Abstract
The effect of repeated multicycle gonadotropin-releasing hormone antagonist (GnRH-ant) protocols on oxidative stress (OS) in follicular fluid (FF) and ovarian granulosa cells (GCs) remains unclear. This study investigated the effects of repeated multicycle GnRH-ant protocols on OS markers of FF and ovarian GCs. A total of 145 patients were enrolled and divided into four groups: 1 cycle group (n = 42), 2 cycles group (n = 37), 3 cycles group (n = 45), and 4–5 cycles group (n = 21). The FF and ovarian GCs of the patients were collected on the day of last oocyte retrieval and the levels of 8-hydroxy-2-deoxyguanosine (8-OHdG), malondialdehyde (MDA), superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GSH-Px) were tested by ELISA. The results showed that the serum estradiol levels on hCG injection day in the 3 and 4–5 cycles were significantly (P < 0.05) lower than in the 1 and 2 cycles. The number of retrieved oocytes (12.1 ± 3.3 in cycle 1, 11.7 ± 3.1 in cycle 2, 10.4 ± 2.4 in cycle 3, and 9.4 ± 2.4 in cycles 4–5), embryos with two pronuclei (7.6 ± 3.0 in cycle 1, 7.0 ± 2.5 in cycle 2, 6.2 ± 2.6 in cycle 3, and 5.5 ± 2.1 in cycles 4–5), and the rates of high-quality embryos (52.2% in cycle 1, 47.9% in cycle 2, 38.6% in cycle 3, and 36.5% in cycles 4–5), implantation (35.4% in cycle 1, 32.4% in cycle 2, 23.8% in cycle 3, and 22.9% in cycles 4–5) and clinical pregnancy (50.0% in cycle 1, 43.2% in cycle 2, 33.3% in cycle 3, and 23.8% in cycles 4–5) in cycles 3 and 4–5 were significantly (P < 0.05) lower than those in cycles 1 and 2. Compared with 1 and 2 cycles, the 8-OHdG and SOD were significantly increased in the 3–5 cycles, while the CAT and GSH-Px levels were significantly decreased. Together, this study reveals repeated COS with the use of GnRH-ant protocols results in OS and changes the follicle microenvironment of FF and GCs, possibly leading to poor IVF outcomes in patients with 3–5 cycles of COS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Controlled ovarian stimulation (COS) is the use of exogenous gonadotropin to promote the growth of multiple follicles in in vitro fertilization (IVF) procedures. Although the technology continues to improve, the average pregnancy rate per cycle in assisted reproduction is about 30–40% [1], and some patients even need repeated COS for successful pregnancy. Furthermore, clinical evidence has suggested that fertilization, implantation, and pregnancy rates decline with increase of repeated COS cycles [2,3,4]. Repeated COS has been shown to induce oxidative stress (OS) and increase the levels of DNA damage marker 8-hydroxy-2-deoxyguanosine (8-OHdG) and lipid peroxidation marker 4-hydroxynonenal (4-HNE) in the mice ovaries and poor-quality oocytes [5, 6]. However, the effect of repeated COS, especially the gonadotropin-releasing hormone antagonist (GnRH-ant) protocol, on the OS markers in follicular fluid (FF) and ovarian granulosa cells (GCs) of IVF patients was largely unclear.
GnRH-ant protocol is one of the commonly used protocols in assisted reproduction. It has the advantages of short ovulation induction time, low gonadotropins hormone (Gn) dosage, and low risk of ovarian hyperstimulation [7,8,9]. However, the effect of the antagonist protocol on pregnancy outcomes remains controversial. Studies have shown no difference between antagonist and flare-up protocols [10]. Lainas et al. believed that antagonist protocol has a higher sustained pregnancy rate [11], while Demirol et al. suggested that the flare-up protocol is more suitable for patients with low ovarian response [12]. A study confirmed that different COS protocols had different effects on the follicular microenvironment [13], and the GnRH-ant protocol was associated with an increase in OS compared with the GnRH agonist protocol [14]. However, it was not clear whether an increase of the COS cycle in the GnRH-ant protocol would aggravate OS. Furthermore, whether the OS is associated with the pregnancy outcome of multiple COS cycles with GnRH-ant protocol was unclear.
In the COS process, FF and GCs play an important role in the development of follicles and maturation of oocytes [15,16,17]. Under pathological conditions, OS can impair FF microenvironment and ovarian GCs, thereby affecting oocyte quality and pregnancy outcomes [18, 19]. 8-OHdG is a sensitive indicator of DNA damage caused by OS. In the process of assisted reproduction, excessive 8-OHdG in ovarian GCs can reduce the fertilization rate and embryo quality [20]. Malondialdehyde (MDA) is an aldehyde substance produced during lipid peroxidation that can indirectly reflect the severity of reactive oxygen species (ROS) damage to cells. After COS, the MDA level was significantly increased [21], and the level of MDA in the FF of successful pregnant women undergoing IVF was lower [22]. Superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GSH-Px) are important antioxidant enzymes in the body. Matos et al. [23] found that a high level of SOD activity was related to successful IVF pregnancy. Patients with good IVF outcomes had higher CAT levels in endometrial secretions [24], and CAT activity in FF was correlated with fertilization rate and cleavage rate [25]. Cocchia et al. [26] have reported that the cleavage rate of embryos cultured in vitro was significantly increased after adding GSH-Px. Therefore, we speculated that the 8-OHdG, MDA, SOD, CAT, and GSH-Px in FF and ovarian GCs could reflect the changes in the microenvironment during repeated COS process and affect the pregnancy outcome.
