Abstract
Background and Objectives
Piperacillin/tazobactam is extensively used off-label to treat late-onset neonatal sepsis, but safety and pharmacokinetic data in this population are limited. Additionally, the organic immaturity of the newborns contributes to a high piperacillin pharmacokinetic variability. This affects the clinical efficacy of the antibiotic treatment and increases the probability of developing drug resistance. This study aimed to evaluate the predictive performance of reported piperacillin population pharmacokinetic models for their application in a model-informed precision dosing strategy in preterm and term Mexican neonatal intensive care patients.
Methods
Published population pharmacokinetic models for piperacillin which included neonates in their study population were identified. From the reference models, structured models, population pharmacokinetic parameters, and interindividual and residual variability data were extracted to be replicated in pharmacokinetic software (NONMEM® version 7.4). For the clinical study, a sampling schedule was designed, and 2–3 blood samples of 250 µL were taken from neonates who met the inclusion criteria. Piperacillin plasma concentrations were determined by liquid chromatography/tandem mass spectrometry. The clinical treatment data were collected, and piperacillin plasma concentrations were estimated using reference pharmacokinetic models for an a priori or Bayesian approach. Statistical methods were used in terms of bias and precision to evaluate the differences between observed and estimated neonatal piperacillin plasma concentrations with the different approaches and to identify the pharmacokinetic model that best fits the neonatal data.
Results
A total of 70 plasma samples were collected from 25 neonatal patients, of which 15 were preterm neonates. The overall median value (range) postnatal age, gestational age, body weight, and serum creatinine at the sampling collecting day were 12 (3–26) days, 34.2 (26–41.1) weeks, 1.78 (0.08–3.90) Kg, 0.47 (0.20–0.90) mg/dL, respectively. Three population pharmacokinetic models for piperacillin in infants up to 2 months were identified, and their predictive performance in neonatal data was evaluated. No pharmacokinetic model was suitable for our population using an a priori approach.
The model published by Cohen-Wolkowiez et al. in 2014 with a Bayesian approach showed the best performance of the pharmacokinetic models evaluated in our neonatal data. The procedure requires two blood samples (predose and postdose), and, when applied, it predicted 66.6% of the observations with a relative median absolute predicted error of less than 30%.
Conclusions
The population pharmacokinetic model developed by Cohen-Wolkowiez et al. in 2014 demonstrated superior performance in predicting the plasma concentration of piperacillin in preterm and term Mexican neonatal intensive care patients. The Bayesian approach, including two different piperacillin plasma concentrations, was clinically acceptable regarding bias and precision. Its application for model-informed precision dosing can be an option to optimize the piperacillin dosage in our population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Piperacillin-tazobactam, an extended-spectrum antibiotic lacking FDA approval for neonatal use, is extensively employed in Neonatal Intensive Care Units (NICU) |
The current study demonstrated the process of evaluating a population pharmacokinetic model and pharmacokinetic approaches (a priori and Bayesian) to assess their potential for use in model-informed precision dosing for tailoring treatment in the neonatal population |
The population pharmacokinetic model published by Cohen-Wolkowiez et al. 2014 shows the best prediction capacity with a Bayesian forecasting approach in our study population and offers an option that could be used for model-informed precision dosing |
1 Introduction
Neonatal sepsis is a major contributor to neonatal morbidity and mortality worldwide and poses a significant public health challenge [1]. Antibiotic management in newborns is challenging because it can be difficult to accurately diagnose the infection and isolate the specific bacteria causing it. Additionally, determining the appropriate dosage of antibiotics to treat the infection effectively can be complicated. Furthermore, some antibiotics used in this population may not be officially approved for this use[2, 3]. Unfortunately, the number of multidrug-resistant microorganisms has been increasing in NICU, making clear the necessity to require appropriate treatment regimens for this population [4,5,6,7].
Piperacillin-tazobactam is a commonly prescribed extended-spectrum antibiotic with U.S. Food and Drug Administration (FDA)-approved indications for complicated appendicitis, peritonitis, and nosocomial pneumonia treatments in children 2 months or older [8]. An injectable combination of piperacillin-tazobactam is extensively and empirically used for severe intra-abdominal infection and late-onset sepsis treatment in neonates [9,10,11]. The pharmacokinetic–pharmacodynamic objective for evaluating antimicrobial therapy was defined in terms of piperacillin plasma concentrations, which exhibit time-dependent bactericidal activity. Therefore, dosing recommendations are made in terms of piperacillin dosage, considering that the antibiotic was used concurrently with tazobactam. The most common proportion used in commercial presentations is an 8:1 ratio of piperacillin-tazobactam [12, 13]. Both piperacillin and tazobactam have a low plasma protein binding, approximately 20–30%, and are primarily eliminated by the kidneys through glomerular filtration, and tubular secretion [14, 15]. Evidence in infants of age < 2 months indicates an association between piperacillin-tazobactam plasma concentrations and body weight, postmenstrual age, postnatal age, and serum creatinine levels [16,17,18]. The recommended dosage regimens of piperacillin-tazobactam for neonatal patients in fast-track clinical decision support bases and guidelines like Neofax and The Pediatric & Neonatal Dosage Handbook are based on limited population pharmacokinetic and clinical studies conducted in infants [19, 20].
