Abstract
Diabetic foot ulcer (DFU) is the commonest condition for hospital admission and usually the starting point of most diabetic related lower limb amputations. Considering the significant role played by vascularity in the outcome of ulcer healing, we undertook this study to find out the comparative utility of commonly used vascular assessment methods. This study was a single center prospective non-randomized observational study, conducted for a period of 6 months, in diabetic patients presenting with foot ulcers of Wagner Grade II and III. The aim of our study was to compare the performances of ankle-brachial index (ABI) and transcutaneous partial pressure of oxygen (tcPO2) measurement in predicting wound healing in diabetic ulcers and to define the optimal cut-off value for Indian patients. Five hundred sixty-four patients were included in this study, with the mean age of 58 years. Eighty-seven patients (15%) had peripheral arterial occlusive disease. Four hundred seventy ulcers (83%) healed with the mean healing days of 42.6 days. Age, duration of diabetes, serum creatinine level, and presence of infection were the factors with negative impact in wound healing. In our study, ABI value of 0.6 was found to have 100% sensitivity and 70% specificity, and tcPO2 value of 22.5 was found to have 75% sensitivity and 100% specificity in predicting wound healing. Both ABI and tcPO2 are complementary, but tcPO2 is a better predictor for amputation while ABI is a better predictor for ulcer healing. While assessing the ischemic status of foot ulcer, the cut-off values should be higher in diabetics than non-diabetics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic foot ulcers (DFU) affect 15% of diabetic patients during their life time [1], and it is one of the commonest cause for hospital admissions. Unless an early holistic approach of the patient is not taken, this devastating complication ends up in loss of limb and possibly life. A total of 85% of diabetes-related amputations are due to DFU, causing a leg amputation in every 30 s somewhere in the world [2]. With a general rise in elderly population and wider availability of better medical facilities, in India, more and more patients are being diagnosed with diabetes mellitus (DM), and we see more complications related to diabetes in a major way. DFU itself is worrisome, causing not only morbidity, but also lots of financial burden to the patient. Long-term morbidity can be avoided by determining the contributory factors for ulcer healing. Predicting the wound healing in a diabetic patient is difficult, considering the complex and contributory role of various factors in play, but not impossible. One of the important and established factors, determining the outcome of any ulcer in the extremities, is peripheral arterial occlusive disease (PAOD). Assessment of vascularity plays a significant role in the management of DFU.
The primary goal of any physician treating DFU is to obtain epithelial cover as early as possible. Predicting the ulcer healing is an essential step in the management of DFU, especially when there are variety of factors like age, sex, body mass index, smoking, associated infection, elevated blood sugar, elevated serum creatinine, and local blood supply, affecting the healing [3]. To evaluate the degree of role of PAOD in the outcome of DFU, a range of various non-invasive techniques have been proposed—ankle-brachial index (ABI), transcutaneous tissue oxygen tension (tcPO2), and toe pressure and toe-brachial index. ABI is the conventional test, but not useful in calcified pedal vessels, which is a very common finding in diabetic patients, showing normal or high values [4,5,6]. TcPO2 measures subclinical micro-vascular involvement, which shows the local tissue oxygen supply available for wound healing, rather than blood supply, but this method is not useful in major vessel involvement [7,8,9,10].
There is a physician’s dilemma in the management of DFU, in assessing the course of disease and to predict the outcome, so as to take a well-informed decision. When there is a clear cut lesion causing critical ischemia, the role of revascularization is clear to the treating physician to define the course of management. His dilemma starts when he finds diffuse arterial disease, associated with neuropathy and/or severe infection, which is a very common presenting picture in DFU. Whether the patient will, or not, benefit with revascularization, cannot be decided purely on the basis of ABI alone. The role of tcPO2 in such difficult cases is to be defined, to help the physician to take an informed decision. To assess the extent of PAOD, thereby assessing and predicting the wound outcome, the utility of ABI and tcPO2 measurement should be validated. Unclear about which one will accurately predict the wound outcome, this study was done to find out the comparative utility of ABI and tcPO2 in predicting wound outcomes in DFU and to define the cut-off values for both measurement in Indian diabetic patients.
