Abstract
Objective
Diabetes is an important risk factor for cardiovascular disease. The purpose of this study was to explore the role of diabetes and prediabetes in the risk of cardiovascular disease.
Methods
This prospective study was performed on three groups of non-diabetic (n = 7291), prediabetic (n = 438), and diabetic (n = 1713) in the age range of 40–70 years in Kharameh (Iran) in 2014–2021. The participants were followed for 4 years. Demographic information, chronic disease history, behavioral habits, and laboratory parameters were examined. Initially, the incidence density was calculated and the difference between the risk of cardiovascular disease in the three groups was examined using the log-rank test. The Cox regression model was performed to investigate the association between prediabetes and diabetes with the risk of cardiovascular disease.
Results
The mean age of the participants was 51.47 years. The density incidence in the three groups of non-diabetic, prediabetic, and diabetic individuals was estimated to be 1.5, 1.5, and 3.9 cases per 100,000 person-days, respectively. There was no statistically significant relationship between prediabetes and the incidence of cardiovascular disease. However, the incidence of cardiovascular disease in diabetics was 2.55, 2.16, and 2 times higher than in non-diabetics in the simple, adjusted for age and sex, and in multiple Cox regression, respectively.
Conclusion
Due to the independent role of diabetes in the incidence of cardiovascular disease, diabetic individuals should be screened periodically for cardiovascular conditions. Furthermore, it is very important for these individuals to control the important risk factors that contribute to the incidence of cardiovascular disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes is one of the leading causes of morbidity and mortality worldwide [1]. According to the report by the World Health Organization (WHO), the prevalence of all types of diabetes (type one, type two, and gestational diabetes) has exponentially increased in recent decades. The number of individuals living with diabetes has risen from 108 million in 1980 to 425 million in 2017, and it is predicted that this figure will reach 629 million by 2045 [2]. There are many complications of diabetes. Retinopathy and nephropathy are among the microvascular complications of diabetes, and cardiovascular disease (CVD), which is responsible for the morbidity and mortality of many diabetics, is a macrovascular complication of diabetes [3]. In general, CVDs are one of the most serious and important complications in diabetics and prediabetic individuals (a condition in which blood sugar is between normal glycemia and diabetes) [4].
CVDs are disorders of the heart and blood circulation system, of which atherosclerosis (thickening and hardening of the walls of the arteries) is the main cause. These diseases can remain hidden for a long time and appear gradually. The most important causes of atherosclerosis are endothelial dysfunction, inflammatory factors, oxidative, and genetic factors. In general, the interactions of molecular and cellular elements, oxidative stress, and elements of the immune system are known to be effective in the pathophysiology of this disease [5, 6]. CVDs are the leading cause of death worldwide, and many people die from these diseases every year. So that 17.3 million deaths in 2008 were due to CVDs, and it is predicted that this figure will reach 23.6 million by 2030 [7]. In addition, CVDs are one of the leading causes of death in individuals living with diabetes, so the risk of death due to CVDs in diabetics is 3 times higher than in non-diabetics [8], and while diabetics are at high risk of developing these diseases [9].
Due to the clinical burden and complications of CVDs in diabetics and also the role of diabetes in increasing the incidence of CVDs, the focus of health policymakers on the management of diabetic patients has increased. For this reason, developing treatment guidelines is important for the prevention of diabetes and CVDs in diabetic individuals [10]. To be able to make the right decisions in this regard, we need to accurately estimate the incidence of CVDs among patients with diabetes and prediabetes. However, epidemiological studies are limited in this regard and there is no updated information in this field in Iran. Therefore, assessing the current situation regarding diabetes and the risk of developing CVDs will greatly help health policymakers to make more informed decisions to control these diseases. For this reason, this study was performed to investigate the role of diabetes and prediabetes on the risk of CVDs in a population of 40–70 years old in southern Iran.
Materials and methods
Study design
This prospective study was conducted on individuals aged 40–70 years who lived in Kharameh, Fars province (Iran). The Kharameh cohort study is part of a large Persian cohort study in Iran. This study aimed to investigate and identify the risk factors associated with non-communicable diseases in 18 regions of Iran. More details are provided in other articles [11,12,13].
