Abstract
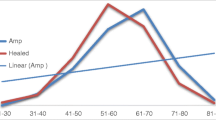
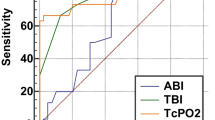
Foot ulcer is a common complication of diabetes mellitus. The co-existence of peripheral arterial disease (PAD) increases the risk of non-healing of the ulcer. Ankle brachial index (ABI) and transcutaneous partial pressure of oxygen (TcPO2) are two tests used to assess the vascularity of the foot, using two different parameters. This study was done to compare the sensitivity, specificity and diagnostic accuracy of ABI and TcPO2 and to find out which of these is a better predictor of healing in diabetic foot ulcers in patients without palpable foot pulses. The hospital-based longitudinal study was done from March 2016 to March 2018 among 121 adult patients diagnosed with diabetic foot ulcer without palpable peripheral pulses who fit the inclusion and exclusion criteria. Vascularity of the foot in these patients was assessed using ABI and TcPO2. The participants were followed up for 3 months, and the healing status was recorded. The mean (SD) age of patients was 64.99 (10.03) years. Out of 121 patients, 89 were men and 32 were women. The mean ABI in healed and non-healed group were significantly different (P value < 0.001). TcPO2 also showed significant difference in healed and non-healed groups (P value < 0.001). The values of 0.65 in receiver operating characteristic (ROC) curve showed optimal sensitivity (86.1%) and specificity (75.5%) for ABI. ROC curve with a TcPO2 cut-off value of 27.5 mmHg had optimal sensitivity (84.7%) and specificity (81.6%). Although sensitivity of TcPO2 and ABI is comparable (84.7% v 86.1%), specificity and diagnostic accuracy are better for TcPO2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus (DM) is the commonest metabolic disorder affecting about 20% of the population in various parts of the world [1]. Prevalence of DM is increasing worldwide. In 2011, 366 million adults had DM worldwide, and by 2030, it is proposed to be 552 million [2, 3]. This exponential increase in DM causes an increase in diabetes-related complications like coronary artery disease (CAD), chronic kidney disease (CKD), cardiovascular accidents (CVA), diabetic foot and peripheral arterial disease (PAD). The incidence of DM is increasing worldwide because of increased life expectancy and changing dietary habits [4]. Diabetic foot ulcer is a devastating long-term complication of DM [5]. It has been estimated that 15% of all people with diabetes will develop foot ulcer at some stage of their life and the annual incidence rate is 2% [6, 7]. Diabetic foot ulcers have significant health and socioeconomic implications, affecting the quality of life of the patient and imposing a heavy economic burden on the patient’s family [8].
Diabetic foot ulcers and PAD often coexist. The term PAD indicates narrowing or occlusion of the arteries other than those that supply the heart or the brain. It most commonly affects the legs, but other arteries may also be involved. Peripheral artery disease (PAD) is present in about 50% of patients with diabetic foot ulcer [9]. It affects the outcome of the ulcer, in that it prolongs the healing or may lead to amputation and a poor quality of life [10,11,12]. Ulcers secondary to arterial insufficiency are the second most common lower extremity ulcers [13, 14]. About 85% of non-traumatic major amputations are associated with diabetic foot ulcers [15].
Assessment of the vascularity is a key step for the management of diabetic foot ulcer as PAD is an independent risk factor for the development and non-healing of diabetic foot ulcer. It is often missed, leading to increased morbidity to the patient. There are several methods to assess the vascularity of foot. Absence of pulse is the most important sign of PAD which can be easily assessed [16, 17]. Methods to assess severity of PAD include ankle brachial index (ABI), toe pressure assessment, transcutaneous partial pressure of oxygen (TcPO2) and angiography. ABI is a simple method to assess vascularity of foot. It is the ratio of the systolic pressure at the ankle to that at the arm in a person at rest. TcPO2 is a relatively newer technique which quantifies cutaneous tissue oxygenation.
Understanding how well these methods predict ulcer healing can influence management modalities and help plan treatment. Studies comparing the accuracy of these tests in such prediction are scarce in literature. Hence, this study was done with the objective of comparing ABI and TcPO2 with regard to sensitivity, specificity and diagnostic accuracy in predicting diabetic foot ulcer healing.
