Abstract
Purpose of Review
Catheter-related blood stream infections (CRBSI) pose a significant risk to patients on home parenteral nutrition (HPN). Recurrent loss of catheters can lead to scarring and eventual loss of central access, a potentially fatal situation for patients dependent on HPN.
Recent Findings
In the past, the standard of care to treat these infections required catheter removal. More recently, several studies have indicated that many CRBSI can be treated without removal of the catheter. Successful treatment without removal can be achieved by intentionally following a catheter salvage protocol. We define this as a previously defined protocol to accurately diagnose CRBSI, identify the organism(s) involved, and effectively treat not only the blood stream infection, but also sterilize the catheter.
Summary
For patients on HPN with CRBSI, consider attempting line salvage if the patient is not suffering from severe sepsis, other infection related complications, or certain specific infections. Success rates vary depending on the organism causing the infection and the risks; benefits and chance of success should be considered when deciding to attempt line salvage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Home parental nutrition (HPN) remains a foundation in the management of intestinal failure and can result in extension of life in those who are unable to meet their nutritional needs through oral intake [1]. In contrast to Europe, the prevalence of HPN in the United States (US) has declined slightly over the last few decades with recent data showing that more than 25,000 Americans are receiving HPN [2,3,4]. Despite extensive research and advances in provision of total parenteral nutrition (TPN) at home, HPN can be associated with a number of complications. Catheter-related blood stream infection (CRBSI) remains a primary concern and in some reports has been the most common line associated complication of HPN [5, 6••, 7]. There has been discrepancy on how to best treat these infections with many providers pulling the catheter in order to prevent the CRBSI from turning into a wide-spread infection with sepsis. Unfortunately, this approach can be associated with risk of replacing catheters as well as potential for total loss of intravascular access due to thrombosis or scarring from recurrent catheter placements. Due to this, recent reports and guidelines have begun to recommend catheter salvage in certain situations [7, 8].
While prevention of infection, and other catheter complications, is of utmost importance, this article will briefly review when to consider blood stream infection in HPN patients, how to diagnose CRBSI, when to consider catheter salvage, and some of the uncertainties in management of this complication.
History of CRBSI
From the early days of HPN, infection has been a primary concern and cause for loss of catheters [9,10,11]. Early PN centers reported on the incidence of catheter removal and evaluated prognostic factors that could predict the need for removal [9, 11]. In the early days of HPN, initial management of HPN patients with sepsis that was attributed to a catheter infection precipitated catheter removal [9]. Several of these early papers do note that at times, the infection was able to be treated without removal of the catheter, but this was not described with an intent to salvage the catheter [9]. Unlike catheter removal, salvage involves an intentional process or protocol intended to attempt to save the CVC from removal by accurately diagnosing CRBSI, identification of the causative organism, and treatment not only of the blood stream infection, but also sterilization of the catheter. Development of silicone catheters and other advances in the CVCs utilized to administer HPN have contributed to the reduced risk of complications [10].
Identification of Blood Stream Infections (CRBSI and CLABSI)
Different definitions have been used when reporting CRBSI or central line associated blood stream infections (CLABSI). While often used interchangeably, the Center for Disease Control and Prevention differentiates between CRBSI and CLABSI noting that CRBSI requires testing to identify the catheter as the source of blood stream infection, while CLABSI is a blood stream infection that occurs within 48 h of a patient having a central line and is not due to a metastatic infection [12]. Differences in definitions and use of CRBSI and CLABSI utilized in the HPN literature have most likely contributed to the significant variation in reported rates of blood stream infections in HPN patients [13]. Given the implications for removal of a CVC, potential loss of vascular access, and need for recurrent invasive procedures, we recommend use of CRBSI criteria to minimize these complications by localizing the source of infection from the catheter in HPN patients. Reported rates of CRBSI have ranged from 0.38–4.58/1000 catheter days in one review [14] to 0.35–11.5/1000 catheter days in another report [6••]. The most common organism identified is gram-positive cocci, consistent with skin flora [14, 15••, 16].
Diagnosis of blood stream infections in HPN patients has been an area of controversy since the early days of HPN [11, 17]. While HPN monitoring includes routine laboratory testing, as well as instructions to patients on how to monitor for symptoms of infection including fever, these may not be as sensitive as anticipated as one retrospective review noted that 13 of 37 episodes of CRBSI did not have documented fever [18]. This study found that laboratory studies including white blood cell count, c-reactive protein (CRP), albumin, and bilirubin were associated with infection [18]. Others have reported that given lack of specific symptoms, there was a delay of an average of 6 days between start of symptoms and evaluation for infection [19]. Given the potential life-threatening nature of blood stream infections, patients and providers must be vigilant monitoring for these symptoms and be swift to seek evaluation when there is concern for possible infection. While patients can be treated based on symptomatic concern for infection, if considering catheter salvage, verification of the diagnosis of line infection is critical, particularly as treatment will need to be tailored based on confirmation of the diagnosis, and identification of the organism.
