input into an equation that creates a comprehensive risk score. This is composed of a preoperative risk score (PRS) that incorporates patient risk factors such as age, presence of heart disease, pulmonary disease, diabetes, performance status index, as well as ASA score. Included within the E-PASS score is the Surgical Stress Score (SSS), which incorporates intraoperative factors such as blood loss, surgical time, and extent of skin incision. Both the preoperative risk score and surgical stress scores create a Comprehensive Risk Score (CRS) (Table 2).
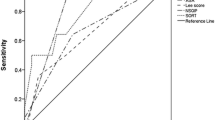
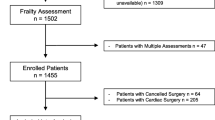
Hirose et al. recently performed a retrospective review evaluating the use of the E-PASS score for use in the hip fracture population over eight hospitals in Japan and found the E-PASS to be a reasonable predictor of postoperative morbidity and mortality [34]. Mortality prediction models use an area under the curve (AUC) of receiver operating characteristic curves (ROC), also known as “C-score,” to represent sensitivity and specificity by estimating the ability of a test to discriminate between outcome groups, with 1.0 indicating perfect discrimination [35]. Acceptable discrimination is considered 0.70–0.79, and greater than 0.80 is considered excellent discrimination [35]. The E-PASS score has been found in a retrospective study of 30-day mortality of 1120 hip fracture surgeries to have an AUC of 0.72 [35].
Morbidity and mortality rates estimated by the PRS also have been shown to correlate with the observed morbidity and mortality rates (p < 0.0001 and p = 0.002, respectively) [36]. Observed/estimated ratios were found to be 1.06 for morbidity and 0.71 for mortality [36]. Postoperative morbidity and mortality rates increased linearly with the PRS and CRS, but no correlation was seen with use of the SSS and postoperative morbidity and mortality [36]. However, SSS has been shown to correlate to length and cost of hospital stay [34]. Inability to apply the SSS to hip fracture surgery may be due to its original designation as a general surgery score, which are procedures that can have large variations in size of incisions and EBL which may not vary significantly for hip fracture procedures [36]. However, CRS can help guide care; a CRS greater than 0.5 was found to have a complication rate of 37% in elderly patients undergoing hip fracture surgery; thus, care must be taken perioperatively in patients with a high CRS score [37••]. Alternatively, a low PRS can be predictive of lack of development of postoperative complications—Hirose et al. found that no postoperative complications developed in patients with a PRS less than 0.3. The authors thus recommend only use of the E-PASS equation in patients with PRS greater than or equal to 0.213 and less than 3.163 as mortality rates exceed 100% when the PRS is greater than 3.163 [36].
More recently, the E-PASS score has been investigated for use in predicting morbidity after various general orthopaedic procedures including total joint arthroplasty, spine surgery, and tumor surgery. It has been shown to have an AUC of 0.777 for overall complications, and 0.794 for non-surgical site complications, which is an improved predictive value compared to the E-PASS in the hip fracture population [37••]. A retrospective review of 1883 patients who underwent the aforementioned general orthopaedic procedures revealed a positive linear association of morbidity with E-PASS score. The E-PASS CRS was found to have 83% sensitivity and 62% specificity for predicting overall complications. Additionally, the SSS was found to be 83% sensitive and 88% specific for predicting a surgical site complication [37••].
Acute Physiology and Chronic Health Evaluation II Score
The APACHE II score uses data from physiologic and laboratory measurements obtained during the early admission period, including heart rate, pH, and various measurements that are taken frequently in the ICU setting [38]. Originally developed for use in the general surgery ICU population, the APACHE score has not been validated for use in older orthopaedic patients. Rogers et al. did not find a difference between APACHE groups in the hip fracture population in regard to actual or predicted survival [38].
Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity Score
Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity (POSSUM) was developed for general surgical procedures through multivariate regression analysis of 48 physiologic and 18 operative factors [39, 40]). It has since been reduced to 14 physiologic and six operative variables (Table 2) to predict mortality and morbidity. It has been validated for use in orthopaedic surgery with good predictive value, sometimes referred to as O-POSSUM [41]. Mohamed et al. evaluated the O-POSSUM score for 2326 elective and emergency/traumatic orthopaedic procedures and found an observed/expected ratio of 0.96 for mortality and 0.99 for mortality [41].
