Abstract
Pseudorabies virus (PRV) is known to cause severe encephalitis in juvenile pigs and various non-native hosts; recent evidences suggest that PRV might cause encephalitis in humans. In a multicenter cohort study in China, next-generation sequencing of cerebrospinal fluid (CSF) was performed to detect pathogens in all patients with clinically suspected central nervous system infections. This study involved all the patients whose CSF samples were positive for PRV-DNA; their clinical features were evaluated, and species-specific PCR and serological tests were sequentially applied for validation. Among the 472 patients tested from June 1, 2016, to December 1, 2018, six were positive for PRV-DNA, which were partially validated by PCR and serological tests. Additionally, we retrospectively examined another case with similar clinical and neuroimaging appearance and detected the presence of PRV-DNA. These patients had similar clinical manifestations, including a rapid progression of panencephalitis, and similar neuroimaging features of symmetric lesions in the basal ganglia and bilateral hemispheres. Six of the patients were engaged in occupations connected with swine production. PRV infection should be suspected in patients with rapidly progressive panencephalitis and characteristic neuroimaging features, especially with exposure to swine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Infectious encephalitis, which is a central nervous system (CNS) infection caused by a wide range of pathogens, causes significant morbidity and mortality worldwide (Brown et al. 2018). However, even in the best-equipped medical centers, specific etiologies are identified in less than two thirds of patients with encephalitis (Brown et al. 2018). Previous studies have demonstrated the power of next-generation sequencing (NGS) for identifying unknown pathogens of CNS infections (Brown et al. 2018; Hoffmann et al. 2015).
Pseudorabies virus (PRV), also known as suid herpesvirus 1 or Aujeszky’s disease virus, is a neurotrophic alphaherpesvirus with a double-stranded DNA genome (Zimmerman et al. 2012). PRV almost infects its only natural host, swine (Zimmerman et al. 2012). PRV infection causes extremely high mortality in young pigs and only innocuous respiratory signs in older pigs (Zuckermann 2000). In addition, PRV infects a wide range of other non-native hosts, including cattle, sheep, dogs, cats, chickens, rodents, rabbits, foxes, and some nonhuman primates (Baskerville and Lloyd 1977; Hurst 1936; Pomeranz et al. 2005). Although the recent in-vitro experiment has suggested the possibility of PRV infection in humans (Li et al. 2017), there are limited data on the transmission of PRV infection from animal to human. To our knowledge, suspected cases of PRV infection in human are rare worldwide, and even fewer have been laboratory-confirmed (Tischer and Osterrieder 2010). In 1914, two suspected cases of pseudorabies in laboratory technicians with exposure to infectious material were reported, but serological or pathogenic evidence was lacking. In 1987, three human cases of PRV infection identified by serological evidence were first reported (Mravak et al. 1987). Recently, Ai et al. reported a case of swineherd who developed endophthalmitis caused by PRV (Ai et al. 2018). In general, the reported PRV infections of humans differ from those of other non-native hosts, which is fatal and characterized by severe central nervous system signs (Zimmerman et al. 2012).
In April 2018, we reported four cases with suspected PRV encephalitis in humans (Zhao et al. 2018). Since then, several cases were reported in China (Wang et al. 2019; Yang et al. 2019a, b). Here, we present the further pathogen investigation results of the three previous reported cases (one case without pathogen validation is not present here) and add four new cases. The detailed clinical, neuroimaging, CSF, NGS, PCR, and serological data are provided.
Materials and methods
Case series
We obtained the data from the multicenter unbiased NGS of CSF project for the period June 1, 2016, to December 1, 2018. The NGS of CSF project is a multicenter cohort study. In this project, patients with clinically suspected CNS infections of undiagnosed etiologies (see Supplementary Table 1 for case definitions and exclusion criteria) were enrolled, and all medical information was recorded in the research database. CSF and blood samples were collected and stored at − 80 °C; unbiased NGS was performed on all of the CSF samples. In this study, we selected the six cases with PRV DNA in CSF.
A retrospective case (Case 4) was also reported in this study. This patient was admitted to hospital in October 2011. When reviewing the medical records in 2017, we found that her clinical and neuroimaging features were similar to those of other PRV encephalitis cases. Laboratory tests were therefore performed, and PRV DNA was detected by NGS in the remained CSF samples.