In this study, we aimed to investigate the levels of OS markers in FF and ovarian GCs of patients with one or repeated COS cycles using GnRH-ant protocols, as well as the relationship between OS and clinical pregnancy outcomes, so as to provide an experimental basis for clinical treatment selection.
Materials and methods
Experiment design
This study was approved by the Ethics Committee of Hebei University of Chinese Medicine (Shijiazhuang, China), and all enrolled IVF-ET patients had signed informed consent to participate. All methods were performed in accordance with the relevant guidelines and regulations. In this study, 145 patients who met the inclusion criteria were enrolled from January 2018 to August 2019. The inclusion criteria were: (1) IVF-ET due to tubal factors or male factors or both; (2) age < 38 years; (3) regular menstruation; (4) basic follicular stimulating hormone (FSH) < 10 IU/L; and (5) COS with GnRH-ant protocols for 1–5 cycles. The exclusion criteria were the same as in the previous study [27]: (1) the uterus does not have pregnancy function or cannot bear pregnancy due to serious physical disease, patients suffering from serious mental disorders, urinary and reproductive system infection, sexually transmitted diseases, drug use and other serious bad habits, and patients with exposure to teratogenic radiation or poison and in the action period; (2) endometriosis, uterine fibroids, tuberculosis, uterine adhesion, and endometrial lesions; and (3) polycystic ovary syndrome, ovarian cyst, and hydrosalpinx.
IVF process
All patients were treated with a GnRH-ant protocol. Recombinant gonadotropin (Gn, Gonal-F; Merck Serono; Merck KGaA, Darmstadt, Germany) was used on the second day of menstruation to promote follicular growth. Gn dosage was adjusted according to B-ultrasound and serum estrogen levels. GnRH-ant was added daily after the leading follicle reached a diameter of 14 mm and carried on until the human chorionic gonadotrophin (hCG) injection day. hCG (250 μg, Merck Serono; Merck KGaA, Darmstadt, Germany) was injected at night when the diameter of at least 2 or 3 follicles reached 18 mm in both ovaries, and the number of follicles above 14 mm matched the level of estrogen in the serum. Oocytes were harvested 36 h after hCG injection via ultrasound-guided transvaginal puncture oocyte retrieval surgery. Oocytes were picked out and placed in incubators for fertilization. The ratio of the number of 2PN and 2PB to the number of COCs inseminated is the IVF fertilization rate, whereas the ratio of the number 2PN and 2PB to the number of MII oocytes injected is the ICSI fertilization rate. The FF containing GCs was placed in sterile enzyme-free centrifuge tubes for further separation and detection.
Embryos were transferred on the third day after fertilization. Morphology and cell number of embryos were observed before transplantation to determine embryo quality. According to the Istanbul Consensus [28] and Vienna Consensus [29] when 7–9 cells of the third-day embryo have uniform cell size and the fragmentation rate was less than 10%, the embryo was classified as grade 1. The number of blastomeres in grade 2 embryos was consistent with the development stage, and the fragmentation rate was 11–25%. The blastomeres were even without vacuoles or multinucleation, and the zona pellucida was normal. The number of blastomeres in grade 3 embryos was not consistent with the development stage, and the fragmentation rate was 26–35%. The blastomeres were uneven, with a few vacuoles, no multinucleation, and abnormal zona pellucida. Grade 1 and 2 embryos are considered high-grade embryos. Implantation rate was defined as the ratio of the number of gestational sacs to the number of embryos transferred. Each patient was transplanted with 1–2 embryos, and the gestational sac and even fetal heart were observed under B-ultrasound 4 weeks after transplantation, which was considered as a clinical pregnancy.
Isolation and extraction of FF and ovarian GCs
The collected FF and GCs suspensions were centrifuged at 4 °C (433×g, 10 min). The supernatant, namely FF, was absorbed and stored in a − 80 °C refrigerator for further detection. PBS was added into the below sediment to 5 ml and mixed upside down. Human lymphocyte separation fluid (Lympholyte-H, Cedarlane Laboratories, Canada) was added to 5 ml in a 10 ml centrifuge tube with an inclined angle of 45°. PBS suspension was slowly added to the surface of the human lymphocyte separation solution before being centrifuged at 4 °C (680×g, 10 min). The white floc in the middle layer was GCs. About 200–300 μl of 0.2% hyaluronidase (H8030, Beijing Solarbio Science & Technology, Beijing, China) was added to the extracted GCs. After blowing and digestion for 3 min, 1 ml of PBS was added to terminate digestion and centrifuged at 4 °C (982×g, 5 min). The supernatant was removed and PBS was added to wash twice. The GCs were put into a − 80 °C refrigerator for further detection.
