Abstract
The purpose of conducting the present research work was to develop resveratrol nanostructured in situ gel for the treatment of Alzheimer’s disease. Resveratrol loaded lipid carrier was prepared by melt emulsification-probe sonication method, and the final product was evaluated for particle size (132 ± 11.90 nm), polydispersity index (0.209 ± 0.005), zeta potential (− 23 ± 3.79 mV), drug loading (9.26 ± 3.79%), and entrapment efficiency (74 ± 11.40%). Following incorporation of the resveratrol nanostructured lipid carrier in gellan gum and xanthan gum, in situ gel was formulated and characterized. The optimized in situ gel showed fivefold higher permeation across the nasal mucosa as compared to resveratrol suspension-based in situ gel. Finally, optimized in situ gel was evaluated using in vivo pharmacodynamic study by the scopolamine-induced amnesia model in rats using Morris Water Maze test. It showed significant improvement in memory function in rats treated with optimized in situ gel as compared to orally administered resveratrol suspension. The enhanced permeation across nasal mucosa and improved memory function suggest that the resveratrol nanostructured lipid carrier-based in situ gel could be an effective and promising approach for the treatment of Alzheimer’s disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) results in slow but a progressive loss of mental, behavioral, and functional abilities of human being. It is the most common neurodegenerative disease and affects more than 80% of elder people worldwide [1]. Different causes of AD include aggregation of amyloid precursor protein (APP), aggregation of Aβ peptides, and neuronal damage [2].
Resveratrol (RES) (trans-3,4,5-trihydroxystilbene) is a natural occurring polyphenolic compound found in grape, wine, peanuts, and soy. Resveratrol promote the non-amyloidogenic cleavage of an amyloid precursor protein (APP) and enhance clearance of Aβ peptides. Owing to this inherent property of RES, it has been used in Alzheimer’s disease treatment [3,4,5,6]. Moreover it is low water solubility, poor bioavailability, chemical instability, extensive metabolism, and excretion for effective drug delivery system [7,8,9]. Hence, a suitable drug delivery system is required to overcome these problems and to deliver RES into the brain.
Researchers reported various lipid-based formulations of RES, to improve solubility and stability [10, 11], to increase oral bioavailability [12, 13], for topical delivery [14], in treatment of cancer [15], in treatment of inflammation and infections [16], and other diseases [17, 18]. The nasal route is evaluated by many researchers for drug delivery of drugs into the brain [19, 20]. However, nasal delivery in the form of nanostructured lipid carrier-based in situ gel is a still unexplored area for the treatment of AD. The numbers of small molecules are available in the market as nasal products for the treatment of various diseases [21]. Nasal route of delivery overcomes drawbacks of oral route of administration such as a high first-pass metabolism and gastrointestinal drug degradation [22].
Researchers have developed various nanocarrier-based formulation of light-sensitive, oxidative-degradable, and hydrolysis-susceptible drugs to improve their bioavailability [23]. Nanostructured lipid carrier offers many advantages like lowering toxicity of drugs and providing higher safety in addition to higher drug loading compared to the other nanocarriers. Furthermore, organic solvents are not required in its manufacturing processes which resulted in economically viable production with higher acceptance by the regulatory agencies across the global markets [24,25,26,27].
Different drug delivery systems viz. spray, solution, and in situ gel are available in the market to administer the drug via nasal route in the olfactory lobe region targeting brain delivery. The purpose of developing in situ gel was to maintain high drug concentration in the nasal cavity for prolonged period assuring maximum absorption [28]. In situ gel demonstrates different benefits such as rapid absorption, fast onset of action, and direct targeting to the brain by olfactory or trigeminal pathway avoiding hepatic first-pass metabolism [29].
Hence, inherent positive features of in situ gel delivery system and necessity to deliver RES to brain target laid the foundation of this research work. To accomplish determined objective, nanostructured lipid carrier-based in situ gel of RES was developed. The objective of present research work was to develop nanostructured lipid carrier-based in situ gel for nasal administration of RES. Further, in situ gel with superior in vitro permeation and rheological properties was selected for in vivo study using scopolamine-induced amnesia in rat using Morris Water Maze test.
Materials and methods
Materials
Resveratrol (RES) was obtained as a gift sample from Sami Labs (Bengaluru, India). Gellan gum and Xanthan gum were received as a gift samples from C. P. Kelco (Mumbai, India). Mohini Organic Limited (Mumbai, India) supported by providing cetyl palmitate as a gift sample. Capmul MCM and Acrsol K150 were obtained as a gift samples from Abitec Corporation Limited (Mumbai, India) and Corel Pharma Limited (Ahmedabad, India), respectively. Poloxamer 188 and Tween 80 were obtained as a gift samples from BASF Limited (Mumbai, India). All other chemicals and reagents were of analytical reagent grade and procured from SD Fine chemicals (Mumbai, India). Solvents were of HPLC grade and procured from Merck (Mumbai, India).
Methods
Screening of lipid, oil, and surfactant
Different lipids, oils, and surfactants were screened for maximum solubilization of RES by solubilization method, 5 mg of RES was transferred in a test tube containing molten lipid, and test tube was incubated at 5 °C above the melting point of lipid. Successive addition of 5 mg of lipid was done in stepwise manner until RES was completely solubilized.
