Abstract
Predicting the postoperative course of patients with hip fractures would be helpful for surgical planning and risk management. We therefore established equations to predict the morbidity and mortality rates in candidates for hip fracture surgery using the Estimation of Physiologic Ability and Surgical Stress (E-PASS) risk-scoring system. First we evaluated the correlation between the E-PASS scores and postoperative morbidity and mortality rates in all 722 patients surgically treated for hip fractures during the study period (Group A). Next we established equations to predict morbidity and mortality rates. We then applied these equations to all 633 patients with hip fractures treated at seven other hospitals (Group B) and compared the predicted and actual morbidity and mortality rates to assess the predictive ability of the E-PASS and Physiological and Operative Severity Score for the enUmeration of Mortality and Morbidity (POSSUM) systems. The ratio of actual to predicted morbidity and mortality rates was closer to 1.0 with the E-PASS than the POSSUM system. Our data suggest the E-PASS scoring system is useful for defining postoperative risk and its underlying algorithm accurately predicts morbidity and mortality rates in patients with hip fractures before surgery. This information then can be used to manage their condition and potentially improve treatment outcomes.
Level of Evidence: Level II, prognostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The aging of the population in developed countries has led to a worldwide increase in the number of patients with hip fractures [12]. Physical reserve capacity is decreased in the elderly [19], and 26% to 79% of patients admitted with hip fractures present with systemic complications and require physical assistance [11, 24, 27]. Fracture treatment can be problematic because concomitant medical conditions increase operative risk. In older patients, operative risk is a major determinant of the postoperative course. Numerous factors (eg, age, gender, comorbidity, dementia, walking ability before injury, fracture type, and timing of surgery) are reportedly associated with increased risk for mortality after hip fracture, and several risk scores for predicting postoperative risk have been proposed [4, 11, 13, 14, 27].
The Estimation of Physiologic Ability and Surgical Stress (E-PASS) score originally was developed by multiple regression analysis of patients treated with elective gastrointestinal surgery and included preoperative and intraoperative parameters (Table 1) [6]. When E-PASS was applied to gastrointestinal and pulmonary surgery, the comprehensive risk score (CRS) correlated with mortality and morbidity rates [6, 17, 31]. We reported the postoperative hospital morbidity and mortality rates increased linearly with the preoperative risk score (PRS) and CRS and they correlated in patients who had undergone osteosynthesis or arthroplasty for hip fracture [8, 9]. Furthermore, equations for predicting 30-day and inhospital mortality rates using the CRS correlated well with observed mortality rates in patients undergoing elective gastrointestinal surgery [7].
The Physiological and Operative Severity Score for enUmeration of Mortality and Morbidity (POSSUM) involving physiologic and operative assessments (Table 2) was developed by multivariate discriminant analysis as a means for predicting 30-day morbidity and mortality [3]. The Portsmouth predictor modification (P-POSSUM) [28] was developed to overcome the overprediction of hospital mortality by POSSUM, especially in low-risk patients. The POSSUM and P-POSSUM systems are the most reliable and widely applicable scoring methods devised to date in general surgery [3, 22]. The orthopaedic POSSUM system (O-POSSUM) also has been validated as a method to assess 30-day morbidity and mortality rates in patients having orthopaedic surgery [15]. However, these scoring systems are not practical to predict postoperative risk in patients with hip fractures. If the postoperative course can be predicted before surgery, this information will aid in obtaining proper informed consent from the patients and in treatment planning and risk management discussions.
The purpose of our study was therefore to (1) establish equations for estimating morbidity and mortality rates in candidates for hip fracture surgery using the E-PASS system; (2) determine the usefulness of the equations in a different patient group; and (3) compare the predictive quality of the E-PASS and POSSUM systems.
Materials and Methods
This study was performed at eight member hospitals of the Japanese National Hospital Organization. We retrospectively reviewed all 722 patients (154 men, 568 women) operated on between April 2002 and December 2005 at an emergency hospital for hip fracture (Group A; Table 3). Surgical procedures were selected based on the type of fracture. We perform hip arthroplasty in patients with displaced femoral neck fractures and osteosynthesis in those with nondisplaced neck fractures or intertrochanteric or subtrochanteric fractures (Table 3). We calculated their E-PASS scores using their preoperative status and surgical stress parameters derived from medical records and applied the algorithms and definitions to calculate their individual E-PASS scores (Table 1) [6, 8]. We then examined the relationship between the E-PASS scores and the rate of postoperative morbidity and inhospital mortality. Postoperative complications were included only if the patient had received medical or interventional treatment; complications such as pneumonia, hypotension, stroke, heart failure, renal dysfunction, wound infection, delirium, cutting out of lag screw, hip dislocation, and decubitus ulcer were recorded in the patient’s medical record. Complications developed in 124 of the 722 patients in Group A (17.2%; Table 3). The crude mortality rate was 1.7% (12 of 722 patients). Using these data, we obtained equations to predict the morbidity and mortality rates with the PRS.