This study was approved by the Institutional Review Board of Peking Union Medical College Hospital (PUMCH) (IRB no. JS-890). The use of the patients’ clinical data and CSF samples was approved by the Ethics Committee of PUMCH. Written informed consent was obtained from each patient or their legal surrogate in accordance with the Declaration of Helsinki.
NGS of CSF
NGS of patients’ CSF samples was performed according to a standard flow, which has been used for detecting herpes simplex virus 1 (HSV-1), HSV-2, varicella zoster virus (VZV), Listeria monocytogenes, and Brucella (Fan et al. 2017; Guan et al. 2016; Yao et al. 2016). Sequencing was performed on a BGISEQ-100 platform. The qualified reads were mapped to the human reference genome using the Burrows-Wheeler Aligner. The remaining data were aligned to the NCBI microbial genome database (ftp://ftp.ncbi.nlm.nih.gov/genomes/) for the detection of pathogens (PRV: KF017583.1 2, KT824771.1 1).
PCR and Sanger validation
To verify the presence of PRV sequences, we used species-specific PCR to amplify target fragments with the forward, CGGCGAACTGCGGGATAT, and reverse, CCCGTCAACGAGGTCATCG, primers. Agarose gel electrophoresis was used to analyze PCR products, and Sanger sequencing with an ABI Prism 3730 DNA Analyzer (Applied Biosystems, Foster City, CA, USA) was conducted for validation purposes. Sequences were aligned to the NT database using NCBI BLAST (http://blast.ncbi.nlm.nih.gov/Blast.cgi?PROGRAM=blastn&PAGE_TYPE=BlastSearch&LINK_LOC=blasthome).
Anti-PRV antibody detection
Glycoprotein B (gB) and glycoprotein E (gE) antibodies in serum or CSF were detected using a Pseudorabies Virus gB Antibody Test Kit (IDEXX Laboratories, Westbrook, ME, USA) and gE Antibody Test Kit (IDEXX Laboratories, Westbrook, ME, USA), which are commercially available inhibition enzyme-linked immunosorbent assays (ELISAs) that make use of anti-PRV gB and gE monoclonal antibodies, respectively.
Results
Clinical findings
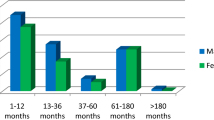
During the study period, 472 patients with clinical symptoms of CNS infection were enrolled in the prospective research. Of the 472 CSF samples, six (Cases 1, 2, 3, 5, 6, and 7) contained PRV DNA. One retrospective case (Case 4) with similar clinical and neuroimaging features was also detected to contain PRV DNA. Their clinical features are summarized in Table 1; the laboratory and neuroimaging examinations are summarized in Table 2 and Supplementary Table 2. These patients shared some striking clinical and neuroimaging features.
Part of the medical history of Cases 5, 6, and 7 were reported previously (Zhao et al. 2018). Herein, we made further pathogen investigations, including the analysis of the NGS results and the performance of PCR and serological tests. The detailed medical history of Cases 1, 2, 3, and 4 is provided here. The brain MRI of Cases 5 and 7, which was not presented previously, is provided (Fig. 1i–x).
