Abstract
Purpose
For distal rectal tumors, abdominoperineal resection may achieve local control but with significant morbidity. High-dose radiation can improve pathologic response and allow for full-thickness local excision (FTLE) with comparable outcomes and improved morbidity. We report 15 years of data on distal rectal cancer treated with chemotherapy, intensity-modulated radiotherapy (IMRT), and FTLE via transanal endoscopic microsurgery.
Methods and materials
Forty-four patients were treated for cT1–T3, N0, and M0 distal rectal cancer using IMRT at 5580 cGy with 5-FU chemotherapy, followed by FTLE. Local recurrence (LR), disease-free survival (DFS), and overall survival (OS) were reported.
Results
Median follow-up was 51 months. Three patients (6.8%) had LR, all salvaged surgically. Mean DFS and OS are 8.56 and 9.10 years, respectively. DFS and OS were strongly associated with pathologic response to chemoradiotherapy (p = 0.043 and p = 0.023, respectively). Thirty-four patients (77%) are alive with no disease. Postoperative grade I–II complications noted in 17 patients and grade III complications in 2 patients. No patients required a diverting colostomy.
Conclusions
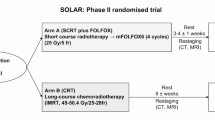
High-dose IMRT and chemotherapy followed by FTLE to treat distal rectal cancers are well tolerated and effective. FTLE may improve outcomes and minimize complications in appropriately selected patients. Randomized clinical trials are needed to compare it with standard surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Standard of care in the treatment of locally advanced rectal cancer involves neoadjuvant chemoradiotherapy (CRT) followed by surgical resection [1,2,3]. The method of surgical resection has historically been determined by the location of tumor within the rectum. For proximal tumors far from the anorectal ring, low anterior resections (LARs) may be performed, typically with preservation of the anus and without the need for a permanent colostomy. Treating rectal cancer in the distal third of the rectum, however, continues to be a challenge. Definitive treatment of locally invasive distal rectal cancer near or directly involving the anus often includes neoadjuvant therapy followed by an abdominoperineal resection (APR). In an APR, the anal sphincter is completely removed, and patients are left with permanent endostomy dependence. This standard multimodality therapy may achieve low rates of regional recurrence; however, it carries high rates of morbidity and mortality, up to 35% and 4–5%, respectively [4, 5].
As an alternative to the standard approach, many surgeons are performing local excision with transanal endoscopic microsurgery (TEM) as curative therapy in patients with localized disease. TEM was first pioneered by Dr. Buess, in collaboration with the Richard Wolf Company in Germany in the 1980s, and introduced into clinical practice in 1983 [5, 6]. TEM machinery allows for exceptional three-dimensional visualization of the surgical field and 6-fold magnification through a stereoscope. The TEM equipment provides a stable transanal surgical platform through an operating rectoscope, 4 cm wide and 20 cm long, and an endosurgical unit which allows for highly precise dissection capabilities [6]. Local excision has historically only been considered for patients who are high risk for more radical surgical resection, as local recurrence rates remained disappointingly high. More recent studies, however, suggest that early-stage tumors without high-risk features such as poor differentiation, vascular and neural invasion, mucinous histology, and ulceration have good long-term outcomes with local excision alone [5, 7,8,9,10].
A prior report evaluated short-term outcomes for rectal cancer patients undergoing TEM with or without preoperative chemoradiation. It was found that improved neoadjuvant therapies prior to TEM could decrease rates of local recurrence and improve both survival and sphincter preservation [11]. Assessment of response after neoadjuvant therapy plays an important role in predicting local recurrence postoperatively [12,13,14]. Park et al. showed that complete response was associated with a 5-year recurrence-free survival of 90.5% versus 78.7% and 58.5% for intermediate and poor response, respectively [15, 16]. Additionally, there is evidence to suggest a dose-adjusted response to radiation in rectal tumors [17,18,19]. Toxicities, however, mainly to the small bowel, remain the major limiting factor. Several studies have shown the ability of intensity-modulated radiation therapy (IMRT) to reduce the radiation dose to organs at risk (OARs) and therefore reduce the risk of gastrointestinal side effects [20,21,22,23,24,25].