Methodology
It was a longitudinal observational study conducted in a tertiary care centre in Kerala, South India. The study population was all adult patients (above 18 years of age) admitted in the surgical wards with diabetic foot ulcer. The inclusion criteria were that the ulcer should be below the level of the ankle joint and belong to Wagner’s grades 1–4 and the patient should not have palpable pulsations in both dorsalis pedis and posterior tibial arteries on the affected limb on clinical examination. Wagner’s grade 5 ulcers and ulcers extending above ankle joint were excluded from this study as difficulties were expected to arise in feeling foot pulses and in the accurate measurement of ABI and TcPO2. Patients with varicose vein of grade C2 or above and those with grade 2 or 3 of lymphedema also were excluded because the co-occurrence of these conditions was expected to interfere with wound healing. As some of the patients are under revascularisation procedures like angioplasty or bypass surgeries, those patients with palpable peripheral pulsations after successful revascularisation procedures also were excluded from this study. Diabetes mellitus was defined as per the diagnostic criteria of the World Health Organization (WHO), as someone with a fasting blood glucose level of ≥ 126 mg/dl, 2-h post-prandial glucose of ≥ 200 mg/dl and HbA1c value of ≥ 6.5 DCCT%.
Sample Size and Sampling
Sample size was calculated based on the results of a previous study [18]. Assuming the specificity of ABI and TcPO2 in predicting wound healing to be 75% and 53.6%, respectively, and the ulcer healing rate to be 76%, at 80% power and at 5% alpha error, minimum sample size required was 103 cases of diabetic foot ulcer. Consecutive sampling of all eligible cases that were admitted during the study period was done, and a total of 121 patients were recruited to account for possible attrition.
Study Procedure
The study was approved by the Institute Ethical Committee (IEC) of Malabar Institute of Medical Sciences Limited, Kozhikode. Recruitment of participants was done between March 2016 and March 2018. Eligible patients admitted in the wards who fit the inclusion and exclusion criteria were approached, and all those who gave informed consent were enrolled into the study. Socio-demographic details like age and gender were collected, and history of comorbidities was collected from the case notes. The sites of ulcer, ABI and TcPO2 were assessed by the investigator.
Using a blood pressure cuff and a handheld Doppler, systolic pressure of dorsalis pedis and tibialis posterior were recorded. In a similar technique, brachial artery systolic pressures on both sides were also recorded. ABI was calculated by dividing the higher ankle pressures (dorsalis pedis or posterior tibial artery) in the affected foot by the higher of the two brachial artery systolic pressures. The ABI values were categorised as false elevation (> 1.3), normal/borderline (0.91–1.29), mild PAD (0.7–0.9), moderate PAD (0.4–0.69) and severe PAD (< 0.4).
TcPO2 was recorded by keeping an adhesive sensor (fixation ring with contact liquid) containing a platinum electrode on the affected foot near the ulcer on a relatively flat surface (Fig. 1). The value of partial pressure of oxygen in the tissue was recorded after 15 min as seen on a monitor. Once the test was completed, the sensors were removed, the testing sites were cleaned, and any dressings were reapplied on the ulcers.
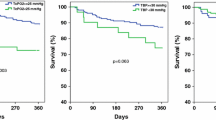
Follow-up review was done after 3 months, when the condition of the ulcer was recorded again. Those patients with ulcers that had healed or had healing changes like granulation tissue were grouped into one group, and those ulcers without any healing changes or those that led to amputation at a level above the ankle were grouped into another. Values of ABI and TCPO2 in each group were compared.
Data Entry and Analysis
Data was collected on paper-based forms and entered into Microsoft Excel 2013. Data analysis was done using Statistical Package for the Social Sciences (SPSS) v22. Continuous variables like age, ABI and TcPO2 were expressed in mean (SD) when normally distributed and median (IQR) when non-normal. These values were also categorised based on standard definitions and expressed as proportions. Categorical variables were expressed as frequency and proportion. Healing status was considered primary outcome variable. ABI on the affected foot and TcPO2 on the affected foot were considered primary explanatory variables. The association between explanatory variables and categorical outcomes was assessed by cross tabulation and comparison of percentages. Chi-square test was used to test statistical significance. ROC analysis: The utility of ABI on the affected foot and TcPO2 on the affected foot in predicting healing status was assessed by receiver operative curve (ROC) analysis. Area under the ROC curve along with its 95% CI and P value are presented. The test results were categorised into high and low based on the cut-off obtained from receiver operating characteristic (ROC) analysis. The sensitivity, specificity, predictive values and diagnostic accuracy of the screening along with their 95% CI were presented. Chi-square test was also employed to look at association of healing status with the test categories. A P value < 0.05 was considered statistically significant.