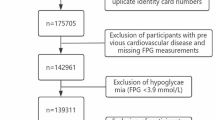
In the Kharameh cohort study, 10667 individuals aged 40–70 years participated with informed consent (participation rate 97.3%). During the study period, 4 people were lost, and finally, 10,663 people remained in the study. The inclusion criteria included individuals aged 40–70 years who lived in the Kharameh for at least 9 months. This is because during this time they were somewhat adapted to the environmental and cultural conditions that can affect their health. The exclusion criteria for the Kharameh cohort study included individuals with mental disorders, mental retardation, and other untreated diseases and those who were unwilling to participate in the study. The exclusion criteria for this study also included a history of any type of CVDs and a history of heart attack and stroke. Accordingly, 1221 individuals were excluded from the study, and finally, 9442 individuals remained in the study, they were divided into three groups: non-diabetic (n = 7291), prediabetic (n = 438), and diabetic (n = 1713) (Fig. 1).
The baseline data of the Kharameh cohort study were collected from March 2015 to March 2017, and the information about the incidence of chronic diseases in individuals has been collected during four stages of follow-up, in 2018, 2019, 2020, and 2021. Baseline data were collected by trained experts and physicians through face-to-face interviews and using previously validated Persian cohort study questionnaires. The individuals’ clinical records according to their self-declaration as well as their medical records were registered. If there was a need to verify the self-declaration of individuals, more diagnostic procedures were performed for them, and they were examined by two physician specialists.
In this study, demographic characteristics including sex, age, occupation, place of residence, marital status, socioeconomic status (SES), and education level were examined. In addition, subjects’ behavioral habits including the level of physical activity, alcohol consumption, smoking, and anthropometric characteristics including body mass index (BMI), waist, and hip circumference were evaluated. A history of diabetes, fatty liver disease, and chronic kidney disease (CKD) was also examined. In the present study, fatty liver disease was recorded based on the self-reports of people and the examination of their medical documents (laboratory tests, ultrasound, etc.) by the doctor of the Kharameh cohort team. The laboratory parameters including low-density lipoprotein (LDL), triglyceride (TG), and fasting blood sugar (FBS) were assessed.
Persian cohort questionnaires related to assets were used to assess the SES individuals. The collected data were analyzed using the principal component analysis (PCA) method, and based on the obtained value, the subjects were ranked at four levels: low, moderate, high, and very high. The level of physical activity was also assessed using questionnaires related to daily activities. To determine the level of physical activity of the participants, the collected information was converted into a metabolic equivalent of task (MET) index. Each MET is defined as 1 kcal energy consumed per kilogram (KG) of body weight at rest. Individuals based on the MET index were also divided into four categories: low, moderate level, high level, and severe.
BMI was calculated by dividing weight (KG) by height (m2), based on which the participants were divided into four categories: (underweight ≤ 18.5, normal: 18.5 to 24.9, overweight: 25 to 29.9, and obese ≥ 30). The subjects’ weight was measured using light clothing and barefoot with a German-made Seca scale, and their height was measured using a standard measuring tape. Blood samples were collected after 12 h without alcohol or cigarette consumption. All samples were measured using the MINDREY branded tool and Pars kit.
Definition of diabetes and prediabetes
Diabetes and prediabetes were defined according to the criteria of the diabetes association in 2020. All individuals with FBS equal to or greater than 6.99 mmol/L (126 mg/dL), and those who had diabetes and were taking medication were considered diabetics in this study. Individuals with FBS between 5.55 and 6.9 mmol/L (110 to 125 mg/dL) were also defined as prediabetic.
In this study, the participants were followed for 4 years, from 2018 to 2021. At each follow-up period, their CVDs status was assessed and their medical records were reviewed by physicians. If physicians confirm the development of CVDs in a person, it is recorded as a new case of CVDs. In this study, CVDs included any type of coronary heart disease, rheumatoid arthritis, cerebrovascular disease, stroke, myocardial infarction, myocardial infarction, and heart valve disease.
