Abstract
Conventional thyroidectomy often results in visible scarring postoperatively. Endoscopic thyroidectomy offers the advantage of scarless surgery, especially beneficial for young adult women. The retroauricular approach uses a facelift incision well-known among surgeons and eliminates the need for gas insufflation due to the large working space. An early retrospective analysis was conducted on thirty-one individuals who underwent gasless retroauricular endoscopic thyroidectomy approach, focusing on isthmolobectomies (n = 26) and lobectomies (n = 5), with one case necessitating conversion to open thyroidectomy, from January 2016 to April 2017. Physical examination, laboratory, and histopathology findings were collected. The scar was evaluated using the Vancouver Scale System, while other surgical and oncological outcomes were documented and assessed. The average operative time was 154.2 ± 21.3 min, with an average bleeding volume of 69.2 ± 52.1 mL. The average length of stay was 4.7 ± 2.2 days. All complications occurred were temporary and all subjects remained in good condition throughout the follow-up period. Most subjects (65.6%) were very satisfied with the scar concealed in the retroauricular area. Retroauricular endoscopic thyroidectomy is a safe and feasible remote access technique with excellent postoperative results.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Postoperative scarring resulting from Kocher’s transverse incision on the anterior neck may lead to various problems, such as hypesthesia, paresthesia, and dysphagia. Additionally, it is also esthetically unpleasant, particularly impacting the self-esteem of young women [1, 2]. In response to these concerns, remote access surgical techniques were developed towards the latter part of the twentieth century [3].
Among the techniques used in endoscopic thyroidectomy, the retroauricular approach provides a shorter, more direct route to the neck, with minimal tissue dissection, and an adequate operating space [2]. For surgeons less experienced with the transaxillary or breast approach, the retroauricular approach may be preferable due to its similarity to a familiar facelift incision [4, 5].
A study conducted by Kartini, et al. at Dr. Cipto Mangunkusumo General Hospital in Indonesia revealed that most (72%) of their subjects had baseline tumor size larger than 4 cm, categorized as large-sized tumors according to Pemayun [6, 7]. While this may pose limitations for other endoscopic thyroidectomy approaches, it is not a concern with the retroauricular approach as it offers a larger working area, eliminating the need for gas insufflation.
Indonesia, as a developing country, is adopting this approach to enhance aesthetic outcomes and improve postoperative results. However, surgical safety remains the most important thing to consider. Our center at the Division of Surgical Oncology, Department of Surgery, Dr. Cipto Mangunkusumo General Hospital in Indonesia has previously reported favorable outcomes with endoscopic thyroidectomy via an axillary-breast-shoulder approach by Yulian, et al. [8]. In this study, we present an initial retrospective analysis of the retroauricular approach for specific thyroid nodules, aiming to evaluate surgical safety, feasibility, and patient satisfaction with postoperative scarring, as well as tumor recurrence rates.
Methods
This retrospective study focused on women with thyroid nodules and was conducted at Dr. Cipto Mangunkusumo General Hospital, Jakarta, Indonesia, from January 2016 to April 2017.
Subjects
Before undergoing endoscopic thyroidectomy, candidates underwent standard preoperative diagnostic assessments, including clinical examinations, neck ultrasound, thyroid function tests, chest X-ray, and fine needle aspiration biopsy (FNAB). Chest X-rays were integrated into the preoperative diagnostic protocol to evaluate potential pulmonary involvement or abnormalities that could impact surgical planning or postoperative management.
Inclusion criteria for subjects selected for the endoscopic thyroidectomy procedure were as follows: (1) presence of a benign tumor (with a predominant thyroid nodule diameter of less than 5 cm) or a malignant thyroid nodule with a size less than 2 cm; (2) absence of evidence of metastasis to the lymph nodes or local invasion; (3) normal thyroid function; and (4) high motivation, particularly concerning aesthetic outcomes in a specific region [9, 10]. Candidates who had undergone previous surgery and irradiation, exhibited extra-thyroidal extension (ETE), adjacent organ invasion, retrosternal extension, suspicion of distant metastases based on preoperative imaging, or had poor general condition were excluded.
All subjects received comprehensive information regarding the advantages and disadvantages of the procedure, as well as the potential need for conversion to an open surgical method. Written informed consent was obtained from all patients before surgery.