The solubility of RES in surfactant and oil was estimated by solubilizing an excess quantity of RES in 2 mL of 1% aqueous solution of surfactant and neat oil, respectively. The mixtures were shaken using a hot water bath shaker maintained at 25 ± 0.5 °C for 24 h (EIE instruments Pvt. Ltd., India). After attaining equilibrium, mixtures were centrifuged at 3000 RPM (Remi, India) for 10 min. The upper layer of liquid was separated and the quantity of the RES present was determined by using HPLC (Jasco, Japan) coupled with UV detector at 306 nm [30].
Preparation of nanostructured lipid carrier
Melt emulsification-probe sonication method was used to prepare nanostructured lipid carrier as described by Patil et al. [31]. Weighed quantity of cetyl palmitate (solid lipid, melting point 54 °C), Capmul MCM (oil), and Acrysol were melted at 60 °C. Precisely weighed quantity of RES was added to the above molten mixture and vortexed (Remi, India) for 2 min. Simultaneously, surfactants (Poloxamer 188, Tween 80) were dissolved in distilled water and heated up to 60 °C. The surfactant solution was added to lipid phase to form a clear primary emulsion which was then subjected to particle size reduction using probe sonicator (Sonics and Materials, USA) at an amplitude of 30% for 2 min (pulse cycle-3:2 s on/off). The fabricated nanostructured lipid carriers were cooled to room temperature. The composition of nanostructured lipid carrier is shown in Table 1.
Characterization of nanostructured lipid carrier
Determination of particle size, polydispersity index, and zeta potential
The mean particle size, polydispersity index, and zeta potential of the formulated nanostructured lipid carriers were estimated by dynamic light scattering (DLS) principle using a zetasizer (Malvern Instruments, Malvern, UK). All the measurements were done after dispersing formulated nanostructured lipid carrier in an appropriate volume of HPLC-grade water at 25 ± 2 °C with the scattering angle of 90° [32]. All measurements were performed in triplicate.
Drug loading and entrapment efficiency
Two milliliter of nanostructured lipid carrier dispersion was centrifuged (Remi, India) at 20,000 RPM for 60 min at 4 °C. Separated upper layer of liquid was collected, filtered through 0.45-μm filter and subjected to HPLC analysis for determination of the free drug present in nanostructured lipid carrier [33]. Drug loading and entrapment efficiency were calculated by Eqs. (1) and (2), respectively (n = 3),
Incorporation of nanostructured lipid carrier into in situ gel
Gellan gum (0.5%, w/v) was dissolved in distilled water at 90 °C with continuous stirring (Remi, India). Afterwards, gellan gum solution was allowed to cool below 40 °C. On the other hand, xanthan gum (0.15%, w/v) was dissolved separately in distilled water with stirring. The RES-loaded nanostructured lipid carrier was slowly added in xanthan gum solution by stirring, and resultant solution was added to the gellan gum solution, mixed thoroughly by stirring for 15 min to obtain the final in situ gel formulation [34].
Evaluation of in situ gel
Physical appearance and pH
The appearance, color, and homogeneity of the gel were observed visually. The pH of the gel was measured by pH meter (Analab Scientific Instruments Pvt. Ltd., India) (n = 3) [31].
Gelling time
The gelling time was determined using aluminum pan method. In this, pan was placed on a water bath maintained at 32 ± 2 °C. Five drops of the solution were placed onto the pan using a micro pipette. The pan was then tilted at 90° in water bath to initiate the gel formation. Time required to convert free-flowing solution converted into a thick gel was recorded as a gelling time (n = 3) [35].
Expansion coefficient (S %)
The expansion coefficient was estimated by adding 1 mL of the formulation in 0.25 mL simulated nasal fluid (7.45 mg/mL NaCl, 1.29 mg/mL KCl, and 0.32 mg/mL CaCl2·2H2O, pH − 6.5) [36] in a 10 mL measuring cylinder. The cylinder was incubated in the water bath at 32 ± 2 °C with an initial volume of 1.25 mL (V1). The formulation was allowed to gel, and its volume was recorded (VG). Furthermore, 2 mL of simulated nasal fluid was added and the volume VT was recorded. Thus, VG = VT − 2 and expansion coefficient was calculated using Eq. 3 (n = 3) [35]:
Viscosity
Twenty-five milliliters sample was used to measure viscosity using Brookfield viscometer (Brookfield Engineering Pvt. Ltd., USA). The spindle was rotated at 10 RPM for 10 s. The measurement was done before and after gelation using spindle number 18 and 96, respectively, in triplicate [34].
Gel strength
Fifty grams of the solution was placed in a 100-mL measuring cylinder and gelled using a specific quantity of simulated nasal fluid. Then, 35 g weight was placed onto the gel surface. Gel strength was determined by measuring the time required by the weight to penetrate 3 cm inside the gel at physiological condition [37].
In vitro permeation study
Fresh nasal mucosa of sheep was collected from the local slaughter house and stored in a saline solution. Mucosal membrane was washed thrice with saline solution to remove the blood and bony cartilage and used for permeation study.
In vitro permeation study of in situ gel was conducted using multiple Franz diffusion cell (Orchid scientific, India). Sheep nasal tissue was placed onto the donor compartment of the cell with a permeation area of 4.52 cm2. The receptor compartment of the cell was filled with simulated nasal fluid (7 mL). After 20 min, 1 g of in situ gel was placed in the donor compartment. The whole system was maintained at 32 ± 0.5 °C with constant stirring at 50 RPM. At predetermined time intervals, 1 mL of a sample was withdrawn from the receptor compartment and replaced with 1 mL fresh simulated nasal fluid to maintain sink condition. Then, samples were analyzed by HPLC method to measure amount of drug [38]. Further, the cumulative amount of drug permeated across the nasal tissue, permeation coefficient, and flux was calculated.