Brain magnetic resonance imaging (MRI) of patients with PRV encephalitis. a–d Brain MRI for Case 3 (35 days after disease onset) showed lesions of FLAIR hyper-intensities in the bilateral insular lobes, temporal lobes, frontal lobes, hippocampus, and brainstem and a left basal ganglia hemorrhage. e–h Brain MRI for Case 4 (42 days after disease onset) showed symmetric lesions of FLAIR hyper-intensities in the basal ganglia, insular lobes, medial temporal lobes, frontal lobes, and parietal lobes bilaterally. i–l Brain MRI for Case 5 (37 days after disease onset) showed symmetric lesions of FLAIR hyper-intensities in the bilateral insular lobes, temporal lobes, frontal lobes, parietal lobes, thalami, hippocampus, basal ganglia, and cerebral peduncle. m–t Brain MRI for Case 7 (13 days after disease onset) symmetric lesions of FLAIR and DWI hyper-intensities in the bilateral insular lobes, temporal lobes, frontal lobes, hippocampus, and basal ganglia. u–x Brain MRI for Case 7 (5 months after disease onset) showed diffuse symmetric lesions of FLAIR hyper-intensities and cerebral atrophy. CP cerebral peduncle, He: hemorrhage of left basal ganglia, Hi hippocampus, IL insular lobe, FL frontal lobe, TL temporal lobe, Th thalamus, BG basal ganglia
Case 1: A mid-aged male presented with high fever, recurrent epileptic seizures, and loss of consciousness (LOC). One day before admission, his symptoms began with high fever and involuntary jerk movements of the right hand. On admission, PE revealed apathy, dullness, and cognitive decline. About 2 h after admission, he developed recurrent tonic–clonic seizures. He was intubated and sedated. Lumbar puncture revealed increased opening pressure, pleocytosis, and normal protein and glucose levels. Lung CT (day 3 after admission) showed diffuse ground-glass opacification bilaterally. A funduscopic examination showed bilateral retinal necrosis. The patient received VPA for seizures and was empirically treated with acyclovir, IVIg, and high-dose methylprednisolone. One week later, NGS of CSF resulted in the detection of PRV DNA. Acyclovir was continued. The patient died 2 weeks later.
Case 2: A mid-aged male presented with high fever, cognitive decline, recurrent epileptic seizures, and LOC. One month before the symptoms began, two older pigs and several other pigs weighing 15–20 kg died on his farm; there were also many stillbirths. Symptoms began with high fever 4 days before admission. Meanwhile, the patient developed recurrent seizures, each episode was several seconds in duration. Eight hours before admission, he developed cognitive decline and recurrent tonic–clonic seizures. Brain MRI showed symmetric lesions of T1WI hypo-intensities and T2WI hyper-intensities in the insular lobes and medial temporal lobes bilaterally. Lumbar puncture revealed increased opening pressure, normal WBC count, and normal protein and glucose levels. The seizures were well controlled by treatment with VPA, PB, and carbamazepine (CBZ). The patient was also empirically treated with acyclovir, foscarnet, and methylprednisolone. Nine days later, NGS of CSF resulted in detection of PRV DNA. Ten days later, he was intubated because of respiratory failure. Three weeks later, he was extubated and was able to communicate and walk. One month later, the patient developed blindness bilaterally, and a funduscopic examination showed vasculitis bilaterally, with occlusion of the right retinal arteries and part of the left retinal arteries (Fig. 2a, b). Optical coherence tomography (OCT) showed right epiretinal membranes and macular edema, as well as left retinal thinning (Fig. 2c, d). Acyclovir and methylprednisolone were continued. Two and a half months later, the patient’s vision had partially improved. Four months later, he had residual symptoms of memory loss and hand tremor bilaterally.
Ophthalmologic examination of a patient with PRV encephalitis. a, c Funduscopic examination showed vasculitis bilaterally, with occlusion of the right retinal arteries and part of the left retinal arteries. b, d Optical coherence tomography (OCT) showed right macular edema, accompany with a moth-eaten appearance, as well as left retinal thinning. e, g Funduscopic examination photograph of a healthy adult. e Right side. g Left side. f, h OCT of a healthy adult. f Right side. h Left side. VH vitreous humor, R retina, MF macula fovea, RPE retinal pigment epithelium, RA retinal artery, O occlusion of the retinal artery, T thinning of the retina, M moth-eaten appearance
Case 3: A young male presented with fever, seizures, and LOC for 3 days. On admission, a brain CT showed no abnormality. Lumbar puncture revealed pleocytosis, mild elevation of the protein level, and a normal glucose level. The creatinine and creatine kinase levels were significantly elevated. He was intubated and treated with continuous renal replacement treatment and was given VPA, clonazepam, and phenobarbital for his seizures. One week later, NGS of CSF resulted in detection of PRV DNA. Therefore, he was treated with acyclovir and IVIg. Three weeks later, the pupils of the patient were dilated and did not react to light. A brain CT was repeated and showed a left basal ganglia hemorrhage. Four weeks later, he was extubated. Five weeks later, a brain MRI showed lesions of FLAIR hyper-intensities in the bilateral insular lobes, temporal lobes, frontal lobes, hippocampus, and brainstem and a left basal ganglia hemorrhage (Fig. 1a–d). Ten weeks later, he resumed consciousness and was able to obey commands.