Controversy exists regarding the use of POSSUM scoring in hip fractures. POSSUM has been applied to the femoral neck fracture population and demonstrated overestimation of mortality in the higher risk populations [42]. POSSUM scoring in a 1164 patient cohort study found a receiver-operator characteristic curve of 0.62, indicating poor predictive value due to overestimation of risk of death [42]. Furthermore, the POSSUM score has been shown to overestimate morbidity for general orthopaedic procedures as well [43•]. Despite this, the POSSUM score may be helpful in assessing long term risk. Van Zeeland et al. found good predictive value of the POSSUM score for 5-year mortality in both femoral neck fractures and trochanteric region hip fractures when dividing patients into high-, intermediate-, and low-risk groups [44]. Significant predictors of mortality included age, blood loss, blood level of urea, sodium and potassium, and physical signs such as cardiac and respiratory signs, systolic blood pressure, EKG, and presence of malignancy [44]. Strikingly, at 5 years, the mortality for hip fracture in a high-risk group was found to be 25% [44].
Recently, POSSUM was evaluated against many frequently used scoring systems and found to have good predictive value for assessing serious in-hospital complications, along with the Charlson comorbidity index and RISK-VAS, which is a scoring system based off of physician intuition of global risk after assessment of the patient [45]. Other indices compared included the Goldman cardiac index, which was not found to have prognostic value in hip fracture surgery [45].
Charlson Comorbidity Index
The Charlson Comorbidity Index (CCI) was initially developed in 1987 as predictive tool to identify comorbid conditions which may affect the risk of mortality in medical patients [46]. The original index included 19 comorbidities which were assigned different weights based on their association with mortality. While the CCI has been studied in various aspects of orthopaedics, it has been specifically examined in the elderly hip fracture population. In a prospective study of 232 elderly hip fracture patients, the CCI was shown to exhibit sufficient predictive value for serious complications during the initial hospital stay but underperformed when compared to the POSSUM scoring system [45]. A score of greater than or equal to 6 has also been correlated with increased 30 day mortality in hip fracture patients [47], although with a low discriminatory power [35]. Again, in a meta-analysis, it was shown to be moderately discriminant for in-hospital morbidity and 1-year mortality. In 30-day mortality after hip fracture surgery, the CCI has been shown to have an AUC of 0.71 indicating acceptable discrimination [35]. While the CCI has been found to be helpful for assessing mortality, its long-term predictive value has not been demonstrated [48]. Additionally, a criticism of the CCI is its lack of incorporation of functional outcomes and mental status which may decrease its usefulness in assessing morbidity [35].
Nottingham Hip Fracture Score
To counter the identified weakness of the CCI, the Nottingham Hip Fracture Score (NHFS) aimed to include functional as well as mental status in its model. It was developed to predict 30-day mortality after hip fracture using individual patient factors, including age, gender, Mini-Mental State Evaluation (MMSE), as well as common comorbidities [49]. Elderly age, male sex, the presence of two comorbidities, a MMSE score of less than six, anemia on admission, living status, and the presence of malignancy were found to be independent predictors of mortality at 30 days [49]. While the CCI derives its score from major medical comorbidities, the NHFS incorporates functional factors, such as living in an institution, that are independent mortality factors [49]. The NHFS is ergo a score that reflects more subtle and patient-specific factors that may ultimately impact mortality. Additionally, the NHFS was found to have improved discrimination with an AUC of 0.77 when compared to four other risk prediction models in 30-day mortality after hip fracture, which may be attributed to the NHFS being designed specifically for hip fractures [35].
Risk Scoring Systems in Spinal Surgery
Spinal surgery is indicated in elderly patients for a variety of pathologies, including radiculopathy, spinal stenosis, and deformity. Complications can vary in severity from pressure sores and superficial wound infections to DVT, neurologic injury, and even death. Eighty-seven percent of patients have been reported to experience a single complication [50]. Thus, scoring systems have been developed to help predict those at risk for such events.
E-PASS has been evaluated specifically for use in spinal surgery and has demonstrated good predictive power [51••]. In a retrospective review of 275 patients who underwent spinal surgery, the PRS was correlated with complications at non-surgical sites with an AUC of 0.819 while the SSS was associated with complications at the surgical site with an AUC of 0.834 [35]. Thus, this scoring system can be applied to spinal surgery and may be useful in guiding patients in their decisions for surgery as well as physicians in directing their care.