Statistical analysis
In the present study, the dependent variable was considered from the time individuals entered the study until the time of the event of CVDs. This interval is calculated based on the number of days. In addition, individuals were considered the right censors if they did not have a CVD event by the end of the study. All demographic variables, behavioral habits, chronic disease history, and laboratory parameters were compared in three non-diabetic, prediabetic, and diabetic groups. Quantitative variables were described by mean and standard deviation, and qualitative variables were described by number and percentage. The normality of quantitative variables was examined by the Kolmogorov-Smirnov test. The density incidence was calculated in three groups. To analyze the survival; Kaplan Meier curve for cardiovascular disease was drawn on three groups of non-diabetic, prediabetic, and diabetic, and the log-rank test was calculated to compare the survival rate between these three groups. The Cox regression model was used to estimate the effect of the prediabetes and diabetes on the incidence of CVD, in three ways. The first model investigated the effect of prediabetes and diabetes without adjusting for other variables. The second model was adjusted for age and sex variables, and the third model was adjusted for all studied variables with p-value less than 0.2 in Cox’s simple regression. The power of association was also reported with hazard ratio (HR). All analyses were performed in statistical software for data science(Stata 12) with a significant level of 0.05.
Results
Demographic, clinical, laboratory parameters, and behavioral habits
The present study was performed on 9442 individuals aged 40–70 years. The subjects were divided into three groups: non-diabetic (n = 7291), prediabetes (n = 438), and diabetic (n = 1713). The mean age of the participants was 51.47 ± 8.04 years, which was significantly higher in the diabetic group than in the two groups of prediabetic and non-diabetic (54.5 vs. 51.8 and 50.7 years). Mean TG levels were significantly higher in diabetics than in the other two groups. (150.8 vs. 145.3 and 129.9 mg/dL). The mean waist circumference was significantly higher in individuals with diabetes than in the other two groups. Women made up 65.67% of the diabetics and 57.63% of the prediabetic. In addition, 87.5% of diabetics and 64% of prediabetics were obese and overweight. Almost 30% of diabetics and 21.4 % of prediabetic had low levels of physical activity. Additional descriptive information on demographic characteristics, medical history, behavioral habits, and laboratory parameters is presented in Table 1.
Duration of follow-up and occurrence of cardiovascular disease
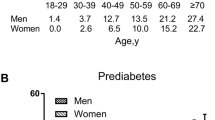
In this study, the subjects were followed for 4 years. Non-diabetic individuals were followed for 15,378,504 person-days, prediabetic individuals for 931,980 person-days, and diabetic individuals for 3,434,470 person-days. The density incidence was estimated in non-diabetic individuals with 235 cases of CVD at 1.5 per 100,000 person-days, in the prediabetic group with 14 cases of CVD at 1.5% per thousand person-days, and in the diabetic group with 137 cases at 3.98 per 100,000 person-days (Table 2) displays the incidence curve of CVD in three groups. The log-rank test showed a statistically significant difference in incidence between the three groups (chi2: 84.81 p < 0.00001) (Fig. 2).
Kaplan Meier survival curve in three groups of individuals with prediabetes, diabetes, and non-diabetes. Legend: Although the y-axis shows the probability of survival between 0 and 1, given that the probability of survival in all three study groups is above 90%, we have only shown the interval 0.9 to 1 for better clarity of the graph
Association between prediabetes and diabetes with the occurrence of cardiovascular disease
The Cox regression model was performed in three ways to investigate the relationship between prediabetes and diabetes with the incidence of CVDs, in three ways. In all three models, no statistically significant relationship was found between prediabetes and the risk of CVD (p > 0.05). However, in the first model, the risk of CVD in diabetics was found to be 2.5 times higher in non-diabetics (HRadj: 2.55 95% CI: 2.06, 3). In the second model, after adjusting for age and sex with a slight reduction, the risk of CVD in diabetics was 2.16 times higher than in non-diabetics (HRadj: 2.16 95% CI: 1.74,2.63); Finally, the third model was adjusted for the variables of age, sex, occupation, marital status, level of physical activity, education, hip circumference, smoking, alcohol consumption, chronic kidney disease, LDL, and TG. The results showed that the risk of CVD among diabetics is 2 times higher than among non-diabetics. (HRadj: 2.03 95% CI: 1.61, 2.55) (Table 3).