A few studies regarding the use of piperacillin-tazobactam in neonates have been published [10, 21,22,23,24,25], and the results have indicated that piperacillin-tazobactam was safe and well-tolerated in the neonatal population. However, only three studies analyzed the efficacy of the antimicrobial therapy of the monotherapy of piperacillin-tazobactam [10, 24, 25]. Berger et al. [10] reported that 37% (10/27 patients) of the patients had an unfavorable clinical response, which was partly due to the very low birth weight of the patients and the characteristics of severe infection, in contrast to Tewari et al. [24] and Wu et al. [25] who reported treatment failure in only 2.1% (2/94 patients) and 16% (8/49 patients), respectively. Additionally, a recent study utilized physiological-based pharmacokinetic modeling to examine the pharmacokinetics of piperacillin-tazobactam in preterm and term neonates, and concluded that more information was needed in terms of the plasma protein binding and solubility of piperacillin-tazobactam into tissues in neonates, particularly preterm neonates [26]. These studies suggested that further research is necessary to understand how a disease can modify the pharmacokinetic parameters of piperacillin-tazobactam in neonates.
Model-informed precision dosing (MIPD) offers personalized antimicrobial treatment based on clinical and demographic variables associated with pharmacokinetic parameters in previous studies. For this purpose, an external evaluation of population pharmacokinetic models before their use for individualization of drug therapy is especially important. The external evaluation of the population pharmacokinetic models allows us to select the most adapted model for our population [27,28,29]. This study aimed to evaluate the predictive performance of reported population pharmacokinetic models for piperacillin in neonates using clinical data collected for preterm and term Mexican NICU patients to identify a suitable population pharmacokinetic model that could be used for MIPD of piperacillin-tazobactam in these patients.
2 Patients and Methods
2.1 Population Pharmacokinetic Models Literature Review
A literature review was conducted to identify piperacillin population pharmacokinetic models which include neonates in the study population using the search terms “piperacillin”, “tazobactam”, “neonates”, “pharmacokinetics”, in PubMed to retrieve articles published from January 2000 to June 2023. Studies were included if they described (1) a population pharmacokinetic model of piperacillin, (2) from neonatal data, and (3) provided sufficient information of the population pharmacokinetic model structure and typical values of pharmacokinetic parameters to reproduce the population pharmacokinetic model.
2.2 Patients and Data Collection
A prospective observational study was conducted at the NICU, Department of Pediatrics, Hospital Central “Dr. Ignacio Morones Prieto” in San Luis Potosi, Mexico. It was approved by the Research Ethics Committee at the Hospital (Register number 36-20) and carried out in concordance with the principles of the Declaration of Helsinki. Data were collected in the period from January 2021 to November 2023. Written informed consent was obtained from each patient's parents or legal guardians before collecting and analyzing blood samples. Patients with the following characteristics were included: postnatal age ≤ 29 days, body weight ≥ 850 g, and hematocrit ≥ 30%. Preterm and term neonates admitted to the NICU and treated with piperacillin-tazobactam were included in the study. Clinical and laboratory information was collected from medical records, and the serum creatinine level of the sampling day was used to calculate the creatinine clearance (CLCR) based on the Schwartz formula [30]:
where k was set to 0.45 for term neonates and 0.33 for preterm neonates.
Intravenous doses of piperacillin-tazobactam of 100 mg/Kg were administered to each neonate by intermittent infusion for 0.5 or 1 h every 8 or 12 h depending on the postmenstrual and postnatal age by Neofax® recommendations. Blood samples (2 or 3 samples depending on the clinical status of the neonate) were collected into EDTA (ethylenediaminetetraacetic acid) BD Microtainer® blood collection tubes, taking a sample volume of 250 µL of venous blood. Samples were collected and processed according to standardized procedures to ensure sample stability. Transport of the samples was meticulously controlled to prevent any deviations in temperature or other environmental factors that could affect sample integrity. After centrifuging at 11,000 rpm for 15 min, the plasma was separated and stored at – 80 °C until processing for quantification by ultra-high performance liquid chromatography with tandem mass spectrometry (UPLC-MS/MS). Notably, to ensure sample stability, no more than 30 days elapsed between the collection and analysis days.
2.2.1 Bioanalytical Assay
The piperacillin in plasma quantification was conducted using a validated UPLC-MS/MS spectrometry method reported by Rodriguez-Baez et al [31]. Chromatographic separation was obtained in a Waters Acquity HSS T3 column (100 Å, 1.8 µm, 2.1 × 100 mm) kept at 35 °C. The sample manager cooling unit was set at 10 °C. The mobile phase consisting of 0.1% formic acid solution and acetonitrile, with an elution gradient starting at a flow rate of 0.2 mL/min. The gradient program was as follows: 0–2 min: 72% A; 2–3.6 min: linear decrease to reach 30% A; 3.6–4 min: 30% A; 4–4.3 min: linear reduction to 15% A; 4.3–4.75 min: 15% A; 4.75-5 min: linear return to initial conditions; finally, 1.5 min for column re-equilibration.
The piperacillin working range was 0.65–100 µg/mL, and quality control levels were 4 µg/mL, 20 µg/mL, and 80 µg/mL. The sample volume was 5 µL and the internal standard was dicloxacillin. For the sample preparation, a volume of 100 µL of dicloxacillin-acetonitrile 10 µg/mL solution was added to 50 µL of plasma, and the obtained mixture was centrifuged at 14,000 rpm for 20 min at 4 °C. Later, 100 µL of the supernatant were centrifugated for 10 min. Finally, 50 µL of the supernatant were diluted with water (1:1 proportion) and injected into the UPLC-MS/MS system for the analyses.
The analytical method was validated according to applicable U.S. FDA guidance for bioanalysis, and presented appropriate values of measures of linearity, accuracy, precision, and recovery over the whole range of quantification. Samples with piperacillin plasma concentrations that exceeded the upper limit of quantification (ULOQ) were diluted to bring the concentrations within the quantifiable range. For this purpose, a dilution with a 1:2 proportion was performed by mixing 50 µL of the processed sample with 100 µL of blank plasma. The mixture was vortexed for 30 s to ensure homogeneity. The dilution was conducted at room temperature, after which the samples were subjected to the processing procedures. To validate the integrity of the dilution quality control samples above the ULOQ were diluted following the same procedure.
