Abstract
Repair of an incisional hernia (IH) generates costs on several levels and domains of society. The aim of this study was to make a complete cost analysis of incisional hernia repair (IHR) with synthetic and biological mesh and to compare it with financial reimbursement. Patients were grouped into three levels to determine the complexity of their care, and hence, the costs involved. Group 1 included patients without comorbidities, who underwent a “standard” incisional hernia repair (SIHR), with synthetic mesh. Group 2 included patients with comorbidities, who underwent the same surgical procedure. Group 3 included all patients who underwent a “complex” IHR (CIHR) with biological mesh. Total costs were divided into direct (including preoperative and operative phases) and indirect costs (medications and working days loss). Reimbursement was calculated according to Diagnosis-Related Group (DRG). From 2012 to 2014, 76 patients underwent prosthetic IHR: group 1 (35 pts); group 2 (30 pts); and group 3 (11 pts). The direct costs of preoperative and operative phases for groups 1 and 2 were €5544.25 and €5020.65, respectively, and €16,397.17 in group 3. The total reimbursement in the three groups was €68,292.37 for group 1, €80,014.14 for group 2, and €72,173.79 for group 3, with a total loss of €124,658.43, €69,675.36, and €100,620.04, respectively. All DRGs underestimate the costs related to IHR and CIHR, thus resulting in an important economic loss for the hospital. The cost analysis shows that patient-related risk factors do not alter the overall costs. To provide a correct “cost-based” reimbursement, different DRGs should be created for different types of hernias and prostheses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Incisional hernias are a common complication in abdominal surgery. Despite many studies on the optimal closing technique, their incidence reaches 10–11% among patients who undergo laparotomy [1]. Some patient-related risk factors have been identified, such as: smoking habits, diabetes, obesity, malnutrition, steroid use, chronic obstructive pulmonary disease (COPD), and recent chemotherapy. Nevertheless, a correct method for prevention has not been developed yet.
The repair of ventral IH remains a challenging surgical problem and outcomes are often disappointing.
Many procedures have been proposed for IHR. In several studies, the relapse rate ranges from 12 to 50% [1, 2] with the use of direct herniorrhaphy, to 19–32% [1, 3, 4] with the use of prosthetic materials. The prosthetic approach should be considered mandatory for defects >2 cm [5]. Synthetic meshes are not recommended in wound and/or mesh infection, in clean-contaminated cases, in those with concurrent intra-abdominal procedures, and in complex hernia repair if the mesh comes in contact with the intraperitoneal cavity. In these cases, biological meshes are now available [5, 6]. The financial impact of using a biological mesh is still not well known.
The repair of an incisional hernia generates costs on several levels of society.
The aim of this study was to make a complete cost analysis of incisional hernia repair with synthetic mesh and biological mesh and to compare it with the financial support received by our Institute according to DRG [7].
Materials and methods
This study was performed in collaboration with the Management Control System of the Hospital of Padua, Italy.
Eligible patients were those with diagnosis of incisional hernia, considered as the main surgical indication.
Exclusion criteria were: inability to provide the informed consent; out-patients; direct herniorrhaphy; and age younger than 18.
The decision to use synthetic or biological mesh was based on hernia features, as described in the following. We divided patients into three groups:
-
1.
“Standard” incisional hernia repair type 1 (group 1) Surgical repair of IH with synthetic mesh in patients without comorbidity: ventral hernia working group (VHWG) grade I hernia [5]. The cost of consumables and drugs was calculated for incisional hernia repair according to Rives technique with a hernia defect of 10 cm, considering it as the prototype of this operation.
-
2.
“Standard” incisional hernia repair type 2 (group 2) Surgical repair of IH with synthetic mesh in patients with comorbidity, without history of wound infection (VHWG grade II hernia). Comorbidities considered as risk factors for complications, according to Ventral Hernia Working Group, are smoking habit, obesity, immunosuppression, and COPD [5]. These diseases concurred in determining physical status classification (ASA >1).
-
3.
“Complex” incisional hernia repair (group 3) Surgical repair of IH requiring a biological mesh, as in VHWG grades III and IV: (a) wound and/or mesh infection; (b) mesh in contact with the intraperitoneal cavity; (c) clean-contaminated cases; and (d) concurrent intra-abdominal procedure (ostomy reversal, bowel resection, and fistulotomy) [5].