Discussion
The present prospective study was performed on 9442 individuals aged 40–70 years in three groups of prediabetic, diabetic, and non-diabetic to evaluate the effect of prediabetes and diabetes on the risk of CVD. After 4 years of follow-up, the density incidence in prediabetic and diabetic individuals was estimated to be 1.5 and 3.9 cases per 100,000 persons-days, respectively. The results of the present study did not show a statistically significant relationship between prediabetes and the risk of CVDs, while diabetes increased the risk of CVDs by 2.5 and 2-fold before and after adjustment of other variables. This indicates the independent role of diabetes in increasing the incidence of CVDs.
Many studies have examined the role of prediabetes in the incidence of CVDs, but their results are inconsistent. In line with the results of our study, a meta-analysis of the cohort studies showed that there was no statistically significant relationship between prediabetes and the risk of CVDs [14]. Prakash et al. also stated that prediabetes was not an independent risk factor for CVDs [15]. Unlike the results of our study, Dorte and colleagues found that the risk of CVDs was twice as high in individuals with prediabetes [16]. Another meta-analysis of 53 cohort studies showed that the risk of developing CVDs in prediabetes was 1.3 times [4]. In addition, another study reported a 1.9-fold higher risk of death due to CVDs in prediabetes [17]. Khosravi and his colleagues believed that the reason for not seeing the relationship between prediabetes and the incidence of CVDs is that prediabetes causes a mild dysfunction of the microvascular and coronary arteries of the heart; therefore, prediabetes cannot cause ischemic heart disease [18]. However, some studies have shown that prediabetes may develop into diabetes and this may be a risk factor for CVDs. It is believed that prediabetes can disrupt some of the molecular processes that disrupt the structure of blood vessels, leading to arterial inflammation and vasoconstriction, resulting in the onset of atherosclerosis [18]. It is important to understand that prediabetes is accompanied by microangiopathy and atherosclerotic vascular defect. In addition, prediabetes individuals typically have an older age, obesity, hypertension, and dyslipidemia, which all increase the risk of CVDs [19]. However, these different results can be due to various reasons, including the age of individuals under study, the use of different definitions for prediabetes, and the sample size of different studies. It is also important to keep in mind that in our study, the number of prediabetic individuals was very small, which may be the reason why we do not see the relationship. Therefore, it is necessary to investigate the relationship between prediabetes and CVD incidence more precisely in other studies.
Our study showed a statistically significant relationship between diabetes and the incidence of CVDs, and this has been confirmed by the findings of other studies [20]. Sanne et al. stated that the risk of CVDs in men and women with diabetes was 2.8 and 2.1 times higher than in non-diabetics, respectively [21]. Dorte et al. report that diabetics 54% are more likely to develop CVDs than non-diabetics [16]. Dinesh Shah and colleagues also reported a direct relationship between diabetes and the incidence of CVDs [22]. However, the majority of studies have shown a direct link between diabetes and the risk of CVDs, while CVDs are responsible for half of all cases of death in diabetics [10]. In addition, in the CVD prevention study, it has been shown that the risk of CVDs increases by 9% with each mmol increase in blood sugar [23]. Diabetes contributes to the occurrence of CVDs by causing vascular dysfunction. In general, the mechanism of the effect of diabetes in increasing the incidence of CVDs can be several factors, including endothelial dysfunction, changes in the vessel wall, hyperglycemic toxicity, oxidative stress and inflammation, and insulin resistance [24]. The pathogenesis mechanisms of CVDs in diabetes are related to genetic, epigenetic, and cell-signaling defects in inflammatory and inter-related metabolic pathways. These metabolic defects (especially in the liver, endothelium, β cells, and skeletal muscle) can be incited by various environmental factors such as smoking, high caloric intake, glucose toxicity, and glycation end-products. Some patients may express mixed or clear phenotypes of hyperglycemia, dyslipidemia, inflammation, hypertension, or thrombosis, which also represent risk factors for CVDs. Diabetes has multiple cell-signaling pathways in survival, cell growth, and proliferation such as AMP-activated protein kinase pathways and pAkt, endothelial nitric oxide synthase pathway, that could potentiate the development of CVDs. In addition to this, oxidized lipids and glucose exert important effects in tissues at the epigenetic level [25].