2.2.2 Antibiotic Treatment Evaluation
Clinical data concerning the evaluation of antibiotic treatment were collected during and after piperacillin-tazobactam therapy. The data collected included previous antibiotic treatment schemes, blood culture results, indication for starting the antibiotic treatment, duration of antibiotic treatment, concomitant medication, length of hospitalization, obvious adverse events, necessity to change antibiotic therapy, and recurrence of the infection. The obvious adverse events were focused on what was feasible to detect in the routine medical evaluation: diarrhea, vomiting, hypersensitivity reactions, and rash, based on the piperacillin-tazobactam U.S. FDA product label [15]. The definition of recurrent infection is a relapse occurring within 72 h of completing piperacillin-tazobactam treatment, necessitating further antibiotic therapy.
2.2.3 Sampling Strategy
A blood sampling schedule using a limited sampling strategy was developed. First, potential sampling times used in previous pharmacokinetic studies involving neonates were selected to design various sampling schedules based on practical considerations and were evaluated. The practical considerations were the need for up to 3 blood samples and recommended large sample windows. For the latter, a virtual population of 100 neonates was simulated using the population pharmacokinetic model and the characteristics distribution derived from the study by Li et al. [17]. The simulations were developed using the non-linear mixed-effects modeling software package, NONMEM® (version 7.4). Plasma piperacillin concentrations at different times after dose were simulated for each of the 100 subjects, along the dosing interval (τ) up to 12 h. The interindividual variabilities for piperacillin clearance and volume of distribution were 0.0320 and 0.0432, respectively, these values being calculated from the square of the variability coefficient reported for each pharmacokinetic parameter in the reference study. The value of sigma in the simulation corresponds to squaring the decimal value of the variability coefficient reported for the residual error in the reference population pharmacokinetic model. The designed sampling windows include times that estimate the pharmacokinetic parameters reported in the reference model with a 95% confidence interval. Two sampling schedules for a 0.5-h infusion with at least 3 blood samples were designed:
Dosing interval of 8 h: the first blood sample (A) between 0.5 and 3 h, the second blood sample (B) between 4 and 6 h, and the last blood sample (C) between 6 and 8 h after the last dose.
Dosing interval of 12 h: the first blood sample (A) between 0.5 and 3 h, the second blood sample (B) between 4 and 8 h, and the last blood sample (C) between 8 and 12 h after the last dose.
2.3 Model Evaluation for a priori Dosing
The a priori prediction performance of the population pharmacokinetic models identified during the literature review was evaluated in the neonatal population. In this approach, the piperacillin plasma concentrations were estimated using only the patient's characteristics. All the simulations were carried out using NONMEM®. Control files were created considering the model structure and parameter values from the literature population pharmacokinetic models. Demographic, clinical, and dosing information were used from the NICU patients included in the current study. This information was used to predict the piperacillin plasma concentrations at the same time as the observed piperacillin concentrations for each patient. The predicted piperacillin plasma concentrations with each literature population pharmacokinetic model were compared with the observed concentrations in the neonatal population. The bias and precision of the model predictions were evaluated based on the relative prediction error percentage (rPE), relative mean prediction error percentage (rMPE), relative median absolute prediction error percentage (rMAPE), and relative root mean squared error (rRMSE):
where PRED and OBS represent the predicted and observed piperacillin plasma concentrations, respectively. In these equations, '\(n\)' represents the total number of observations, and '\(i\)' represents the index of each observation in the dataset. The model prediction performance was clinically acceptable when their rMPE value was ± 20% and their rMAPE value was less than 30% [28].
2.4 Model Evaluation for Bayesian Dosing
Bayesian dosing by including different number of piperacillin plasma concentrations measured was performed to evaluate their applicability in piperacillin MIPD for neonates. In this case, the individual pharmacokinetic parameters, which were estimated using 1, 2, or 3 piperacillin plasma concentrations observed in the patient at different time windows (A, B, C), were used to predict the piperacillin plasma concentrations. The Bayesian forecasting of the literature models was evaluated by comparing the individual predicted (iPRED) to the observed piperacillin plasma concentrations. The relative individual prediction error percentage (riPE) was calculated. The parameters used to evaluate the Bayesian forecasting were relative mean individual prediction error percentage (rMiPE), and relative median absolute individual prediction error percentage (rMAiPE):
Values of rMiPE between − 20% and 20% and of rMAiPE less than 30% were considered clinically acceptable. The proportion of observations with a rMAiPE less than 30% (f30) was calculated to compare the Bayesian performance of the different literature population pharmacokinetic models evaluated [28].