Hernia grading system as per The Ventral Hernia Working Group is shown in Table 1.
The costs analysis included direct and indirect costs.
We performed a complete health economics analysis of IHR. The analysis included only direct costs, expressed in Euros, because not all indirect costs could be monetized.
Direct costs
In the cost analysis, we considered the following phases for each type of intervention: preoperative phase, operative phase, and immediate postoperative phase.
The preoperative phase included instrumental investigations, such as computerized tomography (CT) and magnetic resonance imaging (MRI) of the abdominal wall.
The operative phase (surgical operation) included personnel costs (surgeons, anesthesiologist, and nurses) and calculated for all units involved and for the hours of surgical operation, costs of disposable materials and drugs, cost of sterilization, and general costs (depreciation, management, and administration).
The postoperative phase included costs of ward and intensive care unit (ICU) stay. The service management control of the Hospital provided us with updated costs. The biological mesh (fascia lata or pericardium allograft) was provided by the tissue bank of Treviso (Italy), through the Plastic Surgery department of our Hospital.
Indirect costs
Indirect costs included those related to outpatient medications and working days’ loss; only outpatient medications could be monetized.
Reimbursement rates
In the International classification of Diseases, 9th revision, Clinical Modification (ICD-9CM), the code for incisional hernia is 553.21 and for its surgical operation is 5361 (IHR with mesh).
According to the official classification at the time of the study in Veneto region (Italy), IHR with mesh was categorized in DRG 160, without CC (complicating and concomitant diseases) or DRG 159 with CC (incisional hernia repair with CC) [7].
DRG 160 also includes other hernia repairs (mainly umbilical hernias), excluded from our database.
Our data excluded the diagnosis 551.20 and 552.20 (IH with obstruction and strangulation), since the IHR is made by direct suture in emergency situations (contaminated, clean-contaminated cases and/or those with concurrent intra-abdominal procedures: ostomy, bowel resection, and fistulotomy).
The reimbursement for DRG 160 was €1704.03 and for DRG 159 was €3475.47.
The other reimbursements for DRG in our series are listed in Table 2.
Statistical analysis
The data set was analyzed as a whole sample and stratified by the type of mesh and the presence or absence of complications and comorbidities (groups 1, 2, and 3). Qualitative data were reported as counts and percentages. For quantitative variables, we recorded the median and the interquartile range. Proportions were compared with the Chi-square test. The statistical significance of differences between median values was tested using Wilcoxon’s rank sum test. For each test, the threshold for statistical significance level was set at 0.05. Statistical analyses were performed using the SPSS package, version 22.
Results
Clinical data
From January 2012 to November 2014, 76 patients (35 male and 41 females, median age 64 years) underwent prosthetic IHR; a synthetic mesh (polypropylene) was used in 65 (86%), a biological mesh (homologous tissue in 10 and heterologous tissue in 1) in 11 (14%). In most patients (58), IHR according to Rives was performed, while in few cases, other techniques were used: mesh in contact with the intraperitoneal cavity (4), Ramirez (3), Chevrel (8), and other techniques (3). Groups 1 and 2 did not differ in age (66.1 vs 65.5, p = 0.80) and sex.
Clinical data and their comparison are shown in Table 3.
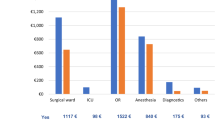
Direct costs
Description of DRG and equivalent reimbursement costs are reported in Table 2.
Details on times and costs of IHR in groups 1, 2, and 3 are shown in Tables 4 and 5.
“Standard” IHR type 1 (35 pts)
The median surgery time was 140 min and the median time spent by the patient in the operating room was 312 min. The median of hospital stay was 7 days. Total costs were €5544.25.
In group 1, 31 patients (89%) had DRG 160 and 4 (11%) had DRG 151.
“Standard” IHR type 2 (30 pts)
The costs of preoperative examinations, disposable materials, drugs, and sterilization were the same as in the first group. The median surgery time (123 min) and the median time spent by the patient in the operating room (290 min) can be considered comparable; the median length of hospital stay was the same (7 days).