Surgical procedure
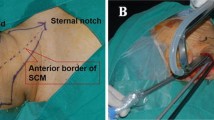
Under general anesthesia, the patient was positioned supine on the operative table with the head slightly rotated away (contralateral) from the side of the procedure. The neck was relaxed and not extended. Approximately 1 cm of hair was shaved along the occipital hairline, and then the incision line was marked along the post-auricular sulcus and continued on the occipital hairline inside the shaved area. The angle of the mandible, the v notch of the thyroid cartilage, the anterior border of the sternocleidomastoid (SCM) muscle, and the thyroid lobar bulge were also marked. At about the level of the tragus, the incision was extended posteriorly and then curved towards the occipital direction below the hairline (Fig. 1).
A subplatysmal plane was developed and the flaps were elevated above the SCM muscle, preserving the external jugular vein and great auricular nerve (GAN) (Fig. 1). Care was taken when approaching the anterior border of SCM, which connects the anterior jugular vein with the common facial vein. Flap elevation was continued superiorly to the lower border of the mandible, anteriorly along the anterior border of the SCM muscle to reveal the contralateral lobe of the thyroid gland, and inferiorly to the level of the sternal notch. The working space had to be sufficient for introducing the endoscopic instrument.
To establish the working space, an assistant held the subplatysmal flap with a retractor. The anterior border of the SCM was then visualized and retracted posteriorly to expose the carotid sheath, which was located laterally to the ipsilateral lobe of the thyroid gland. The ipsilateral omohyoid muscle and strap muscles were identified and dissected away from the thyroid gland, then lifted and secured by the retractor to reveal the ipsilateral thyroid lobe. It was maintained superiorly by the retractor to reveal the superior pole of the thyroid gland. Once the contour of the thyroid gland was fully exposed and sufficient working space was established, a self-retaining retractor was applied (Fig. 2). Then a 30° endoscope was introduced and held by another assistant on the superior side, and the main operator stood toward the inferior side.
While holding the superior pole by endoscopic forceps and pulling it laterally, the superior thyroid artery and the vein were divided using ultrasonic devices. The dissection was continued to the medial side by separating the thyroid from the cricothyroid muscle, and then dissection of the posterolateral area of the thyroid gland was performed by retracting the thyroid to the anteromedial side. Next, the thyroid gland was held and retracted in a superior to inferior manner, as it was being dissected off the trachea toward the lower pole. The dissection was carefully performed to identify and preserve the recurrent laryngeal nerve (RLN) and parathyroid glands. Appropriate retraction of the specimen was carefully done by medially turning the direction, taking care not to damage the previously identified RLN.
After detaching the specimen from the trachea and connecting Berry’s ligament, the specimen was removed (Fig. 3). The surgical bed was irrigated, and meticulous bleeding control was performed, then a closed suction drain was inserted behind the hairline (Supplementary Appendix 5). The wound was closed with simple interrupted sutures. All surgical procedures were performed by a single surgeon.
Surgical outcomes
Surgical outcomes were assessed from two perspectives: surgical parameters and scar satisfaction reported by the subjects.
Intraoperative outcomes consist of surgery duration, estimated blood loss, and instances of conversion to open surgical procedures. Postoperative outcomes included the length of hospital stay, duration of drain placement, pain intensity measured by the Visual Analog Scale (VAS), and satisfaction with scar appearance. A comprehensive analysis of complications was conducted, comprising voice hoarseness, earlobe numbness, temporary mouth corner deviation, hypocalcemia, hematoma, seroma, and surgical-site infections. Oncologic outcomes were determined by the final histopathological diagnosis and monitoring for tumor recurrence.
Subjects’ satisfaction was evaluated within six months following surgery. The evaluation was performed using the Vancouver Scale System, consisting of a 4-point satisfaction scale (1. Very satisfied; 2. Satisfied; 3. Unsatisfied; 4. Dissatisfied) [11].
Follow-up
Subjects underwent regular follow-up examinations, including physical assessments, ultrasound evaluations, and thyroid function tests, conducted at six-month intervals for up to two years to monitor for recurrence. All subjects received oral levothyroxine once daily (at a dose of 50 µg/day) to maintain normal thyroid-stimulating hormone levels.
Results
In this study, 31 subjects were included, primarily consisting of young adults with tumors ranging from 2 to 4 cm in size. Preoperative histological assessments revealed that 14 subjects (45.2%) had benign nodules (Supplementary Appendix 1). The most frequently performed procedure was isthmolobectomy, conducted in 26 subjects (83.9%). One subject out of the total 31 required open thyroidectomy (OT) due to tracheal injury (Table 1).