3 Results
3.1 Study Population
A total of 70 samples were collected from 25 neonates enrolled in the study. Of these neonates, 15 were preterm, of whom one was extremely preterm with a gestational age of less than 28 weeks. The median (range) body weight, postnatal age, postmenstrual age, and serum creatinine levels at the sampling collection day were 1.81 (0.89–3.57) Kg, 14.0 (6.0–27.0) days, 35.3 (28.1–43.3) weeks, and 0.47 (0.20–0.90) mg/dL, respectively. A median of three (2–3) blood samples were collected from each patient. Necrotizing enterocolitis was the most common clinical indication for the use of piperacillin-tazobactam treatment in the study population (13/25). According to the modified Bell's criteria for necrotizing enterocolitis diagnosing, we found that 47% (6 neonates) of the cases in the study population were classified as stage IA, 23% (3 neonates) were stage IB, 15% (2 neonates) were stage IIA, and 15% (2 neonates) were stage IIIB [32]. On average, the patients received at least one course of antibiotics before starting the piperacillin-tazobactam regimen. Only six patients had positive blood cultures, three of whom required a change in antibiotic therapy due to the presence of a blood culture isolate that was either not susceptible to piperacillin or showed resistance to β-lactam antibiotics. The mean duration of the antibiotic treatment was 6.4 days. The piperacillin infusion rates used in our population varied between 0.5 and 1.5 mL/h. Among 25 patients, 10 (40%) had an infusion rate of 0.5 mL/h, 14 (56%) had an infusion rate of 1 mL/h, and just 1 neonate had an infusion rate of 1.5 mL/h. No obvious adverse events related to the use of piperacillin-tazobactam were found in the neonates. After finishing treatment with piperacillin-tazobactam, the infection recurred in one newborn within 72 h and presented an extended-spectrum β-lactamase positive bacteria blood culture isolate. The clinical and demographic characteristics of the neonates are shown in Table 1.
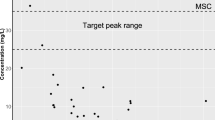
Using the sampling strategy adopted, which includes three sampling occasions (A/B/C) at different times: A (0.5–3 h after last dose), B (4–6 h after last dose for τ = 8, and 4–8 h after last dose for τ = 12 h), and C (6–8 h after last dose for τ = 8, and 8–12 h after last dose for τ = 12 h), piperacillin plasma concentrations ranged from 5.7 to 302.6 µg/mL. The piperacillin concentrations versus time after last dose observed in the neonates are presented in Fig. 1.
3.2 Literature Review on Population Pharmacokinetic Models
The PubMed search resulted in 19 articles, of which 16 were excluded due to the predefined criteria. Three population pharmacokinetic models were included, and no additional relevant publications were found in the references of the selected articles [16,17,18]. All the population pharmacokinetic models selected provided sufficient information to enable replication for dose individualization using MIPD techniques. The covariates included in the published final piperacillin population pharmacokinetic models were body weight, serum creatinine levels, postnatal age, and postmenstrual age for the clearance, and body weight for the volume of distribution. The population pharmacokinetic model’s structures and their median covariable values are described in Table 2. All the identified population pharmacokinetic models included preterm and term neonates, and their median postnatal age was less than 29 days. The dosing strategies used in the identified pharmacokinetic studies differ from those applied in the present study. HPLC-MS/MS was used to quantify the piperacillin plasma levels in the three studies. The characteristics of the pharmacokinetic population studies compared with the current study are provided in Supplementary Table S1.
3.3 External Evaluation of Population Pharmacokinetic Models
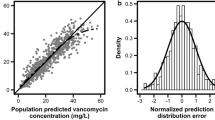
The published population pharmacokinetic models were evaluated for bias and precision using rMPE, rMAPE, and rRMSE, also using a population-level pharmacokinetic parameters (a priori) approach for their possible application in MIPD. The distribution of the rPE for each piperacillin plasma concentration predicted by the different population pharmacokinetic models is presented in Fig. 2. Based on these evaluation metrics, the models by Cohen-Wolkowiez et al. [16, 18] showed a better predictive performance than the model reported by Li et al. [17]. None of the tested models meet the acceptance criteria for rMPE ± 20%, and rMAPE < 30%. The predictive performance of the three population pharmacokinetic models is presented in Table 3.
Evaluation of a priori predictive performance of piperacillin population pharmacokinetic models applied in neonates using relative prediction error (RPE); black circles represent the RPE in percentage units for each observation of piperacillin plasma concentration in this study; horizontal line the relative mean prediction error
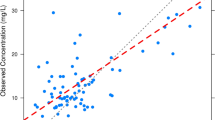
Bayesian forecasting was performed for all the population pharmacokinetic models using different times and numbers of samples to predict the piperacillin plasma concentrations in the neonatal data with individualized dosing purposes. The sampling schemes were shaped for one, two, or three blood samples at different time windows (A, B, C) throughout the dosing interval. Quantitative measures of bias and precision are shown in Table 4. The predictive performance of all the population pharmacokinetic models in terms of riPE and rAiPE is shown in Fig. 3. The observed versus predicted piperacillin plasma concentrations for the evaluated models using the neonatal data are presented in Supplementary Figs. S1–S3. In addition to the rMiPE and rMAiPE, the proportion f30 was used to evaluate the individual predictive performance of the population pharmacokinetic models, and nthe values obtained are presented in Fig. 4.