In vivo studies
Pharmacodynamic study
Animals
Animal care and handling were carried out according to the CPCSEA guidelines throughout the study. The study protocol was approved by the Institutional Animal Ethical Committee (IP/PCEU/PHD/18/017). Male Sprague-Dawley (SD) rats weighing 200–250 g, 4–6 weeks old were kept at 25 ± 2 °C with 12 h light and dark cycle.
Drug schedule and groups
Scopolamine (SC) was used to induce amnesia in rats. All animals were divided into four groups having six animals in each group as below:
-
Normal control group
-
Group A—scopolamine-induced amnesia group (1 mg/kg) by intraperitoneal route
-
Group B—in situ gel (equivalent to 2 mg/kg body weight of RES) by intranasal route
-
Group C—resveratrol suspension (equivalent to 2 mg/kg body weight of RES) by oral route
Study protocol
The administration of scopolamine induces transient memory loss in rats. Morris Water Maze test is widely used to study spatial memory activity of the various drugs. The study was carried out as described by method described in Parle et al. [39]. The apparatus used for Morris Water Maze test (rat) consists of a circular tank (150 cm in diameter and 45 cm in height) and a platform (12 cm in diameter and 28 cm in height). Platform was made invisible to the rats, by placing it 2 cm below the water level inside the tank, and tank was maintained at 25 ± 2 °C. The position of the central platform remained unchanged throughout the experiment. The rats were trained for finding an invisible platform and rats were allowed to stay on it for 30 s. Rats which were failed to find the platform within 120 s were placed on the platform manually only in the first session. The animals were given a daily training for four times [40].
Procedure
Rats were weighed and divided into four groups (n = 6) as mentioned above. Rats were trained for four consecutive days from different starting points in the tank for finding central paltform. Study was performed on the fifth day by administering scopolamine (1 mg/kg intraperitoneal) 30 min prior to trial to the three groups (A, B, and C). Optimized in situ gel was administered 30 min before scopolamine injection through the intranasal route using micropipette to group B rats. RES suspension (equivalent to 2 mg/kg body weight of RES) was administered by an oral route to group C rats [19, 41]. After 2 h of administration of formulations, the time taken to find platform (escape latency in second), distance traveled (cm), total time spent in target quadrant(s), and number of annulus crossing in 90 s were recorded with the help of a video tracking system [42].
Statistical study
The statistical analysis was performed by a Student’s (paired) t test and one-way analysis of variance (ANOVA) followed by Tukey’s multiple comparison test using GraphPad Prism statistical software package (GraphPad software Inc. La Jolla, CA, USA, version 5.03). A probability had a value of 0.05 or less was considered as a statistically significant [43].
Results and discussion
Screening of lipid, oil, and surfactant
The solubility of RES was studied in a various short, medium, and long-chain glycerides. Cetyl palmitate depicted maximum solubility of RES, and hence, it was selected for further studies. Figure 1a shows the amount of solid lipid required to solubilize RES. Muller et al. reported that the addition of oil to the solid lipid decreases crystallinity of drug and increases drug loading by preventing its leakage from nanocarrier [44]. Figure 1b shows the amount of oil required to solubilize RES. Resveratrol showed higher solubility in Capmul MCM, and hence, it was selected as an oil for further formulation development. Capmul MCM is a mixture of caprylic and capric mono-diglyceride esters. Capmul MCM also shows bacteriostatic activity, which may help in the preservation of gel during storage [45].
Surfactants were used for emulsification and stabilization of a system. However, selected surfactants should exhibit poor drug solubility, which will promote higher drug entrapment in oil-lipid matrix. Figure 1c shows the amount of surfactants required to solubilize RES. Poloxamer 188 and Tween 80 had shown less solubility of RES, and hence, they were selected as choice of surfactants for further formulation development. Nanostructured lipid carrier was formulated using a combination of surfactants (Poloxamer 188 and Tween 80) which showed higher entrapment efficiency and drug loading than individual surfactant (data not shown). The Poloxamer 188 alone resulted in an insufficient emulsification. It also causes the drug exclusion from lipid phase to external surfactant phase [46]. Therefore, further trials were carried out using the combination of Poloxamer 188 and Tween 80.
Preparation of nanostructured lipid carrier
Nanostructured lipid carrier was prepared by melt emulsification-probe sonication method using a cetyl palmitate (lipid) and Capmul MCM (oil). During preliminary trials, lipid to oil ratio was varied from 1:1 to 1:5. Different process parameters such as amplitude (10 to 50%) and sonication time (1 to 5 min) were also studied for optimization purpose. The high amplitude (40 and 50%) for longer time (3 min) resulted in a higher particle size due to the aggregation of particles [data not shown]; this finding was strengthened by reported data [31]. Hence, 1:1 lipid to oil ratio 30% sonication amplitude for 2 min resulted in optimized nanostructured lipid carrier with particle size less than 200 nm.