The mean total operative time, from skin incision to skin closure, was 154.2 ± 21.3 min, which comprised 47.3 ± 7.2 min for surgical pocket creation (time from skin incision to self-retaining retractor placement) and 92.2 ± 18.1 min for the endoscopic procedure. The average amount of blood loss during surgery was 69.2 ± 52.1 mL. Postoperative pain, as assessed by mean VAS scores, showed a decreasing trend from the first to the seventh day. The mean duration of drain placement post-surgery was 3.4 ± 0.99 days, with an average drain production of 50.7 ± 40.5 mL. The average length of hospital stay was 4.7 ± 2.2 days (Table 1).
Voice hoarseness due to temporary RLN injury, diagnosed via laryngoscope, was observed in 4 patients (12.9%) (Supplementary Appendix 2). Throughout the follow-up period, all complications were temporary and did not have any permanent impact on the overall condition of the patients.
Final histopathological findings following the initial lobectomy or isthmolobectomy are shown in (Supplementary Appendix 3). This study found that 12 subjects (38.7%) had nodular goiter, with no frozen biopsies conducted during surgery. Four of nine subjects with papillary carcinoma were identified with specific subtypes, which were two cases of tall cell variants and two with ETE. These four subjects subsequently underwent completion thyroidectomy in the second week following the initial procedure. Based on AMES classification, completion of thyroidectomy was deemed unnecessary for other cases categorized as low risk. The mean size of malignant nodules was 1.5 ± 1.4 cm.
Table 2 illustrates subjects’ satisfaction, with a majority (65.6%) expressing being “Very Satisfied.” Recurrence was evaluated based on clinical symptoms and routine imaging such as thyroid ultrasound, with a mean follow-up period of 7.29 ± 7.03 months (range 1–24 months). Three subjects experienced tumor recurrence: one (3.2%) on the tumor bed and two (6.5%) on the contralateral side, as shown in (Supplementary Appendix 4).
Discussion
Conventional open thyroidectomy often results in scarring and neck skin contractures, which may be aesthetically unpleasant for patients [2]. Sun et al. highlighted the high incidence of keloid in the Asian population, which leads to significant morbidity in younger women [12]. To address these concerns, remote access surgical techniques have been developed as an innovative solution to minimize scarring.
The concept of remote access surgery emerged in the 1980s, with the first head and neck endoscopic-assisted procedure performed by Gagner in 1996 [3]. Several portals for endoscopic thyroidectomy have since been introduced, including the transaxillary, axillary-breast-shoulder, retroauricular, and transoral routes [13]. The retroauricular approach began to develop when the transaxillary approach caused dramatic complications, which may be attributed to higher body mass indices [14]. Meanwhile, the retroauricular approach received considerable attention regarding its combination of Terris’ facelift parotidectomy, Chung’s gasless robotic thyroidectomy, and Lee’s retroauricular insufflation which was expected to be safer [1, 14,15,16].
The retroauricular approach provides a shorter and more direct route to the neck, requiring minimal dissection and providing adequate working space [2]. In a prior study, the area of dissection required in the retroauricular approach is 38% less than that in the transaxillary approach, potentially minimizing tissue trauma [17, 18]. Despite the unconventional positioning of the operator cranial to the thyroid, the familiarity of the facelift incision to head and neck surgeons is advantageous [2, 14].
According to The Global Cancer Observatory in 2020, in Indonesia, thyroid cancer ranks 12th among all cancers [19]. Dating from 2012 to 2016, there were 7,384 outpatient thyroid cases in Dr. Cipto Mangunkusumo General Hospital, a national referral hospital in Indonesia, with approximately 68.7% being thyroid nodule cases [20].
As an initial investigation, we conducted gasless endoscopic lobectomy and isthmolobectomy using the retroauricular approach in 31 female subjects presenting with thyroid nodules, with an average participant age of 35 years. Given the concern for malignancy, the subjects were monitored for two years.
Regarding surgical outcome, blood loss, length of stay, drain placement, and postoperative pain were within good ranges. In this study, the mean total operative time was 154.2 ± 21.3 min, which comprised 47.3 ± 7.2 min of surgical pocket creation and 92.2 ± 18.1 min of endoscopic thyroidectomy procedure. The additional time needed for skin flap elevation and working space creation contributed to longer operation time compared to the conventional method. However, the surgical pocket creation provides an adequate working space; hence the tumor size is not a limitation of this study. Notably, Yulian, et al. highlighted tumor size as a limitation in the axillary-breast-shoulder approach; therefore, gas insufflation is needed to provide a large working space [8].