Case 4: A young female presented with high fever, psychotic behavior, and recurrent seizures for 5 days. On admission, a brain MRI showed symmetric lesions of T1WI hypo-intensities and T2WI hyper-intensities in the basal ganglia, insular lobes, medial temporal lobes, frontal lobes and parietal lobes bilaterally (Fig. 1e–h). Lumbar puncture revealed pleocytosis, mild elevation of the protein level, and a normal glucose level. Funduscopic examination showed bilateral fundus hemorrhage and papilledema. The patient was empirically treated with acyclovir and foscarnet and was given VPA and CBZ for her seizures. She rapidly fell into a comatose state and was intubated. She died 2 months later.
Pathogen investigation
PRV DNA was detected by NGS in the CSF samples of all seven patients, but not in non-template controls (NTCs). An additional 466 patients with clinically suspected CNS infections, including tuberculous meningitis, cryptococcal meningitis, and neurobrucellosis (Fan et al. 2017), were negative for PRV. Among these seven patients, the numbers of raw reads ranged from 13,170,121 to 48,512,319. The numbers of reads corresponding to PRV ranged from 6 to 242, with genomic coverage ranging from 0.2 to 16% and reads per million (RPM) ranging from 0.18 to 18.37. The NGS results are provided here (see Table 4; Supplementary Table 3 and Supplementary Figure 3). Common contaminating microorganisms at our center have been discussed elsewhere (Fan et al. 2017).
The presence of PRV DNA in the CSF was confirmed by PCR in Cases 2 and 6 (Supplementary Figure 4A-B.). In other cases, the volume of CSF samples was insufficient for PCR.
The serological results are summarized (see Table 3). The serum and CSF samples of Cases 5 and 6 were positive for both gB and gE antibodies, and the serum sample of Case 3 was positive for both gB and gE antibodies (PRV-gE antibody is applied for determining wild-type virus infection and the PRV-gB antibody for evaluating vaccine immunization).
Discussion
Here, we report a case-series of PRV encephalitis in humans diagnosed with NGS of CSF (Table 4). Some of them were further confirmed by Sanger sequencing and/or serological tests. Along with the seven cases here, there were 14 cases with PRV encephalitis reported (Wang et al. 2019; Yang et al. 2019a, b; Zhao et al. 2018). The clinical features of the 14 cases were summarized in Table 5. The first case emerged in 2011, and the other cases occurred after 2017. Our findings suggest that PRV can cause encephalitis and is highly lethal in human, as in other non-native hosts. It also highlights the importance of pathogen-discovery programs in encephalitis of unknown etiology as a strategy for pandemic preparedness.