Characterization of nanostructured lipid carrier
Particle size, polydispersity index, and zeta potential
Particle size, polydispersity index, and zeta potential dictate the physical stability of nanostructured lipid carrier. The results are shown in Table 2. Incorporation of Acrysol K150, a solubilizer cum stabilizer, resulted in a decreased particle size of nanostructured lipid carrier (batches R1 and R2) [47]. The increment in concentration of lipid and oil resulted into the formation of larger particles (batches R3 and R4). Reduction in particle size was observed with an increase in surfactant concentration from 100 to 150 mg (batch R5) which might be due to system stabilization. The higher drug loading makes the system economic and desirable.
Polydispersity index is used as an indicator of size uniformity. The lipid carriers are homogenous in size when polydispersity index is below 0.30 [48, 49]. The polydispersity of all batches was below 0.33 with singlet peak indicated uniform particle size distribution.
Zeta potential indicates surface charge of a particle, which plays an important role in stabilization of colloidal dispersion. The charged particles have a tendency to repel each other if the system possesses high zeta potential (positive or negative) and thus avoid aggregation of the particles. A nanocarrier system having ± 30 mV value of zeta potential is considered as stable formulation [50]. Ruktanonchai et al. has reported that, as cetyl palmitate concentration increases, zeta potential of the system increases [51]. However, slight increase in zeta potential was observed in batches R3 and R4.
Though, Tween 80 and Poloxamer 188 stabilize the particles by steric mechanism, but this has negative influence on zeta potential of the formulations [52]. Reduction in magnitude of zeta potential is either due to shift of electric double layer or due to presence of the free fatty acids impurity in the system [53, 54]. R6 batch was shown all optimal characteristics of nano structured carrier and was considered as an optimized formulation for further studies.
Drug loading and entrapment efficiency
It was observed that addition of oil (Capmul MCM) to the solid lipid (cetyl palmitate) resulted in increase in drug loading and entrapment efficiency. This phenomenon is supported by reduction in crystallinity of particles due to combination of lipid and oil, which makes nano structured lipid carrier system more superior than SLN [44, 55]. High drug loading and subsequent higher entrapment efficiency can be attributed by higher drug solubilizing power of Acrysol K150 (batches R1 and R2) [56]. Higher lipid concentration assists in higher drug accumulation in nano structured lipid carrier and reduces drug’s exclusion into external phase, eventually leading for higher entrapment efficiency (Batch R3) [15].
Moreover, with increase in the amount of oil in nanostructured lipid carrier, it was observed that the percentage of encapsulated drug was increased [57]. This finding is supported by preferential solubilization of drug in oil as compared to lipid. Capmul MCM being a monosaccharide of caprylic acid forms an unstructured matrix with many imperfections which provides larger space to incorporate more amount of drug [58, 59]. A high proportion of oil had resulted in higher entrapment efficiency by solubilizing higher amount of drug (batch R4) [60]. The increase in the oil concentration resulted in increased drug loading (Batches R5 and R6) by preventing exclusion of the drug into the surfactant phase [61]. Entrapment efficiency of nanocarrier system is also affected by lipid and surfactant concentration. The higher lipid and surfactant concentration resulted in higher entrapment efficiency as reported in batches R5 and R6. A difference in fatty acid chain lengths of lipids resulted in structural imperfections of matrices and provides extra space for entrapment of drug. Higher surfactant concentration stabilizes the formulation and also increases an incorporation of the drug into the lipid matrix of the system [62].
Incorporation of nanostructured lipid carrier into in situ gel
Various batches of blank gels (without drug) were prepared using a different gelling agents such as gellan gum, xanthan gum, Carbopol 934, Carbopol 971P, Carbopol 980, Carbopol ultrez 10, Poloxamer 188, and Poloxamer 407. Batches were also prepared using combination of gelling agents such as gellan gum with Poloxamer 407, gellan gum with Hypromellose (HPMC K4M), and gellan gum with xanthan gum. The gels were evaluated for viscosity of sol-gel formation upon addition of nasal fluid, and minimum time required for the gel formation was recorded [34, 63]. Based on positive results of screening experiments, mixture of gellan gum and xanthan gum was chosen as gelling an optimum gelling system for in situ gel formation (data not shown).
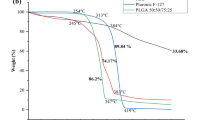
Three batches were prepared with 0.25, 0.5, and 1% w/v of gellan gum. A lower concentration of gellan gum (0.25% w/v) was not sufficient to form a gel, while the gel prepared with higher concentration (1% w/v) concentration showed high gel strength (more than 50 s) and stiffness. Hence, 0.5% w/v concentration of gellan gum and 0.15% w/v of xanthum gum were as an optimum concentration yielding transparent gel with sufficient gel strength and optimum viscosity (Fig. 2). The pH, gelling time, expansion coefficient, viscosity of gel before and after gelation, gel strength, and percentage drug permeation after 480 min of batches R1 to R6 are shown in Table 3. Acidic and alkaline pH may cause nasal irritation, and hence the pH of nasal formulation should be between 4 and 6 [64]. pH of the batches was between 4.5 and 5.8.
The gelling time depicts the time required for the formation of gel, and lesser gelling time is preferred for faster onset of drug delivery. During gelling time, gellan gum interacts with component of simulated nasal fluid (calcium, sodium, and potassium ions) which results into cross linking and formation of gel [65]. All batches have shown acceptable gelling time of 33 to 49 s.
When gellan gum solution was converted into gel, there was no substantial expansion in gel volume. An ideal expansion coefficient should be less than 3%, and such a small change in expansion volume will not impart uneasiness to patients after nasal administration of gel [35]. Batches R1 to R6 have shown lower expansion volume of less than 3%.