Our aim is to show the feasibility and resultant toxicities of patients treated using high-dose IMRT with concurrent chemotherapy followed by TEM for T1–T3, N0, and M0 rectal cancer with a focus on tumors arising within the distal rectum. We reported on local recurrence (LR), disease-free survival (DFS), overall survival (OS), and resulting toxicities and compared outcomes based on response with neoadjuvant therapy.
Methods and materials
A retrospective analysis was performed on prospectively registered data collected from December 2004 to April 2017. It included forty-four patients who underwent neoadjuvant chemotherapy and concurrent radiation with IMRT, followed by TEM. Criteria used in the selection of patients included patients who were considered grade 3 or 4 high surgical risk based on the American Society of Anesthesiologists (ASA) or patients who had refused a more aggressive resection. Written informed consent was obtained with regard to the oncological risks of local excision and to possible intra- and postoperative complications.
Inclusion criteria were cT1–cT3, N0, and M0 tumors with a pathologically proven diagnosis of adenocarcinoma of the rectum. This included patients with variable high-risk features in the fixity of tumor, size, and associated ulceration. cT4 or node-positive patients were excluded from this study. Stage was determined by full-history and physical, detailed digital rectal exam (DRE), transrectal ultrasound (TRUS) to determine T stage, whole-body PET/CT, and pelvic MRI. In cases where T stage differed between diagnostic modalities, the most advanced T stage was used. Labs were drawn prior to treatment to confirm platelets > 100,000, absolute neutrophil count > 1800 cells/mm, hemoglobin > 8 g/dl, and calculated creatinine clearance > 50 ml/min. Preoperative tattooing of the tumor was performed prior to neoadjuvant therapy, and all patients were evaluated and presented at multidisciplinary rectal cancer conference before a treatment plan was decided upon. Patients went on to receive a median dose of 5580 cGy to the pelvis using a 9-field plan or volumetric arc therapy (VMAT) to the tumor and uninvolved lymph nodes. All patients received concurrent 5-FU-based chemotherapy; 52% received an infusion regimen, and 48% received oral capecitabine. All decisions regarding surgical approach were based on the postirradiated rectal cancer. TEM surgery was determined at the time of posttreatment evaluation by the surgeon after discussion with the patient and case review in multidisciplinary conference. TEM was considered an elective option for postirradiated < T2 cancers, 4 cm or less in size. Patients are comprised of two groups: (1) medically compromised patients: those patients who were too infirm to tolerate major surgery, and TEM represented their definitive therapy and (2) elective patients: patients who refused radical surgery or had a higher risk profile, but could withstand radical surgery. In this patient population, if the pathology was < T2, TEM represented definitive therapy; if the pathology was > T3 or N+, then an interval radical resection would take place after 12 weeks time. Patients that went on the received TEM were included in the study. Pathologic response to neoadjuvant therapy was evaluated on all surgical specimens. Complete response was defined as absence of viable tumor cells in the surgical specimen (ypT0N0). Intermediate response was defined as an improvement in stage to ypT1–2. Patients with ypT3–4 were considered poor responders. Patients were followed for evaluation of disease-free survival (DFS), overall survival (OS), and toxicity. Toxicity from neoadjuvant chemoradiation was graded according to the Common Terminology Criteria for Adverse Events (CTCAE). Postsurgical complications were graded according to the Dindo–Demartines–Clavien classification [26].
Surgery
Local excision/TEM
Transanal endoscopic microsurgery (TEM) is a local excision technique typically performed under general anesthesia. Preoperative localization and characterization of the tumor was performed with rigid and flexible sigmoidoscopy in the office setting. In the operating room, a TEM rectoscope with a diameter of 4 cm and a length of 20 cm was used. The scope has 4 work channels, a stereo optic vision channel, and a light source. There was also an insufflation port for maximum exposure. Twenty-six patients (59%) underwent disc excision, and 18 patients underwent hemicircumferential excision (41%). All patients were able to undergo complete closure of the defect as is our regular practice.