The patients with PRV encephalitis had several shared clinical features. First, they all demonstrated severe CNS involvement with rapid progression and an extremely poor prognosis. Previously reported cases had mild symptoms and good outcomes (Ai et al. 2018; Mravak et al. 1987). The three patients reported in 1987 developed symptoms of fever, sweating, weakness, and cranial nerves I, V, and IX involvement. All recovered completely without sequelae (Sawitzky 1997). The clinical symptoms and severity of the virus infection in humans in our case series seem to match those seen so far in other non-native hosts, such as monkeys (Hurst 1936). In PRV-infected monkeys, nervous symptoms appeared abruptly about 3 to 7 days after inoculation, followed by epileptic seizures in the next 12 h; in severe cases, the monkey experienced status epilepticus after an additional 24 or 48 h (Hurst 1936). PRV encephalitis in human progresses even more rapidly, with development of status epilepticus in less than 1 week. All seven patients were admitted to the ICU and required intubation and mechanical ventilation. The prognosis of our patients was extremely poor, supported by the fact that four died and three had poor outcomes (mRS 3 and 5, respectively). Second, simultaneous ocular infection could be caused by PRV, symptoms of which were observed in three of the seven cases in this study. This is consistent with a previous report of human endophthalmitis caused by PRV infection (Ai et al. 2018). Third, simultaneous pneumonia can be caused by PRV. Although previous studies suggested that PRV attacks only neural tissue in monkeys (Baskerville and Lloyd 1977; Hurst 1936), accompanying pneumonia seems plausible because pneumonia can precede encephalitis (as demonstrated in Case 5) and PRV is tropic for the respiratory system of swine (Zimmerman et al. 2012). The question of whether PRV can infect the human respiratory system warrants further investigation. Fourth, the CSF changes may be mild in PRV encephalitis, especially in the early stage. In our case series, CSF samples showed mild inflammation with increased opening pressure, mild pleocytosis, a normal or slightly increased protein level, and a normal glucose level. WBC counts were nearly normal in the first week of symptom presentation. Fifth, PRV encephalitis is refractory to treatment. In our case series, PRV encephalitis responded poorly to acyclovir and immunotherapy. A previous in vitro study suggested that dexamethasone potentiates PRV-induced CNS damage (Clase and Banfield 2003). Sixth, it is possible that a negative result was observed in the gE/gB antibody tests within 10 days after disease onset. Further studies are necessary to determine the time course of the antibody response. Similar clinical features can be seen in other reported cases (Wang et al. 2019; Yang et al. 2019a, b).
The patients with PRV encephalitis also had several shared neuroimaging features. First, the grey matter, including the cortex and nuclei in the basal ganglia, was the main area injured. The neuropathology of monkeys infected with PRV also suggests that PRV affects predominantly the grey matter (Baskerville and Lloyd 1977). Second, lesions in the brain were extensive and not limited to the limbic system. Cases 2, 4, 5, and 7 had symmetric lesions of T1WI hypo-intensities and T2WI hyper-intensities in the bilateral insular, temporal, frontal, and parietal lobes and in the basal ganglia. Cases 3, 4, and 5 also had lesions in the bilateral cerebral peduncle. Previous pathological studies demonstrated that young piglets tend to develop panencephalitis, with the most severe lesions in the cerebral cortex, brain stem, spinal ganglia, and basal ganglia of the brain (Zimmerman et al. 2012; Olander et al. 1966). In infected monkeys, the principal injured areas are the pyriform area, cornu Ammonis, island of Reil, lower lip of the Sylvian fissure, and basal surface of the frontal lobe (Hurst 1936). The lesion distribution in our patients is consistent with the finding of pathological studies in other mammals. Third, head CT is not sufficiently sensitive to detect early stage lesions. Head CT was negative within 2 weeks of disease onset in our case series.
It is notable that most of the patients in our case series reported a history of sustained exposure to swine production; moreover, most were from northern China, the area of swine pseudorabies (PR) outbreaks. Therefore, it is plausible that human PRV encephalitis is of swine origin. The prevalence of PRV in swine was high in China before introduction of the glycoprotein E (gE)-deleted PRV vaccine (Bartha-K61 strain) from Hungary in the 1970s, which effectively controlled PR (Liu et al. 2018; Tong et al. 2015). Although more than 90% of pigs are positive for PRV-gB antibody (Liu et al. 2018), another outbreak of swine PR occurred in late 2011 in northern China (An et al. 2013; Luo et al. 2014; Tong et al. 2015; Wu et al. 2013; Yu et al. 2014; Zhang et al. 2015) and was associated with a substantial increase in the PRV-gE antibody positive rate (Liu et al. 2018; Gu et al. 2018) and in the infection rates of non-native hosts (Jin et al. 2016; Liu et al. 2017; Wang et al. 2018; Zhang et al. 2015). This evidence supports the hypothesis that a PRV variant, genetically different from classic PRV strains, is the cause of the outbreak of PR (An et al. 2013; Luo et al. 2014; Tong et al. 2015; Ye et al. 2015). The absence of human infection in China prior to 2011 might be because the original version of the virus does not easily infect humans or because it is not particularly pathogenic, whereas a mutated pseudorabies virus might be responsible for the more recent reports. Unfortunately, we are unable to establish causation due to the small number of samples; further phylogenetic studies are needed to confirm our findings.
