Abstract
Antitumor immunotherapeutic strategies represent an especially promising set of approaches with rapid translational potential considering the dismal clinical context of high-grade gliomas. Dendritic cells (DCs) are the body’s most professional antigen-presenting cells, able to recruit and activate T cells to stimulate an adaptive immune response. In this regard, specific loading of tumor-specific antigen onto dendritic cells potentially represents one of the most advanced strategies to achieve effective antitumor immunization. In this study, we developed a DC-specific adenoviral (Ad) vector, named Ad5scFvDEC205FF, targeting the DC surface receptor, DEC205. In vitro analysis shows that 60% of DCs was infected by this vector while the infectivity of other control adenoviral vectors was less than 10%, demonstrating superior infectivity on DCs. Moreover, an average of 14% of DCs were infected by Ad5scFvDEC205FF-GFP, while less than 3% of non-DCs were infected following in vivo administration, demonstrating highly selective in vivo DC infection. Importantly, vaccination with this vehicle expressing human glioma-specific antigen, Ad5scFvDEC205FF-CMV-IE, shows a prolonged survival benefit in GL261CMV-IE-implanted murine glioma models (p < 0.0007). Furthermore, when rechallenged, cancerous cells were completely rejected. In conclusion, our novel, viral-mediated, DC-based immunization approach has the significant therapeutic potential for patients with high-grade gliomas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma (GBM) is a highly aggressive, malignant primary brain tumor that carries a dismal prognosis even when treated by the standard care of surgery, chemotherapy, and radiation in most patients [1]. Given this poor outcome for patients and the inadequate therapeutic efficacy of current treatments, the field of neuro-oncology demands new and advanced treatment options to extend patient survival. In this study, we explored the potential of a novel dendritic cell (DC)-based immunotherapy—a strategy that takes advantage of the body’s own immune system to generate a specific adaptive immune response [2] against the tumor—by way of adenoviral tropism redirection via genetic manipulation to specifically target DCs and deliver a tumor antigen to elicit an antitumor immune response.
DCs, the body’s professional antigen-presenting cells, are ideal for creating tumor-specific adaptive immune process [2]. In addition to antigen presentation, mature dendritic cells (mDCs) release cytokines and chemokines to induce the activation of tumor-specific T cells [2, 3]. Immature dendritic cells (iDCs), on the other hand, are incapable of inducing an antigen-specific immune response and may partially induce T-cell differentiation to immunosuppressive regulatory T cells, which negates the therapeutic benefit of a DC-based cancer vaccination. Therefore, it is imperative for any dendritic cell vaccine or immunization approach to selectively deliver the tumor antigen (TA) to mDCs or otherwise induce DC maturation upon TA delivery [2,3,4,5,6].
One potential GBM-specific TA that may be ideal for DC presentation is the cytomegalovirus immediate early gene product (CMV-IE) [7,8,9,10]. This CMV-IE antigen is reportedly seen in more than 90% of GBM patient samples evaluated, making CMV’s presence in GBM a potential target for DC immunotherapy [7,8,9,10]. Our own analysis of CMV-IE in patient tissue corroborated these findings and an experiment in a glioma murine model cell line confirmed the validity of this TA target.
To create an adenoviral vector-mediated DC vaccination, we genetically engineered the human adenovirus serotype 5-based vector (Ad5). We selected the Ag receptor dendritic and epithelial cell receptor with a molecular weight of 205 kDa (DEC205), which is known to be nearly exclusively expressed by DCs and its expression is significantly upregulated in mature DCs [11,12,13,14], for the purpose of redirecting the adenovirus to DCs. To accomplish this, we incorporated a single-chain antibody (scFv) specific for DEC205 onto the adenoviral fiber domain, which dictates the adenoviral tropism (this new adenoviral vector is thus named Ad5scFvDEC205FF) [15,16,17,18]. Furthermore, previous work has suggested that the infection of adenovirus, itself, can induce DC maturation upon cell entry, an attractive trait for the in vivo translation of this viral-based DC immunotherapy [19, 20].
To further optimize this novel adenoviral vehicle, we overcame the generic hurdles facing systemic adenovirus administration. For example, most people have neutralizing antibodies (NAb) against Ad5, especially the fiber (i.e., the most structurally protruding viral domain) and the hexon (most structurally abundant domain) [21, 22]. In addition to this immune-mediated vector clearance, it is known that systemic delivery of adenovirus can cause liver sequestration and toxicity due to the interaction between coagulation factor X (FX) and the adenoviral hexon protein [23,24,25,26]. To overcome the first obstacle of NAb against the fiber domain, we modified the structurally exposed fiber domain with the scFvDEC205 and incorporated this into a chimeric fiber fibritin structure, which originates from bacteriophage (Sup Fig 1). Secondly, to minimize liver sequestration and the recognition of NAbs against the viral hexon, we replaced the hexon domain of Ad5 with that of human Ad serotype 3 (Ad3), since it has been shown the hexon of Ad3 has relatively low affinity to FX, and this serotype 3 is less prevalent in humans, making pre-existing NAb formation less likely [23,24,25,26].
Hence, in this study, we generated a highly specific DC-targeting adenoviral vector suitable for the systemic administration that carries a tumor antigen payload through a series of advanced genetic modifications. Next, we showed the capability of this modified virus to efficiently infect DCs both in vitro and in vivo, while simultaneously inducing DC maturation following viral infection. Moreover, we demonstrated that following viral infection, the infected DCs induce an antigen-specific T-cell activation, and these T cells can kill tumor cells expressing the TA. Finally, this adenoviral-mediated vaccination of DCs significantly prolonged the survival of mice bearing murine gliomas that expressed human glioma-specific antigen (CMV-IE) in both pre- and posttreatment models. Furthermore, the immunological antitumor memory was long-lasting, successfully preventing mortality in a tumor rechallenging experiment. Collectively, our data support the further exploration of this adenoviral vaccination strategy as a potential treatment strategy for humans with malignant gliomas.
Material and Methods
Cell Lines
Human embryonic kidney (HEK) 293, HEK 293- F28 stably expressing Ad5 wild-type fibers, Chinese hamster ovary (CHO) cells, CHO-hCAR cells stably expressing human CAR, murine glioma cell, and GL261 and GL261CMV-IE cells stably expressing CMV-IE gene products were cultured in the media that contained 10% fetal bovine serum, (FBS; Hyclone; Logan, UT), 100 unit/ml penicillin, and 100 mg/ml streptomycin (Mediatech, Inc., Herndon, VA) and incubated at 37 °C in 5% CO2 in humidified conditions. To generate murine DCs, bone marrow from C57BL/6 mice was harvested from tibias and femurs. Red blood cells (RBCs) were lysed with RBC lysing (ACK) buffer (Lonza, Basel, Switzerland).