With the equations acquired with the E-PASS system, we assessed the morbidity and mortality rates in all 633 patients (139 men, 494 women) operated on between September 2003 and December 2005 for hip fractures at seven other participating hospitals (Group B; Table 3). We then compared these rates with the patients’ actual postoperative course. We considered the observed to estimated ratio (O/E ratio) of morbidity and mortality a risk-adjusted quality measure. The O/E ratios defined by E-PASS were subjected to linear analysis [7, 29]; it calculates the average individual risk in each risk band and multiplies the result by the number of individuals in the band. Ratios greater than and less than 1.0 are indicative of underprediction and overprediction, respectively. When the value of observed and expected rates was zero, the ratio was recorded as 1.0.
We also calculated the estimated morbidity and mortality rates using the POSSUM systems (Table 2) [3] and evaluated the O/E ratios. We predicted the inhospital mortality rates with P-POSSUM [28] and the morbidity and mortality rates 30 days after surgery with O-POSSUM [15]. We used Group B data for prediction of inhospital mortality by P-POSSUM and defined the O/E ratios by linear analysis [29]. For the assessment of 30-day morbidity and mortality rates, we used data acquired in patients whose postoperative hospital stay exceeded 30 days and in patients who manifested morbidity or died within fewer than 30 postoperative days. The O/E ratios for O-POSSUM were determined by exponential analysis [29], which considers a cutoff risk at each stage of the calculation. All patients with a predicted risk greater than the cutoff threshold were grouped together. For the lowest cutoff (0%), we avoided multiplication by zero by using the median predicted risk of the less than 10% mortality band. We then compared the O/E ratios obtained with the E-PASS and POSSUM systems for inhospital and 30-day morbidity and mortality rates. The end point of our study was discharge from the hospital or predischarge death at the hospital where the patients underwent surgery.
We applied regression analysis, including simple, polynomial, multiple, stepwise, exponential, logarithmic, power, and growth regression, to best fit the coordinates of the morbidity and mortality rates and the PRS [7]. Using the ranked Spearman correlation coefficient, we analyzed the correlation between the E-PASS scores and the rate of postoperative morbidity or mortality and between the predicted and actual postoperative course. Intergroup differences between Groups A and B were assessed with the Mann-Whitney U test for continuous variables or with the chi square test with Yates’ correction for continuity in categorical variables. For statistical analyses, we used StatView® 5.0 software (SAS Institute Inc, Cary, NC).
Results
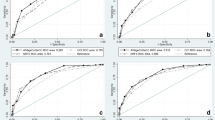
Postoperative morbidity rates increased linearly with the PRS (Fig. 1A) and CRS (Fig. 1B) and correlated with the PRS (ρ = 0.17, p < 0.0001) and CRS (ρ = 0.17, p < 0.0001) in all 722 patients in Group A. The mortality rates also correlated with the PRS (ρ = 0.16, p < 0.0001) (Fig. 1A) and CRS (ρ = 0.18, p < 0.0001) (Fig. 1B). However, the surgical stress score (SSS) was not correlated with postoperative morbidity (ρ = 0.01, p = 0.8) or mortality rates (ρ = 0.01, p = 0.8). Among the regression models we used to analyze the relationship between the morbidity and mortality rates and the PRS, a polynomial model best fit these relationships (Fig. 2). These analyses yielded the following equations: Y1 = −16.15X2 + 48.189X − 9.535 for morbidity rates (R = 0.991, n = 6, p = 0.002) and Y2 = 13.362X2 − 11.277X + 1.969 for mortality rates (R = 0.988, n = 6, p = 0.004), in which Y1 is the estimated morbidity rate, Y2 is the estimated mortality rate, and X is the PRS.
(A) A bar chart shows the relationship between the PRS and postoperative morbidity and mortality rates in 722 patients in Group A. The PRS correlated with the morbidity (ρ = 0.17, p < 0.0001) and mortality rates (ρ = 0.16, p < 0.0001). (B) A bar chart shows the relationship between the CRS and postoperative morbidity and mortality rates. The CRS correlated with the morbidity (ρ = 0.17, p < 0.0001) and mortality rates (ρ = 0.18, p < 0.0001).