Viscosity of the formulation also plays important role in its easy administration. Formulation must build up its viscosity after interaction with simulated nasal fluid. In addition to that, the formed gel should preserve its integrity to facilitate the drug release for a desired time period without dissolving or eroding. Gellan gum gels quickly in the presence of ions present in simulated nasal fluid, and therefore, rapid in vivo gelation is expected [66]. A higher value of viscosity of gel form compared to sol form emphasizes effective sol-gel transformation of in situ gel system as shown in Table 3. The stability study of optimized in situ gel (R6) was conducted at 25 °C for 6 months. The particle size (136 ± 8.1 nm) and zeta potential (− 26.6 ± 2.1 mV) were determined after 6 months, which was comparable with its initial values (132 ± 11.9 nm and − 23 ± 3.79 mV). The developed in situ gel, being a liquid sol, having a low viscosity (ranging from 1.40 to 4.08 cps) and hence gellan gum and xanthan gum might not affect the particle size and zeta potential.
In vitro permeation study
In vitro permeation study shows that an optimized in situ gel (R6) has a fivefold higher permeation compared to RES-based gel after 480 min as shown in Fig. 3. The residence time of the optimized formulation in the nasal cavity is expected to be more as compared to suspension, and therefore, it resulted in higher permeation. Similar observation has been reported in earlier research [67]. Additionally, the lipophilic nature of nanostructured lipid carrier may increase uptake of the drug [68]. The aqueous fluid present into the formulation causes an increase in the interlamellar volume of the tissue and cause leakages in the membrane structure. This resulted into higher drug uptake through the tissue [69]. Furthermore, permeability coefficient and flux were calculated for the optimized in situ gel and RES suspension-based in situ gel (Table 4). Higher permeability coefficient and flux of nanostructured lipid carrier-based in situ gel signify higher permeation of the drug.
Pharmacodynamic study
Based on previously reported literature, the cognitive function of the brain is regulated by a vital neurotransmitter acetylcholine. Alzheimer’s disease is the most known cause of dementia characterized by cognitive dysfunction with memory loss and behavioral changes [70]. Morris Water Maze apparatus is very useful for spatial memory study. It is based on cues to locate a submerged escape platform from different start points. Spatial learning was determined by conducting the repetitive trials, and reference memory was determined by ability to find a platform area when the platform was absent [71]. The various parameters such as escape latency time, distance traveled, time spent in target quadrant, and numbers of annulus crossings are considered as an indicator of memory enhancement.
Scopolamine-induced Alzheimer’s is considered as a widely accepted model for cognitive deficit study. Scopolamine acts as a muscarinic acetylcholine receptor antagonist and acts by inhibiting muscarinic receptors throughout the brain. It induces a memory loss and reduces neuronal excitability by blocking the conduction neurotransmitter of the cholinergic system [43].
In acquisition training phase, the rats were trained for four consecutive days from different starting points and taught to locate the hidden platform. During training phase, all rats have shown significant reduction in escape latency time and insignificant difference in the escape latencies amongst the groups tested on the same day.
On the fifth day, rats of groups A, B, and C received a scopolamine injection before the probe trial test in order to induce memory loss. The group B and group C have received in situ gel via nasal and RES suspension via oral route respectively 30 min prior of scopolamine injection.
The escape latency time is the time taken by the rat to reach to the central platform. Insignificant difference was observed between normal control group and optimized in situ gel group (group B). The rats in normal control group showed shorter escape latency (Fig. 4a) followed by optimized in situ gel (group B) and RES suspension group (group C). Hence, it implies that, the developed formulation is more effective than RES suspension to treat AD.
Pharmacodynamic study in scopolamine-induced amnesia model in rats using Morris Water Maze test. Each data point represents the mean ± SD of six animals in each group. Statistical analysis was carried out using one-way ANOVA followed by Tukey’s multiple comparison test; values are statistically significant at *p < 0.05 vs. scopolamine-induced amnesia; #p < 0.05 vs. optimized in situ gel. Group A—scopolamine-induced amnesia. Group B—optimized in situ gel (R6). Group C—Resveratrol suspension. a Escape latency time. b Distance traveled. c Total time spent in target quadrant. d Number of annulus crossings
In case of the distance traveled by rat, no significant difference was observed between normal control and optimized in situ gel group (group B). The rats of normal control group took smaller path amongst all the three groups (Fig. 4b).
In probe trial test, the average time spent in target quadrant for each rat was calculated for comparison amongst the groups, and the results are shown in Fig. 4c. The rats treated with optimized in situ gel had better memory and could spend more time in a target quadrant compared to normal control group. However, the rats treated with RES suspension group (group C) had spent comparatively lesser time. Based on this observation, in situ gel formulation could be choice of formulation over RES suspension.
The rats of normal control group had remembered the path to reach to centrally placed platform in the tank. Hence, they have crossed the place of platform 11 times in 90 s. The optimized formulation-treated group (group B) showed similar annulus crossings (i.e., 10) (Fig. 4d). However, rats of RES suspension-treated group (group C) had crossed the place of platform only half of the time compared with the in situ gel-treated group (group B). The rats of scopolamine treated group (group A) have shown only two annulus crossings, probably due to loss of memory. Thus, the developed formulation of nanostructured lipid carrier based in situ gel has potential to treat AD after nasal administration followed by higher drug targeting into the brain.