In our study, we observed a prolonged mean operative time. In comparison to procedures such as transoral endoscopic or robot-assisted thyroidectomy, our approach required less time than the bilateral axillo-breast approach (BABA), which averaged 190 min [21]. However, it exhibited a longer duration to the transoral endoscopic thyroidectomy vestibular approach (TOETVA) at 134.11 ± 31.48 min and the breast at 84.70 min [22, 23].
Comparing our findings to other studies on retroauricular endoscopic thyroidectomy, our results were like those reported by Lee et al., where the mean total operative time was 152 ± 48 min. In their study, the mean flap creation time was 75 ± 24 min, and the mean endoscopic procedure time was 58 ± 18 min [18]. Similarly, the endoscopic cephalic access thyroid surgery (EndoCATS) utilizing the retroauricular approach reported a mean operation time of 132.79 ± 50.52 min [24]. However, it was longer than the Minimally Invasive Video-Assisted Thyroidectomy (MIVAT) reported in Miccoli’s study (1999) at 87 min or in Berti’s study (2004) at 56.90 min [25, 26]. Although our operative time was long, it is expected to decrease after with increasing case volume [27].
The major limitation of this method comes from the necessity of bilateral retroauricular incision when total thyroidectomy is indicated [18]. Other limitations include 2-dimensional visualization, limited instrument movement due to the rigidity of the endoscope, the fulcrum effect, and potential collisions between the operator and assistant [2, 28]. Overcoming these limitations necessitates surgeons' proficiency in handling endoscopic instruments and familiarity with the endoscopic surgical view [29].
Robotic systems are anticipated to address these limitations by enhancing the maneuverability of robotic arms in comparison to conventional rigid endoscopic instruments [2]. However, their accessibility remains limited in many medical facilities, especially in developing nations [2]. Yoo, et al. reported that the average cost of endoscopic thyroidectomy was $829, significantly lower than robotic thyroidectomy which costs eight times as much yet yields equivalent outcomes [2]. In our investigation, the endoscopic approach remains cost-effective and worthy of further advancement.
Despite the numerous advantages of this approach, prioritizing patient safety remains paramount in this study. We observed several complications, including voice hoarseness, earlobe numbness, transient mouth corner deviation (MCD), tracheal injury, skin flap necrosis, and hypertrophic scarring. Despite this being our inaugural experience with the retroauricular approach, no instances of mortality or permanent complications occurred.
The occurrence of voice hoarseness, a common complication following thyroidectomy procedures, warrants further discussion. Partial necrosis of the skin flap in one subject along the angular margin of the incision was noted, highlighting a potential complication associated with the surgical technique. Previous studies have suggested that modifying the angle of the incision and ensuring adequate thickness of the cutaneous flap can mitigate the risk of necrosis [30].
Regarding the observed high number of vocal cord paralysis (VCP) cases, it is crucial to consider potential contributing factors. Voice hoarseness, which manifested in 4 patients (12.9%) in our study, is a well-recognized complication following thyroidectomy. All patients underwent postoperative laryngoscopy during the follow-up period, confirming the temporary nature of the condition. These cases were resolved in 3, 4, 6, and 8 weeks, respectively.
Several factors may contribute to the occurrence of voice hoarseness post-thyroidectomy, including thermal damage from the use of ultrasonic scalpels and limitations in instrument movement within the surgical site. These factors can potentially affect the integrity of the recurrent laryngeal nerve, resulting in temporary vocal cord paralysis and subsequent voice hoarseness.
One subject (3.2%) experienced 1 cm perforation on the anterior side of the trachea. The injury was detected early during the procedure, then surgery was converted to open thyroidectomy. This event occurred to the initial subject of this study. Later, the injury healed well and the subject was fully recovered during the follow-up period. Early diagnosis, proper preparation, and effective communication within the surgical team are the keys to the successful management of tracheal injury [31].
Earlobe numbness (9.6%) and MCD (6.4%) were specific complications that occurred due to the transient damage of the nerve from the dissection area of the retroauricular approach. Temporary MCD was the result of indirect injury of the marginal mandibular nerve, meanwhile, the earlobe numbness was the result of indirect injury to the GAN [18]. To prevent numbness around the earlobe, surgeons can carefully preserve the sensory nerves overlying the sternocleidomastoid muscles which innervates the region during the elevation of the long and wide skin flap. Direct identification along the mandible angle from the parotid gland or upward retraction after ligation of the facial vein may lower the risk of marginal mandibular nerve injury [32]. In this study, these complications were managed with pain control and reported to be normal within four weeks after surgery.
The white arrows show minimal scar appearance.