Methodology
This was a single-center prospective non-randomized observational study, conducted for a period of 6 months from September 2015 to February 2016, at MV Diabetic Research Center, Chennai. All diabetic patients who attended the outpatient department with Wagner Grade II and III foot ulcers were included in this study. On admission, basic demographic, medical details and clinical features of all patients were recorded. On evaluation, biochemistry investigation reports, microbiology lab results, ABI, and tcPO2 were recorded for all patients. Comprehensive wound care was offered by a multidisciplinary team as per institute protocol, which includes strict control of hyperglycemia and co-morbid factors, wound debridement by mechanical, chemical, and surgical methods, offloading, and management of complications. All patients were followed up to complete wound healing or up to 3 months. Complete epithelialization of the ulcer or healed amputation stump was considered as primary wound outcome.
The outcome was categorized as healed and amputation. Amputations were defined as minor which includes mid-foot and distal amputations, while major amputation was defined as amputations above the ankle. Patients, who had clear treatable lesions, underwent revascularization procedures and who had non-healing ulcers at the end of the study period, due to lost to follow-up or extensive infection were excluded from the study. All data were entered in a Microsoft excel sheet and statistical analysis was done using SPSS. Binary demographic factors, baseline risk factors, and outcome variables were compared between the outcome groups using the χ 2 test, the Fisher exact test, and the odds ratio with 95% confidence interval, wherever appropriate. Continuous demographic factors and outcome variables were summarized using a mean with 95% standard deviation and compared between outcome groups by using t test. The performances and optimal cut-off values for the studies factors were calculated and presented using an ROC curve.
Results
A total of 582 patients attended the hospital with DFU of grade II and III, during the study period. Out of that, 5 patients who underwent revascularization procedures and 13 patients with a non-healing ulcer at the end of the study period were excluded. The remaining 564 patients were included in this study, including 380 males and 184 females [Table 1]. The mean age of the study group was 58.23 ± 10.11 years. The age distribution in both groups is shown in Fig. 1. Neither sex of the patient (p = 0.039) nor body mass index (BMI) (p = 0.07) had any effect in the wound outcome. Various studies have proven the effect of BMI in the occurrence of diabetic complications. In our study as the mean BMI was 23, it may not have any effect in the wound healing. The mean BMI for the healed group was 26.8 ± 4.8, while that of the amputation group was 25.7 ± 4.3. Only 7 patients in our study group were current smokers, which is an insignificant number to come to any conclusion (p = 0.865).
Duration of DM in our study group showed a wide variation, ranging from recently diagnosed within 1 month to disease of 43 years duration, with an average of 23 years. There were 54 patients (9.8%) who had the disease for more than 20 years and 218 patients with the duration of 10–20 years. The mean duration of the disease in the amputation group was 14.22 ± 7.1 years and that of the healed group was 11.96 ± 7.3 years. Duration of DM has got a significant negative role in wound healing as well as higher degree of amputation (p = 0.007). HbA1c levels were measured on admission and reassessed periodically to treat and bring it under control. On admission, 495 patients (88%) had their HbA1c level more than 7, indicating poor control (mean HbA1c on admission = 9.28). But on statistical analysis, p value was 0.058, excluding its role in wound outcome. These may be due to the in-house control of blood sugar level with insulin, oral anti diabetic drugs, and proper diet, which controls the hyperglycemia and prevents its adverse effects. All patients with uncontrolled hyperglycemia were given priority treatment with a strict regime on diet and drugs. And, in the end of study period, all of them had their blood sugar under control and their HbA1c level less than 7. This strict control may be the reason in their negative role in the poor DFU outcome.