Results
A total of 382 patients were admitted for the treatment of diabetic foot ulcer during the study period. After applying the inclusion and exclusion criteria, 121 patients were included in the study. The socio-demographic details of the patients are given in Table 1. The age of the patients ranged between 40 and 85 years with a mean (SD) age of 64.9 (10.03) years. Men constituted 73.6% of the study sample. Coronary artery disease and hypertension were the most common comorbidities, found in 38.8% and 30.6% subjects, respectively.
The ABI and TcPO2 values recorded on the affected foot are given in Table 2. ABI values were found to be normal/borderline in 24 (19.8%) and high (above 1.3) indicatory of calcified vessel wall in 20 (16.5%) participants. Mild, moderate and severe PAD were found in 24 (19.8%), 31 (25.6%) and 22 (18.2%), respectively.
After 3 months of follow-up, 72 (59.5%) participants had a positive outcome, and the remaining had a negative outcome. Out of the 72 participants with positive outcome, 43 (59.7%) had ulcers that were partially healed and 29 (40.3%) had complete healing. Out of the 49 participants with a negative outcome, 35 (71.4%) presented with an unhealthy wound, 13 (26.5%) had undergone a below knee amputation, and 1 (2.1%) had undergone an above knee amputation.
Analysis based on receiver operator characteristic curve (ROC) revealed that both ABI and TcPO2 can be used as a tool to predict healing of diabetic ulcer, and this result was statistically significant for both the variables. The ROC curve is shown in Fig. 2. Areas under the curve for ABI and TcPO2 were 0.817 (95% CI 0.732–0.900; P value < 0.001) and 0.896 (95% CI 0.836–0.960; P value < 0.001), respectively. The optimum cut-off point identified for ABI was 0.65 and that for TcPO2 27.5. Higher values of ABI and TcPO2 were associated with higher recovery, and this was found to be statistically significant, as seen in Table 3.
An ABI value of 0.65 or more on the affected foot had a sensitivity of 86.1% (95% CI 78.11% to 94.1%) and specificity of 75.5% (95% CI 63.46 to 87.5) in predicting healing status. Positive and negative predictive values were 83.8% (95% CI 75.41 to 92.2) and 78.7% (95% CI 66.99–90.4), and the total diagnostic accuracy was 81.8% (95% CI 74.95 to 88.7). TcPO2 value of 27.5 and above on the affected foot had a sensitivity of 84.7% (95% CI 76.38 to 93.0) and specificity of 81.6% (95% CI 70.75 to 92.4). Positive predictive value was 87.1% (95% CI 79.25% to 95.0%), negative predictive value was 78.4% (95% CI 67.11% to 89.7%), and the total diagnostic accuracy was 83.5% (95% CI 76.85% to 90.1%). These are summarised in Table 4.
Discussion
The study was conducted among 121 participants, majority of whom were men and above 50 years of age. The older age group is explained as diabetes mellitus has skewed prevalence that progresses with the aged demographic. The definitive male predominance in diabetic foot ulcers may be due to higher exposure of males to smoking. A similar observation was made by Veves et al. [19].
According to ROC analysis, both ABI and TcPO2 can be good predictors in diabetic foot ulcer healing, with area under the curve being slightly higher for TcPO2. ABI showed better sensitivity, but TcPO2 had better specificity, positive predictive value and overall diagnostic accuracy. The cut-off obtained by the ROC analysis was 0.65, which is close to the conventionally used cut-off of 0.7 for the presence of PAD. A study conducted in South India documented the optimal cut-off to be 0.77. The cut-off identified for TcPO2 in the same study was 25 mmHg, which is two points lower than the present study [18]. Another study in China has also recorded that ulcer healing was better in those with higher TcPO2, and everyone with a value at or above 40 mmHg achieved wound closure, and 25 mmHg was identified as the best threshold for predicting wound healing [20]. These differences may be attributed to instrumental errors, or sampling error, and are nevertheless coherent with the results generated.