Data regarding which scoring system is most predictive of adverse events are lacking, however. Ying et al. performed a retrospective review of 158 lumbar surgeries using a modified POSSUM score [41, 52] and found that the POSSUM score tended to over predict in low-risk patients. Conversely, the predictive value of the modified POSSUM was best in high-risk patients, with an observed to expected ratio of one in the highest risk cohorts [52].
Risk Scoring Systems in Total Joint Arthroplasty
There have been multiple prediction tools developed for hip and knee arthroplasty patients, with models estimating complications, discharge disposition, readmission, and infection all having been described [53•]. These models all share the common goal of predicting postoperative complications and mortality. The ACS NSQIP calculator is a model that has been used to predict 30-day complications following primary total joint arthroplasty [54••]. Through use of this tool, investigators were able to identify population level complications as well as discharge disposition, but it has been shown to have a poor predictive value in a subsequent validation study (AUC of 0.586) [53•, 55]. Wuerz et al. developed a model that evaluated in-hospital major complications with good predictive value but included a diverse group of surgical procedures including partial arthroplasty, revision arthroplasty, and arthroplasty for fracture and tumors [56]. It has not been externally validated and its value in elective total joint arthroplasty has not be assessed [53•]. Lastly, HealthGrades developed a model to predict 14-day complications and mortality following primary total joint arthroplasty. In an external validation study using a Medicare data set, patients with higher predicted values did experience more complications, although the calculator overestimated the risks in these groups and has been shown to have an AUC of 0.609 [53•, 57]. While these risk calculators may be useful to help stratify patients into high-risk groups, there are limits to their predictive abilities.
How to Optimize Patients
Although these scoring systems provide helpful information regarding the outcome of patients, the real question is how to optimize the elderly for an unanticipated surgery. Using these scoring systems to help identify the at-risk patient can be helpful for managing postoperative complications. The presence of comorbidities can be used to predict mortality as well as risk of developing complications. Lawrence et al found a complication rate of 19% in a retrospective review of 8,930 patients over 60 years old who underwent surgical treatment of a hip fracture [58]. Of these complications, cardiac and pulmonary complications occurred most frequently at rates of 8% and 4%, respectively [58].
There are a multitude of issues that threaten the elderly orthopaedic patient population. A careful history and physical exam to identify the cause of the fracture, whether it be from a mechanical fall or a balance issue, or electrolyte abnormalities is paramount. Many patients arrive at the hospital dehydrated in anticipation of acute surgery or from delay to care and require adequate fluid resuscitation [2]. Cardiac issues are the most severe complications that can result in mortality, with myocardial infarction, arrhythmia, and decompensated heart failure being some of the most common [59]. DVT and PE can occur secondary to damage to endothelial vessels, hypercoaguability, and venous stasis from surgery and decreased ambulation after orthopaedic procedures [59]. Renal problems present perioperatively due to decreased renal clearance that occurs with age, that is often compounded by other comorbidities such as hypertension, diabetes or heart failure [59]. Delirium is a frequent occurrence perioperatively, occurring at a rate of 50-61% in the hip fracture population [2]. Of many strategies available to reorient patients and prevent delirium, adequate analgesia is important to promote not only early ambulation and locomotion but also prevent delirium [60, 61]. Safe treatment of pain can be difficult in the elderly, as both opioid abstinence and low dose opioid treatment have both been shown to increase the risk of delirium [61]. Lastly, addressing chronic comorbidities such as diabetes, anemia, and nutritional status, as well as balancing any coagulopathies, can be vital in helping the elderly patient have a successful outcome after orthopaedic surgery [2].
Conclusion
Scoring systems in the elderly population are critical to providing safe and effective care in the aging population, as many of the preoperative risk assessment tools used in general medicine do not apply to the often osteoporotic patient with multiple comorbidities and poor social support systems [1]. The development of scoring systems makes it easier for the orthopaedist to identify high-risk patients and those who may require additional preoperative optimization and postoperative care. In addition to this identification, it is important to remember the physiologic changes associated with aging that affect multiple organ systems and are oftentimes overlooked. Care of the elderly patient undergoing an orthopaedic procedure is best handled in a team-approach, involving the close care of an internist or gerontologist in addition to the surgical team.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kim S, Brooks AK, Groban L. Preoperative assessment of the older surgical patient: honing in on geriatric syndromes. Clin Interv Aging. 2014;10:13–27.