There are many risk factors for CVDS in diabetics. In fact, these factors are common among diabetes and CVDs. For this reason, we should note that the high prevalence of CVD risk factors (obesity, hypertension, dyslipidemia, etc.) in diabetic people can contribute to the occurrence of CVDs in these people. For example, obesity is known as one of the risk factors for CVDs in diabetic [26]. About 68% of diabetics and 64% of prediabetic in our study were obese and overweight. These factors are one of the most important risk factors for CVDs. In our study, 36.2% of individuals with diabetes and 19.5% of the prediabetics had hypertension. In general, hypertension is a common comorbidity with diabetes that increases the risk of CVDs. Naqipour and her colleagues in their study in the north of Iran stated that control of hypertension in adults reduced the risk of CVDs by 26% [27]. Dyslipidemia disorders are very common in individuals with diabetes and these disorders are an important risk factor for CVDs [26]. The UK prospective diabetes study (UKPDS 23) showed that increased concentrations of low-density lipoprotein cholesterol, decreased concentrations of high-density lipoprotein cholesterol, and systolic blood pressure are the main risk factors for the development of CVDs in diabetic patients [28]. A meta-analysis study showed that treatment with statins to reduce dyslipidemias in 18,000 diabetics resulted in a 13% reduction in the mortality of CVDs [29]. In addition, we must note that the presence of physical and psychological problems can, along with diabetes, worsen the prognosis of cardiovascular events in an individual patient. Ruth and Andrew stated that psychological and social factors in diabetic people potentially affect the risk of CVDs through processes such as reduced physical activity and lifestyle change [30]. Thus, given the presence of many risk factors that lead to CVDs, in individuals with diabetes, it is essential to develop strategies to prevent CVDs in diabetic patients including lifestyle interventions, medication interventions, treatment of hypertension, and anti-diabetic treatment [24]. Lifestyle intervention is also an essential management approach to control these patients so that these interventions can reduce the risk of developing diabetes. Changes in daily activities can also significantly reduce the risk of CVD [4]. In addition, given the importance of this issue, the screening of diabetics for CVD is an important strategy for the reduction of mortality and the incidence of CVDs.
Limitations
This study is a prospective study with a large sample size that was performed under completely standard conditions and examined numerous risk factors. However, the follow-up period of our study was relatively short and the number of individuals with prediabetes was low, which can affect the results of the study. Another one of the limitations of the present study was the lack of access to the status of COVID-19 in the subjects under study. Therefore, we could not investigate the effect of COVID-19 on the development of CVDs in diabetic and prediabetic patients. Also, another limitation of our study was the lack of access to information on the duration of diabetes, which can affect the risk of CVDs.
Conclusion
The results of this study demonstrate that diabetes is an independent risk factor for increasing the risk of CVDs. The high prevalence and rapid growth of diabetes and its complications will lead to an increase in the incidence of CDVs. Therefore, it is necessary to carry out effective interventions for the timely identification of people with diabetes and also to control diabetes in them. In addition, due to the high prevalence of CVD risk factors in diabetics, lifestyle change education to reduce modifiable risk factors in them can help reduce the incidence of CVDs.
Data availability
Not applicable.
References
Brannick B, Dagogo-Jack S. Prediabetes and cardiovascular disease: pathophysiology and interventions for prevention and risk reduction. Endocrinol Metab Clin. 2018;47(1):33–50.