Predicted Bayesian performance of population piperacillin pharmacokinetic models applied to neonatal clinical data. The performance was evaluated with the relative individual prediction error (riPE) and the relative absolute individual prediction error (rAiPE). Different numbers of samples at different time points were provided for the neonate's piperacillin plasma concentrations estimation: A (one post-dose sample taken between 0.5–3 h after last dose), B (one sample taken between 4 and 6 h after last dose for τ = 8, and between 4 and 8 h after last dose for τ = 12 h), C (one pre-dose sample taken between 6 and 8 h after last dose for τ = 8, and between 8-12 h after last dose for τ = 12 h). Black triangles (vertical bars) represent the mean (range) of the relative individual prediction errors (riPE), and closed circles (vertical bars) represent the median (interquartile range) of the relative absolute individual prediction errors (rAiPE);e dashed lines clinically acceptable values ± 20% for riPE and 30% for rAiPE
Percentage of piperacillin plasma concentrations predicted with clinically acceptable values of relative absolute individual prediction error (rAIPE). The colors and patrons at the columns represent a different population pharmacokinetic model applied to estimate the piperacillin concentrations. The letters indicate the different sampling times applied: A (0.5–3 h after last dose), B (4–6 h after last dose for τ = 8, and 4–8 h after last dose for τ = 12 h), and C (6–8 h after last dose for τ = 8, and 8–12 h after last dose for τ = 12 h), where τ = dosing interval
The results of the bias and precision evaluation demonstrated that the inclusion of one or two piperacillin plasma concentrations can improve the predictive capacity of almost all the population pharmacokinetic models. The population pharmacokinetic model developed by Li et al. [17] did not exhibit a better fit with the neonatal data, regardless of the number of piperacillin plasma concentrations provided for the prediction. The population pharmacokinetic models of Cohen-Wolkowiez et al. [16, 18] presented an improvement in their bias and precision evaluation parameters including one piperacillin plasma concentration at time B or two piperacillin plasma concentrations at times B and C. The rMiPE and rMAiPE obtained by the Cohen-Wolkowiez et al. [16] population pharmacokinetic model were acceptable in some cases with the use of one or two piperacillin plasma concentrations, but their f30 proportion was less than 50%. Moreover, the individual predictability of the Cohen-Wolkowiez et al. [18] population pharmacokinetic model with two samples at times A and C presented an acceptable threshold of rMiPE, rMAiPE, and f30 values of 20.55%, 21.61%, and 66.6%, respectively. Although the rMiPE value was marginal, the graphical evaluation of observed versus predicted piperacillin plasma concentrations was considered acceptable.
The most accurate predictive results were obtained using the Cohen-Wolkowiez et al., [18] population pharmacokinetic model and the three piperacillin plasma concentrations, which presented the smallest value of rMAiPE with a f30 proportion of 98%.
4 Discussion
Piperacillin-tazobactam has been used extensively in the NICU to treat late-onset sepsis, nosocomial infections, and intra-abdominal complicated infections like necrotizing enterocolitis, although safety and pharmacokinetic data in this population are limited to a few studies. Recently, the piperacillin-tazobactam effectivity and safety in neonatal and infant populations has started to be evaluated by the application of previously published pharmacokinetic information [25, 33, 34]. It is important to mention that tazobactam plasma concentrations are not measured to make dosage adjustments in clinical practice because piperacillin-tazobactam dosing recommendations and antimicrobial therapy evaluations are made in terms of piperacillin. Additionally, tazobactam is not available for individual acquisition for individual administration in case dose adjustment is needed.
In this study, one preterm newborn with a very low birth weight experienced a reoccurrence of infection caused by a β-lactam-resistant bacteria within 72 h of stopping the piperacillin-tazobactam treatment. This patient had a piperacillin plasma concentration of 218 µg/mL 2 h after starting the intravenous infusion, which is higher than the median value reported in previous studies for infants with a postnatal age of less than 2 months. [16,17,18]. A relationship between piperacillin exposure and induced bacterial resistance has not been reported in neonates.
An association between total piperacillin exposure and the development of acute kidney injury in critically ill children and young adults has been reported [35]. The nephrotoxicity induced by piperacillin principally results from the competitive inhibition of organic anion transporters (OAT) 1 and 3, which are responsible for tubular creatinine secretion [36]. The toxicity threshold for piperacillin plasma concentrations is undefined, and only a few studies have been conducted to evaluate the safety of piperacillin-tazobactam in neonates [10, 22, 33, 34]. In the present study, 60% (15/25) of the neonates who received piperacillin-tazobactam treatment were premature, and no obvious adverse events were reported. In addition, none of the patients developed kidney failure. These results are consistent with the previous studies mentioned, where no adverse effects or clinically relevant changes in laboratory parameters have been found [10, 22, 33, 34].
All the piperacillin population pharmacokinetic models identified included preterm and full-term neonates. Two population pharmacokinetic models used a 1-compartment population pharmacokinetic model, while one model, by Li et al. [17], used a 2-compartment model. Our population showed a better fit with the 1-compartment models, which could be attributed to the number of samples obtained from each patient.
The study evaluated the performance of population pharmacokinetic models for individualizing piperacillin dosing based on patients' clinical and demographic characteristics. However, none of the population pharmacokinetic models were found appropriate for this a priori approach in the population studied. This may be because the a priori approach assumes that the population used to develop the population pharmacokinetic model and their drug administration characteristics are exactly the same as the one used for estimations. The study population differed in demographic and clinical characteristics, piperacillin-tazobactam administration schemes, and posology from populations in published pharmacokinetics studies. The studies by Li et al.[17] and Cohen–Wolkowiez et al.[18] report similar mean gestational and postmenstrual ages to our study, whereas the study conducted by Cohen-Wolkowiez et al.[16] included only premature neonates and infants. Additionally, the articles by Cohen-Wolkowiez et al.[18] and Li et al.[17] do not provide the proportion of term and preterm neonates included in the studies. The postnatal age and serum creatinine values observed in the three studies (0.2–2.4 mg/dL) are wider than those in our study population (0.2–0.9 mg/dL). Other variables, such as birth weight and APGAR score, which could give more information about the maturation of the neonates, were not mentioned in the studies evaluated.
The population pharmacokinetic model that performs best for our population was from Cohen-Wolkowiez et al.[18], because it presented the lowest rMiPE and rMAiPE, and consequently the higher proportion f30, indicating that the bias and precision of the model were clinically acceptable for predicting piperacillin plasma concentrations, taking into account the body weight and postmenstrual age of the newborn and using three piperacillin plasma concentrations. However, this method was not suitable for MIPD due to the impracticality of drawing three blood samples from a neonate during a dosing interval in clinical practice. The alternative to taking two blood samples at the windows times A and C for the Bayesian estimation could be an option for precision dosing in the neonate population. If only one blood sample can be obtained for the piperacillin dosing individualization, for the clinical status of the neonate, the same population pharmacokinetic model with one sample at the window time B can be an option for the MIPD. However, this approach should be used with caution since the rMiPE bias observed was 5% higher than the clinically acceptable threshold.