Conclusion
Nanostructured lipid carrier drug delivery system was developed for administration of RES via nasal route for brain targeting for treatment of AD. Optimized formulation of resveratrol nanostructured lipid carrier was incorporated into an in situ gel using gellan gum and xanthan gum for easy administration and longer adhesion time. An optimized formulation was further studied using a scopolamine-induced amnesia using Morris Water Maze test in rats. The results of Morris Water Maze test emphasizes that developed nanostructured lipid carrier, after nasal administration, could effectively treat AD as compared to the orally administered RES suspension. Pharmacokinetic studies can be conducted in near future to understand the brain targeting potential of nanostructured lipid carrier via nasal route.
References
Anand R, Gill KD, Mahdi AA. Therapeutics of Alzheimer’s disease: past, present and future. Neuropharmacology. 2014;76:27–50.
Fe L, Gong Q, Dong H. Resveratrol: a neuroprotective supplement for Alzheimer’s disease. Curr Pharm Des. 2012;18(1):27–33.
Pallas M, Prouquet D, Vincete V. Resveratrol: new avenues for a natural compound in neuroprotection. Curr Pharm Des. 2013;19(38):6726–31.
Bhavna MS, Ali M. Donepezil nanosuspension intended for nose to brain targeting: in vitro and in vivo safety evaluation. Int J Biol Macromolec. 2014;67:418–25.
Laserra S, Basit A, Sozio P. Solid lipid nanoparticles loaded with lipoyl–memantine co-drug: preparation and characterization. Int J Pharm. 2015;485(1–2):183–91.
Qian S, Wong CY, Zuo Z. Development, characterization and application of in situ gel systems for intranasal delivery of tacrine. Int J Pharm. 2014;468(1–2):272–82.
Neves AR, Lucio M, Lima JL. Resveratrol in medicinal chemistry: a critical review of its pharmacokinetics, drug-delivery and membrane interactions. Curr Med Chem. 2012;19(11):1663–81.
Walle T, Hsieh F, DeLegge MH. High absorption but very low bioavailability of oral resveratrol in humans. Drug Metab Dispos. 2004;32(12):1377–82.
Vitaglione P, Sforza S, Galaverna G. Bioavailability of trans-resveratrol from red wine in humans. Mol Nutr Food Res. 2005;49(5):495–504.
Sanna V, Roggio AM, Siliani S, Piccinini M, Marceddu S, Mariani A, et al. Development of novel cationic chitosan- and anionic alginate-coated poly (D, L lactide- co-glycolide) nanoparticles for controlled release and light protection of resveratrol. Int J Nanomedicine. 2012;7:5501–16.
Mohanty C, Sahoo SK. The in vitro stability and in vivo pharmacokinetics of curcumin prepared as an aqueous nanoparticulate formulation. Biomaterials. 2010;31:6597–611.
Shaikh J, Ankola DD, Beniwal V, Singh D, Kumar MN. Nanoparticle encapsulation improves oral bioavailability of curcumin by at least 9-fold when compared to curcumin administered with piperine as absorption enhancer. Eur J Pharm Sci. 2009;37:223–30.
Oganesyan EA, Miroshnichenko I, Vikhrieva NS, Lyashenko AS, Leshkov SY. Use of nanoparticles to increase the systemic bioavailability of transresveratrol. J Pharm Chem. 2010;44:74–6.
Gokce EH, Korkmaz E, Dellera E, Sandri G, Cristina M, et al. Resveratrol-loaded solid lipid nanoparticles versus nanostructured lipid carriers: evaluation of antioxidant potential for dermal applications. Int J Nanomedicine. 2012;7:1841–50.
Jose S, Anju SS, Cinu TA. In-vivo pharmacokinetic and biodistribution of resveratrol loaded solid lipid nanoparticles for brain delivery. Int J Pharm. 2014;474(1–2):6–13.
Joraholmen MW, Basnet NS, Acharya G, Basnet P. Resveratrol-loaded liposomes for topical treatment of the vaginal inflammation and infections. Pharm Sci. 2015;79:112–21.
Lazar AN, Mourtas S, Youssef I, Parizot C, Dauphin A, Delatour B, et al. Curcumin-conjugated nanoliposomes with high affinity for Abeta deposits: possible applications to Alzheimer disease. Nanomedicine. 2013;9:712–21.
Guo W, Li A, Jia Z, Yuan Y, Dai H, Li H. Transferrin modified PEG-PLA resveratrol conjugates: in vitro and in vivo studies for glioma. Eur J Pharmacol. 2013;718:41–7.
Serralheiro A, Alves G, Fortuna A. Intranasal administration of carbamazepine to mice: a direct delivery pathway for brain targeting. Eur J Pharm Sci. 2014;60:32–9.
Hafy AS, Farid RM, Gamal SS. Complexation as an approach to entrap cationic drugs into cationic nanoparticles administered intranasally for Alzheimer’s disease management: preparation and detection in rat brain. Drug Dev Ind Pharm. 2015;41(12):1–4.
Touitou E, Illum L. Nasal drug delivery. Drug Deliv Transl Res. 2013;3(1):1–3.
Singh R, Kumar A, Pathak K. Mucoadhesive in situ nasal gelling drug delivery systems for modulated drug delivery. Expert Opin Drug Deliv. 2013;10(1):115–30.
Neves AR, Lúcio M, Martins S. Novel resveratrol nanodelivery systems based on lipid nanoparticles to enhance its oral bioavailability. Int J Nanomedicine. 2013;8:177–87.