With so many patients in our study group having DM for prolonged duration (> 10 years in 272 patients), incidence of chronic kidney disease and elevated serum creatinine is not an unexpected finding. In our study group, 154 patients (27.3%) had elevated serum creatinine levels > 1.2 g/dl. With the outcome of amputation, the p value was 0.002, establishing level of serum creatinine as a significant factor in the wound outcome. Infection in the patients was diagnosed by clinical signs of cellulitis, abscess, local lymphangitis, presence of associated systemic signs, such as fever, hyperleucocytosis, and bacteriological samples were taken, in cases of clinically established infection. A total of 309 patients were admitted with local infection in the DFU, of whom 62/309 (20%) patients had amputation, while 87.5% (223/255) of patients without infection had their ulcer healed. p value = 0.017 was significant, but not on a greater scale.
Out of 470 healed ulcers, 65% (304 patients) healed within 41 to 45 days. Only 81/470 patients (17%) had delayed healing of > 45 days. The average healing days were 42.6 ± 2.7 days. A total of 94 patients underwent amputation, 32 patients with minor and 62 patients with major amputation. The most difficult situation in the management of DFU is to take decision at the appropriate time and appropriate level of amputation. The decision for minor amputation is comparatively easier, considering the less morbidity and tissue loss associated. The decision for major amputation is taken considering the grade of DFU (higher the grade more proximal the level), associated infection (whether controlled or severe uncontrollable infection to regular antibiotics), and the general functional capacity of the patient. Out of 62 patients who underwent major amputation, 46 DFU were graded up to Wegener grade IV/V, in spite of adequate antibiotic control and 16 patients had severe ischemic foot, with non-reconstructable vessels. Most major amputations are considered as a life-saving procedure rather than trying for limb salvage.
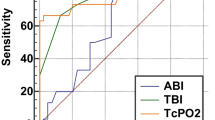
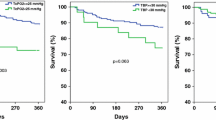
The prevalence of PAOD is 18% (87 patients) in our study. Out of 470 patients with healed ulcers, 422 (90%) had recorded ABI > 0.9 and 395 (84%) patients recorded tcPO2 > 40. In the category of amputation, the values were 55/94 (59%) patients and 53/94 (56%) patients, respectively. A total of 39/94 patients (42%) in the amputation category and 48/470 patients (10%) in the healed category showed abnormal ABI measurement of < 0.9. In the measurement of tcPO2, 41/94 patients (44%) in the amputation group and 75/470 patients (16%) in the healed group showed low values of < 40. The diagnostic ODDS ratio for wound healing for ABI was 23 and for tcPO2 was 4.23, with a positive predictive value of 75 and 35%, respectively [Table 2]. By plotting the ROC curve, for the state of healed, a tcPO2 value of 22.5 must have 100% sensitivity and 75% specificity. The corresponding value for ABI was 0.6, with sensitivity of 99% and specificity of 68%. By decreasing the value of ABI to 0.4, it had the sensitivity of 100% and specificity of 80% [Fig. 2a]. By plotting the ROC curve, for the positive state of amputation, an ABI value of < 0.6 was found to have 68% sensitivity and 99% specificity. The corresponding value for tcPO2 was 22.5, with sensitivity of 75% and specificity of 100% [Fig. 2b]. Multivariate logistic regression analysis showed an ODD ratio of 3.5 (95% CI 2.2–5.7) for the effect of wound healing with ABI and an ODDS ratio of 3.0 (95% CI 2.1–4.3) for the effect of abnormal tcPO2 in amputation [Table 3].