The total cost of surgical operation was €5020.65.
In this group, 17 patients (56%) had DRG 160, 9 (30%) had DRG 159, 2 (7%) had DRG 150, and 2 (7%) had DRG 151.
“Complex” IHR (11 pts)
The characteristics of group 3 are shown in Tables 4 and 6. The surgery time was 360 min and the time spent by the patient in the operating room was 505 min. The cost of disposal materials and drugs was similar between this group and the other groups, except for prosthetic materials costs.
Biological mesh is more expensive and the price ranges from €1700 to €9396 based on the number of pieces and the size of the tissue used to fill the abdominal defect.
Five patients required hospitalization in the ICU for a median time of 2 days. The median overall hospital stay was 13 days.
Six different DRGs were considered for these patients.
For example, in a complex abdominal wall reconstruction, DRG code is 160 and the reimbursement does not even cover the cost of the mesh (€2316).
The total cost differences between standard and complex IHR (with synthetic and biological meshes) depend on preoperative investigations, personnel, mesh, and hospitalization (ward and ICU stay) and are statistically significant, as shown in Table 5.
Indirect costs
Indirect costs include medications and working days’ loss. In our series, 12/76 (16%) patients required ambulatory care, for a total of 100 medications (total cost: €1512).
A mean of 21 working days were lost in the synthetic mesh group vs 30 days in the biological mesh group.
Reimbursement analysis
-
1.
The direct cost for each patient’s individual hospitalization in group 1 was €5544.25 with a total cost of €194,048.75 between January 2012 and June 2014.
The reimbursement for DRG 160 was €1704.03 and for DRG 151 €3866.86, resulting in a total reimbursement of €68,292.37 and a total loss of €125,756.38.
-
2.
The cost for each individual hospitalization of patients in group 2 was €5020.65, with a total cost of €149,689.50 between January 2012 and June 2014. The reimbursement for DRG 160 was €1704.03, DRG 159 €3475.47, DRG 151 €3866.86, and DRG 150 €6016.34, resulting in a total reimbursement of €80,014.14 and a total loss of €69,675.36.
-
3.
The cost for each individual hospitalization of patients in group 3 ranges between €13,420.87 and €22,038 with a total cost of €172,793.83 between January 2012 and June 2014. The reimbursement was €72,173.79, resulting in a total loss of €100,620.04.
Comparison between costs and DRG reimbursement is shown in Fig. 1.
Discussion
Incisional hernia can present a wide range of clinical features, thus determining the development of various classification systems [5, 8]. In complex cases, the incisional hernia repair can be a true reconstruction of the abdominal wall.
In the literature, there are many studies on IH, a common surgical disease, but only a few of them analyze in detail the economic and social costs of the disease, as we do in our study. A systematic review of the literature underlines that little is known about the costs of IHR [9].
It is difficult to decrease the incidence of IH and this fact results in an increase of costs for the healthcare system.
The use of mesh in open incisional ventral hernia repair is superior to direct herniorrhaphy in terms of recurrence; the placement of a mesh becomes mandatory in elective surgery for IH (defects >2 cm) if the repair is not associated with other intra-abdominal surgical procedures. The standard mesh is polypropylene prosthesis, as it limits the cost.
In 2009, Finan et al. performed a cost-utility analysis comparing open suture vs mesh repair [10]. In the study, the costs for open suture compared with mesh repair were similar ($16,355 vs $16,947), but mesh repair proved to be a more effective treatment, with 73.8% of recurrence-free patients at 3-year follow-up, compared with 56.3% in the open suture group. They concluded that in subjects without contraindication to mesh placement, open mesh repair is the most effective surgical treatment for ventral hernia repair, with a lower risk of recurrence. Polypropylene mesh is highly discouraged in large infected IHs; in these cases, biological implants represent a viable alternative.
In our Italian series, the criteria for the use of biological mesh were the following: (1) the presence of wound and/or mesh infection; (2) contact between mesh and intraperitoneal cavity; (3) clean-contaminated cases; (4) concurrent intra-abdominal procedures (ostomy reversal, bowel resection, and fistulotomy); and (5) complex elective IHs in which a true reconstruction of the abdominal wall was mandatory (the “disasters of the wall”).