Cells were plated in 6 well plates at 1−3 × 105 cells/ml in 2 ml of DC culture media containing RPMI 1640 (Mediatech) with 10% fetal bovine serum (Hyclone), 100 unit/ml penicillin, 100 mg/ml streptomycin (Mediatech), and murine GM-CSF (20 ng/ml, Miltenyi, Auburn, CA). On day 3, half of the media was removed without any agitation and 2 ml of the DC culture media was supplemented. Cells were cultured for 6 days to obtain dendritic cells.
Genetic Modifications and Virus Production
To generate a fiber shuttle vector, pKan-566 containing the gene of fiber fibritin was used [27]. The plasmids containing single-chain antibody against DEC205 were kindly offered by Dr. Miguel A. Gómez-Lima. The nucleotide sequence of the single-chain antibody against DEC 205 was inserted at the C-terminal of fiber fibritin by using a standard molecular technique, resulting in pKan566-scFvDEC205. Recombinant HAd5 backbones containing an enhanced green fluorescence protein (eGFP) or ovalbumin or CMV-IE under the control of the CMV promoter in the E1 deleted region was used to perform homologous recombination with pKan566-scFvDEC205, generating Ad5scFvDEC205FF-GFP, Ad5scFvDEC205-OVA, and Ad5scFvDEC205-CMV-IE, respectively. Hexon modification was done in the same manner as previously described [26]. The recombinant viruses were rescued and propagated in HEK293-F28 until the last propagation step, and the last propagation in 20 × 175 ml flasks was done in HEK293 cells. Viruses were purified by two rounds of CsCl gradient ultracentrifugation and their titer was determined at 260 nm [28]. The virus titer of Ad5scFvDEC205 was highly equivalent to that of Ad5WT (Sup. Fig. 2).
PCR Analysis and Western Blot
Purified adenoviral DNA contained in Ad5GFP and Ad5scFvDEC205-GFP was used as templates for PCR amplification of fiber genes using a HAdV-5-specific primer set: (fwd) 5′-CAGCTCCATCTCCTAACTGT-3′ and (rev) 5′-TTCTTGGGCAATGTATGAAA-3′, and a scFvDEC205-specific primer set: (fwd) 5′-ATGGGATGGTCTTGCATCATT-3′ and (rev) 5′-GAGCTCGTCGACTCTCTTAAGC-3′. For Western blot analysis, purified adenoviral particles (1 × 1010) were diluted in Laemmli buffer, incubated either at room temperature (unboiled samples) or at 95 °C (boiled samples) for 10 min and loaded to a 4–10% SDS-polyacrylamide gel (Bio-Rad, Hercules, CA). After electrophoretic separation, samples were transferred onto a PVDF membrane and detected with a 4D2 monoclonal antifiber tail antibody (1:3000) (Thermo Scientific, IL, USA) followed by HRP tagged anti-mouse IgG secondary antibody (1:5000) (Santa Cruz, CA, USA).
Virus Infectivity Analysis
For in vitro analysis, 3 × 105 cells were plated in 24 well plates and incubated overnight. Each virus sample was diluted to a multiplicity of infection of in-text-described viral particles (vp)/cells in 500 μl of infection media containing 2% FBS in DMEM. The cells were infected with each virus for 2 h at 37 °C. Virus-containing media was replaced with the fresh media containing 2% FBS and cells were maintained at 37 °C in atmospheric humidification containing 5% CO2 for 3 days until flow cytometry analysis. In virus infectivity analysis of DCs, percentage of GFP-positive cells in CD45+/CD11+ DC population were utilized. For in vivo analysis, 109 viral particles were subcutaneously administrated. After 5 days, spleens and draining lymph nodes were harvested, followed by FACS analysis. For DC maturation analysis, bone marrow-derived DCs were prepared and the viral infections were done as described above. After confirmation of bone marrow-derived DCs, DCs were analyzed against the expression level of maturation markers.
FACS Analysis
Spleen or draining lymph nodes from mice administrated with Ad5scFvDEC205-GFP (109 vp, s.c.) were harvested into complete RPMI (Mediatech) 3 days after the injection. Single-cell suspension was prepared by processing organs through a 70-μm nylon cell strainer (Thermo Fisher, Waltham, MA). Red blood cells were lysed using 1 ml ACK buffer (Lonza) followed by inactivation, centrifugation, and resuspension. All antibody staining was performed in 2% PBS/FBS. Cells were stained for 15 min at 4 °C with fluorescently labeled antibodies for the following surface markers (and their dilutions): anti-CD45 APC-Cy7 1:200, anti-CD11b Pacific Blue 1:400, and anti-CD11c APC 1:200, anti-CD8α BV605 1:200, anti-CD80 FITC 1:200, and anti-CD40 PE 1:200 were all purchased from Biolegend. Samples were acquired using a LSR-Fortessa flow cytometer (Becton Dickinson, Franklin Lakes, NJ). All flow cytometry gating and data analysis were performed using FLOWJO Software (Flowjo LLC, OR, USA).
Activated T Cell-Mediated Cytotoxicity Analysis
For LDH assay, DC culture and virus infection were performed in the same way as described above. After 3 days, isolated CD8+ T cells (EasySep Mouse CD8+ T Cell Isolation Kit, Stemcell, MA, USA) were incubated with the post Ad5scFvDEC205FF-CMV-OVA-infected DCs. Activated CD8+ T cells were transferred to GL261 or GL261-OVA in different ratios as indicated in the text, followed by LDH cytotoxicity analysis according to the company instruction (Thermo Scientific). For MTT assay, virus infection was done in the same way as described above except for which MOI of 100 vp/cells was used instead. MTT assay was performed using cell proliferation kit I according to the manufacture’s instruction (Roche, Mannheim, Germany). For chromium51 (Cr51) release assay, standard chromium (Cr51) release assays were performed as previously described.
Briefly, 1 × 105 target cells were labeled with 0.1 mCi (3.7 MBq) Cr51 and mix with activated CD8+ T cells by virus-infected DCs. The ratio of the virus to DCs and DCs to CD8+ T cells is as described in the text. Spontaneous and maximum Cr51 release controls were generated incubating the target cells (GL261 or GL261-OVA) in complete medium alone or in 1% Triton X-100, respectively. After incubating in each condition for 4 h, the radioactivity from the supernatants was measured in a gamma counter (Cobra Quantum; PerkinElmer, Wellesley, MA). The cytotoxicity was calculated according to the following a formula (%): (test release − spontaneous release) / (maximal release − spontaneous release) × 100.