The PRV-gE positive rate is more than 50% in northern China, indicating severe variant PRV infection pressure (Luo et al. 2014; Ye et al. 2015). However, it does not necessarily indicate that the virus is on course to cause a severe epidemic; PRV is not highly transmissible between animals except swine, and the spread of PRV in pig farms responds vigorously to the traditional vaccine. Additionally, there is no evidence of human-to-human transmission. However, vigilance with regard to human infections is necessary due to their clinical severity, and continuous monitoring and regular assessments of the epidemiological characteristics and clinical severity of human infections are required for pandemic risk assessment.
In conclusion, clinicians should be aware of the possibility of PRV encephalitis especially in patients with severe panencephalitis with characteristic neuroimaging features, especially with occupations associated with swine products.
References
Ai JW, Weng SS, Cheng Q, Cui P, Li YJ, Wu HL, Zhu YM, Xu B, Zhang WH (2018) Human endophthalmitis caused by pseudorabies virus infection, China, 2017. Emerg Infect Dis 24:1087–1090. https://doi.org/10.3201/eid2406.171612
An TQ, Peng JM, Tian ZJ, Zhao HY, Li N, Liu YM, Chen JZ, Leng CL, Sun Y, Chang D, Tong GZ (2013) Pseudorabies virus variant in Bartha-K61-vaccinated pigs, China, 2012. Emerg Infect Dis 19:1749–1755. https://doi.org/10.3201/eid1911.130177
Baskerville A, Lloyd G (1977) Experimental infection of monkeys with Herpesvirus suis (Aujeszky's-disease virus). J Med Microbiol 10:139–144. https://doi.org/10.1099/00222615-10-1-139
Brown JR, Bharucha T, Breuer J (2018) Encephalitis diagnosis using metagenomics: application of next generation sequencing for undiagnosed cases. J Inf Secur 76:225–240. https://doi.org/10.1016/j.jinf.2017.12.014
Clase AC, Banfield BW (2003) Corticosteroids are unable to protect against pseudorabies virus-induced tissue damage in the developing brain. J Virol 77:4979–4984. https://doi.org/10.1128/jvi.77.8.4979-4984.2003
Fan S, Ren H, Wei Y, Mao C, Ma Z, Zhang L, Wang L, Ge Y, Li T, Cui L, Wu H, Guan H (2017) Next-generation sequencing of the cerebrospinal fluid in the diagnosis of neurobrucellosis. Int J Infect Dis 67:20–24. https://doi.org/10.1016/j.ijid.2017.11.028
Gu J, Hu D, Peng T, Wang Y, Ma Z, Liu Z, Meng F, Shang Y, Liu S, Xiao Y (2018) Epidemiological investigation of pseudorabies in Shandong Province from 2013 to 2016. Transbound Emerg Dis 65:890–898. https://doi.org/10.1111/tbed.12827
Guan H, Shen A, Lv X, Yang X, Ren H, Zhao Y, Gong Y, Ni P, Wu H, Zhu Y, Cui L (2016) Detection of virus in CSF from the cases with meningoencephalitis by next-generation sequencing. J Neuro-Oncol 22:240–245. https://doi.org/10.1007/s13365-015-0390-7
Hoffmann B, Tappe D, Hoper D, Herden C, Boldt A, Mawrin C, Niederstraßer O, Müller T, Jenckel M, van der Grinten E, Lutter C, Abendroth B, Teifke JP, Cadar D, Schmidt-Chanasit J, Ulrich RG, Beer M (2015) A variegated squirrel bornavirus associated with fatal human encephalitis. N Engl J Med 373:154–162. https://doi.org/10.1056/NEJMoa1415627
Hurst EW (1936) Studies on pseudorabies (infectious bulbar paralysis, mad itch) III. The disease in the rhesus monkey, Macaca mulatta. J Exp Med 63:449–463. https://doi.org/10.1084/jem.63.3.449
Jin HL, Gao SM, Liu Y, Zhang SF, Hu RL (2016) Pseudorabies in farmed foxes fed pig offal in Shandong province, China. Arch Virol 161:445–448. https://doi.org/10.1007/s00705-015-2659-9