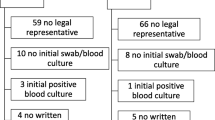
The first step when considering catheter salvage in an HPN patient is appropriate evaluation of symptoms of infection. While different societies have used different diagnostic criteria over time, European Society for Clinical Nutrition and Metabolism (ESPEN) guidelines state that “diagnosis of CRBSI is best achieved by (a) quantitative or semi-quantitative culture of the catheter (when the CVC is removed or exchanged over a guide wire), or (b) by paired quantitative blood cultures or paired qualitative blood cultures from a peripheral vein and from the catheter, with continuously monitoring of the differential time to positivity (if the catheter is left in place).” [8] Such diagnostic criteria are consistent with the 2009 clinical practice guidelines of Infectious Disease Society of America (IDSA) [20]. The IDSA guidelines provide more detailed guidance based on duration of line, type of line, etc.
Certainly, the ability of patients to have blood cultures obtained from both the periphery and central line may not be feasible. In such instances, it is advisable to obtain blood cultures from whatever source possible, prior to the administration of antibiotics. Further treatment decisions will depend on these results and clinical course.
Factors Impacting Salvage Attempts and Success
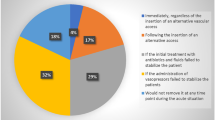
There are multiple published studies with detailed catheter salvage protocols [13, 15••, 16, 21••]. Consistent across the published protocols, salvage is not considered in the hemodynamically unstable patient or when there is concern for metastatic infection (endocarditis, osteomyelitis, etc.) [15, 21••]. It is also recommended that salvage not be performed in short-term catheters, such as peripherally inserted central catheters (PICCs) [8]. This recommendation is presumably based on ease of insertion and removal, the design to be temporary, and data suggesting that salvage is more successful in tunneled catheters as opposed to non-tunneled catheters [19]. However, in patients nearing total loss of vascular access who have a PICC, a blood stream infection and subsequent loss of access with concern about the possibility of achieving new access, consideration could be given to an attempt to salvage a PICC.
These reports have demonstrated high overall rates of salvage ranging from 67 to 81% of the salvages attempted but success is impacted by the organism(s) causing the infection (see Table 1) [15••, 16, 18, 21••]. While salvage success rates vary in the studies, best success is reported with coagulase negative staph with reported success rates ranging from 78 to 92% [15••, 16, 18, 21••]. While there has been less success with other bacteria, there have been varying rates of success with both gram-positive and gram-negative bacteria, including polymicrobial infections [15••, 21••]. Infection with methicillin-resistant staphylococcus is more difficult to salvage than methicillin-sensitive staphylococcus (MSSA), but has been achieved even though the IDSA guidelines recommend not to salvage for this organism [15••, 20, 21••]. One of the potential reasons MSSA may be salvageable in HPN patients is that typical CRBSI is detected early prior to hemodynamic instability thus allowing for clearance of the bacteria source contained in the catheter. Two studies have reported attempts and success at salvaging lines in fungal infections [13, 15••]. The likely reason for attempted salvage in fungal infections is that the catheter may be the last option for vascular access in patients almost completely dependent on HPN for nutrition. No studies have reported success in salvaging mycobacterial infections [9, 15••]. In general, given the poor success of salvaging MRSA, fungal, polymicrobial, mycobacterial, and pseudomonal infections, given the low risk of success, strong consideration should be given to the risks versus benefits before attempting salvage in these cases.
Once infection has been suspected and cultures are drawn, the line is not used for parenteral nutrition of IV fluids for at least 24 h [9, 12, 16]. The protocols vary in whether antimicrobial therapy is administered via the CVC or the periphery; regardless of how systemic antimicrobials are administered, the line should be “locked” with antimicrobials [6••, 15••, 19]. Some of the protocols also included treatment with a thrombolytic (urokinase); however, it does not appear that treatment with a kinase has been compared head to head to treatment without a kinase [21••]. See Fig. 1 for a suggested starting algorithm for evaluation and management of CRBSI.
Success has been reported when comparing both 10–15-day courses of IV therapy [19, 21••]. One protocol indicates the possibility of 7–14 days of treatment, but does not delineate how it was determined how long patients should be treated [15••]. There is also no consensus on empiric antimicrobial therapy to start while awaiting culture results that will allow for targeted antimicrobial therapy. Clinical judgment in each CRBSI considering severity of illness, duration of need of HPN, medication allergies, antibiotic availability, and local resistance patterns should all be considered when selecting initial antimicrobials for systemic and lock therapy.