Animal Study
Intracranial glioma xenograft implantation: GL261or GL261CMV-IE (1 × 105 cells) murine glioma cells were implanted via cranial guide screws as described previously [29]. The 109 viral particles of Ad5scFvDEC205-CMV-IE (prevaccination) and Ad5scFvDEC205H3-CMV-IE (postvaccination) were subcutaneously administrated. Detailed vaccination strategies are in each figure. For survival analysis, animals losing ≥ 30% of their body weight or having trouble ambulating, feeding, or grooming were euthanized by CO2 administration followed by cervical dislocation. For rechallenging analysis, the same number of glioma cells was implanted on the opposite site of the initial injection site. After 75 days, animals were sacrificed. Brains were harvested, sectioned, and H&E-stained.
Statistical Analysis
All statistical analyses were performed using GraphPad Prism 4 (GraphPad Software Inc., San Diego, CA). The sample size for each group was ≥ 3 and numerical data was reported as mean ± S.E. Student’s t test was used for comparisons between two groups, and ANOVA with Tukey’s post hoc test was used for comparisons between more than two groups. Kaplan–Meier survival curve was generated and log rank test was applied to compare survival distributions. All reported p values were two-sided and were considered to be statistically significant at *p < 0.05, **p < 0.01, ***p < 0.001.
Results
Generation and Confirmation of DC-Targeting Adenoviral Vector
The natural tropism of Ad5 is dictated by the fiber knob domain which can be genetically modified to redirect Ad5 to a specific cell/tissue other than those that express the coxsackie and adenovirus receptor (CAR), which is the primary receptor for determining Ad5 tropism [15, 18, 30]. DCs are deficient in CAR expression, which makes targeting DCs with wild-type Ad5 unachievable [31,32,33]. To address this critical barrier, a novel Ad5 that can infect DCs was developed by incorporating a single-chain fragment variable (scFv) antibody against a cell surface DC marker, DEC205, into the knob domain with an additional fiber-stabilizing modification of the fiber shaft domain, called fiber fibritin (namely, Ad5scFvDEC205FF, Sup. Fig 1) [17]. Generation of this modified virus DC targeting Ad5scFvDEC205FF was confirmed at the DNA level (PCR analysis, Fig. 1A) and at the protein level (Western blot analysis Fig. 1B). Purified viral DNA of wild-type (WT) Ad5 and that of Ad5scFvDEC205 (DEC205) were used for PCR analysis with a fiber-specific primer set and scFvDEC205-specific primer set. For Western blot analysis, purified virus particles (109) were boiled (B) to dissociate fiber trimer (a monomeric form of the fiber) and unboiled (U) to keep the trimeric fiber intact. The fiber proteins were detected by an antifiber tail antibody, recognizing trimeric and monomeric form of recombinant fiber. Thus, PCR analysis revealed the insertion of the scFvDEC205 gene on the fiber gene of the purified viral gene (Fig. 1A) and Western blot analysis shows that scFvDEC205 incorporated fibers are stably trimerized and incorporated into Ad5 (Fig. 1B) as the bands of scFvDEC205 incorporated fibers from the trimers and monomers were comparable to those of wild-type Ad5 with an increased molecular weight. Since the knob and shaft domains of Ad5scFvDEC205FF were replaced with scFvDEC205FF (Sup Fig 1), it should not be able to infect a cell in a CAR-dependent manner. To verify CAR-independent infectivity of Ad5scFvDEC205FF-GFP, we performed a viral infection (300 virus particles(vp)/cell) followed by a flow cytometric analysis in a human CAR-negative cell line, Chinese hamster ovary (CHO) cell line, and a CHO-derived cell line, CHO-hCAR (Fig. 1C), which stably expresses human CAR. While the infection rate of Ad5GFP is dramatically increased in CHO-hCAR cells, as expected, there was no difference in the infection rate of Ad5scFvDEC205FF-GFP from both cell lines (Fig. 1D). Therefore, we confirmed the generation of Ad5scFvDEC205FF and demonstrated that Ad5scFvDEC205FF infects cells in a CAR-independent manner.
Generation and confirmation of the novel virus. (A) PCR analysis of fiber genes of the adenoviral DNA from purified viral particles as PCR templates. Purified viral DNA from Ad5GFP (lanes 2 and 4) and Ad5scFvDEC205FFGFP (lanes 3 and 5) were used as DNA templates to amplify each fiber gene with a fiber-specific primer set (lanes 2 and 3) or with scFvDEC205-specific primers (lanes 3 and 5). Lane 1 shows DNA size standards (Kb). (B) Detection of fiber trimerization and incorporation in the viral particles by Western blot analysis with an HAdV-5 tail antibody (4D2). Purified viral particles (1 × 1010vp) of Ad5GFP (lanes 1 and 2) or those of Ad5scFvDEC205GFP (lanes 3 and 4) were analyzed. Samples were identified as U (unboiled, incubation at room temperature for 10 min) in lanes 1 and 3 and as B (boiled, incubation at 95 °C for 10 min) in lanes 2 and 4 show the nondenatured trimeric fiber composition and the denatured monomeric fiber composition, respectively. Makers indicate kiloDaltons (kDa). (C) Flow cytometric analysis of CAR-independent infection of Ad5scFvDEC205GFP. Cells were infected with Ad5CMV-GFP or Ad5scFvDEC205GFP at an MOI of 300 vp/cell for 2 h on CAR-negative CHO and CAR-positive CHO-hCAR cell line, and the virus containing media was removed and replaced with fresh media containing 2% FBS. 72 h after infection, flow cytometric analysis was performed. Each column is the average of three independent replicates. Data presented as mean ± S.E.