Only one of the three identified population pharmacokinetic models, published by Cohen-Wolkowiez et al. [16] in 2012, includes serum creatinine levels as a covariate. The elimination of piperacillin-tazobactam is mainly renal and depends on tubular secretion and glomerular filtration, and these mechanisms are very variable in the neonatal population [37,38,39,40]. Therefore, including a covariate in the population pharmacokinetic model to describe this variability can improve its performance. Maturation covariates such as gestational and postmenstrual age can reflect renal maturation in the neonatal population. The model published by Cohen-Wolkowiez et al.[18] in 2014, was the only one that included postmenstrual age as a covariate and exhibited the best fit with the neonatal data obtained in this study. This model does not include between-subject variability in the volume of distribution of piperacillin and instead presents the best fit with our data. This could be explained by the significant influence that piperacillin clearance has on its plasma levels compared to its volume of distribution in our population. This behavior is expected because piperacillin is primarily eliminated by the kidney. It has been reported that the maturational physiological changes are most prominent in early infancy, which is reflected in the large variability reported in serum creatinine in neonates in their first days of life [41].
The high variability of piperacillin plasma concentration in neonatal patients highlighted the need for individualized piperacillin-tazobactam treatment, aligning with previous studies.[16,17,18, 25]. MIPD can be a useful tool to improve the pharmacotherapy of neonates using piperacillin-tazobactam. Although monitoring piperacillin plasma levels is not considered mandatory, the probability of causing neurotoxicity or nephrotoxicity when serum concentrations are too high, the off-label use and the large interindividual variability observed in critically ill neonates make the drug monitoring for individualized antibiotic therapy important [42]. Micro-sampling procedures, and high-performance bioanalytical techniques, and population pharmacokinetic approaches, can enable individualized dosing in this vulnerable population. Despite limited sampling volumes in neonates, the methods mentioned in this study can help optimize drug therapy in the neonatal population. The present study can aid in evaluating and selecting a population pharmacokinetic model appropriate for a neonatal intensive care population and explore its potential to be used for MIPD. It is important to make an external evaluation of the published models before using them for individualization of therapeutic treatment [26]. Future studies should be made to evaluate the feasibility and measure the impact of applying MIPD in a NICU.
The study had a few limitations. Differences were found between the time the antibiotic was scheduled and the time it was administered, but, in these cases, the exact time of the monitored dose was used for the pharmacokinetic evaluation. The body weight measurements for neonates were filled using the most recent body weight value (no more than 2 days before) of the same subject if a body weight value was not available on the day of piperacillin level sampling. On the other hand, we observed variability among healthcare personnel in determining the infusion rate to administer piperacillin-tazobactam. The results obtained in this evaluation are specific to the population studied in this particular center.
5 Conclusions
The population pharmacokinetic model by Cohen-Wolkowiez et al. [18], which includes body weight and postmenstrual age as covariates to describe piperacillin clearance, and body weight to describe the volume of distribution of piperacillin, shows the best performance in predicting the plasma concentration of piperacillin in preterm and term Mexican NICU patients. This population pharmacokinetic model does not satisfy the acceptability criteria for the a priori approach, but it demonstrates good performance for the Bayesian approximation in terms of bias and precision for our study data. The Bayesian strategy includes two different piperacillin plasma concentrations measured at the window times A (0.5-3 h after last dose) and C (6-8 h after last dose for τ = 8, and 8-12 h after last dose for τ = 12 h). MIPD can be a usable tool for individualized pharmacotherapy in vulnerable populations like neonates, combining a micro-sampling strategy, high-performance bioanalytical techniques, and population pharmacokinetic approaches.
References
Dong Y, Speer CP. Late-onset neonatal sepsis: Recent developments c. 2015;100:257–63. https://doi.org/10.1136/archdischild-2014-306213.
Williams PCM, Bradley J, Roilides E, Olson L, Kaplan S, Lutsar I, et al. Harmonising regulatory approval for antibiotics in children. Lancet Child Adolesc Health. 2021;5:96–8. https://doi.org/10.1016/S2352-4642(20)30365-5.
Williams P, Qazi S, Agarwal R, Velaphi S, Bielicki J, Nambiar S, et al. Antibiotics needed to treat multidrug-resistant infections in neonates. Bull World Health Organ. 2022;100:797–807. https://doi.org/10.2471/BLT.22.288623.
Mundal HS, Rønnestad A, Klingenberg C, Stensvold HJ, Størdal K. Antibiotic use in term and near-term newborns. Pediatrics. 2021;148: e2021051339. https://doi.org/10.1542/peds.2021-051339.
Russell NJ, Stöhr W, Plakkal N, Cook A, Berkley JA, Adhisivam B, et al. Patterns of antibiotic use, pathogens, and prediction of mortality in hospitalized neonates and young infants with sepsis: a global neonatal sepsis observational cohort study (NeoOBS). PLoS Med. 2023;20: e1004179. https://doi.org/10.1371/journal.pmed.1004179.
Graus JM, Herbozo C, Hernandez R, Pantoja AF, Zegarra J. Managing antibiotics wisely in a neonatal intensive care unit in a low resource setting. J Perinatol. 2022;42:965–70. https://doi.org/10.1038/s41372-022-01388-4.