Radiation therapy
Simulation
The patients were simulated on a General Electric Lightspeed CT scanner (GEHC 3000 N Grandview, Blvd., Waukesha, WI, 53188) in the arm up supine position with a full bladder. The anal verge was marked with a radiopaque marker. Patients were then scanned with a 2.5-mm slice thickness, and images were obtained from the level of the L4 vertebral body to 5 cm below the ischial tuberosities. The CT image set and a magnetic resonance imaging (MRI) were fused prior to treatment planning.
IMRT target volume definition
Following the definitions of the International Commission on Radiologic Units and Measurements Reports Nos. 50 and 62 [27], the gross tumor volume (GTV) was defined as all-known disease as determined from the combination of physical exam, colonoscopy, endoscopic ultrasound, and MRI or PET/CT. Clinical target volume (CTV) was defined as the GTV plus all areas at risk for microscopic disease extension. The CTV for a T3 tumor included all areas of known rectal disease as well as internal iliac lymph nodes, the perirectal soft tissue space (mesorectum), and the presacral space. The planning target volume (PTV) provided 0.5-mm expansion around the CTV to compensate for intrafraction motion consequent to daily setup uncertainty and potential internal organ motion. The PTV was generated by expanding the above structures plus 0.5 cm. All OARs, including the small bowel, femoral heads, and bladder, were also contoured.
Treatment planning using IMRT
Step and shoot IMRT plans or VMAT plans were generated using Eclipse 11.0 treatment planning software (Varian Medical Systems, Palo Alto, CA). The planning systems produce optimal intensity-modulated profiles based on prescription dose–volume constraints of target and normal tissues defined by the user. A nine-field coplanar plan was generated using 6 MV photons equally spaced at 40-degree entry angles separating each. A prescription dose of 180 cGy per day to 5580 cGy was delivered to the PTV. The inverse planning goals included a homogeneous dose to the PTV while minimizing the dose delivered to the small bowel, rectum, and bladder. PTV dose–volume constraints were > 98% of the PTV receives ≥ 93% of the prescribed dose, ≤ 10% receives > 105%, and < 5% receives ≥ 110% of the prescribed dose, respectively.
OAR dose limitations were as follows: bladder dose limit was 50% to 40 Gy and 25% above 45 Gy with 10% of bladder volume receiving 50 Gy, small bowel dose constraints 200 cc to 35 Gy, 100 cc to 40 Gy, and 70 cc to 45 Gy. No small bowel received 50 Gy. The femoral heads were limited to 40% to 30 Gy, 25% above 45 Gy, and none received more than 50 Gy. The treatment plans and dose–volume histograms (DVHs) were then evaluated for absolute dose, coverage of PTV, and dose to OAR. All patients were in compliance with the criteria.
Chemotherapy
Concurrent preoperative chemotherapy was begun on day 1 of radiation and continued to the completion of radiation. Intravenous versus oral chemotherapy was at the physicians’ discretion. Intravenous 5-flurouracil (5-FU) was given at 225 mg/m2 continuous infusion over 24 h, 5 days a week during radiation. Capecitabine was given at 825 mg/m2 oral twice daily, 5 days a week with radiation. Twelve patients received adjuvant chemotherapy after surgery.
Statistical analysis
Disease-free survival was measured from the date of surgery to first occurrence of local disease recurrence, distant metastases, or death from any cause. Overall survival was measured from the date of surgery to the date of death from any cause. The Kaplan–Meier method was used to calculate the cumulative proportion surviving and to plot the survival curves; the log-rank test was used to compare multiple survival curves. All statistical analyses were performed using SPSS statistical software.
Limitations
Although the research has reached it aims, there were some limitations. First, likely the patients that went on to receive TEM included a well-selected group, likely reflecting the better overall, at baseline, group of patients. Therefore, to generalize the results to a broader group of patient, additional studies will have to be done involving more participants.