Ad5scFvDEC205FF Can Efficiently and Selectively Infect DC In Vitro and In Vivo
Next, to determine whether scFvDEC205 in the fiber of Ad5scFvDEC205FF dictates the viral infection to DCs, we isolated the murine splenic cells for the viral infection. The infectivity of DCs by Ad5scFvDEC205FF was compared against three other adenoviral vectors: Ad5PK7-GFP (infectivity enhanced adenoviral vector via addition of poly-lysine on the fiber which binds to anionic surface proteins) [34,35,36], Ad5/3-GFP (DC infectivity enhanced adenoviral vector by replacing the Ad5 knob with the Ad3 knob, which binds to CD46, CD80, CD86, and desmoglein 2) [32, 34, 37], and wild-type Ad5-GFP. After viral infection, cells were gated on CD45+/CD11c+ (general DC surface markers [3, 5, 38,39,40,41]) and GFP-positive populations were analyzed via flow cytometric analysis. As shown in Fig. 2A, the infectivity of Ad5scFvDEC205FF on DCs was superior to that of all other viruses and the infectivity kinetics was observed as highly stable (Sup. Fig 2). To further examine the in vivo DC selectivity of Ad5scFvDEC205FF-GFP, we subcutaneously (s.c.) administered 109 vp of Ad5scFvDEC205FF-GFP and Ad5-GFP in mice. Three days after the viral infection, spleens and lymph nodes were isolated and analyzed with flow cytometric analysis. After gating with CD45+ (nucleated hematopoietic cells), the DC population (CD11c+) was analyzed for the presence of an infected DC population (GFP positive). Of note, we did not detect GFP-positive cells from wild-type Ad5-GFP-adminstrated mice since it is well known that wild-type Ad5-GFP gets aggregated in the liver and cleared out fast (data not shown). An average of 14% of DCs were infected by Ad5scFvDEC205FF-GFP, while less than 3% of non-DCs were infected following in vivo Ad5scFvDEC205FF-GFP administration (Fig. 2B). It has been suggested that the expression of DEC205 on DCs is highly correlated with CD8α+ DC subset which is known to cross-present antigens more efficiently and activate robust cytotoxic CD8+ T cell responses [13, 14, 42, 43]. For this reason, we further analyzed the Ad5scFvDEC205FF-GFP-infected DC population. After gating with CD45+ (nucleated hematopoietic cells), the DC population (CD11c+) was analyzed for the presence of a CD8α+ DC population. We observed ~19% of CD8α+ DCs from CD45+CD11c (Fig. 2C). An average of 91% of CD45+CD11c+ CD8α+ DCs were infected by Ad5scFvDEC205FF-GFP (Fig. 2D). Therefore, Ad5scFvDEC205FF possess enhanced and selective DC infectivity (highly preferential for CD8α+ DC subset) not only in vitro but also in vivo. On this basis, the tropism-modified Ad5scFvDEC205FF represents a promising agent for active GBM immunotherapy.
Enhanced and selective DC infection of Ad5scFvDEC205. (A) In vitro infectivity enhancement analysis. Spleen-derived DCs were infected with wild-type Ad5-GFP, Ad5PK7-GFP, Ad5/3-GFP, and Ad5scFvDEC205FF-GFP at an MOI of 300 vp/cell for 2 h on DCs and the virus-containing media was removed and replaced with fresh media containing 2% FBS. After 72 h, cells were stained with DC markers (CD45 and CD11c) followed by flow cytometric analysis. Infected DCs were identified with GFP expression. (B) In vivo DC flow analysis. After gating with CD45+, the DC population (CD11c+) was analyzed to identify GFP-positive DC population. (B) In vivo selective DC infectivity analysis. 109 vp of Ad5scFvDEC205FF-GFP were administrated subcutaneously. Spleens and lymph nodes were isolated 5 days after the viral administration, followed by flow cytometric analysis. GFP-positive DCs (CD45+/CD11c+/GFP+) were first analyzed. Among DCs, percentage of CD8α+ DC subset (C) and that of GFP positive in CD8α+ DC subset (D) are shown. Each data point is the average of three independent replicates. Data presented as mean ± S.E.
Infection of Ad5scFvDEC205FF Itself Induces DC Maturation
It is imperative to deliver TA to mature DCs or induce DC maturation upon TA delivery [5, 38,39,40,41, 44, 45]. The targeting motif, DEC205, is known to be highly upregulated when DCs are mature [11, 13, 14]. Furthermore, it is perceived that the infection of adenovirus, itself, induces DC maturation [46]. Since Ad5scFvDEC205FF selectively infects DCs both in vitro and in vivo, we confirmed in this study that the infection of Ad5scFvDEC205FF induces DC maturation of infected immature DCs. Bone marrow-derived DCs were infected with Ad5scFvDEC205FF-CMV-OVA. Within this novel DC-specific delivery vehicle, the glioma-specific antigen gene (i.e., CMV-IE) was inserted by replacing a viral replication essential early gene 1 (E1). This modification ensured that the viral delivery vehicle cannot replicate in or lyse the infected DCs but instead would transiently express the loaded tumor antigen within the DCs so that these DCs can present and/or cross-present this TA. Three days after infection, the levels of DC maturation markers have been analyzed via flow cytometric analysis. As shown in Fig. 3, the levels of CD40 and CD80 markers of DC maturation from infected DCs were highly elevated compared to those of non-infected DCs, confirming that Ad5scFvDEC205FF-CMV-OVA infection of DCs indeed induces the maturation of DCs. Therefore, the infection of Ad5scFvDEC205FF can facilitate the maturation of DCs if the infected DCs are immature.
Induction of DC maturation via Ad5scFvDEC205FF-GFP infections. The 3 × 105 bone marrow-derived DCs and an MOI of 300 vp/cell of Ad5scFvDEC205FF-GFP were used for the infection. After 72 h, DCs were stained with (A) DC markers (CD45 and CD11c) and (B) DC maturation markers (CD80 and CD40) followed by cytometric analysis. Each data point is the average of three independent replicates. Data presented as mean ± S.E.
Vaccinated DCs Induce TA-Specific T-Cell Activation, Leading to T Cell-Mediated Cytotoxicity of TA-Expressing Tumor Cells
Since Ad5scFvDEC205FF can infect DCs both efficiently and selectively in vitro and in vivo, and can further induce the maturation of DCs, we investigated the question as to whether Ad5scFvDEC205FF-CMV-OVA-mediated DC vaccination can induce TA-specific T-cell activation so as to kill the TA-expressing tumor cell line. To assess this, we first performed a LDH release assay. After DC infection with Ad5scFvDEC205FF-CMV-OVA at different MOIs, isolated CD8+ T cells were added to activate these T cells in a TA (OVA)-specific manner. Activated CD8+ T cells were transferred to TA-expressing target tumor cells (GL261-OVA). The cell death of TA-expressing glioma cells (GL261-OVA) by activated T cells was analyzed. As DCs were infected with a high titer of Ad5scFvDEC205FF-CMV-OVA, CD8+ T cells could be more efficiently activated in a TA-specific manner, rendering these activated T cells able to kill target tumor cells more effectively (Fig. 4A). In order to investigate the activated CD8+ T cell-mediated cytotoxicity at different time points, we also performed an MTT (Supp. Fig 3). DCs were infected with Ad5scFvDEC205FF-CMV-OVA at different MOIs, followed by CD8+ T-cell incubation for 72 h. Since the LDH assay showed the optimal ratio of CD8+ T cells to tumor target cells (GL261-OVA) at 1:1 (Fig. 4A), we incubated these activated CD8+ T cells in GL261-OVA in 1:1 ratio and analyzed the cytotoxicity in a time-dependent manner (12, 24, and 48 h). As observed from the LDH assay, the cytotoxic activity of activated CD8+ T cells was the most efficient when DCs were infected with Ad5scFvDEC205FF-CMV-OVA at an MOI of 300 vp/cell at all time points (Fig. 4).