This study was performed in Italy and the cost analysis was conducted according to Italian reimbursement rates.
The cost analysis included direct and indirect costs, but only direct costs could be completely monetized.
To analyze the association of risk factors and costs, we divided patients with “standard” IH into two groups that were homogeneous in the number of patients, sex, and age, but differed in the absence (group 1) and presence (group 2) of patient-related risk factors (body mass index—BMI and ASA).
The analysis of the direct costs for these two groups showed that patient-related risk factors (smoking habit, obesity, malnutrition, steroid use, COPD, diabetes, and recent chemotherapy) do not alter the overall cost.
The direct costs in our study appeared to be in accordance with those of Reynolds [11]: in fact, in his work, the direct costs for IHR with synthetic mesh were $7590.
Despite our cost analysis showed no significant difference between the costs in groups 1 and 2, the reimbursement was still different in the two groups, according to DRG 160 and DRG 159. In addition, if another procedure was associated with the IHR (adhesiolysis, for instance) in groups 1 and 2, it would become the main procedure and its DRG (150 or 151) would replace the DRG of the IHR (159 or 160), thus providing a greater reimbursement. However, this reimbursement is still not sufficient to cover the costs of IHR, thus causing a great economic loss to the hospital.
In our series, hospitalization in groups 1 and 2 had the same length (7 days), which was longer than in other series [12]; in fact, to reduce the incidence of seromas and hematomas, we prefer to maintain drainages for a longer time.
The difference in costs of biological vs synthetic mesh repairs depends on the characteristics of group 3 hernias. In fact, these required a more complex repair, with a higher number of hours of intervention and a longer stay in the operating room; therefore, a true comparison between group 1/2 and group 3 is not possible. The higher costs in group 3 also depend on the more expensive material of the prosthesis and on a longer hospital stay, with a further need of ICU monitoring.
The third group includes a limited series of patients (only 11) but six different codes. In fact, despite all patients had a main diagnosis of incisional hernia, in some of them, another procedure (bowel resection, ostomy) was added and this became the main procedure during the codification process. Therefore, the different codes in our series depend on the procedure associated with IHR.
When the IHR with biological mesh is the only surgical procedure performed, its DRG code is 160 and its reimbursement is €1704.03; the reimbursement does not even cover the cost of the mesh.
In addition, in group 3, our data appeared to be in accordance with those of Reynolds [11], whose direct costs for IHR with biological mesh were $16,970.
Mesh materials represent a significant component of operating room supply costs and the use of biological mesh has been demonstrated to increase the cost of IHR [11]. In addition, in our study, a difference between costs of synthetic and biological meshes was noted (€31 vs €3274). There is a full agreement in the literature about the fact that biological mesh adds significant costs to IHR: its use should, therefore, be limited to a short range of indications.
At the moment, the DRG system does not distinguish between different types of prostheses and it does not provide a specific code for group 3 hernias. Reimbursement strategies for patients undergoing IHR should be re-evaluated considering surgical complexity: we propose to consider the “complex” IHs as a different disease and to create a specific DRG code. In alternative, we propose to provide a separate reimbursement for biological meshes, out of DRG, which is already possible in some cases.
Indirect costs are more difficult to quantify: return to work and sick leave are very individual and depend on many biological, social, psychological, and economical factors; therefore, a monetary extrapolation is complicated (different trades, retired or unemployed patients, housewives, etc).
To align costs to reimbursements, we propose: (1) early diagnosis and treatment, resulting in a reduction of the costs for surgery (less need for “complex” IHRs), of postoperative hospital stay and in a rapid resumption of work; (2) hospital wide protocols on the indications for the use of biological mesh; and (3) the creation of a specific DRG code for “complex” IHs or a separate reimbursement for biological meshes.
This study has several limitations: (1) as a single-center study, it does not take into consideration the local variations of IHR costs and reimbursements; (2) indirect costs are difficult to quantify and only outpatient care could be monetized; and (3) the low numerosity of all groups, in particular group 3 (including only 11 patients).