Measurement of 8-OHdG, MDA, SOD, CAT, and GSH-Px levels
The kits used for the detection of MDA, SOD, CAT, and GSH-Px were purchased from Jiancheng Bioengineering Institute (Nanjing, China), and 8-OHdG was tested using 8-hydroxy-2-deoxyguanosine ELISA kits (ab201734, Abcam, USA). The FF and ovarian GCs sample lysis fluid was diluted to the optimal concentration to meet the standard curve. Then, the operation was carried out according to manual instructions. The absorbance values were measured by the enzyme-linked immunoassay (VersaMax, Molecular Devices, USA). Because different samples had different numbers of GCs, the BCA protein concentration assay kit (PC0020, Solarbio, China) was used to determine the protein concentration in each GCs sample.
Statistical analysis
The SPSS 21.0 software (SPSS Inc., Chicago, IL, USA) was used for data analysis. Continuous variables were tested for normality using the Shapiro–Wilk test. Student t test was used for data conforming to the normal distribution. For non-normally distributed data, Mann–Whitney U test was used. The Pearson Chi-square test was used to compare the rates between samples. The logical regression analysis was used to predict the effect of COS cycles on clinical pregnancy outcomes, and the OR value (95% CI) indicated the degree of correlation. The Spearman correlation coefficient was used to analyze the correlation between OS markers and antioxidant enzymes, and the r value represented the correlation coefficient. Statistical results were expressed as mean ± standard deviation, median (interquartile range [IQR]), and proportions. P values < 0.05 were considered statistically significant.
Results
Basic characteristics of patients
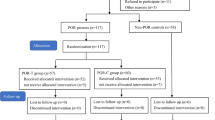
145 patients were enrolled and divided into four groups: 1 cycle (n = 42), 2 cycles (n = 37), 3 cycles (n = 45), and 4–5 cycles (n = 21). No significant (P > 0.05) differences existed in age, body mass index (BMI), duration of infertility, primary infertility rate, infertility reasons, levels of basic FSH, anti-mullerian hormone (AMH), endometrial thickness on hCG administration day, and days of stimulation among the four groups (P > 0.05) (Table 1 and Fig. 1a–c, f).
Comparison of characteristics and laboratory indicators in four groups. aP < 0.05 compared with group cycle 1; bP < 0.05 compared with group cycle 2; cP = 0.072 compared with group cycle 1. BMI body mass index, FSH follicular stimulating hormone, Gn gonadotropin hormone, 2PN embryos with two pronuclei
Compared with the 1 cycle group (12.6 ± 2.6 and 3271.6 ± 1229.3, respectively), the antral follicular count (AFC) and serum estradiol levels on hCG day were significantly (P < 0.05) decreased in 3 cycles (11.3 ± 2.4 and 2783.8 ± 766.2, P = 0.017 and 0.031, respectively) and 4–5 cycles group (10.8 ± 3.1 and 2490.8 ± 1055.5, P = 0.019 and 0.016, respectively), whereas total gonadotropin hormone (Gn) dosage was significantly increased in 3 cycles (2674.2 ± 557.1 vs 2399.1 ± 502.3, P = 0.018) compared with 1 cycle group (Table 1 and Fig. 1d, e, g).
The AFC was significantly decreased in the 3 cycles (11.3 ± 2.4, P = 0.031) and 4–5 cycles (10.8 ± 3.1, P = 0.028) group compared with the 2 cycles group (12.5 ± 2.5). The serum estradiol levels on hCG day were significantly (P = 0.030) decreased in the 4–5 cycles (2490.8 ± 1055.5) compared with the 2 cycles (3154.9 ± 1110.0) group (Table 1). These data suggested that 3 and more cycles of GnRH-ant protocol COS decrease the number of basal antral follicles and serum estradiol levels on hCG day, but increase the total Gn dosage in these patients (Table 1 and Fig. 1d, e, g).
Laboratory indicators and pregnancy outcomes
Compared to the 1 cycle group, the number of retrieved oocytes and 2PN, and high-grade embryo rate (12.1 ± 3.3, 7.6 ± 3.0, and 52.2% in cycle 1) (Table 2 and Fig. 1h, i) were significantly lower in the 3 cycle (10.4 ± 2.4, 6.2 ± 2.6, and 38.6%, with P = 0.006, 0.027, and 0.001, respectively) and 4–5 cycles group (9.4 ± 2.4, 5.5 ± 2.1, and 36.5%, with P = 0.000, 0.006, and 0.004, respectively). The rates of implantation and clinical pregnancy were significantly lower in the 4–5 cycles (22.9% and 23.8%, respectively, P < 0.05) than in the 1 cycle (35.4% and 50%) group.
The number of retrieved oocytes and high-grade embryos rate were significantly lower in the 3 cycles (10.4 ± 2.4 and 38.6%, with P = 0.032 and 0.029, respectively) and 4–5 cycles group (9.4 ± 2.4 and 36.5%, with P = 0.005 and 0.041, respectively) compared with the 2 cycles (11.7 ± 3.1 and 47.9%) group. The number of 2PN embryos was significantly (P = 0.022) lower in the 4–5 cycles (5.5 ± 2.1) than in the 2 cycles (7.0 ± 2.5) group, with no significant (P = 0.252) differences detected in the 3 cycles (6.2 ± 2.6) compared with the 2 cycles group (5.5 ± 2.1) (Table 2 and Fig. 1h, i). These results confirmed that repeated GnRH-ant protocol cycles of COS can affect IVF outcomes and decrease the number of retrieved oocytes and 2PN embryos, as well as the rates of high-grade embryo, implantation, and clinical pregnancy.