Cytotoxicity analysis of TA-specific CD8+ T cell activated by Ad5scFvDEC205FF-OVA-transduced DCs. 3 × 105 bone marrow-derived DCs were infected with Ad5scFvDEC205FF-OVA at an MOI of 100, 200, and 300 vp/cell for 2 h on DCs and the virus-containing media was removed and replaced with a fresh media containing 2% FBS. After 72 h, CD8+ T cells isolated from syngeneic mice were incubated with infected DCs in the ratio of 1:1. Activated CD8+ T cells were transferred to either GL261 or GL261-OVA followed by (A) LDH assay and (B) Cr51 release assay. The ratio of 1:3 = target cells: T cells from LDH analysis were used for (C) the microscopic observation. Arrows and dot arrows indicate glioma cells and CD8+ T cells, respectively. The bar indicates 100 μm. Each data point is the average of three independent replicates. Data presented as mean ± S.E.
To further confirm this finding, we utilized another classic assay for accessing T cell-mediated cytotoxic function using Cr51. Since Cr51 is only loaded in target tumor cells, it is a classic and efficient way to measure cytotoxicity by T cells by analyzing the release of Cr51 from dying target cells. Infection of DCs and T-cell activation was done in the same way as described already. Next, to analyze if T cells were activated in a TA-specific manner (OVA-specific), activated T cells were added into the Cr51-loaded GL261 and GL261-OVA cell lines, followed by analyzing the release of Cr51 from dead target tumor cells. Since CD8+ T cells were activated specifically against an antigen (OVA), GL261 cells (no antigen-expressing cells) were not recognized by OVA-specifically activated T cells evidenced by no observable cytotoxicity (Fig. 4B). On the other hand, antigen-expressing GL261-OVA cells were efficiently recognized by OVA-specifically activated CD8+ T cells, thereby causing high cytotoxicity in GL261-OVA cells (Fig. 4B). Interestingly, OVA-specifically activated T cells localized evenly away from GL261 cells while these T cells clustered around GL261-OVA cells, inducing cell death (Fig. 4C). Therefore, combining the data from the experiments described, strongly supports that 1) Ad5scFvDEC205FF-CMV-OVA-infected DCs can be matured and present OVA antigens, 2) this OVA antigen-presenting mature DCs can activate CD8+ T cells against OVA antigen, specifically, and 3) these T cells can recognize the specific antigen (OVA) on the tumor cells and kill the tumor cells in an antigen-specific manner (Figs. 3 and 4).
Confirmation of GBM-Specific Tumor Antigen (CMV-IE) Expression and Generation of a Murine Glioma Cell Line Expressing the Antigen, GL261-CMV-IE
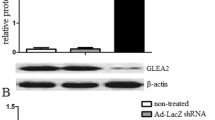
Although several GBM-specific targets for immunotherapy have been identified, such as EGFRvIII and IL13Rα2, these molecules are, unfortunately, only targetable in a limited percentage (< 30%) of GBM patients [46]. Recently, there have been reports demonstrating the presence of cytomegalovirus (CMV) in more than 90% of GBM patients [47,48,49] examined and though some established relationship between CMV persistence [50,51,52] and glioma tumorigenesis has been elucidated, this intriguing correlation and its potential for targeted immunotherapy inspired us to further verify the presence of CMV immediate early gene product (CMV-IE) in patient-derived glioma tissues (Fig. 5A). Brain cancer and adjacent normal tissue array (GL803b, Biomax, Rockville, MD) were stained with anti-CMV-IE antibody. We could only observe CMV-IE-specific staining from glioma tissues but none from peripheral normal tissue (Fig. 5A). This patient tissue-based analysis suggests that CMV-IE could be a highly applicable molecular target for GBM immunotherapy. Hence, to investigate our GBM immunotherapeutic approach with this CMV-IE antigen, we generated a murine glioma model cell line, GL261CMV-IE. The gene of CMV-IE was intrachromosomally incorporated into GL261 cell line with a Lentivirus encoding CMV-IE, generating GL261-expressing CMV-IE stably. The expression of CMV-IE from GL261CMV-IE cell line was confirmed via Western blot analysis (Fig. 5B). Therefore, CMV-IE is a highly suitable target for human glioma vaccine therapy and our established murine cell line (GL261CMV-IE) can serve as a highly valuable therapeutic experimental model cell line in this regard.
Validation of human glioma-specific antigen (CMV-IE) and generation of the CMV-IE-expressing murine glioma model cell (GL261CMV-IE). (A) Brain cancer and adjacent normal tissue array (GL803b, Biomax) were stained with anti-CMV-IE antibody. All the GBM tissue staining with anti-CMV-IE showed CMV-IE positive. The representative tissue staining is shown including a normal brain tissue staining. (B) Murine glioma GL261 cells were lenti-virally transduced to generate a stably CMV-IE-expressing GL261CMV-IE cell line. The expression of CMV-IE were confirmed by Western blot analysis
Prevaccination with Ad5scFvDEC205FF-CMV-IE Shows a Prolonged Survival Benefit in TA-Specific Manner
Our in vitro analysis showed that Ad5scFvDEC205FF efficiently infects, loads an antigen, and induces maturation of DCs (Figs. 2 and 3). These Ad5scFvDEC205FF-infected and matured DCs can activate CD8+ T cells in an antigen-specific manner that efficiently lyses the target tumor cells (Fig. 4). Therefore, we utilized the versatile Ad5scFvDEC205FF virus to selectively load the GBM-TA (CMV-IE, Fig. 5) in DCs in order to trigger a strong antitumor immune response via generating Ad5scFvDEC205FF-CMV-IE. As an initial approach, we first investigated the prevaccination-based tumor-specific therapeutic efficacy as depicted in Fig. 6A. In antigen-expressing tumor cell line (GL261CMV-IE)-implanted mice, there is no survival benefit from PBS subcutaneous-injected group (mean survival, 20 days) while Ad5scFvDEC205FF-CMV-IE showed a statistically significant prolong survival (p < 0.02). Moreover, when Ad5scFvDEC205FF-CMV-IE is subcutaneously injected in non-antigen-expressing glioma cell (GL261)-implanted mice, there is no survival benefit which indicates that Ad5scFvDEC205FF-CMV-IE specifically induces an immune response against CMV-IE (Fig. 6B). Therefore, our in vivo prevaccinated survival analysis suggests that Ad5scFvDEC205FF-CMV-IE is highly efficient as a vaccination strategy against a human glioma antigen (CMV-IE) and extended survival periods in the human glioma-carrying murine model.