Discussion
In 2014, the prevalence of DM in India had increased to 9.1% and is expected to continue rising [11]. With the rise in diabetic patients, complications related to DM are also in rise. In this study, we undertook to analyze the utility of ABI and tcPO2 in predicting wound outcomes in DFU, one of the commonest morbidity in DM. Over a period of 6 months, 564 patients with DFU are evaluated. Our average wound healing days of 42.6 ± 2.7 is much less than those reported in other studies. Average ulcer duration of 133 days had been reported in the literature [12]. The better result of our study might be due to the strict wound care protocol, followed at the institute, comprising a multidisciplinary team, involving physician, surgeon including plastic and vascular surgeon, podiatrist, special wound care nursing team, and specific consultancy for diet and life-style modification, including smoking cessation. A recent study by Wang et al. showed an average age of patients with DFU as 66.96 years [13]. Our study showed a relatively younger population of mean age of 58 years, which is similar to other Indian statistics. Age, as a contributory factor, is proven to be statistically significant in our study and another interesting factor revealed is that the age of amputation (mean = 63.7 years) is one decade later than the healed group (mean = 51.6 years). Older patients are more prone for amputation than younger patients. In a study by Marston [14], it was found to have female gender as a positive effect in healing, but our study did not find any significant difference based on sex of the patient (p = 0.039), even though females formed one third of the study group (33%). Another noted factor, which was proven negative in our study, is smoking [15]. This may be due to very small number of patients (N = 7), who were active smokers in our study. As suggested by previous studies [13], a significant correlation to the duration of disease is noted. In our study, the range was so wide, from a recently diagnosed patient with less than a month to a 71-year-old patient with 43 years of disease. Another proven factor is that of serum creatinine level, which had a negative impact on healing [16, 17]. Several risk factors proven to affect healing were not found to be significant in this study. BMI is a known factor, proven by several studies [18]. The non-significance of BMI in our study may be due to lower near normal values (mean of 25). Improved glucose control is a proven factor that promotes wound healing [15]. This may be the reason why there is no significant role in wound healing for abnormal HbA1c (p = 0.058) in our study, because strict glycemic control is one of the basic management in our protocol and we have only taken the glycemic level at admission, which may not affect the course of the disease. This proves the effective role of strict glycemic control in preventing poor wound outcome and possibly, amputation. A recent report by Lee et al. also stated higher HbA1c levels in the successful wound treatment group [16].
Previous studies have suggested a negative role of infection in wound healing [19, 20]. Our study established a weak role for infection (p = 0.017). This may be due to the present availability of higher antibiotics, appropriate use of antibiotics after determining extent and severity of the infection, and thorough surgical debridement to remove the infected tissue and earliest epithelial cover, as per our protocol. The prevalence of PAOD among diabetics has been found to be low in Indian population, but is on the rise, and may be due to better diagnostic facilities, increasing duration of diabetes, and increasing older population. Previous Indian studies published in the later years of the twentieth century reported 3–6% [21, 22] prevalence, while recent studies from India, reported 12.6–31.6 and 19.7% [23,24,25]. In the west, the prevalence is said to be high, ranging 25–45% [26,27,28]. To assess the ischemic nature of the wound, if ABI is used, we have 87 patients (15%), but if tcPO2 is used, we have an increase by 29 patients, i.e., 116 patients (21%). As tcPO2 measures the microangiopathic involvement by DM, it scores as a better marker to diagnose the vascularity of a distal wound. By assessment of diagnostic odds ratio, ABI with a score of 23, proves itself as a better indicator for predicting wound healing. Even though the negative predictive value of both parameters is the same, the positive predictive value of ABI is much higher than tcPO2, signifying its position as a better indicator for wound healing. Even the results of multivariate regression analysis confirm the significance of ABI with an odds ratio of 3.5 for wound healing. But, for the predicament of amputation as outcome, tcPO2 scores better than ABI with an odds ratio of 3.