Association of COS cycles with the number of fertilization, high-grade embryos, and clinical pregnancy
The Spearman correlation coefficient was used to analyze the association, and a statistically significant (P < 0.05) negative correlation was found in the COS cycles with the number of fertilization (r = − 0.295, P < 0.000) and high-quality embryos (r = − 0.338, P < 0.000) (Table 3). The logical regression approach was used to analyze the effect of different COS cycles on clinical pregnancy outcomes. The results showed that the number of COS cycles was significantly (P < 0.05) negatively correlated with the clinical pregnancy outcome. Compared with the first cycle, COS in the 4–5 cycles significantly reduced the clinical pregnancy rate (OR 0.284, P = 0.035, Table 4).
OS markers in FF and ovarian GCs
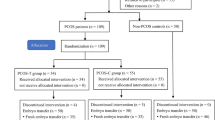
The OS markers in FF and GCs were tested. In the FF (Table 5 and Fig. 2), the 8-OHdG content was significantly increased in the 3 cycles (14.5 ± 2.8, P = 0.003) and 4–5 cycles (14.3 ± 3.6, P = 0.047) compared with the 1 cycle (12.7 ± 2.5) group. The SOD activity level was also significantly increased in the 4–5 cycles (38.6 ± 5.2, P = 0.040) compared with the 1 cycle (35.8 ± 5.0) group. The CAT activity level was significantly lower in the 3 cycles (1.1 ± 0.4, P = 0.033) than in the 1 cycle (1.3 ± 0.5) group. Compared to the 2 cycles group (2.0 ± 0.6 and 13.2 ± 3.0, respectively), the MDA and 8-OHdG content were significantly increased in the 3 cycles (2.3 ± 0.7 and 14.5 ± 2.8, with P = 0.032 and 0.047, respectively). The SOD activity level was significantly higher in the 4–5 cycles (38.6 ± 5.2, P = 0.007) than in the 2 cycles (35.0 ± 4.5) group. No significant (P > 0.05) difference was found in the GSH-Px activity level among the four groups.
Comparison of OS markers including a 8-OHdG, b MDA, c SOD, d CAT and e GSH-Px levels in FF and ovarian GCs of the four groups. aP < 0.05 compared with the 1 cycle group; bP < 0.05 compared to the 2 cycles group; cP = 0.053 compared to the 1 cycle group; dP = 0.071 compared to the 2 cycles group. FF follicular fluid, GCs granulosa cells, 8-OHdG 8-hydroxy-2-deoxyguanosine, MDA malondialdehyde, SOD superoxide dismutase, CAT catalase, GSH-Px glutathione peroxidase
In the GCs (Table 5 and Fig. 2), the 8-OHdG content (26.8 ± 7.8) and the SOD activity level (84.2 ± 29.5) were significantly (P < 0.05) higher in the 4–5 cycles than those in the 1 cycle (22.9 ± 5.3 and 66.6 ± 18.6, respectively) and 2 cycles (23.1 ± 5.4 and 69.4 ± 21.1, respectively) group. The GSH-Px activity level was significantly lower in the 3 cycles (47.4 ± 22.0) than in the 1 cycle (57.7 ± 20.1, P = 0.026) and 2 cycles (60.1 ± 19.0, P = 0.007) group. The GSH-Px activity level in the 4–5 cycles (50.4 ± 20.1) group also showed a downward trend compared with the 2 cycles (60.1 ± 19.0, P = 0.071) group. No significant (P > 0.05) difference was found among the four groups in MDA content and CAT activity level. These data showed that repeated COS for 3 or more cycles can significantly change the levels of OS markers, resulting in the oxidation–antioxidant imbalance.
A statistically significant negative correlation between 8-OHdG and antioxidant enzyme CAT (r = − 0.178, P < 0.05) in FF, between MDA and SOD (r = − 0.188, P < 0.05) in GCs, and between 8-OHdG and CAT (r = − 0.171, P < 0.05) in GCs were observed in four groups (Fig. 3). These results suggested that 8-OHdG, MDA, SOD, and CAT may play a more important role in detecting OS in follicles.
Discussion
This study was the first to assess OS markers in FF and ovarian GC of patients with different GnRH-ant protocol COS cycles, which found that with the increase of GnRH-ant protocol cycles, the serum estradiol levels on hCG day, number of retrieved oocytes and 2PN embryos, and rates of high-quality embryo, implantation, and clinical pregnancy were all significantly decreased, whereas the Gn usage showed an increasing trend. Compared with 1 or 2 cycles, the levels of 8-OHdG, SOD, GSH-Px, and CAT in the FF and ovarian GC of patients with 3–5 cycles were significantly changed, suggesting that repeated COS with the GnRH-ant protocol can result in OS and alter the follicle microenvironment, which might be one of the reasons for poorer IVF outcomes and decreased pregnancy rate in patients with 3–5 cycles compared to those with 1 or 2 cycles.