Hexon-Modified Adenoviral Vaccine Mediates Superior Vaccine Efficacy on a Postvaccination Glioma Model and Rejected Rechallenged Tumor Implantation
It is known that liver sequestration of human adenovirus serotype 5 (Ad5) limits therapeutic efficacy. Recent findings suggest that interactions of Ad5 capsid protein, hexon, with the blood coagulation factor X (FX) lead these complexes to attach to cell surface heparin sulfate proteoglycans (HSPGs) on hepatocytes [22, 24, 26]. The attachment of this complex causes sequestration of adenoviral therapeutic vehicles on liver [22, 24]. One strategy to overcome this challenge is to replace the Ad5 hexon with the hexon from Ad3, which has been shown to minimize the liver sequestration and toxicity since the hexon of human adenovirus serotype 3 has a relatively low affinity to FX [26]. Based on this rationale, we generated hexon-modified DC-targeting adenoviral vector, Ad5H3scFvDEC205FF-CMV-IE and investigated the vaccine efficacy after the tumor implantation (postvaccine approach). As shown in Fig. 7, while the median survival of PBS-treated group was 19 days, all the vaccinated group showed no signs of tumor and was healthy until day 75. To further verify this vaccination efficacy and possibility to induce memory cells against CMV-IE, we rechallenged GL261CMV-IE on the other side of previously tumor-implanted site. Again, all the tumor-rechallenged mice were healthy without any sign of illness. After another 75 days of tumor rechallenging (150 days in total), we sacrificed mice and looked for any signs of tumor on the brain. As shown in Fig. 7B, there were no observable tumor cells around the injection site confirming that the vaccinated mice remained tumor free following tumor rechallenging.
The efficacy of the postvaccination (Ad5scFvDEC205-CMV-IE) on the primary and rechallenged glioma murine models. Tumor implantation and vaccination procedures were done as described in (A). After 75 days of prolonged survivals from the vaccinated mice, the same number of GL261CMV-IE cells was rechallenged on the opposite site of the initial tumor implantation (B). After 75 days of tumor rechallenge, brains were harvested and sectioned and H&E staining was done to check any residual tumor cells (C). The Kaplan–Meier survival curves of treated mice were analyzed (B). ***p < 0.001
Discussion
Antitumor vaccination (ATV) strategies represent an especially promising set of approaches with rapid translational potential, especially considering the dismal clinical context of high-grade gliomas. In this regard, the most recent strategies to achieve effective antitumor immunization have sought to capitalize on the active loading of tumor-specific antigen(s) to the most professional antigen-presenting cells: dendritic cells (DCs) [2,3,4, 44]. Therefore, efficient and selective in vivo DC delivery vehicles that can facilitate highly efficient multi-epitope TA loading for maximal antitumor immunity are needed to achieve efficacious GBM immunotherapy [3, 4, 41, 45].
Here, we engineered a novel adenovirus (named Ad5scFvDEC205FF) that specifically infects DCs by incorporating a single-chain fragment variable (scFv) region antibody against a DC surface marker, DEC205 [13, 14], with an additional fiber-stabilizing modification [17]. This novel viral vector was optimized with a series of genetic modifications to specifically infect dendritic cells and deliver a tumor-specific antigen for presentation to the adaptive immune system. Furthermore, these modifications have the additional benefit of reducing the risk of liver toxicity following systemic viral administration and limiting the effect of potential preformed neutralizing antibodies from previous adenovirus exposure [21, 22]. Also, to investigate our virus in clinically relevant experiments, we generated a murine glioma model cell line that stably expresses a human glioma antigen (CMV-IE) suitable for experimentation in immunocompetent mice.
We first evaluated whether scFvDEC205 in the fiber of Ad5scFvDEC205FF dictates efficient DC infection by comparing the infectivity of DCs by Ad5scFvDEC205FF with three other control adenoviral vectors: Ad5PK7-GFP, Ad5/3-GFP, and Ad5-GFP. By undertaking this study with the use of a DC infectivity assay, we were able to see that DCs had increased infection when subject to the experimental fiber as shown in Fig. 2A. Qualitatively, the infectivity kinetics for the DCs exhibited were highly stable (Sup Fig 3). Furthermore, subcutaneous administration of this vector, Ad5scFvDEC205FF-GFP, showed highly selective infectivity on DC population (14%) as compared to that on non-DC population (3%). As the expression of DC-targeting molecule, DEC205, is highly correlated with the CD8α DC subset, which is known to cross-present an antigen and activate cytotoxic T cells more efficiently [42, 43], our data indicate that Ad5scFvDEC205FF-GFP infects preferentially to these DC subsets. These lines of data suggest the high potential for the therapeutic usages of our novel vector.
Another key aspect of DC targeting for T-cell immune responses is the DC maturation index. DCs must reach maturity in order to facilitate an effective T-cell immune response and it has shown that the DC maturation is affected by adenoviral infection [46]. In this study, we examined that the maturation of DCs as a function of adenoviral infection is a fundamental factor in the maturation of DCs—a factor that is instrumentally important in considering a DC vaccination strategy such as this one. In doing so, we learned that in addition to being a highly efficient and selective DC infector, this adenovirus-induced DC maturation, augmenting the efficacy of a T-cell immune response is mediated by the antigen presentation of DCs.
We then examined the premise of CD8+ T-cell activation via antigen-loaded and mature DCs. Three cytotoxicity analyses (LDH, MTT, and Cr51) were used to test the assumption that such CD8+ T cells are activated by TA-presenting and mature DCs in an antigen-specific manner. Additionally, we found that activated CD8+ T cells can execute a murine glioma cell antitumor response due to resultant cytotoxicity. Such cytotoxic activity for DC infection was found to be dependent on viral particle dose and thus indicative of the antitumor effectiveness.