Li A, Lu G, Qi J, Wu L, Tian K, Luo T, Shi Y, Yan J, Gao GF (2017) Structural basis of nectin-1 recognition by pseudorabies virus glycoprotein D. PLoS Pathog 13:e1006314. https://doi.org/10.1371/journal.ppat.1006314
Liu H, Li XT, Hu B, Deng X, Zhang L, Lian SZ, Zhang HL, Lv S, Xue XH, Lu RG, Shi N, Yan MH, Xiao PP, Yan XJ (2017) Outbreak of severe pseudorabies virus infection in pig-offal-fed farmed mink in Liaoning Province, China. Arch Virol 162:863–866. https://doi.org/10.1007/s00705-016-3170-7
Liu Y, Zhang S, Xu Q, Wu J, Zhai X, Li S, Wang J, Ni J, Yuan L, Song X, Zhao B, Zhou Z, Wang C, Yang L (2018) Investigation on pseudorabies prevalence in Chinese swine breeding farms in 2013-2016. Trop Anim Health Prod 50:1279–1285. https://doi.org/10.1007/s11250-018-1555-1
Luo Y, Li N, Cong X, Wang C, Du M, Li L, Zhao B, Yuan J, Liu DD, Li S, Li Y, Sun Y, Qiu HJ (2014) Pathogenicity and genomic characterization of a pseudorabies virus variant isolated from Bartha-K61-vaccinated swine population in China. Vet Microbiol 174:107–115. https://doi.org/10.1016/j.vetmic.2014.09.003
Mravak S, Bienzle U, Feldmeier H, Hampl H, Habermehl KO (1987) Pseudorabies in man. Lancet 1:501–502. https://doi.org/10.1016/s0140-6736(87)92105-2
Olander HJ, Saunders JR, Gustafson DP, Jones RK (1966) Pathologic findings in swine affected with a virulent strain of Aujeszky's virus. Vet Pathol 3:64–82. https://doi.org/10.1177/030098586600300104
Pomeranz LE, Reynolds AE, Hengartner CJ (2005) Molecular biology of pseudorabies virus: impact on neurovirology and veterinary medicine. Microbiol Mol Biol Rev 69:462–500. https://doi.org/10.1128/MMBR.69.3.462-500.2005
Sawitzky D (1997) Transmission, species specificity, and pathogenicity of Aujeszky's disease virus. Arch Virol Suppl 13:201–206. https://doi.org/10.1007/978-3-7091-6534-8_19
Tischer BK, Osterrieder N (2010) Herpesviruses—a zoonotic threat? Vet Microbiol 140:266–270. https://doi.org/10.1016/j.vetmic.2009.06.020
Tong W, Liu F, Zheng H, Liang C, Zhou YJ, Jiang YF, Shan TL, Gao F, Li GX, Tong GZ (2015) Emergence of a pseudorabies virus variant with increased virulence to piglets. Vet Microbiol 181:236–240. https://doi.org/10.1016/j.vetmic.2015.09.021
Wang GS, Du Y, Wu JQ, Tian FL, Yu XJ, Wang JB (2018) Vaccine resistant pseudorabies virus causes mink infection in China. BMC Vet Res 14:20. https://doi.org/10.1186/s12917-018-1334-2
Wang Y, Nian H, Li Z, Wang W, Wang X, Cui Y (2019) Human encephalitis complicated with bilateral acute retinal necrosis associated with pseudorabies virus infection: a case report. Int J Infect Dis 89:51–54. https://doi.org/10.1016/j.ijid.2019.09.019
Wu R, Bai C, Sun J, Chang S, Zhang X (2013) Emergence of virulent pseudorabies virus infection in northern China. J Vet Sci 14:363–365. https://doi.org/10.4142/jvs.2013.14.3.363
Yang X, Guan H, Li C, Li Y, Wang S, Zhao X, Zhao Y, Liu Y (2019a) Characteristics of human encephalitis caused by pseudorabies virus: a case series study. Int J Infect Dis 87:92–99. https://doi.org/10.1016/j.ijid.2019.08.007
Yang H, Han H, Wang H, Cui Y, Liu H, Ding S (2019b) A case of human viral encephalitis caused by pseudorabies virus infection in China. Front Neurol 10:534. https://doi.org/10.3389/fneur.2019.00534