Marsland D, Colvin PL, Mears SC, Kates SL. How to optimize patients for geriatric fracture surgery. Osteoporos Int. 2010;21:S535–46.
Bergström U, Jonsson H, Gustafson Y, Pettersson U, Stenlund H, Svensson O. The hip fracture incidence curve is shifting to the right. Acta Orthop. 2009;80:520–4.
Higuera CA, Elsharkawy K, Klika AK, Brocone M, Barsoum WK. 2010 mid-America orthopaedic association physician in training award: predictors of early adverse outcomes after knee and hip arthroplasty in geriatric patients. Clin Orthop Relat Res. 2011;469:1391–400.
Saklad M. Grading of patients for surgical procedures. Anesthesiology. 1941;2:281–4.
Wolters U, Wolf T, Stützer H, Schröder T. ASA classification and perioperative variables as predictors of postoperative outcome. Br J Anaesth. 1996;77:217–22.
Wong DH, Weber EC, Schell MJ, Wong AB, Anderson CT, Barker SJ. Factors associated with postoperative pulmonary complications in patients with severe chronic obstructive pulmonary disease. Anesth Analg. 1995;80:276–84.
Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100:1043–9.
Smetana GW. Preoperative pulmonary evaluation. N Engl J Med. 1999;340:937–44.
Peled E, Keren Y, Halachmi S, Soudry M, Zinman C, Kats Y, et al. Patients aged 80 and older undergoing orthopedic or urologic surgery: a prospective study focusing on perioperative morbidity and mortality. Gerontology. 2009;55:517–22.
Kastanis G, Topalidou A, Alpantaki K, Rosiadis M, Balalis K. Is the ASA score in geriatric hip fractures a predictive factor for complications and readmission? Scientifica (Cairo). 2016;2016:1–6.
Yeoh CJC, Fazal MA. ASA grade and elderly patients with femoral neck fracture. Geriatr Orthop Surg Rehabil. 2014;5:195–9.
Goldman L, Caldera DL, Nussbaum SR, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med. 1977;297:845–50.
Detsky AS, Abrams HB, McLaughlin JR, Drucker DJ, Sasson Z, Johnston N, et al. Predicting cardiac complications in patients undergoing non-cardiac surgery. J Gen Intern Med. 1986;1:211–9.
Zeldin RA. Assessing cardiac risk in patients who undergo noncardiac surgical procedures. Can J Surg. 1984;27:402–4.
Lopez-Jimenez F, Goldman L, Sacks DB, Thomas EJ, Johnson PA, Cook EF, et al. Prognostic value of cardiac troponin T after noncardiac surgery: 6-month follow-up data. J Am Coll Cardiol. 1997;29:1241–5.
Ackland GL, Harris S, Ziabari Y, Grocott M, Mythen M. Revised cardiac risk index and postoperative morbidity after elective orthopaedic surgery: a prospective cohort study. Br J Anaesth. 2010;105:744–52.
•• Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014;64:e77–137. Presents updated guidelines on perioperative cardiovascular evaluation and management of non-cardiac surgical patients.
Collins TC, Daley J, Henderson WH, Khuri SF. Risk factors for prolonged length of stay after major elective surgery. Ann Surg. 1999;230:251–9.
Lawrence VA, Hilsenbeck SG, Mulrow CD, Dhanda R, Sapp J, Page CP. Incidence and hospital stay for cardiac and pulmonary complications after abdominal surgery. J Gen Intern Med. 1995;10:671–8.
Qaseem A, Snow V, Fitterman N, Hornbake ER, Lawrence VA, Smetana GW, et al. Risk assessment for and strategies to reduce perioperative pulmonary complications for patients undergoing noncardiothoracic surgery: a guideline from the American College of Physicians. Ann Intern Med. 2006;144:575.
Rodgers A, Walker N, Schug S, et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials. BMJ. 2000;321:1493.
Halbert RJ, Natoli JL, Gano A, Badamgarav E, Buist AS, Mannino DM. Global burden of COPD: systematic review and meta-analysis. Eur Respir J. 2006;28:523–32.