Results
Demographic and tumor characteristics are included in Table 1. All 44 patients completed neoadjuvant therapy without treatment breaks. The median operative time was 2.1 h (range 0.5–6.1 h), and median hospital stay was 2 days (range 0–4 days). Surgical specimens were assessed to determine response to neoadjuvant chemoradiotherapy. Complete response was defined as absence of viable tumor cells in the surgical specimen (ypT0N0). Good response was defined as an improvement in stage to ypT1–2 and ypN0. Patients with ypT3–4 or persistent lymph node metastasis were considered poor responders. Complete pathological response was achieved in 18 patients, and intermediate response was achieved in 25 patients. One patient had poor response and showed evidence of macroscopic tumor. No disease progression was seen between the end of neoadjuvant therapy and TEM. Median follow-up was 51 months. Three patients (6.8%) had isolated local recurrence; all of whom achieved local control with either reirradiation and/or surgical salvage. Six patients developed metastatic disease. One patient was found to have metastatic disease to the liver and lung at the time of TEM; she was censored at the time of analysis. Five (11%) patients eventually died from their metastatic cancer, and one had surgical salvage for an isolated liver lesion and is currently alive with no evidence of disease (NED). Five patients died from other causes outside of their malignancy. Mean DFS was 8.56 years with 95% confidence interval (CI) of 6.34 to 10.78 years (Fig. 1). Five-year DFS was calculated at 67.3%. Mean OS was 9.10 years (95% CI 6.80 to 11.39 years) (Fig. 2). Thirty-four patients (77%) are currently alive with NED. Recurrence according to response to preoperative chemoradiation is highlighted in Table 2. In adjusted analysis, DFS and OS were strongly associated with response to chemoradiotherapy (p = 0.043 and p = 0.023, respectively) (Figs. 3 and 4). Of the 29 patients that had a good response to neoadjuvant therapy, 3 developed local recurrence and 4 developed metastatic disease. Only one of the 19 patients who had a complete response to neoadjuvant therapy developed recurrence (this patient had local and metastatic recurrence found simultaneously).
Complications and toxicities
Toxicity from neoadjuvant chemoradiation was graded according to the Common Terminology Criteria for Adverse Events (CTCAE). There was no reported grade 3 or greater chemoradiotherapy-related toxicities. Thirteen patients (30%) reported grade 1–2 chemoradiotherapy-related toxicities, primarily diarrhea, skin changes, and neutropenia (Table 3). Postoperative grade III complications occurred in 2 patients. One developed delayed major wound separation and stenosis, requiring TEM reoperation about 11 months after the original surgery. The second patient had an early major wound separation requiring a diverting loop sigmoid colostomy which was eventually reversed once the area demonstrated adequate wound healing. Additional grade I–II postoperative complications were noted in 17 patients (Table 4). Minor wound separation accounted for a majority of reported postoperative complications and was managed conservatively with long-term oral antibiotics (doxycycline) and oral analgesics on an outpatient basis. No patients required a permanent diverting colostomy.
Discussion
Early-stage cancer in the distal third of the rectum is typically treated with neoadjuvant chemoradiation followed by extensive surgery with either abdominoperineal resection (APR) or low anterior resection (LAR). APR has shown high cure rates and low rates of local recurrence, but significant postoperative morbidity, including genitourinary and sexual dysfunction, anastomotic leak, long-term bowel dysfunction, and permanent ostomy dependence [5]. Our institutional experience demonstrates the efficacy and feasibility of preoperative radiation using IMRT, combined with single-agent chemotherapy, followed by full-thickness local excision via transanal endoscopic microsurgery (TEM) in early-stage (T1 up to T3) distal tumors [20,21,22,23].