Yao M, Zhou J, Zhu Y, Zhang Y, Lv X, Sun R, Shen A, Ren H, Cui L, Guan H, Wu H (2016) Detection of Listeria monocytogenes in CSF from three patients with meningoencephalitis by next-generation sequencing. J Clin Neurol 12:446–451. https://doi.org/10.3988/jcn.2016.12.4.446
Ye C, Zhang QZ, Tian ZJ, Zheng H, Zhao K, Liu F, Guo JC, Tong W, Jiang CG, Wang SJ, Shi M, Chang XB, Jiang YF, Peng JM, Zhou YJ, Tang YD, Sun MX, Cai XH, An TQ, Tong GZ (2015) Genomic characterization of emergent pseudorabies virus in China reveals marked sequence divergence: evidence for the existence of two major genotypes. Virology 483:32–43. https://doi.org/10.1016/j.virol.2015.04.013
Yu X, Zhou Z, Hu D, Zhang Q, Han T, Li X, Gu X, Yuan L, Zhang S, Wang B, Qu P, Liu J, Zhai X, Tian K (2014) Pathogenic pseudorabies virus, China, 2012. Emerg Infect Dis 20:102–104. https://doi.org/10.3201/eid2001.130531
Zhang L, Zhong C, Wang J, Lu Z, Liu L, Yang W, Lyu Y (2015) Pathogenesis of natural and experimental pseudorabies virus infections in dogs. Virol J 12:44. https://doi.org/10.1186/s12985-015-0274-8
Zhao W, Wu Y, Li H, Li S, Fan SY, Wu HL, Li YJ, Lü YL, Han J, Zhang WC, Zhao Y, Li GL, Qiao XD, Ren HT, Zhu YC, Peng B, Cui LY, Guan HZ (2018) Clinical experience and next-generation sequencing analysis of encephalitis caused by pseudorabies virus. Natl Med J Chin 98(15):6. https://doi.org/10.3760/cma.j.issn.0376-2491.2018.15.006
Zimmerman JJ, Karriker LA, Ramirez A, Schwartz KJ, Stevenson GW (2012) Diseases of swine. Wiley-Blackwel, Chichester
Zuckermann FA (2000) Aujeszky's disease virus: opportunities and challenges. Vet Res 31:121–131. https://doi.org/10.1051/vetres:2000111
Acknowledgments
The authors thank the patients for participating in this study.
Funding
This study was funded by the National Key Research and Development Program of China (Grant No. 2016YFC0901502) and National Science and Technology Major Project of China (Grant No.2018ZX10305409–001-001).
Author information
Authors and Affiliations
Contributions
HG and SF contributed to the study conception design. SF, HY, LL, HL, SW, WZ, YW, YF, YL, XQ, GL, DW, HR, YZ, BP, LC, PW, JW, and HG collected the clinical data. LL, JW, and DW examined and treated Case 4 in 2011. HW, YG, and YL performed NGS, bioinformatics analysis, and PCR. YL, JH, WZ, and PC performed pseudorabies virus antibody detection. SF, LL, JW, and HG analyzed the clinical data. SF wrote the first draft of the manuscript after discussions with HG. HW, YG, and YL wrote portions of the methods section. All authors contributed to manuscript revision and have read and approved the submitted version.
Corresponding authors
Ethics declarations
This study was approved by the Institutional Review Board of Peking Union Medical College Hospital (PUMCH) (IRB no. JS-890). The use of the patients’ clinical data and CSF samples was approved by the Ethics Committee of PUMCH. Written informed consent was obtained from each patient or their legal surrogate in accordance with the Declaration of Helsinki.
Conflict of interest
Authors Honglong Wu, Yanping Gong, and Zhenzi Ma were employed by company BGI-Tianjin and BGI-Shenzhen. Author Yongjun Li was employed by company BGI-Shenzhen and Vision Medical. All other authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fan, S., Yuan, H., Liu, L. et al. Pseudorabies virus encephalitis in humans: a case series study. J. Neurovirol. 26, 556–564 (2020). https://doi.org/10.1007/s13365-020-00855-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13365-020-00855-y