Buist AS, McBurnie MA, Vollmer WM, et al. International variation in the prevalence of COPD (the BOLD study): a population-based prevalence study. Lancet (London, England). 2007;370:741–50.
Kroenke K, Lawrence VA, Theroux JF, Tuley MR, Hilsenbeck S. Postoperative complications after thoracic and major abdominal surgery in patients with and without obstructive lung disease. Chest. 1993;104:1445–51.
Smetana GW, Lawrence VA, Cornell JE, American College of Physicians. Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med. 2006;144:581–95.
Sieber FE, Barnett SR. Preventing postoperative complications in the elderly. Anesthesiol Clin. 2011;29:83–97.
Paksima N, Koval KJ, Aharanoff G, Walsh M, Kubiak EN, Zuckerman JD, et al. Predictors of mortality after hip fracture: a 10-year prospective study. Bull NYU Hosp Jt Dis. 2008;66:111–7.
Jones HJS, De Cossart L. Risk scoring in surgical patients. Br J Surg. 1999;86:149–57.
Donegan DJ. Use of medical comorbidities to predict complications after hip fracture surgery in the elderly. J Bone Jt Surg. 2010;92:807.
Radcliff TA, Henderson WG, Stoner TJ, Khuri SF, Dohm M, Hutt E. Patient risk factors, operative care, and outcomes among older community-dwelling male veterans with hip fracture. J Bone Jt Surg. 2008;90:34–42.
Michel J-P, Klopfenstein C, Hoffmeyer P, Stern R, Grab B. Hip fracture surgery: is the pre-operative American Society of Anesthesiologists (ASA) score a predictor of functional outcome? Aging Clin Exp Res. 2002;14:389–94.
Hirose J, Mizuta H, Ide J, Nomura K. Evaluation of estimation of physiologic ability and surgical stress (E-PASS) to predict the postoperative risk for hip fracture in elder patients. Arch Orthop Trauma Surg. 2008;128:1447–52.
Hirose J, Mizuta H, Ide J, Nakamura E, Takada K. E-PASS for predicting postoperative risk with hip fracture: a multicenter study. Clin Orthop Relat Res. 2008;466:2833–41.
Karres J, Heesakkers NA, Ultee JM, Vrouenraets BC. Predicting 30-day mortality following hip fracture surgery: evaluation of six risk prediction models. Injury. 2015;46:371–7.
Hirose J, Ide J, Irie H, Kikukawa K, Mizuta H. New equations for predicting postoperative risk in patients with hip fracture. Clin Orthop Relat Res. 2009;467:3327–33.
•• Nagata T, Hirose J, Nakamura T, Tokunaga T, Uehara Y, Mizuta H. Evaluation of the utility of the Estimation of Physiologic Ability and Surgical Stress score for predicting post-operative morbidity after orthopaedic surgery. Int Orthop. 2015;39:2167–72. E-PASS score has utility in predicting postoperative complications in orthopaedic patients.
Rogers FB, Shackford SR, Keller MS. Early fixation reduces morbidity and mortality in elderly patients with hip fractures from low-impact falls. J Trauma. 1995;39:261–5.
Copeland GP, Jones D, Walters M. POSSUM: a scoring system for surgical audit. Br J Surg. 1991;78:355–60.
Brooks MJ, Sutton R, Sarin S. Comparison of Surgical Risk Score, POSSUM and p-POSSUM in higher-risk surgical patients. Br J Surg. 2005;92:1288–92.
Mohamed K, Copeland GP, Boot DA, Casserley HC, Shackleford IM, Sherry PG, et al. An assessment of the POSSUM system in orthopaedic surgery. J Bone Joint Surg Br. 2002;84:735–9.
Ramanathan TS, Moppett IK, Wenn R, Moran CG. POSSUM scoring for patients with fractured neck of femur. Br J Anaesth. 2005;94:430–3.
• Bao D, Li N, Xia L. Risk assessment and decision-making for patients undergoing orthopedic surgery. J Orthop Surg Res. 2015;10:169. POSSUM score overpredicts morbidity in orthopaedic patients.
Van Zeeland MLP, Genovesi IPO, Mulder J-WR, Strating PR, Glas AS, Engel AF. POSSUM predicts hospital mortality and long-term survival in patients with hip fractures. J Trauma. 2011;70:E67–72.