The first prospective randomized trial comparing TEM vs. APR in the treatment of T1 N0 rectal cancer was published in 1996 and reported no significant difference in local recurrence (4.2%) and 5-year survival (96%) [28]. This was confirmed in later studies with the rate of local recurrence after resection of ypT1 lesions using TEM at 4–6%, not significantly different from the rates reported for conventional surgery [5]. The role of TEM in managing T2–T3 lesions, however, remains controversial. Lee et al. compared TEM with radical surgery in patients with T1 and T2 rectal adenocarcinomas. While T1 rectal cancer had comparable results in both arms, TEM carried a higher risk of local recurrence for T2 rectal cancers (19.5% vs. 9.4%, respectively, p = 0.04) [29]. A later meta-analysis reported the efficacy of TEM based on clinical stage with a local recurrence rate of 9.7% in T1 and significantly higher in T2 and T3 rectal cancers (25% and 38%, respectively) [30]. For these reasons, TEM had historically only been used in T2 and T3 tumors in patients with multiple comorbidities who are unable to tolerate a complete resection.
In a prior report in 2008, we reported that an improvement in neoadjuvant CRT may improve the previously unacceptable rates of local recurrence after TEM in T2 and T3 rectal tumors [11]. It is now well established that response to neoadjuvant CRT is a strong predictor of success after local excision [12,13,14]. RTOG 0247 demonstrated that an escalated dose of neoadjuvant chemotherapy resulted in unacceptable gastrointestinal toxicity [30]. This suggests that we are close to the acceptable limit of dose intensity of conventional chemotherapy, and in order to gain further improvement in a pathologic complete response, it is prudent to integrate more effective agents in neoadjuvant therapy. IMRT has been presented as an option to deliver higher doses of radiation while avoiding neighboring organs at risk (OARs). Guerrero et al. conducted a dosimetric analysis comparing three-dimensional conformal radiation therapy (3D-CRT) and both forward- and inverse-planned IMRTs. They found that IMRT improved small bowel sparing when compared with 3D-CRT by as much as a 64% reduction in the amount of small bowel receiving 45 Gy [32]. A study by Guerrieri et al. reported on an institutional experience with 425 patients with T1–T3 rectal cancer who underwent TEM after neoadjuvant standard chemotherapy with, a more novel, IMRT to a total dose of 5040 cGy, with an excellent reported local recurrence rate of 4.2%. [5]
In this prospective study, we were able to safely deliver higher doses of radiation, with a median of 5580 Gy, via IMRT. IMRT with chemotherapy resulted in excellent pathologic response in resected tumor specimens, with 41% of patients achieving a complete response. As demonstrated in preceding studies, this improvement in pathologic response was strongly associated with improved DFS and OS. Our local recurrence rate after FTLE via TEM was only 6.8%, with all patients able to proceed with surgical salvage. Our cohort of T1–T3 patients, with distal rectal cancer, that previously may have been subjected to and extensive APR and permanent ostomy, was able to be treated successfully with far more limited morbidity.
In summary, IMRT is well tolerated and effective and may allow for a minimally invasive approach to early-stage rectal cancer patients involving the lower third of the rectum. TEM has been shown to be an effective surgical approach for appropriately selected patients and provides the advantage of preservation of anal continence and avoidance of a colostomy. Additionally, effectively reducing radiation to the small bowel with IMRT may allow investigation of dose escalation of chemotherapy and/or radiation therapy in the neoadjuvant setting to improve pathologic response and disease control. More prospective studies looking at IMRT with TEM with larger numbers of patients need to be performed.