The postoperative scar appearance is shown in Fig. 4. Most subjects (65.6%) were very satisfied with the scar appearance. Several studies also showed subjects’ satisfaction with the scar appearance resulting from the retroauricular approach [2, 5, 13, 18]. This is probably because in retroauricular thyroidectomy, the scar is hidden by hair and placed in a location that cannot be seen with a mirror. One patient (3.2%) was unsatisfied because of the keloid. Keloids are prone to occur in Asians and Africans, including Indonesians [12].
The follow-up was continued for two years after the postoperative period, considering there were six subjects (19.3%) having adenomatous goiter with focus papillary carcinoma, nine subjects (29%) with papillary carcinoma, and one subject (3.2%) with Hashimoto thyroiditis. Originally, endoscopic thyroidectomy was safe and feasible for benign thyroid nodules and controversial for malignancy case management [33]. Kitano et al. noted that an endoscopic approach in thyroid malignancy cases can be performed when the patients are < 45 years old, the tumor size is < 2 cm, and no evidence of lymph node or local invasion [34]. In several studies, technical safety between open and endoscopic thyroidectomy is not significantly different in malignancy cases [33, 35, 36].
In our study, one subject (3.2%) out of 31 experienced tumor recurrence at the site of the original tumor bed. This finding aligns with previous studies reporting cases of tumor seeding around the tumor bed, possibly due to tumor spillage during manipulation or traumatic handling of the tumor, particularly in cases where surgeons are less familiar with the endoscopic technique [37, 38]. Bakkar et al. study in robot-assisted thyroid surgery (RATS) suggested the importance of careful patient selection, especially in high-risk tumors which need adherence to fundamental onco-surgical principles, such as ensuring adequate local control and direct exposure of the lesion during surgery. The fractured specimen retrieved in two fragments in Bakkar’s may have contributed to track seeding, suggesting that routine retrieval of resected specimens using a bag, regardless of their nature and size to mitigate this risk. Furthermore, the consideration of converting to conventional open thyroidectomy in the event of a fractured surgical specimen is deemed a reasonable adaptation [39].
Two subjects (6.5%) in our study experienced tumor recurrence on the contralateral side. This recurrence may be attributed to the multicentricity characteristics of papillary carcinoma, despite being classified as low risk [40]. Nevertheless, while endoscopic thyroidectomy (ETE) management in the retroauricular approach demonstrates technical feasibility and safe intraoperative outcomes with comparable surgical outcomes, the oncologic safety of the procedure for thyroid cancer warrants further investigation [36].
Considering the standard of care until recently, total thyroidectomy (TT) followed by adjuvant radioactive iodine (RAI) has been advocated for patients with differentiated thyroid cancer (DTC), resulting in excellent prognosis with a 10-year overall survival of 98–99% and recurrence rates of 1–3% in low-risk DTC cases [41]. However, recent studies have shed light on the comparative outcomes of hemithyroidectomy (HT) versus TT. Notably, one study found that the HT cohort exhibited higher 10-year recurrence rates of 18.3% compared to 7.5% in the TT cohort (hazard ratio, HR 1.71, p = 0.003). [42] Subsequent reanalysis of the same data also highlighted that TT was associated with better overall survival in patients with papillary thyroid cancers (PTC) > 2 cm when considering histological data (HR 1.53, CI 1.06–2.19, p = 0.023). [43, 44] Furthermore, a systematic review of included studies reporting recurrence data revealed pooled recurrence rates of 9.0% for HT compared to 7.4% for TT, indicating a significantly higher risk of recurrence associated with HT (odds ratio, OR, 1.45; CI 1.16–1.81, p = 0.001). [45] These rates, in comparison, suggest that our study’s recurrence rate is not notably elevated.
We realize that our study has limitations. This is an early study using a retrospective design and a small number of subjects at a single institution with a relatively short follow-up. Prospective randomized controlled studies to specifically compare the tumor recurrence and long-term safety of this method are necessary. However, we are thrilled to share our early experiences in improving a surgical technique in the interest of patient treatment and satisfaction.
Conclusion
Our study has shown that endoscopic thyroidectomy via retroauricular approach is safe, feasible, and esthetically acceptable as an alternative to the conventional one. Gas insufflation is not necessary in this approach. A high-volume surgeon in conventional open thyroidectomy is needed to minimize the number of mortality and complications in the endoscopic approach. In the oncological aspect, the follow-up period needs to be longer to evaluate the tumor recurrence. Thus, we recommend an extended follow-up period of up to ten years and a larger case volume to provide a better representation of subjects who undergo a retroauricular approach.