Though ABI value of < 0.9 is commonly used to predict the PAOD, and value of < 0.3 is used for indication of critical ischemia, in our study, ABI of 0.6 is found to have optimum sensitivity and specificity in predicting wound outcome. An ABI of < 0.6 predicted poor outcome in 32% of DFU, with a sensitivity of 99%. It may be suggested that in diabetic patients, the consideration of critical wound ischemia should be at a lower level than that of non-diabetics, and in patients with DFU and an ABI < 0.6, immediate and adequate treatment measures should be taken to improve vascularity and to save the limb. Same way, the optimal cut-off value for tcPO2 to be considered might be 22.5 mm of Hg, rather than the universally accepted value of 40. A tcPO2 value of < 42.50 predicts 56% of amputation, while it was 70 and 92%, respectively at tcPO2 values of < 22.50 and < 12.50. With the consideration of amputation, thus, tcPO2 values of 22.5 may be considered with more sensitivity and specificity. These results are similar to the results by Lalithambika et al. [29], which has near about the same values of ABI of 0.77 and tcPO2 value of 22.5 mm of Hg, in their study in Indian population. Thus, in patients with DFU and tcPO2 value < 20 mm of Hg, the patient may be alerted to the high probability of amputation.
Conclusion
Indian patients were younger, with a long history of disease duration, moderate BMI, and with high HbA1c. A dedicated multidisciplinary team approach, with strict control of hyperglycemia, infection, and life-style modification such as avoidance of smoking, will result in better wound healing and reduce drastically the average healing days. Due to biological variability of individuals, no parameter can be 100% effective under all conditions. Nevertheless, it has been demonstrated that, within the two parameters assessed, ABI is a better predictor for wound healing and tcPO2 is for predicting amputation. A value of 0.6 for ABI and 22.5 for tcPO2 may be considered for Indian diabetic patients while assessing DFU outcome. However, in the absence of a prospective randomized study with more patients, opinions will continue to be divided.
References
Viswanathan V, Thomas N, Tandon N, Asirvatham A, Rajasekar S, Ramachandran A, et al. Profile of diabetic foot complications and its associated complications—a multicentric study from India. J Assoc Phys India. 2005;53:933–6.
Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA. 2005;293:217–28.
Loslin EP. The menace of diabetic gangrene. N Engl J Med. 1934;211:16–20.
Potier L, Abi Khalil C, Mohammedi K, Roussel R. Use and utility of ankle brachial index in patients with diabetes. Eur J Vasc Endovasc Surg. 2011;41:110–6.
Chang CH, Peng YS, Chang CC, Chen MY. Useful screening tools for preventing foot problems of diabetics in rural areas: a cross-sectional study. BMC Public Health. 2013;13:612.
Aerden D, Massaad D, von Kemp K, van Tussenbroek F, Debing E, Keymeulen B, et al. The ankle-brachial index and the diabetic foot: a troublesome marriage. Ann Vasc Surg. 2011;25:770–7.
de Meijer VE, Van’t Sant HP, Spronk S, Kusters FJ, den Hoed PT. Reference value of transcutaneous oxygen measurement in diabetic patients compared with nondiabetic patients. J Vasc Surg. 2008;48:382–8.
Barnikol WK, Pötzschke H. A novel, non-invasive diagnostic clinical procedure for the determination of an oxygenation status of chronic lower leg ulcers using peri-ulceral transcutaneous oxygen partial pressure measurements: results of its application in chronic venous insufficiency (CVI). Ger Med Sci. 2012;10:Doc11.
Hutchison DC, Rocca G, Honeybourne D. Estimation of arterial oxygen tension in adult subjects using a transcutaneous electrode. Thorax. 1981;36:473–7.
Lalka SG, Malone JM, Anderson GG, Hagaman RM, McIntyre KE, Bernhard VM. Transcutaneous oxygen and carbon dioxide pressure monitoring to determine severity of limb ischemia and to predict surgical outcome. J Vasc Surg. 1988;7:507–14.
Arora NK, Pillai R, Dasgupta R, Garg PR. Whole-of-society monitoring framework for sugar, salt, and fat consumption and noncommunicable diseases in India. Ann N Y Acad Sci. 2014;1331:157–73.
Zimny S, Schatz H, Pfohl M. Determinants and estimation of healing times in diabetic foot ulcers. J Diabetes Complicat. 2002;16:327–32.