Postoperative morbidity and mortality curves were defined by the PRS. The relationship between the PRS and mortality rates was analyzed by polynomial regression analysis. Each coordinate indicates the average PRS and morbidity rate at each PRS range. The equations used to obtain the estimated rates for morbidity and mortality were Y = −16.15(PRS)2 + 48.189(PRS) − 9.535 (R = 0.991, n = 6, p = 0.002) and Y = 13.362(PRS)2 − 11.277(PRS) + 1.969 (R = 0.988, n = 6, p = 0.004), respectively.
In the second cohort of 633 patients (Group B), the morbidity and mortality rates estimated by the PRS correlated with the actual morbidity (ρ = 0.17, p < 0.0001) and mortality rates (ρ = 0.12, p = 0.002). The O/E ratios for morbidity and mortality were 1.06 and 0.71, respectively (Table 4).
Comparison of the E-PASS and POSSUM systems showed the O/E ratios for inhospital and 30-day postoperative morbidity and mortality were closer to 1.0 with E-PASS than with POSSUM (Table 5). All morbidity and mortality rates predicted by POSSUM were overestimated.
Discussion
A fundamental requirement of patient autonomy is acquisition of the patient’s informed consent based on discussions that also address the risks of any proposed treatments. Emphasis has been placed on consent in the process of informed, shared decision making [2, 26]. Morbidity and mortality rates are essential outcome measures to judge the quality of medical care. Surgical risk must be assessed carefully and conveyed to patients, and patients must be managed according to their specific medical conditions. Therefore, we performed this study to (1) establish equations for estimating morbidity and mortality rates in candidates for hip fracture surgery after evaluating the correlation between the E-PASS scores and these rates; (2) evaluate the usefulness of the equations; and (3) compare the predictive quality of the E-PASS and POSSUM systems.
We note several limitations. First, simple application of these equations resulted in some problems; the equation for morbidity yielded a negative value for the morbidity rates when the PRS was less than 0.213, although the PRS varied from 0.120 to 1.548 in these patients. However, there were no postoperative complications in patients whose PRS was less than 0.3. Therefore, this equation should be used only when the PRS is 0.213 or greater. Similarly, the equation for mortality yielded a negative value when the PRS ranged from 0.247 to 0.597 and produced rates exceeding 100% when it was greater than 3.163. Moreover, the mortality rates increased when the PRS decreased to less than 0.247, although no patients whose PRS was less than 0.6 died. Therefore, this equation should be used only when 0.597 ≤ PRS < 3.163. Second, this study is setting the end point at the time of discharge from or predischarge death at the hospital at which the patients underwent surgery. In the calculations of predicted 30-day morbidity and mortality rates, we excluded patients whose postoperative hospitalization was less than 30 days and who manifested no complications, because they were transferred to institutions specializing in rehabilitation or to nursing homes. According to Parker et al. [21], among that group of patients, the incidence of complications within 30 days of hospital discharge is low and their inclusion in our calculations would have resulted in a lower actual morbidity rate within the first 30 postoperative days. Third, the length of postoperative hospitalization in orthopaedic hospitals varies; it is 6.5 days in the United States [16], 25.5 days in England [10], and 50.4 days in Japan [25]. These and differences in healthcare systems in individual countries may affect applicability of the E-PASS system. In a study of 41,331 patients with hip fractures covered by the US Medicare program and operated on between 1999 and 2002, 7579 (18.3%) were readmitted within 30 days [5]. As that percentage was similar to the morbidity rates in our study population, we suggest our equations are applicable not only to patients treated in Japan but also to those treated in the United States.
The E-PASS system considers the patients’ physiologic status and surgical stress [6]. Haga et al. [7] used the CRS to establish equations for predicting 30-day and inhospital mortality rates. They reported an excellent correlation between predicted and observed mortality in patients treated by elective gastrointestinal surgery. We reported the PRS and CRS were well correlated with surgical outcomes in patients with hip fractures and they were effective and reproducible for prediction of the postoperative course at surgical hospitals in earlier [8, 9] and current studies. Because the PRS facilitates prediction of the postoperative course before patients are subjected to surgery, we suggest it is the preferable method for obtaining equations for morbidity and mortality prediction in patients considered for hip fracture surgery.
We applied the equation developed for morbidity estimation in patients treated at an emergency hospital (Group A) to patients treated at different types of hospitals (Group B). The O/E ratio for morbidity that occurred during hospitalization was 1.06 (estimated rate × 0.95), indicating the E-PASS score is valuable for predicting the incidence of postoperative complications; nevertheless, the average duration of hospitalization for Group B was considerably longer than for Group A. However, E-PASS overestimated by 1.4-fold and 1.8-fold the predicted rate of inhospital and 30-day mortality, respectively, compared with the predictive values in gastrointestinal surgery [7]. To validate the mortality rates predicted by E-PASS, we are performing additional studies on larger study populations and long-term followup.