Nguyen CN, Nguyen TT, Nguyen HT. Nanostructured lipid carriers to enhance transdermal delivery and efficacy of diclofenac. Drug Deliv Transl Res. 2017;7(5):664–73.
Muller RH, Radtke M, Wissing SA. Nanostructured lipid matrices for improved microencapsulation of drug. Int J Pharm. 2002;242(1–2):121–8.
Fang CL, Al-Suwayeh SA, Fang JY. Nanostructured lipid carriers (NLCs) for drug delivery and targeting. Recent Pat Nanotechnol. 2013;7(1):41–55.
Pardeike J, Hommoss A, Müller RH. Lipid nanoparticles (SLN, NLC) in cosmetic and pharmaceutical dermal products. Int J Pharm. 2009;366(1–2):170–84.
Khaled MH, Hassan AH. Intranasal in situ gel loaded with saquinavir mesylate nanosized microemulsion: preparation, characterization, and in vivo evaluation. Int J Pharm. 2014;475(1–2):191–7.
Lochhead JJ, Thorne RG. Intranasal delivery of biologics to the central nervous system. Adv Drug Deliv Rev. 2012;66(7):614–28.
Patel K, Padhye S, Nagarsenkar M. Duloxetine hydrochloride lipid nanoparticles: preparation, characterization and dosage form design. AAPS PharmSciTech. 2012;13(1):125–33.
Patil A, Pokharkar V. Montelukast loaded nanostructured lipid carriers: part I oral bioavailability improvement. Eur J Pharm Biopharm. 2014;88(1):160–8.
Nagpal K, Singh SK, Mishra DN. Optimization of brain targeted chitosan nanoparticles of Rivastigmine for improved efficacy and safety. Int J Biol Macromolec. 2013;59:72–83.
Rawal T, Parmar R, Tyagi R, Butani S. Rifampicin loaded chitosan nanoparticle dry powder presents: an improved therapeutic approach for alveolar tuberculosis. Colloids Surf B Biointerfaces. 2017;154:321–30.
Zeinab MA, Vangala A, Longman M. Poloxamer-based thermoresponsive ketorolac tromethamine in situ gel preparations: design, characterization, toxicity and transcorneal permeation studies. Eur J Pharm Biopharm. 2017;114:119–34.
Zheng C, Xiangrong S, Feng S. Formulation and evaluation of in situ gelling systems for intranasal administration of gastrodin. AAPS PharmSciTech. 2011;12(4):1102–9.
Martinac A, Grcić JF, Voinovich D. Development and bioadhesive properties of chitosan-ethylcellulose microspheres for nasal delivery. Int J Pharm. 2005;291(1–2):69–77.
Choi HG, Kim CK, Jung JH. Development of in situ-gelling and mucoadhesive acetaminophen liquid suppository. Int J Pharm. 1998;165(1):33–44.
Dias RJ, Mali KK, Formulation SJV. Evaluation of thermoreversible mucoadhesive nasal gels of metoclopramide hydrochloride. Lat Am J Pharm. 2010;29(3):354–61.
Parle M, Singh N. Animal models for testing memory. Asia Pac Z Pharmacol. 2004;16:101–20.
Puri A, Srivastava P, Pandey P. Scopolamine induced behavioral and biochemical modifications and protective effect of Celastrus paniculatous and Angelica glauca in rats. Int J Nutr Pharmacol Neurol Dis. 2014;4(3):158–69.
Hao J, Zhao J, Zhang S. Fabrication of an ionic-sensitive in situ gel loaded with resveratrol nanosuspension intended for direct nose-to-brain delivery. Colloids Surf B Biointerfaces. 2016;147:376–86.
Sharma D, Puri M, Tiwari A, Singh N. Antiamenic effect of stevioside in scopolamine treated rats. Indian J Pharmacol. 2010;42(3):64–7.
Patel PA, Patil SC, Kalaria DR. Comparative in vitro and in vivo evaluation of lipid based nanocarriers of Huperzine A. Int J Pharm. 2013;446(1–2):16–23.
Müller RH, Radtke M, Wissing SA. Nanostructured lipid matrices for improved microencapsulation of drugs. Int J Pharm. 2002b;242(1–2):121–8.
http://www.abitecorp.com. Accessed 10 January 2016.
Hou DZ, Xie CS, Huang KJ. The production and characteristics of solid lipid nanoparticles (SLNs). Biomaterials. 2003;24(10):1781–5.
http://www.corelpharmachem.com/acrysol.html. Accessed 20 June 2015.
Lippacher A, Muller RH, Mader K. Preparation of semisolid drug carriers for topical application based on solid lipid nanoparticles. Int J Pharm. 2001;214(1–2):9–12.
Ibrahim WM, Omrani AH, Yassin AE. Novel sulpiride-loaded solid lipid nanoparticles with enhanced intestinal permeability. Int J Nanomedicine. 2014;9:129–44.
Suthar V, Butani S, Gohel M. Solid self-emulsified nanostructures of Lercanidipine hydrochloride: a potential approach to improve the fraction of the dose absorbed. J Drug Deliv Sci Technol. 2016;31:11–21.
Ruktanonchai U, Limpakdee S, Meejoo S, Sakulkhu U, Bunyapraphatsara N, Junyaprasert V, et al. The effect of cetyl palmitate crystallinity on physical properties of gamma-oryzanol encapsulated in solid lipid nanoparticles. Nanotechnology. 2008;19(9):1–10.