Wang C, Mai L, Yang C, Liu D, Sun K, Song W, et al. Reducing major lower extremity amputations after the introduction of a multidisciplinary team in patient with diabetes foot ulcer. BMC Endocr Disord. 2016;16:38.
Marston WA. Risk factors associated with healing chronic diabetic foot ulcers: the importance of hyperglycemia. Ostomy Wound Manage. 2006;52:26–8.
Markuson M, Hanson D, Anderson J, Langemo D, Hunter S, Thompson P, et al. The relationship between hemoglobin A(1c) values and healing time for lower extremity ulcers in individuals with diabetes. Adv Skin Wound Care. 2009;22:365–72.
Lee KM, Kim WH, Choi MSS. Risk factors of treatment failure in diabetic foot ulcer patients. Arch Plast Surg. 2013;40:123–8.
Akini B, Yesil S, Eraslan S. The effect of creatinine clearance on the short-term outcome of neuropathic diabetic foot ulcers. J Prim Care Diabetes. 2010;4:181–5.
Sohn MW, Budiman-Mak E, Lee TA, Oh E, Stuck RM. Significant J-shaped association between body mass index and diabetic foot ulcers. Diabetes Metab Res Rev. 2011;27:402–9.
Margolis DJ, Allen Taylor L, Hoffstad O, Berlin JA. Diabetic neuropathic foot ulcers: predicting which ones will not heal. Am J Med. 2003;115:627–31.
Margolis DJ, Kantor J, Santanna J, Strom BL, Berlin JA. Risk factors for delayed healing of neuropathic diabetic foot ulcers: a pooled analysis. Arch Dermatol. 2000;136:1531–5.
Mohan V, Premlatha G, Shastry NG. Peripheral vascular disease in non-insulin-dependent diabetes mellitus in south India. Diab Res Clin Pract. 1995;27:235–40.
Pendsey SP. Peripheral vascular disease: an Indian scenario. Diabtol Croat. 1998;27:153–6.
Jayaprakash P, Bhansali A, Dutta P, Ananthraman R. Magnitude of foot problems in diabetes in the developing world: a study of 1044 patients. Diab Med. 2009;26:939–42.
Parvez N, Dutta P, Ray P, Shah VN, Prakash M, Khandelwal M, et al. Microbial profile and utility of soft tissue, pus and bone cultures in diagnosing diabetic foot infections. Diabetes Technol Ther. 2012;14:669–74.
Sinahary K, Paul UK, Bhattacharyya AK, Pal SK. Prevalence of diabetic foot ulcers in newly diagnosed diabetes mellitus patients. J Indian Med Assoc. 2012;110:608–11.
Walters DP, Gatling W, Mullee MA, Hill RD. The prevalence, detection and epidemiological correlates of peripheral vascular disease: a comparison of diabetic and non-diabetic subjects in an English community. Diabet Med. 1992;9:710–5.
Al-Rubeaan K, Al Derwish M, Quizi S, Youssef AM, Subhani SM, Ibrahim HM, et al. Diabetic foot complications and their risk factors from a large retrospective cohort study. PLoS One. 2015;10:e0124446.
Bowling FL, Rashid TS, Boulton JM. Preventing and treating foot complications associated with diabetes mellitus. Nat Rev Endocrinol. 2015;11:606–16.
Lalithambika CV, Nisha B, Saraswathy L, Varma AK, Jose A, Sundaram KR. Ankle brachial index and transcutaneous partial pressure of oxygen as predictors of wound healing in diabetic foot ulcers. J Diabet Foot Complications. 2014;6:54–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Rajagopalan, C., Viswanathan, V., Rajsekar, S. et al. Diabetic foot ulcers—comparison of performance of ankle-brachial index and transcutaneous partial oxygen pressure in predicting outcome. Int J Diabetes Dev Ctries 38, 179–184 (2018). https://doi.org/10.1007/s13410-017-0580-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-017-0580-3