Finally, we tested this novel adenoviral vector in the GL261CMV-IE murine glioma cell line to evaluate the success and effectiveness of DC vaccination strategy. We found that both pre- and postvaccination strategies resulted in enhanced murine survival to support marked therapeutic benefit in a TA-specific manner that was supported by additional pathological examination, both grossly and histologically. Impressively, surviving mice that were rechallenged with tumor cells still survived without any additional therapeutic injections, indicating long-term immunological memory against the tumor following virus administration.
Our approach differs radically from current antitumor immunotherapies, which typically passively deliver a tumor antigen to DCs following DC harvesting and ex vivo manipulation. Rather, we actively deliver the tumor antigen specifically to DCs in vivo using a viral vector that also stimulates DC maturation upon infection. This has the advantage of being easier to administer and being easier to redose with an additional virus if needed. Future projects can combine this viral-based dendritic cell vaccine with other immunomodulatory agents, such as checkpoint inhibition, to remove the immunosuppression present in human malignant gliomas.
In conclusion, using a series of viral modifications, we created a viral vector capable of being delivered systemically and specifically delivering a tumor antigen directly to dendritic cells that were able to activate effector T cells and lead to a robust and long-lasting immune response against the tumor. This novel approach is an exciting combination of virotherapy and immunotherapy and represents a creative dendritic cell-based immunotherapeutic approach for human tumor with persistence of protumorigenic viruses such as cytomegalovirus.
References
Young, J.S., et al., Therapeutic cell carriers: a potential road to cure glioma. Expert Rev Neurother, 2014. 14(6): p. 651–60.
Murphy, K., et al., Janeway’s immunobiology. 2012, New York: Garland Science.
Banchereau, J., et al., Immunobiology of dendritic cells. Annu Rev Immunol, 2000. 18: p. 767–811.
Apetoh, L., et al., Harnessing dendritic cells in cancer. Semin Immunol, 2011. 23(1): p. 42–9.
Caminschi, I., E. Maraskovsky, and W.R. Heath, Targeting dendritic cells in vivo for cancer therapy. Front Immunol, 2012. 3: p. 13.
Mac Keon, S., et al., Dendritic cell-based vaccination in cancer: therapeutic implications emerging from murine models. Front Immunol, 2015. 6: p. 243.
Ding, D., et al., Does the existence of HCMV components predict poor prognosis in glioma? Journal of Neuro-Oncology, 2014. 116(3): p. 515–522.
Price, R.L., et al., Cytomegalovirus contributes to glioblastoma in the context of tumor suppressor mutations. Cancer Research, 2013. 73(11): p. 3441–3450.
Schuessler, A., D.G. Walker, and R. Khanna, Cytomegalovirus as a novel target for immunotherapy of glioblastoma multiforme. Frontiers in Oncology, 2014. 4.
Söderberg-Nauclér, C., Cytomegalovirus in human brain tumors: role in pathogenesis and potential treatment options. World Journal of Experimental Medicine, 2015. 5(1): p. 1.
Buhler, J., et al., Selective uptake of cylindrical poly(2-oxazoline) brush-antiDEC205 antibody-OVA antigen conjugates into DEC-positive dendritic cells and subsequent T-cell activation. Chemistry, 2014. 20(39): p. 12405–10.
Dhodapkar, M.V., et al., Induction of antigen-specific immunity with a vaccine targeting NY-ESO-1 to the dendritic cell receptor DEC-205. Sci Transl Med, 2014. 6(232): p. 232ra51.
Niezold, T., et al., DNA vaccines encoding DEC205-targeted antigens: immunity or tolerance? Immunology, 2015.
Spiering, R., et al., DEC205+ dendritic cell-targeted tolerogenic vaccination promotes immune tolerance in experimental autoimmune arthritis. J Immunol, 2015. 194(10): p. 4804–13.
Douglas, J., Adenoviral vectors for gene therapy. Molecular Biotechnology, 2007. 36(1): p. 71–80.
Kim, J.W., et al., An adenovirus vector incorporating carbohydrate binding domains utilizes glycans for gene transfer. PLoS One, 2013. 8(2): p. e55533.
Kim, J.W., et al., A genetically modified adenoviral vector with a phage display-derived peptide incorporated into fiber fibritin chimera prolongs survival in experimental glioma. Hum Gene Ther, 2015. 26(9): p. 635–46.
Kim, J.W., et al., Viral vector production: adenovirus. Methods Mol Biol, 2016. 1382: p. 115–30.
Quinn, K.M., et al., Antigen expression determines adenoviral vaccine potency independent of IFN and STING signaling. Journal of Clinical Investigation, 2015. 125(3): p. 1129–1146.
Rea, D., et al., Adenoviruses activate human dendritic cells without polarization toward a T-helper type 1-inducing subset. J Virol, 1999. 73(12): p. 10245–53.
Yu, B., et al., Characteristics of neutralizing antibodies to adenovirus capsid proteins in human and animal sera. Virology, 2013. 437(2): p. 118–23.
Lopez-Gordo, E., et al., Circumventing antivector immunity: potential use of nonhuman adenoviral vectors. Hum Gene Ther, 2014. 25(4): p. 285–300.
Ma, J., et al., Manipulating adenovirus hexon hypervariable loops dictates immune neutralisation and coagulation factor X-dependent cell interaction in vitro and in vivo. PLoS Pathog, 2015. 11(2): p. e1004673.
Lopez-Gordo, E., et al., The importance of coagulation factors binding to adenovirus: historical perspectives and implications for gene delivery. Expert Opin Drug Deliv, 2014. 11(11): p. 1795–813.
Short, J.J., et al., Substitution of adenovirus serotype 3 hexon onto a serotype 5 oncolytic adenovirus reduces factor X binding, decreases liver tropism, and improves antitumor efficacy. Mol Cancer Ther, 2010. 9(9): p. 2536–44.
Kaliberov, S.A., et al., Retargeting of gene expression using endothelium specific hexon modified adenoviral vector. Virology, 2013. 447(1–2): p. 312–25.
Hedley, S.J., et al., An adenovirus vector with a chimeric fiber incorporating stabilized single chain antibody achieves targeted gene delivery. Gene Ther, 2006. 13(1): p. 88–94.
Maizel, J.V., Jr., D.O. White, and M.D. Scharff, The polypeptides of adenovirus. I. Evidence for multiple protein components in the virion and a comparison of types 2, 7A, and 12. Virology, 1968. 36(1): p. 115–25.
Ahmed, A.U., et al., A preclinical evaluation of neural stem cell-based cell carrier for targeted antiglioma oncolytic virotherapy. J Natl Cancer Inst, 2013. 105(13): p. 968–77.