Kheradmandnia S, Vasheghani-Farahani E, Nosrati M. Preparation and characterization of ketoprofen-loaded solid lipid nanoparticles made from beeswax and carnauba wax. Nanomed Nanotechnol. 2010;6(6):753–9.
https://www.researchgate.net/Zeta potential of an emulsion stabilized by non-ionic surfactants. Accessed date 27 November 2017.
Kovacevica A, Savica S, Vuleta G, Müller RH, Keckc CM. Polyhydroxy surfactants for the formulation of lipid nanoparticles (SLN and NLC): effects on size, physical stability and particle matrix structure. Int J Pharm. 2011;406:163–72.
Muller RH, Mader K, Gohla S. Solid lipid nanoparticles (SLN) for controlled drug delivery—a review of the state of the art. Eur J Pharm Biopharm. 2000;50(1):161–77.
Kumar S, Sangwan P, Lather V. Biocompatible PLGA-oil hybrid nanoparticles for high loading and controlled delivery of resveratrol. J Drug Deliv Sci Technol. 2015;30:54–62.
Li F, Wang Y, Liu Z. Formulation and characterization of bufadienolides-loaded nanostructured lipid carriers. Drug Dev Ind Pharm. 2010;36(5):508–17.
Teeranachaideekul V, Souto EB, Junyaprase VB. Cetyl palmitate-based NLC for topical delivery of coenzyme Q10—development, physicochemical characterization and in vitro release studies. Eur J Pharm Biopharm. 2007;67(1):141–8.
Souto EB, Wissding SA, Barbosa CM. Development of a controlled release formulation based on SLN and NLC for topical clotrimazole delivery. Int J Pharm. 2004;278(1):71–7.
Shah NV, Seth AK, Balaraman R. Nanostructured lipid carriers for oral bioavailability enhancement of raloxifene: design and in vivo study. J Adv Res. 2016;7(3):423–34.
Puri A, Loomis K, Smith B. Lipid based nanoparticles as pharmaceutical drug carriers: from concepts to clinic. Crit Rev Ther Drug Carrier Syst. 2009;26(6):523–80.
Khan S, Shaharyar M, Fazil M. Tacrolimus-loaded nanostructured lipid carriers for oral delivery—optimization of production and characterization. Eur J Pharm Biopharm. 2016;108:277–88.
Cao S, Ren X, Zhang Q, Chena E, Xu F, Chen J, et al. In situ gel based on gellan gum as new carrier for nasal administration of mometasone furoate. Int J Pharm. 2009;365:109–5.
Morsi N, Ghoraba D, Refaia H, Tebab H. Ketoroloac tromethamine loaded nanodispersion incorporated into thermosensitive in situ gel for prolonged ocular delivery. Int J Pharm. 2016;506(1–2):57–67.
Moritaka H, Nishanari K, Taki M. Effect of pH, potassium chloride and sodium chloride on thermal and rheological properties of gellan gum gels. J Agric Food Chem. 1995;43:1685–9.
Pathan IB, Chudiwal V, Farooqui I. Formulation design and evaluation of nasal in situ gel as a novel vehicle for Azelastine hydrochloride. Int J Drug Deliv. 2013;5(3):284–90.
Paulsson M, Hagerstrom H, Edsman K. Rheological studies of the gelation of deacetylated gellan gum (gelrite) in physiological conditions. Eur J Pharm Sci. 1999;9(1):99–105.
Kaur S, Nautyal U, Singh R, Singh S, Devi A. Nanostructure lipid carrier (NLC): the new generation of lipid nanoparticles. Asian Pac J Health Sci. 2015;2(2):76–93.
Sanjula B, Faiyaz S, Alka A. Design, development and evaluation of novel nanoemulsion formulations for transdermal potential of celecoxib. Acta Pharma. 2007;57(3):315–32.
Agrawal R, Tyagi E, Saxena G. Cholinergic influence on memory stages: a study on scopolamine amnesic mice. Indian J Pharmacol. 2009;41(4):192–6.
Vorhees CV, Williams MT. Morris water maze: procedures for assessing spatial and related forms of learning and memory. Nat Protoc. 2006;1(2):848–58.
Acknowledgements
The authors extend their gratitude to Dr. Sagar Pandya, Publication Officer, Nirma University, Ahmedabad, Dr. Ruchi Sawhney, Consultant, and Dr. Mukesh Gohel, Research Director, Anand Pharmacy College, Anand, for their suggestions in writing the manuscript. Authors also acknowledge the help extended by the Ranbaxy Research Laboratory, Mohini Organics, Gattefose, Lubrizol Corporation, BASF, C P Kelco, Signet and Cadila Healthcare by providing the gift samples of drug and excipients for research work. The authors are thankful to the Deanship of Scientific Research at Princess Nourah bint Abdulrahman University for funding this work through the Research Groups Program Grant no. (RG-1438-002).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors Shital Butani, Amarjitsing Rajput, Aditi Bariya, Ahmed Allam, and Sarah Othman declared that they have no conflict of interest. This article does not contain any studies with human performed by any of the authors.
Rights and permissions
About this article
Cite this article
Rajput, A., Bariya, A., Allam, A. et al. In situ nanostructured hydrogel of resveratrol for brain targeting: in vitro-in vivo characterization. Drug Deliv. and Transl. Res. 8, 1460–1470 (2018). https://doi.org/10.1007/s13346-018-0540-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-018-0540-6