Burgos E, Gómez-Arnau JI, Díez R, Muñoz L, Fernández-Guisasola J, Garcia Del Valle S. Predictive value of six risk scores for outcome after surgical repair of hip fracture in elderly patients. Acta Anaesthesiol Scand. 2008;52:125–31.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Kirkland LL, Kashiwagi DT, Burton MC, Cha S, Varkey P. The Charlson Comorbidity Index Score as a predictor of 30-day mortality after hip fracture surgery. Am J Med Qual. 26:461–7.
Marufu TC, Mannings A, Moppett IK. Risk scoring models for predicting peri-operative morbidity and mortality in people with fragility hip fractures: qualitative systematic review. Injury. 2015;46:2325–34.
Maxwell MJ, Moran CG, Moppett IK. Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery. Br J Anaesth. 2008;101:511–7.
Street JT, Lenehan BJ, Dipaola CP, Boyd MD, Kwon BK, Paquette SJ, et al. Morbidity and mortality of major adult spinal surgery. A prospective cohort analysis of 942 consecutive patients. Spine J. 2012;12:22–34.
•• Hirose J, Taniwaki T, Fujimoto T, Okada T, Nakamura T, Usuku K, et al. Validity of E-PASS system for postoperative morbidity of spinal surgery. J Spinal Disord Tech. 2015;28:E595–600. E-PASS score predicts morbidity in spine surgery patients with increase in PRS, SSS, and CRS.
Ying L, Bo B, Huo-yan W, Hong Z. Evaluation of a modified POSSUM scoring system for predicting the morbidity in patients undergoing lumbar surgery. Indian J Surg. 2014;76:212–6.
• Manning DW, Edelstein AI, Alvi HM. Risk prediction tools for hip and knee arthroplasty. J Am Acad Orthop Surg. 2016;24:19–27. Provides an overview of risk scores for hip and knee arthroplasty patients.
•• Bilimoria KY, Liu Y, Paruch JL, Zhou L, Kmiecik TE, Ko CY, et al. Development and evaluation of the universal ACS NSQIP surgical risk calculator: a decision aid and informed consent tool for patients and surgeons. J Am Coll Surg. 2013;217:833–42–3. Describes the NSQIP risk calculator which is useful in assessing cardiac and other risks in orthopaedic patients.
Edelstein AI, Kwasny MJ, Suleiman LI, Khakhkhar RH, Moore MA, Beal MD, et al. Can the American College of Surgeons risk calculator predict 30-day complications after knee and hip arthroplasty? J Arthroplast. 2015;30:5–10.
Wuerz TH, Kent DM, Malchau H, Rubash HE. A nomogram to predict major complications after hip and knee arthroplasty. J Arthroplast. 2014;29:1457–62.
Romine LB, May RG, Taylor HD, Chimento GF. Accuracy and clinical utility of a peri-operative risk calculator for total knee arthroplasty. J Arthroplast. 2013;28:445–8.
Lawrence VA, Hilsenbeck SG, Noveck H, Poses RM, Carson JL. Medical complications and outcomes after hip fracture repair. Arch Intern Med. 2002;162:2053–7.
Leme LE, do Carmo Sitta M, Toledo M, da Silva Henriques S. Orthopedic surgery among the elderly: clinical characteristics. Rev Bras Ortop. 2011;46:238–46.
Hung WW, Egol KA, Zuckerman JD, Siu AL. Hip fracture management: tailoring care for the older patient. JAMA. 2012;307:2185–94.
Morrison RS, Magaziner J, Gilbert M, Koval KJ, McLaughlin MA, Orosz G, et al. Relationship between pain and opioid analgesics on the development of delirium following hip fracture. J Gerontol A Biol Sci Med Sci. 2003;58:76–81.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Jesse Hahn, Ryan Gentry, and Hannah Dineen declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Geriatric Orthopedics
Rights and permissions
About this article
Cite this article
Gentry, R.D., Dineen, H.A. & Hahn, J.C. An Overview of Risk Stratification in the Elderly Orthopaedic Population. Curr Geri Rep 7, 92–102 (2018). https://doi.org/10.1007/s13670-017-0230-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13670-017-0230-0