We compared the equations obtained with E-PASS for predicting morbidity and mortality rates with predictions yielded by POSSUM systems, which are the best available systems for assessing outcomes by risk adjustment analysis in various types of surgery [3, 22]. The predicted rates for inhospital and 30-day morbidity and mortality calculated by POSSUM systems were overestimated by 2.6-fold to 6.7-fold compared with those by E-PASS. Others reported O-POSSUM overpredicted mortality and morbidity in 1164 [23] and 225 [32] patients who underwent surgery for hip fractures, whereas Wright et al. [30] reported the rates predicted by O-POSSUM agreed well with the actual morbidity and mortality rates observed in 230 hip fractures. POSSUM also overpredicted mortality in patients undergoing general surgery [22, 29] and in patients subjected to gastrointestinal surgery; POSSUM and P-POSSUM overpredicted mortality in hospitalized patients during the first 30 postoperative days by a greater degree than E-PASS [7]. These findings are consistent with our observations, suggesting E-PASS more correctly predicts the actual morbidity and mortality rates than the POSSUM system.
Using E-PASS, we developed acceptable equations for predicting morbidity and mortality in patients scheduled for hip fracture surgery. In individual patients, our equations yield more accurate predicted morbidity and mortality rates than the POSSUM systems. The spread of computerization and availability of calculation software such as Microsoft® Excel® render calculation of E-PASS scores and of the predictive morbidity and mortality rates easy and practically applicable with E-PASS algorithms and predictive equations. The E-PASS score is effective and reproducible as an audit tool to predict the postoperative course of patients considered for hip fracture surgery.
References
Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–553.
Charles C, Whelan T, Gafni A. What do we mean by partnership in making decisions about treatment? BMJ. 1999;319:780–782.
Copeland GP, Jones D, Walters M. POSSUM: a scoring system for surgical audit. Br J Surg. 1991;78:355–360.
Elliott J, Beringer T, Kee F, Marsh D, Willis C, Stevenson M. Predicting survival after treatment for fracture of the proximal femur and the effect of delays to surgery. J Clin Epidemiol. 2003;56:788–795.
French DD, Bass E, Bradham DD, Campbell RR, Rubenstein LZ. Rehospitalization after hip fracture: predictors and prognosis from a national veterans study. J Am Geriatr Soc. 2008;56:705–710.
Haga Y, Ikei S, Ogawa M. Estimation of Physiologic Ability and Surgical Stress (E-PASS) as a new prediction scoring system for postoperative morbidity and mortality following elective gastrointestinal surgery. Surg Today. 1999;29:219–225.
Haga Y, Wada Y, Takeuchi H, Kimura O, Furuya T, Sameshima H, Ishikawa M. Estimation of Physiologic Ability and Surgical Stress (E-PASS) for a surgical audit in elective digestive surgery. Surgery. 2004;135:586–594.
Hirose J, Mizuta H, Ide J, Nakamura E, Takada K. E-PASS for predicting postoperative risk with hip fracture: a multicenter study. Clin Orthop Relat Res. 2008;466:2833–2841.
Hirose J, Mizuta H, Ide J, Nomura K. Evaluation of Estimation of Physiologic Ability and Surgical Stress (E-PASS) to predict the postoperative risk for hip fracture in elder patients. Arch Orthop Trauma Surg. 2008;128:1447–1452.
Jarman B, Aylin P, Bottle A. Discharge destination and length of stay: differences between US and English hospitals for people aged 65 and over. BMJ. 2004;328:605.
Jiang HX, Majumdar SR, Dick DA, Moreau M, Raso J, Otto DD, Johnston DW. Development and initial validation of a risk score for predicting in-hospital and 1-year mortality in patients with hip fractures. J Bone Miner Res. 2005;20:494–500.
Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726–1733.
Kenzora JE, McCarthy RE, Lowell JD, Sledge CB. Hip fracture mortality: relation to age, treatment, preoperative illness, time of surgery, and complications. Clin Orthop Relat Res. 1984;186:45–56.
Masuda T, Miura N, Ishii S, Hibino Y, Beppu M. New preoperative evaluation system of the physical findings of aged patients with femoral neck fracture. J Orthop Sci. 2004;9:434–439.
Mohamed K, Copeland GP, Boot DA, Casserley HC, Shackleford IM, Sherry PG, Stewart GJ. An assessment of the POSSUM system in orthopaedic surgery. J Bone Joint Surg Br. 2002;84:735–739.