There is not consistency on when blood cultures should be repeated. One study has shown that cultures repeated and negative at 48 h were predictive of successful treatment [16, 18]. Others defined successful salvage as resolution of symptoms without reporting routine repeat culture results [13] and others do not specify how clearance of infection was determined [15].
There remains concern about the long-term safety and impact of catheter salvage. Some data suggests that in patients with salvage, there is less time to diagnosis of new infection as compared to patients treated with catheter removal [22]. However, as there are many patients who have recurrent CRBSI, it remains to be determined if recurrent infection is more closely associated with the salvage of the catheter or other host factors.
Discussion about treatment of tunnel site infection is not routinely discussed and was a cause for catheter removal in some studies [13, 21••]. Another study reports that salvage after tunnel infections has decreased over the years and catheter removal has increased [7]. However, further work is needed to define tunnel infection, identification of microorganisms causing these infections, and treatment protocols.
In addition, while appropriate identification of CRBSI and salvage in appropriate situations is crucial, prevention of these and all catheter-associated infections would be optimal to decrease morbidity and mortality in these patients. Factors to consider in order to decrease the risk of line associated infection when considering placement of a CVC for HPN including a tunneled catheter with the fewest number of lumens possible and appropriate training of the patient and/ or caregivers who will be administering the HPN [14]. There has been controversy regarding the use of prophylactic ethanol or antimicrobial locks and such therapies are not routinely recommended [1, 8, 23, 24].
Conclusion
While and advances are being made in other strategies to manage intestinal failure, HPN remains a life-saving measure for many patients. Given the prevalence of CRBSI, and the potential for recurrence and need for ongoing vascular access, not just for HPN, but also potentially for other IV therapies, dialysis or other treatments, strategies to minimize disruption in, or loss of vascular access is crucial. However, given the poor salvage success in fungal, MRSA, and polymicrobial infections, except in cases of extenuating circumstances, it is generally best to remove these lines and not attempt salvage in these cases. In addition to catheter loss from CRBSI, several studies have reported catheter loss to tunnel infections. Given the paucity of data on this topic, and lack of published protocols, salvage in these situations could be considered based in clinical situations, but further study is needed.
Certainly, prevention of CRBSI and other HPN-associated infections would be optimal and factors associated with increased risk of these infections have been reported [14]. However, as infections continue to arise in this population, catheter salvage is ideal to help maintain vascular access and decrease risks associated with recurrent CVC placement.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Pironi L, Arends J, Bozzetti F, Cuerda C, Gillanders L, Jeppesen PB, et al. ESPEN guidelines on chronic intestinal failure in adults. Clin Nutr Edinb Scotl. 2016;35(2):247–307.
Brandt CF, Hvistendahl M, Naimi RM, Tribler S, Staun M, Brøbech P, et al. Home parenteral nutrition in adult patients with chronic intestinal failure: the evolution over 4 decades in a tertiary referral center. JPEN J Parenter Enteral Nutr. 2017;41(7):1178–87.
Santarpia L, Pagano MC, Pasanisi F, Contaldo F. Home artificial nutrition: an update seven years after the regional regulation. Clin Nutr. 2014;33(5):872–8.
Mundi MS, Pattinson A, McMahon MT, Davidson J, Hurt RT. Prevalence of home parenteral and enteral nutrition in the United States. Nutr Clin Pract. 2017;17:0884533617718472.
Gillanders L, Baxter J, Ball P, Merrie A, McKee RF. Benchmarking home parenteral nutrition in Scotland and New Zealand: disparities revealed. N Z Med J. 2008;121(1284):28–33.
•• Dibb M, Lal S. Home parenteral nutrition: vascular access and related complications. Nutr Clin Pract. 2017;32(6):769–76. This article discussed many different types of vascular complications and procedures to help manage these complications.
Brandt CF, Tribler S, Hvistendahl M, Naimi RM, Brøbech P, Staun M, et al. Home parenteral nutrition in adult patients with chronic intestinal failure: catheter-related complications over 4 decades at the Main Danish tertiary referral center. J Parenter Enter Nutr. 2018;42(1):95–103.
Pittiruti M, Hamilton H, Biffi R, MacFie J, Pertkiewicz M. ESPEN. ESPEN guidelines on parenteral nutrition: central venous catheters (access, care, diagnosis and therapy of complications). Clin Nutr. 2009;28(4):365–77.