Similar to our study, Majid Kalani et al. concluded that TcPO2 was a better predictor than ABI in diabetic patients with chronic foot ulcers [21]. This might be due to several factors. ABI estimates the average blood flow at the level of ankle joint but does not consider the microvascular changes that occur in diabetic foot [22]. However, TcPO2 indicates average oxygen level in the tissue near the ulcer; hence, the microvascular changes at the foot will affect the value. Another drawback of ABI is that it may read falsely high values in calcified vessel wall [23, 24]. The Eurodiale study noted that if ABI was abnormal, there was a greater chance that TcPO2 would also be abnormal, whereas if the ABI was normal, the TcPO2 may have been normal or abnormal. This was well explained by the fact that ABI measures circulation in medium-sized vessels which, if low, will mostly lead to a lower capillary blood flow and low transcutaneous pressure of oxygen [25]. Hence, Tcpo2 is a more reliable predictor of tissue perfusion and wound healing.
However, keeping in mind the higher sensitivity and ease of measuring, ABI may be employed as a screening test to aid identification of individuals at a higher risk for delayed healing and amputation. In such a scenario, a larger sensitivity would help in ensuring lesser false negativity rates.
Our study has several strengths. It is one of the few studies done in India to look at the predictive validity of ABI and TcPO2 in diabetic ulcer healing. As it was a prospective study, temporality could be clearly established. There was no attrition or loss to follow-up. All the measurements and assessments were done by a single investigator with a calibrated instrument; hence, interobserver bias was eliminated. The required sample size was achieved. The main limitation of the study is that it was done at a single centre catering to patients of a limited demographic area. Confounding factors like adherence to treatment and history of smoking was not assessed.
Conclusion
ABI and TcPO2 are both good predictors of ulcer healing among patients with diabetes with area under the curve being slightly higher for TcPO2 in ROC analysis. ABI had better sensitivity, while TcPO2 had better specificity, positive predictive value and diagnostic accuracy.
References
Fard AS, Esmaelzadeh M, Larinjani B (2007) Assessment and treatment of diabetic foot ulcer. Int J Clin Pract 61(11):1931–1938
Armstrong EJ, Walternerger J, Rogers JH (2014) Percutaneous coronary intervention in patients with diabetes: current concepts and future directions. J Diabetes Sci Technol 8(3):581–589
Wild SH, Roglic G, Green A, Sicree R, King H (2004) Global prevalence of diabetes: estimates for the year 2000 and projections for 2030: response to Rathman and Giani. Diabetes Care 27(10):2569–2570
Saad N, Elhadedy K, Ramadan N, Mohmady O, Farid M (2013) The prevalence and risk categorisation of diabetic foot complications in cohort group in Beni Suif, Egypt. Life Sci J 3:10
Jain AKC (2012) A new classification of diabetic foot complications: a simple and effective teaching tool. J Diabetic Foot Complicat 4:1–5
Amogne W, Reja A, Amare A (2011) Diabetic foot disease in Ethiopian patients: a hospital based study. Ethiop J Health Sci 25(1):17–21
Abbot CA, Carrington AL, Ashe H, Bath S, Every LC, Griffiths J et al (2002) The north-west diabetes foot care study: incidence of, and risk factors for, new diabetic foot ulceration in a community-based patient cohort. Diabet Med 19(5):377–384
Kumhar M, Dara N, Saini T (2014) Foot wear and footcare knowledge—an independent risk factor for diabetic foot in Indian diabetics. Indian Med Gazette 148(1):25–28
Prompers L, Huijberts M, Apelqvist J, Jude E, Piaggesi A, Bakker K, Edmonds M, Holstein P, Jirkovska A, Mauricio D, Ragnarson Tennvall G, Reike H, Spraul M, Uccioli L, Urbancic V, van Acker K, van Baal J, van Merode F, Schaper N (2007) High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia. 50(1):18–25