The findings of this study underscore the importance of exercising caution when considering the gasless retroauricular approach endoscopic isthmolobectomy due to the observed high number of complications. While this approach offers potential benefits, such as reduced scarring and improved cosmetic outcomes, the occurrence of numerous complications emphasizes the need for meticulous patient selection, thorough preoperative evaluation, and careful surgical technique. Further research and refinement of surgical protocols may help mitigate the incidence of complications and enhance patient safety in the future.
References
Lee KE, Kim HY, Park WS, Choe JH, Kwon MR, Oh SK et al (2009) Postauricular and axillary approach endoscopic neck surgery: a new technique. World J Surg 33:767–772. https://doi.org/10.1007/s00268-009-9922-8
Lira RB, Chulam TC, Koh YWW, Choi ECC, Kowalski LP (2016) Retroauricular endoscope-assisted approach to the neck: early experience in Latin America. Int Arch Otorhinolaryngol 20:138–144. https://doi.org/10.1055/s-0036-1578807
Gagner M (1996) Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg 83:875. https://doi.org/10.1002/bjs.1800830656
Lee DY, Baek SK, Jung KY (2017) Solo-surgeon retroauricular approach endoscopic thyroidectomy. J Laparoendosc Adv Surg Tech 27:63–66. https://doi.org/10.1089/lap.2016.0140
Alabbas H, Ali DB, Kandil E (2016) Robotic retroauricular thyroid surgery. Gland Surg 5:603–606. https://doi.org/10.21037/gs.2016.12.06
Kartini D, Wibisana G (2017) Accuracy of triple diagnostic test in patients with thyroid nodule at Dr. Cipto Mangunkusumo General Hospital. E J Kedokteran Indonesia https://doi.org/10.23886/ejki.5.7603.38-43
Pemayun TGD (2016) Current diagnosis and management of thyroid nodules. Acta Med Indones 48:247–257
Yulian ED, Kurnia A, Kartini D, Melati PA (2020) Endoscopic thyroidectomy via axillary-breast-shoulder approach: early experience of 42 cases. Surg Oncol 34:318–323. https://doi.org/10.1016/j.suronc.2020.05.007
Kim YS, Joo KH, Park SC, Kim KH, Ahn CH, Kim JS (2014) Endoscopic thyroid surgery via a breast approach: a single institution’s experiences. BMC Surg 14:49. https://doi.org/10.1186/1471-2482-14-49
Yang Y, Gu X, Wang X, Xiang J, Chen Z (2012) Endoscopic thyroidectomy for differentiated thyroid cancer. Scient World J. https://doi.org/10.1100/2012/456807
Elzahaby IA, Fathi A, Abdelwahab K, Eldamshiety O, Metwally IH, Abdallah A, et al (2018) Endoscopic Thyroidectomy Using the Unilateral Axillo-breast Approach Versus the Modified Anterior Chest Wall Approach: A Prospective Comparative Study. Surg Laparosc Endosc Percutan Tech 28:366–70. https://doi.org/10.1097/SLE.0000000000000582 LK - http://findit.library.jhu.edu/resolve?sid=EMBASE&issn=15344908&id=doi:10.1097%2FSLE.0000000000000582&atitle=Endoscopic+Thyroidectomy+Using+the+Unilateral+Axillo-breast+Approach+Versus+the+Modified+Anterior+Chest+Wall+Approach%3A+A+Prospective+Comparative+Study&stitle=Surg.+Laparoscopy+Endosc.+Percutaneous+Tech.&title=Surgical+Laparoscopy%2C+Endoscopy+and+Percutaneous+Techniques&volume=28&issue=6&spage=366&epage=370&aulast=Elzahaby&aufirst=Islam+A.&auinit=I.A.&a.