Mohamed SF, Mwangi M, Mutua MK, Kibachio J, Hussein A, Ndegwa Z, Owondo S, Asiki G, Kyobutungi C. Prevalence and factors associated with pre-diabetes and diabetes mellitus in Kenya: results from a national survey. BMC Public Health. 2018;18(3):1–11.
Deedwania PC, Fonseca VA. Diabetes, prediabetes, and cardiovascular risk: shifting the paradigm. Am J Med. 2005;118(9):939–47.
Huang Y, Cai X, Mai W, Li M, Hu Y. Association between prediabetes and risk of cardiovascular disease and all cause mortality: systematic review and meta-analysis. BMJ. 2016:355.
Frąk W, Wojtasińska A, Lisińska W, Młynarska E, Franczyk B, Rysz J. Pathophysiology of cardiovascular diseases: new insights into molecular mechanisms of atherosclerosis, arterial hypertension, and coronary artery disease. Biomedicines. 2022;10(8):1938.
Scott J. Pathophysiology and biochemistry of cardiovascular disease. Curr Opinion Genet Developm. 2004;14(3):271–9.
Balakumar P, Maung-U K, Jagadeesh G. Prevalence and prevention of cardiovascular disease and diabetes mellitus. Pharmacol Res. 2016;113:600–9.
Niroumand S, Dadgarmoghaddam M, Eghbali B, Abrishami M, Gholoobi A, Taghanaki HRB, Khajedaluee M. Cardiovascular disease risk factors profile in individuals with diabetes compared with non-diabetic subjects in north-east of Iran. Iran Red Crescent Med J. 2016;18(8).
Glovaci D, Fan W, Wong ND. Epidemiology of diabetes mellitus and cardiovascular disease. Curr Cardiol Rep. 2019;21(4):1–8.
Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018;17(1):1–19.
Poustchi H, Eghtesad S, Kamangar F, Etemadi A, Keshtkar A-A, Hekmatdoost A, Mohammadi Z, Mahmoudi Z, Shayanrad A, Roozafzai F. Prospective epidemiological research studies in Iran (the PERSIAN Cohort Study): rationale, objectives, and design. Am J Epidemiol. 2018;187(4):647–55.
Moftakhar L, Jafari F, Ghoddusi Johari M, Rezaeianzadeh R, Hosseini SV, Rezaianzadeh A. Prevalence and risk factors of kidney stone disease in population aged 40–70 years old in Kharameh cohort study: a cross-sectional population-based study in southern Iran. BMC Urol. 2022;22(1):1–9.
Moftakhar L, Rezaeianzadeh R, Ghoddusi Johari M, Hosseini SV, Rezaianzadeh A. Epidemiology and predictors of multimorbidity in Kharameh cohort study: a population-based cross-sectional study in southern Iran. Health Sci Reports. 2023;6(1):e988.
Qiu M, Shen W, Song X, Ju L, Tong W, Wang H, Zheng S, Jin Y, Wu Y, Wang W. Effects of prediabetes mellitus alone or plus hypertension on subsequent occurrence of cardiovascular disease and diabetes mellitus: longitudinal study. Hypertens. 2015;65(3):525–30.
Deedwania P, Patel K, Fonarow GC, Desai RV, Zhang Y, Feller MA, Ovalle F, Love TE, Aban IB, Mujib M. Prediabetes is not an independent risk factor for incident heart failure, other cardiovascular events or mortality in older adults: findings from a population-based cohort study. Int J Cardiol. 2013;168(4):3616–22.
Vistisen D, Witte DR, Brunner EJ, Kivimäki M, Tabák A, Jørgensen ME, Færch K. Risk of cardiovascular disease and death in individuals with prediabetes defined by different criteria: the Whitehall II study. Diabetes Care. 2018;41(4):899–906.
Huang Y, Cai X, Chen P, Mai W, Tang H, Huang Y, Hu Y. Associations of prediabetes with all-cause and cardiovascular mortality: a meta-analysis. Ann Med. 2014;46(8):684–92.