Rallis D, Giapros V, Serbis A, Kosmeri C, Baltogianni M. Fighting antimicrobial resistance in neonatal intensive care units: rational use of antibiotics in neonatal sepsis. Antibiotics. 2023;12:508. https://doi.org/10.3390/antibiotics12030508.
Food and Drug Administration (FDA). Prescribing information: ZOZYN® (piperacillin and Tazobactam) for injection, for intravenous use. www.fda.gov/medwatch.
Suryawanshi S, Pandit V, Suryawanshi P, Panditrao A. Antibiotic prescribing pattern in a tertiary level neonatal intensive care unit. J Clin Diagn Res. 2015;9:21–4. https://doi.org/10.7860/JCDR/2015/14764.6807.
Berger A, Kretzer V, Apfalter P, Rohrmeister K, Zaknun D, Pollak A. Safety evaluation of piperacillin/tazobactam in very low birth weight infants. J Chemother. 2004;16:166–71. https://doi.org/10.1179/joc.2004.16.2.166.
Wolf MF, Simon A. The use of piperacillin–tazobactam in neonatal and paediatric patients. Expert Opin Drug Metab Toxicol. 2009;5:57–69. https://doi.org/10.1517/17425250802614688.
Pfizer Inc. ZOSYN® [package insert]. Philadelphia, PA, 2016. http://www.accessdata.fda.gov/drugsatfda_docs/label/2016/050684s084s086,050750s034s035lbl.pdf.
Perry CM, Markham A. Piperacillin/Tazobactam: an updated review of its use in the treatment of bacterial infections. Drugs. 1999;57:805–43. https://doi.org/10.2165/00003495-199957050-00017.
Sörgel F, Kinzig M. The chemistry, pharmacokinetics and tissue distribution of piperacillin/tazobactam. J Antimicrob Chemother. 1993;31:39–60. https://doi.org/10.1093/jac/31.suppl_A.39.
Wyeth Pharmaceuticals Inc. PIPRACIL® (piperacillin for injection) for intravenous and intramuscular use. dailymed. 2007. https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=fac0c875-111e-4af2-d186-ed4d4ee9de59&type=display#s2.
Cohen-Wolkowiez M, Benjamin DK, Ross A, James LP, Sullivan JE, Walsh MC, et al. Population pharmacokinetics of piperacillin using scavenged samples from preterm infants. Ther Drug Monit. 2012;34:312–9. https://doi.org/10.1097/FTD.0b013e3182587665.
Li Z, Chen Y, Li Q, Cao D, Shi W, Cao Y, et al. Population pharmacokinetics of piperacillin/tazobactam in neonates and young infants. Eur J Clin Pharmacol. 2013;69:1223–33. https://doi.org/10.1007/s00228-012-1413-4.
Cohen-Wolkowiez M, Watt KM, Zhou C, Bloom BT, Poindexter B, Castro L, et al. Developmental pharmacokinetics of piperacillin and tazobactam using plasma and dried blood spots from infants. Antimicrob Agents Chemother. 2014;58:2856–65. https://doi.org/10.1128/AAC.02139-13.
Thomson Reuters clinical editorial staff. Neofax. Micromedexs, 2020.
Taketomo CK. Pediatric & Neonatal Dosage Handbook. 23rd ed. USA: Lexi-Comp; 2017.
Pillay T, Pillay D, Adhikari M, Sturm A. Piperacillin/Tazobactam in the Treatment of Klebsiella Pneumoniae Infections in Neonates. Am J Perinatol. 1998;15:47–51. https://doi.org/10.1055/s-2007-993898.
Flidel-Rimon O, Friedman S, Leibovitz E, Shinwell ES. The use of piperacillin/tazobactam (in association with amikacin) in neonatal sepsis: efficacy and safety data. Scand J Infect Dis. 2006;38:36–42. https://doi.org/10.1080/00365540500372879.
Chong E, Reynolds J, Shaw J, Forur L, Delmore P, Uner H, et al. Results of a two-center, before and after study of piperacillin–tazobactam versus ampicillin and gentamicin as empiric therapy for suspected sepsis at birth in neonates ⩽1500 g. J Perinatol. 2013;33:529–32. https://doi.org/10.1038/jp.2012.169.
Tewari VV, Jain N. Monotherapy with amikacin or piperacillin-tazobactum empirically in neonates at risk for early-onset sepsis: a randomized controlled trial. J Trop Pediatr. 2014;60:297–302. https://doi.org/10.1093/tropej/fmu017.
Wu YE, Hou SS, Fang ZY, Tang BH, Yao BF, Dong YN, et al. Clinical utiliy of a model-based piperacillin dose in neonates with early-onset sepsis. Br J Clin Pharmacol. 2022;88:1179–88. https://doi.org/10.1111/bcp.15058.
Fisher JW, Wu H, Cohen-Wolkowiez M, Watt K, Wang J, Burckart GJ, et al. Predicting the pharmacokinetics of piperacillin and tazobactam in preterm and term neonates using physiologically based pharmacokinetic modeling. Comput Toxicol. 2019;12: 100104. https://doi.org/10.1016/j.comtox.2019.100104.
Darwich AS, Polasek TM, Aronson JK, Ogungbenro K, Wright DFB, Achour B, et al. Model-informed precision dosing: background, requirements, validation, implementation, and forward trajectory of individualizing drug therapy. Annu Rev Pharmacol Toxicol. 2021;61:225–45. https://doi.org/10.1146/annurev-pharmtox-033020.
El Hassani M, Marsot A. External evaluation of population pharmacokinetic models for precision dosing: current state and knowledge gaps. Clin Pharmacokinet. 2023;62:533–40. https://doi.org/10.1007/s40262-023-01233-7.