References
Gérard JP, Conroy T, Bonnetain F, Bouché O, Chapet O, Closon-Dejardin MT, Untereiner M, Leduc B, Francois É, Maurel J, Seitz JF (2006) Preoperative radiotherapy with or without concurrent fluorouracil and leucovorin in T3-4 rectal cancers: results of FFCD 9203. J Clin Oncol 24(28):4620–4625
Hofheinz R, Wenz F, Post S, Matzdorff A, Laechelt S, Mueller L, Link H, Moehler M, Burkholder I, Hochhaus A (2009) Capecitabine (Cape) versus 5-fluorouracil (5-FU)-based (neo-) adjuvant chemoradiotherapy (CRT) for locally advanced rectal cancer (LARC): safety results of a randomized, phase III trial. J Clin Oncol 27(15S):4014
Pozo ME, Fang SH (2015) Watch and wait approach to rectal cancer: a review. World J Gastrointest Surg 7(11):306–312
Guerrieri M, Gesuita R, Ghiselli R, Lezoche G, Budassi A, Baldarelli M (2014) Treatment of rectal cancer by transanal endoscopic microsurgery: experience with 425 patients. World J Gastroenterol: WJG 20(28):9556–9563
Kunitake H, Abbas MA (2012) Transanal endoscopic microsurgery for rectal tumors: a review. Perm J 16(2):45–50
Peeters KC, Marijnen CA, Nagtegaal ID, Kranenbarg EK, Putter H, Wiggers T, Rutten H, Pahlman L, Glimelius B, Leer JW, van de Velde CJ (2007) The TME trial after a median follow-up of 6 years: increased local control but no survival benefit in irradiated patients with resectable rectal carcinoma. Ann Surg 246(5):693–701
Maggiori L, Panis Y (2012) Transanal endoscopic microsurgery (TEM) for T1 rectal cancer. Acta chirurgica Iugoslavica 59(2):87–90
Veereman G, Vlayen J, Robays J, Fairon N, Stordeur S, Rolfo C, Bielen D, Bols A, Demetter P, D’hoore A, Haustermans K (2017) Systematic review and meta-analysis of local resection or transanal endoscopic microsurgery versus radical resection in stage i rectal cancer: a real standard? Crit Rev Oncol Hematol 114:43–52
Lu JY, Lin GL, Qiu HZ, Xiao Y, Wu B, Zhou JL (2015) Comparison of transanal endoscopic microsurgery and total mesorectal excision in the treatment of T1 rectal cancer: a meta-analysis. PLoS One 10(10):e0141427
Allaix ME, Arezzo A, Giraudo G, Morino M (2012) Transanal endoscopic microsurgery vs. laparoscopic total mesorectal excision for T2N0 rectal cancer. J Gastrointest Surg 16(12):2280–2287
Bujko K, Richter P, Smith FM, Polkowski W, Szczepkowski M, Rutkowski A, Dziki A, Pietrzak L, Kołodziejczyk M, Kuśnierz J, Gach T (2013) Preoperative radiotherapy and local excision of rectal cancer with immediate radical re-operation for poor responders: a prospective multicentre study. Radiother Oncol 106(2):198–205
Rödel C, Martus P, Papadoupolos T, Füzesi L, Klimpfinger M, Fietkau R, Liersch T, Hohenberger W, Raab R, Sauer R, Wittekind C (2005) Prognostic significance of tumor regression after preoperative chemoradiotherapy for rectal cancer. J Clin Oncol 23(34):8688–8696
Park IJ, You YN, Agarwal A, Skibber JM, Rodriguez-Bigas MA, Eng C, Feig BW, Das P, Krishnan S, Crane CH, Hu CY (2012) Neoadjuvant treatment response as an early response indicator for patients with rectal cancer. J Clin Oncol 30(15):1770–1776
Habr-Gama A, Gama-Rodrigues J, São Julião GP, Proscurshim I, Sabbagh C, Lynn PB, Perez RO (2014) Local recurrence after complete clinical response and watch and wait in rectal cancer after neoadjuvant chemoradiation: impact of salvage therapy on local disease control. Int J Radiat Oncol Biol Phys 88(4):822–828
Wiltshire KL, Ward IG, Swallow C, Oza AM, Cummings B, Pond GR, Catton P, Kim J, Ringash J, Wong CS, Wong R (2006) Preoperative radiation with concurrent chemotherapy for resectable rectal cancer: effect of dose escalation on pathologic complete response, local recurrence-free survival, disease-free survival, and overall survival. Int J Radiat Oncol Biol Phys 64(3):709–716