Khosravi A, Gharipour M, Nezafati P, Khosravi Z, Sadeghi M, Khaledifar A, Taheri M, Golshahi J, Sarrafzadegan N. Pre-hypertension, pre-diabetes or both: which is best at predicting cardiovascular events in the long term? J Hum Hypertens. 2017;31(6):382–7.
Buysschaert M, Medina JL, Bergman M, Shah A, Lonier J. Prediabetes and associated disorders. Endocrine. 2015;48:371–93.
Larsson SC, Wallin A, Håkansson N, Stackelberg O, Bäck M, Wolk A. Type 1 and type 2 diabetes mellitus and incidence of seven cardiovascular diseases. Int J Cardiol. 2018;262:66–70.
Peters SA, Huxley RR, Woodward M. Diabetes as risk factor for incident coronary heart disease in women compared with men: a systematic review and meta-analysis of 64 cohorts including 858,507 individuals and 28,203 coronary events. Diabetologia. 2014;57(8):1542–51.
Shah AD, Langenberg C, Rapsomaniki E, Denaxas S, Pujades-Rodriguez M, Gale CP, Deanfield J, Smeeth L, Timmis A, Hemingway H. Type 2 diabetes and incidence of cardiovascular diseases: a cohort study in 1· 9 million people. Lancet Diabetes Endocrinol. 2015;3(2):105–13.
Huang D, Refaat M, Mohammedi K, Jayyousi A, Al Suwaidi J, Abi Khalil C. Macrovascular complications in patients with diabetes and prediabetes. Biomed Res Int. 2017;2017.
Wang Y, Yu Q, Fan D, Cao F. Coronary heart disease in type 2 diabetes: mechanisms and comprehensive prevention strategies. Expert Rev Cardiovasc Ther. 2012;10(8):1051–60.
Rodriguez-Araujo G, Nakagami H. Pathophysiology of cardiovascular disease in diabetes mellitus. Cardiovas Endocrin Metab. 2018;7(1):4.
Henning RJ. Type-2 diabetes mellitus and cardiovascular disease. Future Cardiol. 2018;14(6):491–509.
Naghipour M, Joukar F, Salari A, Asgharnezhad M, Hassanipour S, Mansour-Ghanaei F. Epidemiologic profile of hypertension in northern Iranian population: the PERSIAN Guilan Cohort Study (PGCS). Ann Glob. Health. 2021;87(1).
Turner R, Millns H, Neil H, Stratton I, Manley S, Matthews D, Holman R. Risk factors for coronary artery disease in non-insulin dependent diabetes mellitus: United Kingdom prospective diabetes study (UKPDS: 23). BMJ. 1998;316(7134):823–8.
Kearney P, Blackwell L, Collins R, Keech A, Simes J, Peto R, Armitage J, Baigent C. Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomized trials of statins: a meta-analysis. Lancet (London, England). 2008;371(9607):117–25.
Hackett RA, Steptoe A. Psychosocial factors in diabetes and cardiovascular risk. Curr Cardiol Reports. 2016;18:1–12.
Acknowledgments
The authors are grateful to the officers and data management staff of the Kharameh cohort.
Funding
None.
Author information
Authors and Affiliations
Contributions
R.A was responsible for the fieldwork including data collection and management. M.L did the analysis and wrote the method and parts of the manuscript. H.SV collected data. S.M checked all analyses, graphs, and tables and managed how to analyze them. Gh.M and H.SV also wrote the part of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This research is extracted from a Ph.D. dissertation under the supervision of Dr. Abbas Rezaianzadeh. It has also been approved by the ethics committee of Shiraz University of Medical Sciences. (IR.SUMS.SCHEANUT.REC.1400.046)
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Moftakhar, L., Rezaianzadeh, A., Seif, M. et al. The effect of prediabetes and diabetes on the incidence of cardiovascular disease in the population of 40 to 70 years in the south of Iran: a population-based cohort study. Int J Diabetes Dev Ctries 44, 554–561 (2024). https://doi.org/10.1007/s13410-023-01273-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-023-01273-6