Our results showed that the AFC in both ovaries and the serum estradiol levels on hCG day decreased with the increase of COS cycles, except for the 2 cycles, whereas the use of total Gn dosage showed an increasing trend. Compared with 1 cycle and 2 cycles, the IVF outcomes (including the number of retrieved oocytes and 2PN embryos and the rates of high-quality embryo, implantation, and clinical pregnancy) were all significantly reduced in the 3–5 cycles. Current literature is not consistent on the effect of repeated COS on IVF outcomes. Most studies suggest that the success rate of IVF-ET decreased with the increase in the COS cycle [2,3,4, 30,31,32,33]. Rabinson et al. [4] studied the IVF data of patients with 1–8 cycles of antagonist protocols and found that, compared with 1–2 cycles, COS with 3–4 cycles and over 4 cycles could significantly reduce the clinical pregnancy rate, with the Gn usage significantly higher than that with 1–2 cycles. They also suggested that the COS protocols should be adjusted for patients with two failed antagonists [4]. Homburg et al. [33] applied all COS protocols into the scope of the study and found that compared with 1–3 cycles, the clinical pregnancy rate of 4–6 cycles and over was significantly reduced, whereas the Gn usage was significantly increased. Interestingly, there was no significant difference in pregnancy rates between cycles 4 and 6, cycles 7 and 9, cycles 10 and 12, and cycles 13 and 20 [33]. However, these authors did not compare pregnancy rates at cycles 1, 2, and 3. Another study [3] suggested that the number of 2PN and the rates of fertilization, implantations and pregnancy have significant decreased from the second cycle. Moreover, an analysis of data from 1177 patients with 1788 cycles showed that the clinical pregnancy rate in cycles 2 and 3 was significantly lower than that in cycle 1 [3].
However, Caligara et al. [34] showed that successive long agonist protocol stimulation cycles do not impair ovarian response, embryo quality, and pregnancy outcome. Kolibianakis et al. [35] proposed that repeated cycles did not exert a significant effect on the number of oocytes retrieved, but were only related to the age of females. In our study investigating patients with 1–5 cycles of COS, the results were consistent with most studies, suggesting that repeated COS had adverse effects on the patients’ pregnancy outcome. However, no significant difference was found in the pregnancy outcomes between 1 and 2 cycles, consistent with Rabinson’s results [4].
In our study, it was demonstrated that with the increase of COS cycle (3 cycles or more), the levels of oxidative damage product 8-OHdG increased significantly in the FF and ovarian GCs, suggesting repeated COS with antagonist protocol can result in OS and alter the follicle microenvironment. Park et al. [36] demonstrated that repeated superovulation caused OS and damaged the reproductive ovary environment, with the ROS levels being positively correlated with the number of ovulatory cycles [37]. Seino and Tamura et al. [20, 38] also confirmed that the 8-OHdG levels were closely related to the fertilization rate and embryo quality. Chao et al. [5] found that more cycles of ovarian stimulation had a higher content of oxidative damage, including 8-OHdG, lipoperoxides, and carbonyl proteins in ovaries. Similarly, Liu et al. [39] showed that after 1–6 cycles of continuous superovulation induction, the level of 8-OHdG significantly increased, the number of oocytes in stages MI and MII significantly decreased, and the fragmentation rate and proportion of unfertilized oocytes were significantly increased. In our study, the 8-OHdG levels in 3–5 cycles were higher than those 1–2 cycles, which were consistent with the results by Chao et al. [5] and Liu et al. [39]. Our study confirmed that repeated antagonist protocols did cause OS, and 8-OHdG might be an important indicator to predict the correlation between OS and pregnancy outcomes.
MDA is also a closely related indicator of pregnancy outcomes. In our study, the MDA only in the FF was significantly higher in cycle 3 than that in cycle 2, but no significant difference was found between other groups or in GCs. Some authors have suggested that the serum MDA concentration was increased after ovarian stimulation, with the MDA level being significantly higher in patients treated with an antagonist protocol than in those treated with an agonist protocol [21, 40]. However, others had an opposite finding [14]. But, no significant differences were detected in the clinical pregnancy outcomes. Our study did not find any correlation between MDA and IVF outcomes either, indicating that the MDA level is not closely related to repeated COS pregnancy outcomes.
SOD is a more important antioxidant enzyme than GSH-Px and CAT [41], and a low level of SOD is closely related to the low pregnancy rate [42]. However, in our study, it was found that the SOD level was significantly higher, while the pregnancy rate was significantly lower in 3–5 cycles than in 1–2 cycles. OS and 8-OHdG may activate the antioxidant system and increase the SOD level [43]. The increase of SOD might affect the levels of ROS, and a certain concentration of ROS is essential in promoting meiosis [44], consequently inhibiting the oocyte maturation. Crick et al. [14] found that while the GnRH-ant protocol increased the level of oxidative damage products, the SOD level increased correspondingly.