Nguyen-Oghalai TU, Kuo YF, Zhang DD, Graham JE, Goodwin JS, Ottenbacher KJ. Discharge setting for patients with hip fracture: trends from 2001 to 2005. J Am Geriatr Soc. 2008;56:1063–1068.
Oka Y, Nishijima J, Oku K, Azuma T, Inada K, Miyazaki S, Nakano H, Nishida Y, Sakata K, Izukura M. Usefulness of an Estimation of Physiologic Ability and Surgical Stress (E-PASS) scoring system to predict the incidence of postoperative complications in gastrointestinal surgery. World J Surg. 2005;29:1029–1033.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–655.
Oskvig RM. Special problems in the elderly. Chest. 1999;115:158S–164S.
Owens WD, Felts JA, Spitznagel EL Jr. ASA physical status classifications: a study of consistency of ratings. Anesthesiology. 1978;49:239–243.
Parker MJ, Pryor GA, Myles J. 11-year results in 2,846 patients of the Peterborough Hip Fracture Project: reduced morbidity, mortality and hospital stay. Acta Orthop Scand. 2000;71:34–38.
Prytherch DR, Whiteley MS, Higgins B, Weaver PC, Prout WG, Powell SJ. POSSUM and Portsmouth POSSUM for predicting mortality: Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity. Br J Surg. 1998;85:1217–1220.
Ramanathan TS, Moppett IK, Wenn R, Moran CG. POSSUM scoring for patients with fractured neck of femur. Br J Anaesth. 2005;94:430–433.
Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331:1374.
Sakamoto K, Nakamura T, Hagino H, Endo N, Mori S, Muto Y, Harada A, Nakano T, Yamamoto S, Kushida K, Tomita K, Yoshimura M, Yamamoto H. Report on the Japanese Orthopaedic Association’s 3-year project observing hip fractures at fixed-point hospitals. J Orthop Sci. 2006;11:127–134.
Towle A, Godolphin W. Framework for teaching and learning informed shared decision making. BMJ. 1999;319:766–771.
Wehren LE, Hawkes WG, Orwig DL, Hebel JR, Zimmerman SI, Magaziner J. Gender differences in mortality after hip fracture: the role of infection. J Bone Miner Res. 2003;18:2231–2237.
Whiteley MS, Prytherch DR, Higgins B, Weaver PC, Prout WG. An evaluation of the POSSUM surgical scoring system. Br J Surg. 1996;83:812–815.
Wijesinghe LD, Mahmood T, Scott DJ, Berridge DC, Kent PJ, Kester RC. Comparison of POSSUM and the Portsmouth predictor equation for predicting death following vascular surgery. Br J Surg. 1998;85:209–212.
Wright DM, Blanckley S, Stewart GJ, Copeland GP. The use of orthopaedic POSSUM as an audit tool for fractured neck of femur. Injury. 2008;39:430–435.
Yamashita S, Haga Y, Nemoto E, Nagai S, Ohta M. E-PASS (The Estimation of Physiologic Ability and Surgical Stress) scoring system helps the prediction of postoperative morbidity and mortality in thoracic surgery. Eur Surg Res. 2004;36:249–255.
Young W, Seigne R, Bright S, Gardner M. Audit of morbidity and mortality following neck of femur fracture using the POSSUM scoring system. N Z Med J. 2006;119:U1986.
Acknowledgments
We thank Drs. Hiroshi Usui, Yuri Yabuki (NHO Tokyo Medical Center), Yukio Nakatsuchi, Yutaka Tateiwa (NHO Nagano National Hospital), Toshiaki Miyahara, Taro Mawatari (NHO Kyusyu Medical Center), Satoshi Motokawa, Kiyofumi Mitsutake (NHO Nagasaki Medical Center), Kazuhiko Ihara (NHO Beppu Medical Center), Satoshi Maeda (NHO Kumamoto Medical Center), and Tateki Segata (NHO Kumamoto Saisyunso National Hospital) for supplying patient data. We also thank Dr. Haga (NHO Kumamoto Medical Center) for technical advice on statistics.
Author information
Authors and Affiliations
Corresponding author
Additional information
One of the authors (JH) has received funding from a research grant for the Policy-based Medical Services Network for Musculoskeletal Diseases (#771).
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
About this article
Cite this article
Hirose, J., Ide, J., Irie, H. et al. New Equations for Predicting Postoperative Risk in Patients with Hip Fracture. Clin Orthop Relat Res 467, 3327–3333 (2009). https://doi.org/10.1007/s11999-009-0915-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-009-0915-6