Sun LM, Wang KH, Lee YCG (2014) Keloid incidence in Asian people and its comorbidity with other fibrosis-related diseases: a nationwide population-based study. Arch Dermatol Res 306:803–808. https://doi.org/10.1007/s00403-014-1491-5
Terris DJ, Singer MC, Seybt MW (2011) Robotic facelift thyroidectomy: II. Clinical feasibility and safety. Laryngoscope 121:1636–1641. https://doi.org/10.1002/lary.21832
Shaha AR, Nathan C-A, Fernandes JK, de Souza C, Joshi SR (eds) (2020) Surgical and Medical Management of Diseases of the Thyroid and Parathyroid. Plural Publishing, San Diego
Terris DJ, Tuff KM, Fee WE (1994) Modified facelift incision for parotidectomy. J Laryngol Otol 108:574–578. https://doi.org/10.1017/S002221510012746X
Kang SW, Jeong JJ, Yun JS, Sung TY, Lee SC, Lee YS et al (2009) Robot-assisted endoscopic surgery for thyroid cancer: experience with the first 100 patients. Surg Endosc 23:2399–2406. https://doi.org/10.1007/s00464-009-0366-x
Singer MC, Seybt MW, Terris DJ (2011) Robotic facelift thyroidectomy: I. Preclinical simulation and morphometric assessment. Laryngoscope 121:1631–1635. https://doi.org/10.1002/lary.21831
Lee DY, Baek SK, Jung KY (2016) Endoscopic thyroidectomy retroauricular approach. Gland Surg 5:327–335. https://doi.org/10.21037/gs.2015.10.01
The Global Cancer Observatory. Globocan 2018 2020;256:1–2
Harbuwono DS, Soewondo P, Yunir E, Soebardi S, Darmowidjojo B, Purnamasari D et al (2019) Diagnostic approach for thyroid nodules. Acta Med Indones 51:189–193
Kwon H, Koo DH, Choi JY, Kim E, Lee KE, Youn YK (2013) Bilateral axillo-breast approach robotic thyroidectomy for graves’ disease: an initial experience in a single institute. World J Surg 37:1576–1581. https://doi.org/10.1007/s00268-013-2027-4
Jitpratoom P, Ketwong K, Sasanakietkul T, Anuwong A (2016) Transoral endoscopic thyroidectomy vestibular approach (TOETVA) for Graves’ disease: a comparison of surgical results with open thyroidectomy. Gland Surg 5:546–552. https://doi.org/10.21037/gs.2016.11.04
Li ZY, Wang P, Wang Y, Xu SM, Cao LP, Que RS (2010) Endoscopic thyroidectomy via breast approach for patients with graves’ disease. World J Surg 34:2228–2232. https://doi.org/10.1007/s00268-010-0662-6
von Ahnen T, Wirth U, von Ahnen M, Kroenke J, Busch P, Schardey HM et al (2022) Endoscopic cephalic access thyroid surgery (EndoCATS) using the retroauricular approach – a single centre retrospective data analysis. Surg Endosc 36:117–125. https://doi.org/10.1007/s00464-020-08244-6
Miccoli P, Berti P, Conte M, Bendinelli C, Marcocci C (1999) Minimally invasive surgery for thyroid small nodules: preliminary report. J Endocrinol Invest 22:849–851. https://doi.org/10.1007/BF03343657/METRICS
Berti P, Materazzi G, Galleri D, Donatini G, Minuto M, Miccoli P (2004) Video-assisted thyroidectomy for Graves’ disease: report of a preliminary experience. Surg Endosc Other Interv Tech 18:1208–1210. https://doi.org/10.1007/s00464-003-9225-3
Yu J, Rao S, Lin Z, Pan Z, Zheng X, Wang Z (2019) The learning curve of endoscopic thyroid surgery for papillary thyroid microcarcinoma: CUSUM analysis of a single surgeon’s experience. Surg Endosc 33:1284–1289. https://doi.org/10.1007/s00464-018-6410-y
Aidan P, Arora A, Lorincz B, Tolley N, Garas G (2018) Robotic thyroid surgery: current perspectives and future considerations. Orl 80:186–194. https://doi.org/10.1159/000488354
Byeon HK, Holsinger FC, Tufano RP, Park JH, Sim NS, Kim WS et al (2016) Endoscopic retroauricular thyroidectomy: preliminary results. Surg Endosc 30:355–365. https://doi.org/10.1007/s00464-015-4202-1
Roh JL (2005) Retroauricular hairline incision for removal of upper neck masses. Laryngoscope 115:2161–2166. https://doi.org/10.1097/01.MLG.0000181496.22493.5A
Kumar S, Kaushal A, Shamim R (2017) Delayed tracheal perforation, a rare but dreaded complication of thyroidectomy. Saudi J Anaesth 11:351–352. https://doi.org/10.4103/sja.SJA_637_16
Roh JL (2006) Removal of the submandibular gland by a retroauricular approach. Arch Otolaryngol Head Neck Surg 132:783–787. https://doi.org/10.1001/archotol.132.7.783
Sgourakis G, Sotiropoulos GC, Neuhäuser M, Musholt TJ, Karaliotas C, Lang H (2008) Comparison between minimally invasive video-assisted thyroidectomy and conventional thyroidectomy: is there any evidence-based information? Thyroid 18:721–727. https://doi.org/10.1089/thy.2008.0028