In our study, it was found that GSH-Px levels in GCs and CAT levels in FF were significantly reduced in patients with 3–5 cycles compared with 1–2 cycles, which suggested that the repeated antagonist protocol result in the reduction of antioxidant enzyme CAT and GSH-Px levels. GSH-Px increase was associated with the high-quality embryo and a higher chance of pregnancy [45], whereas decreased GSH-Px concentration had a negative impact on fertilization rate [46]. Patients with high ROS levels in FF had lower CAT levels [47]. Our results also confirmed that these two markers might be related to lower rates of high-quality embryo and clinical pregnancy caused by continuous multicycle ovulation induction, which can be used together with SOD as indicators to evaluate pregnancy outcome. In brief, these changes in the level of biochemical markers reflected that repeated GnRH-ant protocol alters the follicular microenvironment in IVF patients, resulting in an imbalance between oxidation and antioxidant.
Some limitations existed in this study, including a small cohort of patients, one single center study, Chinese patients enrolled only, investigation of COS of only 1–5 cycles without more cycles, and only the GnRH-ant protocols, which may all affect the publication bias. Future studies will have to resolve these issues for better outcomes.
Conclusion
In summary, the increase of COS cycle in GnRH-ant protocols has an adverse effect on pregnancy outcomes. Changes in the OS markers levels in FF and ovarian GCs of the patients with repeated COS may result in changes in the microenvironment of oocyte growth, leading to poor clinical pregnancy outcomes in repeated COS. This study provides experimental evidence for fertility specialists to use GnRH-ant drugs again and to adjust ovulation induction protocols for patients with repeated COS failure.
Availability of data and materials
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AMH:
-
Anti-Müllerian hormone
- BMI:
-
Body mass index
- CAT:
-
Catalase
- COS:
-
Controlled ovarian stimulation
- FF:
-
Follicular fluid
- FSH:
-
Follicular stimulating hormone
- GCs:
-
Granulosa cells
- Gn:
-
Gonadotropin hormone
- GnRH:
-
Gonadotropin-releasing hormone
- GSH-Px:
-
Glutathione peroxidase
- hCG:
-
Human chorionic gonadotrophin
- IVF-ET:
-
In vitro fertilization embryo transfer
- MDA:
-
Malondialdehyde
- OS:
-
Oxidative stress
- ROS:
-
Reactive oxygen species
- SOD:
-
Superoxide dismutase
- 4-HNE:
-
4-Hydroxynonenal
- 8-OHdG:
-
8-Hydroxy-2-deoxyguanosine
References
Nuñez-Calonge R, Cortés S, Gutierrez Gonzalez LM, Kireev R, Vara E, Ortega L, et al. Oxidative stress in follicular fluid of young women with low response compared with fertile oocyte donors. Reprod Biomed Online. 2016;32(4):446–56.
Silberstein T, Trimarchi JR, Gonzalez L, Keefe DL, Blazar AS. Pregnancy outcome in in vitro fertilization decreases to a plateau with repeated cycles. Fertil Steril. 2005;84(4):1043–5.
Shapiro BS, Richter KS, Harris DC, Daneshmand ST. Dramatic declines in implantation and pregnancy rates in patients who undergo repeated cycles of in vitro fertilization with blastocyst transfer after one or more failed attempts. Fertil Steril. 2001;76(3):538–42.
Rabinson J, Ashkenazi J, Homburg R, Meltcer S, Anteby EY, Orvieto R. Repeated in vitro fertilization cycle attempts in patients undergoing controlled ovarian hyperstimulation with use of gonadotropin-releasing hormone antagonists. Fertil Steril. 2009;91(4):1473–5.
Chao HT, Lee SY, Lee HM, Liao TL, Wei YH, Kao SH. Repeated ovarian stimulations induce oxidative damage and mitochondrial DNA mutations in mouse ovaries. Ann NY Acad Sci. 2005;1042:148–56.
Zhang J, Lai Z, Shi L, Tian Y, Luo A, Xu Z, et al. Repeated superovulation increases the risk of osteoporosis and cardiovascular diseases by accelerating ovarian aging in mice. Aging. 2018;10(5):1089–102.
Engel JB, Griesinger G, Schultze-Mosgau A, Felberbaum R, Diedrich K. GnRH agonists and antagonists in assisted reproduction: pregnancy rate. Reprod Biomed Online. 2006;13(1):84–7.
Pu D, Wu J, Liu J. Comparisons of GnRH antagonist versus GnRH agonist protocol in poor ovarian responders undergoing IVF. Hum Reprod. 2011;26(10):2742–9.
Al-Inany HG, Youssef MA, Aboulghar M, Broekmans F, Sterrenburg M, Smit J, et al. GnRH antagonists are safer than agonists: an update of a Cochrane review. Hum Reprod Update. 2011;17(4):435.
Akman MA, Erden HF, Tosun SB, Bayazit N, Aksoy E, Bahceci M. Comparison of agonistic flare-up-protocol and antagonistic multiple dose protocol in ovarian stimulation of poor responders: results of a prospective randomized trial. Hum Reprod. 2001;16(5):868–70.