Myint AS (2014 Jun) Novel radiation techniques for rectal cancer. J Gastrointest Oncol 5(3):212–217
Gunther JR, Chadha AS, Shin US, Park IJ, Kattepogu KV, Grant JD, Weksberg DC, Eng C, Kopetz SE, Das P, Delclos ME (2017) Preoperative radiation dose escalation for rectal cancer using a concomitant boost strategy improves tumor downstaging without increasing toxicity: a matched-pair analysis. Adv Radiat Oncol
Verseveld M, De Graaf EJ, Verhoef C, van Meerten E, Punt CJ, de Hingh IH, Nagtegaal ID, Nuyttens JJ, Marijnen CA, de Wilt JH (2015) Chemoradiation therapy for rectal cancer in the distal rectum followed by organ-sparing transanal endoscopic microsurgery (CARTS study). Br J Surg 102(7):853–860
Issa N, Murninkas A, Schmilovitz-Weiss H, Agbarya A, Powsner E (2015) Transanal endoscopic microsurgery after neoadjuvant chemoradiotherapy for rectal cancer. J Laparoendosc Adv Surg Tech 25(8):617–624
Mohiuddin M, Paulus R, Mitchell E, Hanna N, Yuen A, Nichols R, Yalavarthi S, Hayostek C, Willett C (2013) Neoadjuvant chemoradiation for distal rectal cancer: 5-year updated results of a randomized phase 2 study of neoadjuvant combined modality chemoradiation for distal rectal cancer. Int J Radiat Oncol Biol Phys 86(3):523–528
Samuelian JM, Callister MD, Ashman JB, Young-Fadok TM, Borad MJ, Gunderson LL (2012) Reduced acute bowel toxicity in patients treated with intensity-modulated radiotherapy for rectal cancer. Int J Radiat Oncol Biol Phys 82(5):1981–1987
Wang JF, Li H, Xiong H, Huang H, Zou YM (2016) Influence of position and radiation technique on organs at risk in radiotherapy of rectal cancer. J Huazhong Univ Sci Technolog Med Sci 36(5):741–746
Zhao J, Hu W, Cai G, Wang J, Xie J, Peng J, Zhang Z (2016) Dosimetric comparisons of VMAT, IMRT and 3DCRT for locally advanced rectal cancer with simultaneous integrated boost. Oncotarget 7(5):6345–6351
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Bosset JF, Calais G, Mineur L, Maingon P, Radosevic-Jelic L, Daban A, Bardet E, Beny A, Briffaux A, Collette L (2005) Enhanced tumorocidal effect of chemotherapy with preoperative radiotherapy for rectal cancer: preliminary results—EORTC 22921. J Clin Oncol 23(24):5620–5627
Winde G, Nottberg H, Keller R, Schmid KW, Bünte H (1996) Surgical cure for early rectal carcinomas (T1). Dis Colon Rectum 39(9):969–976
Lee W, Lee D, Choi S, Chun H (2003) Transanal endoscopic microsurgery and radical surgery for T1 and T2 rectal cancer. Surg Endosc 17(8):1283–1287
Sengupta S, Tjandra JJ (2001) Local excision of rectal cancer. Dis Colon Rectum 44(9):1345–1361
Wong SJ, Winter K, Meropol NJ, Anne R, Kachnic LA, Rashid A, Watson JC, Mitchell EP, Pollock J, Lee RJ, Willett CG (2008) RTOG 0247: a randomized phase II study of neoadjuvant capecitabine and irinotecan versus capecitabine and oxaliplatin with concurrent radiation therapy for locally advanced rectal cancer. J Clin Oncol 26(15_suppl):4021
Guerrero Urbano MT, Henrys AJ, Adams EJ, Norman AR, Bedford JL, Harrington KJ, Nutting CM, Dearnaley DP, Tait DM (2006) Intensity-modulated radiotherapy in patients with locally advanced rectal cancer reduces volume of bowel treated to high dose levels. Int J Radiat Oncol Biol Phys 65(3):907–916
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Parikh, K., DeNittis, A.S., Marks, G. et al. Neoadjuvant chemotherapy and high-dose radiation using intensity-modulated radiotherapy followed by rectal sparing TEM for distal rectal cancer. J Radiat Oncol 8, 217–224 (2019). https://doi.org/10.1007/s13566-019-00389-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13566-019-00389-9