Waehler, R., S.J. Russell, and D.T. Curiel, Engineering targeted viral vectors for gene therapy. Nat Rev Genet, 2007. 8(8): p. 573–87.
Wilkinson-Ryan, I., et al., Incorporation of porcine adenovirus 4 fiber protein enhances infectivity of adenovirus vector on dendritic cells: implications for immune-mediated cancer therapy. PLoS One, 2015. 10(5): p. e0125851.
van de Ven, R., et al., Selective transduction of mature DC in human skin and lymph nodes by CD80/CD86-targeted fiber-modified adenovirus-5/3. J Immunother, 2009. 32(9): p. 895–906.
Hangalapura, B.N., et al., Selective transduction of dendritic cells in human lymph nodes and superior induction of high-avidity melanoma-reactive cytotoxic T cells by a CD40-targeted adenovirus. J Immunother, 2010. 33(7): p. 706–15.
Arnberg, N., Adenovirus receptors: implications for targeting of viral vectors. Trends Pharmacol Sci, 2012. 33(8): p. 442–8.
Zheng, S., et al., Fiber-knob modifications enhance adenoviral tropism and gene transfer in malignant glioma. J Gene Med, 2007. 9(3): p. 151–60.
Rein, D.T., et al., Gene transfer to cervical cancer with fiber-modified adenoviruses. Int J Cancer, 2004. 111(5): p. 698–704.
Wang, H., et al., Multimerization of adenovirus serotype 3 fiber knob domains is required for efficient binding of virus to desmoglein 2 and subsequent opening of epithelial junctions. J Virol, 2011. 85(13): p. 6390–402.
Dey, M., et al., Dendritic cell-based vaccines that utilize myeloid rather than plasmacytoid cells offer a superior survival advantage in malignant glioma. J Immunol, 2015.
Fromm, P.D., et al., A multi-laboratory comparison of blood dendritic cell populations. Clin Transl Immunology, 2016. 5(4): p. e68.
MacDonald, K.P., et al., Characterization of human blood dendritic cell subsets. Blood, 2002. 100(13): p. 4512–20.
Ueno, H., et al., Targeting human dendritic cell subsets for improved vaccines. Semin Immunol, 2011. 23(1): p. 21–7.
Hildner, K., et al., Batf3 deficiency reveals a critical role for CD8alpha+ dendritic cells in cytotoxic T cell immunity. Science, 2008. 322(5904): p. 1097–100.
Li, L., et al., Cross-dressed CD8alpha+/CD103+ dendritic cells prime CD8+ T cells following vaccination. Proc Natl Acad Sci U S A, 2012. 109(31): p. 12716–21.
Matos, I., et al., Targeting antigens to dendritic cells in vivo Induces Protective Immunity. PLoS One, 2013. 8(6): p. e67453.
Wang, X., et al., Dendritic cell-based vaccine for the treatment of malignant glioma: a systematic review. Cancer Invest, 2014. 32(9): p. 451–7.
Philpott, N.J., et al., Adenovirus-induced maturation of dendritic cells through a PI3 kinase-mediated TNF-alpha induction pathway. Proc Natl Acad Sci U S A, 2004. 101(16): p. 6200–5.
Cobbs, C.S., et al., Human cytomegalovirus infection and expression in human malignant glioma. Cancer Res, 2002. 62(12): p. 3347–50.
Joseph, G.P., et al., Cytomegalovirus as an oncomodulatory agent in the progression of glioma. Cancer Lett, 2017. 384: p. 79–85.
Soderberg-Naucler, C., I. Peredo, and G. Stragliotto, Valganciclovir in patients with glioblastoma. N Engl J Med, 2013. 369(21): p. 2066–7.
Ulasov, I.V., et al., CMV70-3P miRNA contributes to the CMV mediated glioma stemness and represents a target for glioma experimental therapy. Oncotarget, 2017. 8(16): p. 25989–25999.
Soroceanu, L., et al., Cytomegalovirus immediate-early proteins promote stemness properties in glioblastoma. Cancer Res, 2015. 75(15): p. 3065–76.
Fornara, O., et al., Cytomegalovirus infection induces a stem cell phenotype in human primary glioblastoma cells: prognostic significance and biological impact. Cell Death Differ, 2016. 23(2): p. 261–9.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Funding
This work is supported by the National Institute of Health (R01CA122930, R35CA197725, and R01NS093903)-ML and Chicago Biomedical Consortium (PDR-102)-JWK.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
ESM 1.
Supplemental Figure 1. (A) Schematic diagram of a dendritic cell targeting DEC205 chimeric fiber of Ad5scFvDEC205FF. A single chain antibody against DEC205 (scFvDEC205) was incorporated into trimer-stabilizing chimeric fiber fibritin (FF) domain. The knob and the shaft domain of wild-type Ad5 fiber was replaced with this new DC targeting chimeric fiber resulting in a novel Ad5scFvDEC205FF. (B) Schematic diagram of advanced genetic modifications. Adenoviral delivery vehicle was optimized for in vivo DC based anti-tumor immunotherapy through fiber and hexon modification to target DCs and un-target from neutralizing antibodies (NAb) and liver sequestrating inducing coagulation Factor X (FX). Supplementary Figure 2. The kinetics of Ad5scFvDEC205FF infectivity. Cells were infected with Ad5scFvDEC205FF-GFP at an MOI of 100, 200 and 300 VP/cell for 2 hours on DCs and the virus-containing media was removed and replaced with fresh media containing 2% FBS. After 72 hrs, flow cytometric analysis was performed. As expected, DC infectivity increases as more vial particles were added. Each data point is the average of 3 independent replicates. Data presented as Mean ± SEM. Supplementary Figure 3. MTT based cytotoxicity analysis of TA specific CD8+ T cell activated by Ad5scFvDEC205FF-OVA transduced DCs. The bone marrow derived DCs infection with Ad5scFvDEC205FF-OVA were performed in the same way as described in Fig. 4. The antigen specific CD8+ T cell mediated cytotoxicity was analyzed in 12hr, 24 hr and 48 hr. Each data point is the average of 3 independent replicates. Data presented as Mean ± SEM. (PPTX 1583 kb)
ESM 2
(PDF 498 kb)
Rights and permissions
About this article
Cite this article
Kim, J.W., Kane, J.R., Panek, W.K. et al. A Dendritic Cell-Targeted Adenoviral Vector Facilitates Adaptive Immune Response Against Human Glioma Antigen (CMV-IE) and Prolongs Survival in a Human Glioma Tumor Model. Neurotherapeutics 15, 1127–1138 (2018). https://doi.org/10.1007/s13311-018-0650-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13311-018-0650-3