Lainas TG, Sfontouris IA, Papanikolau EG, Zorzovilis JZ, Petsas GK, Lainas GT, et al. Flexible GnRH antagonist versus flare-up GnRH agonist protocol in poor responders treated by IVF: a randomized controlled trial. Hum Reprod. 2008;23(6):1355–8.
Demirol A, Gurgan T. Comparison of microdose flare-up and antagonist multiple-dose protocols for poor-responder patients: a randomized study. Fertil Steril. 2009;92(2):481–5.
Choi YS, Ku SY, Jee BC, Suh CS, Choi YM, Kim JG, et al. Comparison of follicular fluid IGF-I, IGF-II, IGFBP-3, IGFBP-4 and PAPP-A concentrations and their ratios between GnRH agonist and GnRH antagonist protocols for controlled ovarian stimulation in IVF-embryo transfer patients. Hum Reprod. 2006;21(8):2015–21.
Celik E, Celik O, Kumbak B, Yilmaz E, Turkcuoglu I, Simsek Y, et al. A comparative study on oxidative and antioxidative markers of serum and follicular fluid in GnRH agonist and antagonist cycles. J Assist Reprod Genet. 2012;29(11):1175–83.
Clavero A, Castilla JA, Núñez AI, García-Peña ML, Maldonado V, Fontes J, et al. Apoptosis in human granulosa cells after induction of ovulation in women participating in an intracytoplasmic sperm injection program. Eur J Obstet Gynecol Reprod Biol. 2003;110(2):181–5.
Coticchio G, Dal Canto M, Mignini Renzini M, Guglielmo MC, Brambillasca F, Turchi D, et al. Oocyte maturation: gamete-somatic cells interactions, meiotic resumption, cytoskeletal dynamics and cytoplasmic reorganization. Hum Reprod Update. 2015;21(4):427–54.
Ma CH, Yan LY, Qiao J, Sha W, Li L, Chen Y, et al. Effects of tumor necrosis factor-alpha on porcine oocyte meiosis progression, spindle organization, and chromosome alignment. Fertil Steril. 2010;93(3):920–6.
Karuputhula NB, Chattopadhyay R, Chakravarty B, Chaudhury K. Oxidative status in granulosa cells of infertile women undergoing IVF. Syst Biol Reprod Med. 2013;59(2):91–8.
Lu X, Wu Z, Wang M, Cheng W. Effects of vitamin C on the outcome of in vitro fertilization–embryo transfer in endometriosis: a randomized controlled study. J Int Med Res. 2018;46(11):4624–33.
Seino T, Saito H, Kaneko T, et al. Eight-hydroxy-2′-deoxyguanosine in granulosa cells is correlated with the quality of oocytes and embryos in an in vitro fertilization-embryo transfer program. Fertil Steril. 2002;77(6):1184–90.
Tulić L, Vidaković S, Tulić I, Ćurčić M, Stojnić J, Jeremić K. Oxidative stress markers in GnRH agonist and antagonist protocols in IVF. J Med Biochem. 2017;36(2):163–70.
Oral O, Kutlu T, Aksoy E, Fiçicioğlu C, Uslu H, Tuğrul S. The effects of oxidative stress on outcomes of assisted reproductive techniques. J Assist Reprod Genet. 2006;23(2):81–5.
Matos L, Stevenson D, Gomes F, Silva-Carvalho JL, Almeida H. Superoxide dismutase expression in human cumulus oophorus cells. Mol Hum Reprod. 2009;15(7):411–9.
Rahiminejad ME, Moaddab A, Ganji M, Eskandari N, Yepez M, Rabiee S, et al. Oxidative stress biomarkers in endometrial secretions: a comparison between successful and unsuccessful in vitro fertilization cycles. J Reprod Immunol. 2016;116:70–5.
Pasqualotto EB, Lara LV, Salvador M, Sobreiro BP, Borges E, Pasqualotto FF. The role of enzymatic antioxidants detected in the follicular fluid and semen of infertile couples undergoing assisted reproduction. Hum Fertil. 2009;12(3):166–71.
Cocchia N, Tafuri S, Del Prete C, Palumbo V, Esposito L, Avallone L, et al. Antioxidant supplementation to medium for in vitro embryo production in Felis catus. Pol J Vet Sci. 2019;22(3):573–9.
Liang Y, Cao QY, Gao X, Du H. Increased bone morphogenetic protein-6 in follicular fluid and granulosa cells may correlate with fertilization and embryo quality in humans. Exp Ther Med. 2017;14(2):1171–6.
Alpha scientists in reproductive medicine and ESHRE special interest group of embryology. The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Hum Reprod. 2011;26(6):1270–83.
ESHRE special interest group of embryology and alpha scientists in reproductive medicine. The Vienna consensus: report of an expert meeting on the development of art laboratory performance indicators. Hum Reprod Open. 2017;2017(2):hox11.
Simonstein F, Mashiach-Eizenberg M, Revel A, Younis JS. Assisted reproduction policies in Israel: a retrospective analysis of in vitro fertilization-embryo transfer. Fertil Steril. 2014;102(5):1301–6.
Wang F, Sun HX, Wang JX, Zhang NY, Hu YL. Pregnancy results from repeated cycles of in vitro fertilization and embryo transfer. Natl J Androl. 2010;16(11):1007–11.