Buchman AL, Moukarzel A, Goodson B, Herzog F, Pollack P, Reyen L, et al. Catheter-related infections associated with home parenteral nutrition and predictive factors for the need for catheter removal in their treatment. J Parenter Enter Nutr. 1994;18(4):297–302.
Miller DG, Ivey M, Ivey T, Scribner BH. Experience with an indwelling right atrial catheter for home parenteral nutrition. Surg Gynecol Obstet. 1980;151(1):108–10.
Broviac JW, Scribner BH. Prolonged parenteral nutrition in the home. Surg Gynecol Obstet. 1974;139(1):24–8.
Terminology | BSI | Guidelines Library | Infection Control | CDC [Internet]. [cited 2018 Jun 11]. Available from: https://www.cdc.gov/infectioncontrol/guidelines/bsi/background/terminology.html.
Tribler S, Brandt CF, Hvistendahl M, Staun M, Brøbech P, Moser CE, et al. Catheter-related bloodstream infections in adults receiving home parenteral nutrition: substantial differences in incidence comparing a strict microbiological to a clinically based diagnosis. JPEN J Parenter Enteral Nutr. 2018 Feb;42(2):393–402.
Dreesen M, Foulon V, Spriet I, Goossens GA, Hiele M, De Pourcq L, et al. Epidemiology of catheter-related infections in adult patients receiving home parenteral nutrition: a systematic review. Clin Nutr. 2013;32(1):16–26.
•• Edakkanambeth Varayil J, Whitaker JA, Okano A, Carnell JJ, Davidson JB, Enzler MJ, et al. Catheter salvage after catheter-related bloodstream infection during home parenteral nutrition. JPEN J Parenter Enteral Nutr. 2017;41(3):481–8. One large centers experience with CRBSI incidence, organisms, and detailed protocol to salvage catheters.
Bond A, Teubner A, Taylor M, Cawley C, Abraham A, Dibb M, et al. Assessing the impact of quality improvement measures on catheter related blood stream infections and catheter salvage: experience from a national intestinal failure unit. Clin Nutr 2017;1–5.
Hurt RT, Steiger E. Early History of Home Parenteral Nutrition: From Hospital to Home. Nutr Clin Pract [Internet]. [cited 2018 Sep 10];0(0). Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/ncp.10180.
Clare A, Teubner A, Shaffer JL. What information should lead to a suspicion of catheter sepsis in HPN? Clin Nutr. 2008;27(4):552–6.
Reimund J-M, Arondel Y, Finck G, Zimmermann F, Duclos B, Baumann R. Catheter-related infection in patients on home parenteral nutrition: results of a prospective survey. Clin Nutr. 2002;21(1):33–8.
Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O’Grady NP, et al. Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;49(1):1–45.
•• Dibb MJ, Abraham A, Chadwick PR, Shaffer JL, Teubner A, Carlson GL, et al. Central venous catheter salvage in home parenteral nutrition catheter-related bloodstream infections: long-term safety and efficacy data. JPEN J Parenter Enteral Nutr. 2016;40(5):699–704. One large centers experience with CRBSI incidence, organisms and catheter salvage protocol.
Béraud G, Seguy D, Alfandari S, Lenne X, Leburgue F, Faure K, et al. Factors associated with recurrence of catheter-related bloodstream infections in home parenteral nutrition patients. Eur J Clin Microbiol Infect Dis. 2012;31(11):2929–33.
Salonen BR, Bonnes SL, Vallumsetla N, Varayil JE, Mundi MS, Hurt RT. A prospective double blind randomized controlled study on the use of ethanol locks in HPN patients. Clin Nutr. 2018 Aug;37(4):1181–5.
Davidson JB, Edakkanambeth Varayil J, Okano A, Whitaker JA, Bonnes SL, Kelly DG, et al. Prevention of subsequent catheter-related bloodstream infection using catheter locks in high-risk patients receiving home parenteral nutrition. JPEN J Parenter Enteral Nutr. 2017;41(4):685–90.
Author information
Authors and Affiliations
Contributions
SB, MM, RH, and BS made substantial contributions to the concept and design of the article, the interpretation of data, and the critical revision of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of Interest
Sara L. Bonnes declares that she has no conflict of interest.
Manpreet S. Mundi declares that he has no conflict of interest.
Ryan T. Hurt is a consultant for Nestlé Nutrition.
Bradley R. Salonen declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Gastroenterology, Critical Care, and Lifestyle Medicine
Rights and permissions
About this article
Cite this article
Bonnes, S.L., Mundi, M.S., Hurt, R.T. et al. To Pull or Not to Pull: Salvaging Central Line Catheters in Home Parenteral Nutrition. Curr Nutr Rep 7, 324–328 (2018). https://doi.org/10.1007/s13668-018-0245-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13668-018-0245-y