The goal remains the prevention of IHs when possible. The European Hernia Society has recently developed and published detailed guidelines on the closure of ventral incisions [13]; moreover, some studies provide a high level of evidence that prophylactic mesh-augmented fascial reinforcement may lower the rate of IH in high-risk patients, after elective open intra-abdominal surgery [14].
Conclusion
All DRGs still undervalue the expense, thus causing a great economic loss to the hospital.
The analysis of the costs shows that patient-related risk factors do not increase the overall costs.
To provide a precise “cost-based” reimbursement, the DRG system should distinguish between different types of IHR (standard or complex) and prostheses.
References
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Long term follow up of a randomized controlled trial of suture versus mesh repair for incisional hernia. Ann Surg 240:578–583
Millikan KW (2003) Incisional hernia repair. Surg Clin North Am 83:1223–1234
Anthony T, Bergen PC, Kim LT, Henderson M, Fahey T, Rege RV, Turnage RH (2000) Factors affecting recurrence following incisional herniorrhaphy. World J Surg 24:95–100
Luijendijk RW, Hop WC, van den Tol MP, de Lange DC, Braaksma MM, IJzermans JN, Boelhouwer RU, de Vries BC, Salu MK, Wereldsma JC, Bruijninckx CM, Jeekel J (2000) A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 342:392–398
Breuing K, Butler CE, Ferzoco S, Franz M, Hultman CS, Kilbridge JF, Rosen M, Silverman RP, Vargo D, The Ventral Hernia Working Group (2010) Incisional ventral hernias: review of the literature and recommendations regarding the grading and technique of repair. Surgery 148:544–558
Itani KM, Rosen M, Vargo D, Awad SS, Denoto G 3rd, Butler CE, RICH Study Group (2012) Prospective study of single-stage repair of contaminated hernias using a biologic porcine tissue matrix: the RICH Study. Surgery 152:498–505
Bollettino ufficiale della Regione del Veneto. Bur n. 88 del 25 novembre 2011. http://bur.regione.veneto.it/BurvServices/pubblica/DettaglioDgr.aspx?id=235948. Accessed 1 Dec 2016
Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E, Dietz UA, Eker HH, El Nakadi I, Hauters P, Hidalgo Pascual M, Hoeferlin A, Klinge U, Montgomery A, Simmermacher RK, Simons MP, Smietański M, Sommeling C, Tollens T, Vierendeels T, Kingsnorth A (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13:407–414
Gillion JF, Sanders D, Miserez M, Muysoms F (2016) The economic burden of incisional ventral hernia repair: a multicentric cost analysis. Hernia 20:819–830
Finan KR, Kilgore ML, Hawn MT (2009) Open suture versus mesh repair of primary incisional hernias: a cost-utility analysis. Hernia 13:173–182
Reynolds D, Davenport DL, Korosec RL, Roth JS (2013) Financial implications of ventral hernia repair: a hospital cost analysis. J Gastrointest Surg 17:159–166
Israelsson LA, Jönsson L, Wimo A (2003) Cost analysis of incisional hernia repair by suture or mesh. Hernia 7:114–117
Muysoms FE, Antoniou SA, Bury K et al (2015) European Hernia Society guidelines on the closure of abdominal wall incisions. Hernia 19:1–24
Fischer JP, Basta MN, Mirzabeigi MN, Bauder AR, Fox JP, Drebin JA, Serletti JM, Kovach SJ (2016) A risk model and cost analysis of incisional hernia after elective, abdominal surgery based upon 12,373 cases. The case for targeted prophylactic intervention. Ann Surg 263:1010–1017
Author information
Authors and Affiliations
Contributions
SR, MD: study design, data collection and analysis, manuscript writing, final version approval. AG, MD: data collection and analysis, manuscript writing, final version approval. SP, MD: design of the study, data collection and analysis, manuscript writing, final version approval. GP, MD: manuscript writing, final version approval. AG, MD: data collection, final version approval. EP, MD: data collection, final version approval. RB, MD: study design, data collection and analysis, manuscript writing, approval of final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Rampado, S., Geron, A., Pirozzolo, G. et al. Cost analysis of incisional hernia repair with synthetic mesh and biological mesh: an Italian study. Updates Surg 69, 375–381 (2017). https://doi.org/10.1007/s13304-017-0453-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-017-0453-9