Templeton A, Morris JK. Reducing the risk of multiple births by transfer of two embryos after in vitro fertilization. N Engl J Med. 1998;339(9):573–7.
Homburg R, Meltcer S, Rabinson J, Scharf S, Anteby EY, Orvieto R. Is there a limit for the number of in vitro fertilization cycles for an individual patient? Fertil Steril. 2009;91(4 Suppl):1329–31.
Caligara C, Navarro J, Vargas G, Simón C, Pellicer A, Remohí J. The effect of repeated controlled ovarian stimulation in donors. Hum Reprod. 2001;16(11):2320–3.
Kolibianakis E, Osmanagaoglu K, Camus M, Tournaye H, Van Steirteghem A, Devroey P. Effect of repeated assisted reproductive technology cycles on ovarian response. Fertil Steril. 2002;77(5):967–70.
Park SJ, Kim TS, Kim JM, Chang KT, Lee HS, Lee DS. Repeated superovulation via PMSG/hCG administration induces 2-Cys peroxiredoxins expression and overoxidation in the reproductive tracts of female mice[J]. Mol Cells. 2015;38(12):1071–8.
Kalthur G, Salian SR, Nair R, Mathew J, Adiga SK, Kalthur SG, et al. Distribution pattern of cytoplasmic organelles, spindle integrity, oxidative stress, octamer-binding transcription factor 4 (Oct4) expression and developmental potential of oocytes following multiple superovulation. Reprod Fertil Dev. 2016;28(12):2027–38.
Tamura H, Takasaki A, Miwa I, Taniguchi K, Maekawa R, Asada H, et al. Oxidative stress impairs oocyte quality and melatonin protects oocytes from free radical damage and improves fertilization rate. J Pineal Res. 2008;44(3):280–7.
Liu B, Wang JL, Wang XM, Zhang C, Dai JG, Huang XM, et al. Reparative effects of lycium barbarum polysaccharide on mouse ovarian injuries induced by repeated superovulation. Theriogenology. 2020;145:115–25.
Thaker R, Mishra V, Gor M, Agarwal R, Sheth H, Kapadia P, et al. The role of stimulation protocol, number of oocytes retrieved with respect to follicular fluid oxidative stress and IVF outcome. Hum Fertil (Camb). 2020;23(1):23–31.
Cetica PD, Pintos LN, Dalvit GC, Beconi MT. Antioxidant enzyme activity and oxidative stress in bovine oocyte in-vitro maturation. IUBMB Life. 2001;51(1):57–64.
Younis A, Clower C, Nelsen D, Butler W, Carvalho A, Hok E, et al. The relationship between pregnancy and oxidative stress markers on patients undergoing ovarian stimulations. J Assist Reprod Genet. 2012;29(10):1083–9.
Da Broi MG, de Albuquerque FO, de Andrade AZ, Cardoso RL, Jordão Junior AA, Navarro PA. Increased concentration of 8-hydroxy-2′-deoxyguanosine in follicular fluid of infertile women with endometriosis. Cell Tissue Res. 2016;366(1):231–42.
Takami M, Preston SL, Toyloy VA, Behrman HR. Antioxidants reversibly inhibit the spontaneous resumption of meiosis. Am J Physiol. 1999;276(4):E684–8.
Olszak-Wąsik K, Bednarska-Czerwińska A, Olejek A, Tukiendorf A. From, “every day” hormonal to oxidative stress biomarkers in blood and follicular fluid, to embryo quality and pregnancy success? Oxid Med Cell Longev. 2019;2019:1092415.
Paszkowski T, Traub AI, Robinson SY, McMaster D. Selenium dependent glutathione peroxidase activity in human follicular fluid. Clin Chim Acta. 1995;236(2):173–80.
Masjedi F, Keshtgar S, Agah F, Karbalaei N. Association between sex steroids and oxidative status with vitamin D levels in follicular fluid of non-obese PCOS and healthy women. J Reprod Infertil. 2019;20(3):132–42.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81774359, to HLD and No. 81803924, to LJF) and Postgraduate Innovation Funding Project of Hebei Province of China (No. CXZZBS2018150, to YCM).
Author information
Authors and Affiliations
Contributions
YCM, ZMZ and HLD designed this study. ZMZ and GMH collected cell samples, NC and YLF collected clinical data. YCM, YCC, ZWT, JRG and LJF detected the biochemical indicators. YCM, ZMZ and GMH analyzed the data; YCM and YCC wrote the manuscript. GBL revised the manuscript. ZMZ and HLD reviewed the manuscript. YCM and ZMZ contributed equally to this study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflicts of interest.
Ethics approval
This study was approved by the Ethics Committee of Hebei University of Chinese Medicine (Shijiazhuang, China).
Consent to participate
All enrolled patients had informed consent and signed informed consent forms.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ma, Y., Zhao, Z., Hao, G. et al. Effects of multicycle gonadotropin-releasing hormone antagonist protocols on oxidative stress of follicular fluid and ovarian granulosa cells. Human Cell 34, 1324–1334 (2021). https://doi.org/10.1007/s13577-021-00545-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13577-021-00545-9