Nyamu PN, Otieno CF, Amayo EO, McLigeyo SO (2003) Risk factors and prevalence of diabetic foot ulcers at Kenyatta National Hospital, Nairobi. East Afr Med J 80(1):36–43
Prompers L, Schaper N, Apelqvist J, Edmonds M, Jude E, Mauricio D, Uccioli L, Urbancic V, Bakker K, Holstein P, Jirkovska A, Piaggesi A, Ragnarson-Tennvall G, Reike H, Spraul M, van Acker K, van Baal J, van Merode F, Ferreira I, Huijberts M (2008) Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. The EURODIALE Study. Diabetologia 51(5):747–755
Siersma V, Thorsen H, Holstein PE, Kars M, Apelqvist J, Jude EB, Piaggesi A, Bakker K, Edmonds M, Jirkovska A, Mauricio D, Ragnarson Tennvall G, Reike H, Spraul M, Uccioli L, Urbancic V, van Acker K, van Baal J, Schaper NC (2013) Importance of factors determining the low health-related quality of life in people presenting with a diabetic foot ulcer: the Eurodiale study. Diabet Med 30(11):1382–1387
Lazarides MK, Giannoukas AD (2007) The role of hemodynamic measurements in the management of venous and ischemic ulcers. Int J Low Extrem Wounds 6(4):254–261
Renner R, Simon JC (2008) Current therapeutic options of chronic leg ulcers. JDDG 6(5):389–401
Pecoraro RE, Reiber GE, Burgess EM (1990) Pathways to diabetic limb amputation: basis for prevention. Diabetes Care 13(5):513–521
Beckert S, Pietsch AM, Küper M, Wicke C, Witte M, Königsrainer A, Coerper S (2009) MAID: a prognostic score estimating probability of healing in chronic lower extremity wounds. Ann Surg 249(4):677–681
Beckert S, Witte M, Wicke C, Königsrainer A, Coerper S (2006) A new wound-based severity score for diabetic foot ulcers: a prospective analysis of 1,000 patients. Diabetes Care 29(5):988–992
Lalithambika CV, Nisha B, Saraswathy L, Varma AK, Jose A, Sundaram KR (2014) Ankle brachial index and transcutaneous partial pressure of oxygen as predictors of wound healing in diabetic foot ulcers. J Diabetic Foot Complicat 6(2):54–59
Veves A, Murray HJ, Young MJ, Boulton AJ (1992) The risk of foot ulceration in diabetic patients with high foot pressure: a prospective study. Diabetologia. 35(7):660–663
Yang C, Weng H, Chen L, Yang H, Luo G, Mai L, Jin G, Yan L (2013) Transcutaneous oxygen pressure measurement in diabetic foot ulcers: mean values and cut-point for wound healing. J Wound Ostomy Continence Nurs 40(6):585–589
Kalani M, Brismar K, Fagrell B, Ostergren J, Jörneskog G (1999) Transcutaneous oxygen tension and toe blood pressure as predictors for outcome of diabetic foot ulcers. Diabetes Care 22(1):147–151
Park SC, Choi CY, Ha YI, Yang HE (2012) Utility of toe-brachial index for diagnosis of peripheral artery disease. Arch Plast Surg 39(3):227–231
Ix JH, Miller RG, Criqui MH, Orchard TJ (2012) Test characteristics of the ankle-brachial index and ankle-brachial difference for medial arterial calcification on X-ray in type 1 diabetes. J Vasc Surg 56(3):721–727
Aubert CE, Cluzel P, Kemel S, Michel PL, Lajat-Kiss F, Dadon M, Hartemann A, Bourron O (2014) Influence of peripheral vascular calcification on efficiency of screening tests for peripheral arterial occlusive disease in diabetes—a cross-sectional study. Diabet Med 31(2):192–199
Bacharach JM, Rooke TW, Osmundson PJ, Gloviczki P (1992 Mar) Predictive value of transcutaneous oxygen pressure and amputation success by use of supine and elevation measurements. J Vasc Surg 15(3):558–563
Author information
Authors and Affiliations
Contributions
All authors were involved in the clinical care of the patient. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
The study was approved by the Institute Ethical Committee (IEC) of Malabar Institute of Medical Sciences Limited, Kozhikode.
Conflict of Interest
The authors declare no potential conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Thottiyen, S., Kuruvilla, R., George, A. et al. Ankle Brachial Index vs Transcutaneous Partial Pressure of Oxygen for Predicting Healing of Diabetic Foot Ulcers with Peripheral Arterial Disease: a Comparative Study. Indian J Surg 85 (Suppl 1), 183–188 (2023). https://doi.org/10.1007/s12262-020-02587-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-020-02587-z