Kitano H, Fujimura M, Kinoshita T, Kataoka H, Hirano M, Kitajima K (2002) Endoscopic thyroid resection using cutaneous elevation in lieu of insufflation. Surg Endoscopy Intervent Techn 16:88–91. https://doi.org/10.1007/s004640080197
Jong JJ, Kang SW, Yun JS, Tae YS, Seung CL, Yong SL et al (2009) Comparative study of endoscopic thyroidectomy versus conventional open thyroidectomy in papillary thyroid microcarcinoma (PTMC) patients. J Surg Oncol 100:477–480. https://doi.org/10.1002/jso.21367
Chung YS, Choe JH, Kang KH, Kim SW, Chung KW, Park KS et al (2007) Endoscopic thyroidectomy for thyroid malignancies: Comparison with conventional open thyroidectomy. World J Surg 31:2302–2306. https://doi.org/10.1007/s00268-007-9117-0
Kim H, Kim TH, Choe J-H, Kim J-H, Kim JS, Oh YL et al (2017) Patterns of initial recurrence in completely resected papillary thyroid carcinoma. Thyroid 27:908–914. https://doi.org/10.1089/thy.2016.0648
Jung JS, Kim SY, Jung HY, Han SW, Lee JE, Lee DY (2017) Simultaneous seeding of follicular thyroid adenoma both around the operative bed and along the subcutaneous tunnel of the upper chest wall after endoscopic thyroidectomy. J Korean Soc Radiol 76:138. https://doi.org/10.3348/jksr.2017.76.2.138
Bakkar S, Frustaci G, Papini P, Fregoli L, Matteucci V, Materazzi G et al (2016) Track recurrence after robotic transaxillary thyroidectomy: a case report highlighting the importance of controlled surgical indications and addressing unprecedented complications. Thyroid J 26:559561. https://doi.org/10.1089/THY.2015.0561
Zhang XJ, Yang T, Li SH, Liu D, Bin XuD, Li H et al (2016) Multicentric papillary thyroid carcinoma: a clinical analysis of 221 patients. Int J Clin Exp Pathol 9:5680–5686
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE et al (2016) 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the american thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26:1–133. https://doi.org/10.1089/thy.2015.0020
Hwangbo Y, Kim JM, Park YJ, Lee EK, Lee YJ, Park DJ et al (2017) Long-term recurrence of small papillary thyroid cancer and its risk factors in a Korean multicenter study. J Clin Endocrinol Metab 102:625–633. https://doi.org/10.1210/jc.2016-2287
Rajjoub SR, Yan H, Calcatera NA, Kuchta K, Wang CHE, Lutfi W et al (2018) Thyroid lobectomy is not sufficient for T2 papillary thyroid cancers. Surgery (United States) 163:1134–1143. https://doi.org/10.1016/j.surg.2017.12.026
Adam MA, Pura J, Gu L, Dinan MA, Tyler DS, Reed SD et al (2014) Extent of surgery for papillary thyroid cancer is not associated with survival. Ann Surg. https://doi.org/10.1097/SLA.0000000000000925
Chan S, Karamali K, Kolodziejczyk A, Oikonomou G, Watkinson J, Paleri V et al (2020) Systematic review of recurrence rate after hemithyroidectomy for low-risk well-differentiated thyroid cancer. Eur Thyroid J 9:73–84. https://doi.org/10.1159/000504961
Acknowledgements
The authors thank all the operating room crew, surgical oncology fellows, surgical residents, and the research unit of the Department of Surgery, Faculty of Medicine Universitas Indonesia, Dr. Cipto Mangunkusumo General Hospital, Jakarta, Indonesia.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
EDY contributed to the study conception, methodology, and surgical procedure. EDY, SSP, and PAM contributed to data collection, data analysis, drafting of the article, writing-reviewing, and editing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest.
Ethical approval
The research conducted with human participants adhered to the ethical standards set forth by the institutional and/or national research committee, as well as the 1964 Helsinki Declaration and its subsequent revisions, or equivalent ethical guidelines.
Human and animal rights
All procedures were approved by the Faculty of Medicine Universitas Indonesia Ethical Clearance Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yulian, E.D., Panigoro, S.S. & Melati, P.A. Retroauricular endoscopic thyroidectomy: initial single-institution experiences. Updates Surg (2024). https://doi.org/10.1007/s13304-024-01855-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13304-024-01855-x