Simeoli R. Editorial: Therapeutic drug monitoring (TDM): a useful tool for pediatric pharmacology applied to routine clinical practice, Volume II. Front Pharmacol. 2023; 14:1250784. https://doi.org/10.3389/fphar.2023.1250784.
Schwartz GJ, Feld LG, Langford DJ. A simple estimate of glomerular filtration ratein full-term infants during the first year of life. J Pediatr. 1984;104:849–54. https://doi.org/10.1016/S0022-3476(84)80479-5.
Rodríguez-Báez AS, Jiménez-Meseguer M, Milán-Segovia R del C, Romano-Moreno S, Barcia E, Ortiz-Álvarez A, et al. A comparison of pharmacokinetics software for therapeutic drug monitoring of piperacillin in patients with severe infections. Eur J Hosp Pharm. 2022; ejhpharm-2022-003367. https://doi.org/10.1136/ejhpharm-2022-003367.
Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatric Clin North Am. 1986;33:179–201. https://doi.org/10.1016/s0031-3955(16)34975-6.
Salerno S, Hornik CP, Cohen-Wolkowiez M, Smith PB, Ku LC, Kelly MS, et al. Use of population pharmacokinetics and electronic health records to assess piperacillin-tazobactam safety in infants. J Pediatr Infect Dis. 2017;36:855–9. https://doi.org/10.1097/INF.0000000000001610.
Chen Y, Lu J, Dong M, Wu D, Zhu Y, Li Q, et al. Target attainment analysis and optimal sampling designs for population pharmacokinetic study on piperacillin/tazobactam in neonates and young infants. Eur J Clin Pharmacol. 2016;72:1479–88. https://doi.org/10.1007/s00228-016-2131-0.
Girdwood ST, Hasson D, Caldwell JT, Slagle C, Dong S, Fei L, et al. Relationship between piperacillin concentrations, clinical factors and piperacillin/tazobactam-associated acute kidney injury. J Antimicrob Chemother. 2023;78:478–87. https://doi.org/10.1093/jac/dkac416.
Campbell RE, Chen CH, Edelstein CL. Overview of antibiotic-induced nephrotoxicity. Kidney Int Rep. 2023;8:2211–25. https://doi.org/10.1016/j.ekir.2023.08.031.
Reed MD, Goldfarb J, Yamashita TS, Lemon E, Blumer JL. Single-dose pharmacokinetics of piperacillin and tazobactam in infants and children. Antimicrob Agents Chemother. 1994;38:2817–26. https://doi.org/10.1128/AAC.38.12.2817.
Dyson A and Kent AL. The Effect of Preterm Birth on Renal Development and Renal Health Outcome. Neoreviews. 2019; 20: e725–736.; https://doi.org/10.1542/neo.20-12-e725.
Béranger A, Benaboud S, Urien S, Nguyen-Khoa T, Gana I, Toubiana J, et al. Estimation of piperacillin clearance with different glomerular filtration rate formulas in critically ill children. Br J Clin Pharmacol. 2021;87:1275–81. https://doi.org/10.1111/bcp.14505.
Kacet N, Rousel M, Gremillet C, Dubos J, Storme L, Lequien P. Pharmacokinetic study of piperacillin in newborns relating to gestational and postnatal age. Pediatr Infect Dis J. 1992;11:365–9. https://doi.org/10.1097/00006454-199205000-00005.
Allegaert K, Smits A, van Donge T, van den Anker J, Sarafidis K, Levtchenko E, et al. Renal precision medicine in neonates and acute kidney injury: How to convert a cloud of creatinine observations to support clinical decisions. Front Pediatr. 2020;8:366. https://doi.org/10.3389/fped.2020.00366.
Touw DJ, Van Den Anker JN. Therapeutic drug monitoring of antimicrobial drugs in neonates: an opinion article. Ther Drug Monit. 2022;44:65–74. https://doi.org/10.1097/FTD.0000000000000919.
Acknowledgements
The authors express their gratitude to the patients and parents of the neonatal patients who took part in this study. They would also like to acknowledge the assistance of the clinical staff from the NICU at Hospital "Dr. Ignacio Morones Prieto" in San Luis Potosí.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
The authors have no conflicts of interest.
Author Contributions
FSBP, SRM, VLR, RCMS and SEMG conceived the idea of the paper and contributed to the study conception and design. VLR and ARME provided the clinical supervision of the study. SEMG, ASRB, CJRP and FSBP developed and validated the bioanalytical method. Data collection and sampling were performed by FSBP. Blood samples analysis was performed for FSBP and ASRB. The first draft of the manuscript was written by FSBP. All authors revised, contributed, and approved the final manuscript.
Funding
This work was promoted by the Research Support from the Technological Research Council of Science (CONACYT) from México to FSBP for a doctoral fellowship (Grant 811004). CONACYT had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Data Availability
Data from this study cannot be shared publicly, for the data privacy statement included in the consent documents signed by the parents or legal guardians of the patients involved in this research.
Code Availability
Not applicable.
Ethics Approval
This study was approved by the Research Ethics Committee at the Hospital Central “Dr. Ignacio Morones Prieto” (Register number 36-20) in September 2020.
Consent to Participate
Written, informed consent was obtained from all parents or legal guardians of each patient.
Consent for Publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Boer-Pérez, F.S., Lima-Rogel, V., Mejía-Elizondo, A.R. et al. External Evaluation of Population Pharmacokinetic Models of Piperacillin in Preterm and Term Patients from Neonatal Intensive Care. Eur J Drug Metab Pharmacokinet 49, 595–607 (2024). https://doi.org/10.1007/s13318-024-00906-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-024-00906-3