Abstract
Posterior retroperitonoscopic adrenalectomy (PRA) has become a standard approach to the adrenal gland. The aim of this study was to report an initial experience with the procedure following a proper preparatory phase highlighting the rapidity, safety and effectiveness by which it could be introduced into a surgeon’s practice. Between May 2015 and July 2016, 14 PRAs were performed in 14 patients (9 females and 5 males). The average age was 46 years, BMI: 25.5 kg/m2, and ASA score: 2. Indications included: incidenatloma (n = 5), Conn’s adenoma (n = 5), and Cushing’s adenoma (n = 4). Lesions were on average 3.3 cm in size. Outcomes of interest included: operative time (OT), conversion rate, postoperative morbidity and mortality rates, and the length of hospital stay. Mean OT was 87.5 min (range 35–150 min). A significant reduction in OT occurred after the sixth procedure and was progressive thereafter. After the tenth case, the OT became less than 1 h. No conversion was required. No intra- or post-operative complications occurred, and mortality was zero. All patients commenced oral intake and ambulated following full recovery from anesthesia. The mean length of hospital stay was 3 days (range 2–6 days). PRA offers a direct access to the adrenal gland allowing for target-oriented dissection. Cognitive reorientation to the anatomy of this back door access and an adequate learning curve could be rapidly achieved by experienced and properly prepared laparoscopic surgeons.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endoscopic adrenalectomy is the gold standard surgical approach to the adrenal gland with the most widely used technique being lateral transperitoneal adrenalectomy (LTA). Posterior retroperitonoscopic adrenalectomy (PRA) is an alternative technique that was standardized and popularized by Walz in 1994, and ever since it has become “for some” the preferred surgical approach to the gland within the confines of its selection criteria [1–3]. It has been demonstrated that both LTA and PRA are equally safe and effective. However, the latter offers more favorable short- and long-term outcomes [4–6]. These are manifested in a shorter operating time, reduced intraoperative blood loss, reduced postoperative pain, reduced time to oral intake and ambulation, a shorter hospital stay, a lower risk of port-site hernia, and a lower cost. Furthermore, PRA is more appealing than LTA in the setting of a previous abdominal surgical history and/or bilateral adrenal disease as it eliminates the need to reposition the patient. Despite the additional advantages it offers over LTA, PRA’s popularity among surgeons has been growing slowly. This is probably attributed to unfamiliarity of surgeons with the executional steps of the procedure, and the relevant anatomy of this backdoor access. Furthermore, false beliefs regarding the consequences of high-pressure retroperitoneal insufflation may also serve as an additional set back to adopting the procedure [7]. The purpose of reporting this initial experience with PRA is to demonstrate that following a proper preparatory phase of knowledge acquisition, surgeons skilled in endoscopic surgery could not only safely and effectively introduce the procedure into their practice, but also rapidly allowing them to benefit from the additional advantages it offers.
Materials and methods
Between May 2015 and July 2016, 14 patients were carefully selected for RPA. These included 9 women and 5 men aged 23–72 years (average 46 years) with a mean BMI of 25.5 kg/m2 (range 22.7–28 kg/m2), and a mean ASA score of 2. In all patients the distance between rib 12 and the iliac crest was at least 4 cm when patients were examined lying prone to minimize factors that might potentially limit the retroperitoneal working space. Indications for surgery included relatively small functioning and non-functioning adrenal lesions. Mean lesion size was 3.3 cm (range 1.3 cm–5.5 cm); 8 were left-sided and 6 were right-sided. These included: incidentalomas (n = 5), Conn’s adenomas (n = 5), and Cushings’ adenomas (n = 4). None of the lesions were suspicious for malignancy on imaging studies. Outcomes of interest were operative time, conversion rate, perioperative morbidity and mortality, time to oral intake and ambulation, and the length of hospital stay. Table 1 summarizes the features of the cases in this series.
Surgical technique
A detailed description of the procedure has been reported in literature [7]. Nevertheless, a brief description of the surgical technique is provided here. Following proper positioning of the patient (prone in a jack-knife position with the hip joints and knees bent at 75°–90°, and the back flat), access into the retroperitoneum is initially obtained via a 1.5 cm incision made at the midpoint between the patient’s spine and lateral abdominal wall just below rib 12. The retroperitoneum is then entered by blunt and sharp dissection. The index finger is then used to palpate the tip of rib 11, and guide the insertion of the second port (5 mm); just below and lateral to the tip of rib 11, in line with the first port. Prior to placement of the third port, the working space is created by high-pressure CO2 insufflation (20–30 mmHg), and downward displacement of the fatty tissue below the diaphragm until the superior pole of the kidney is visualized. The third port (5 mm) is then placed under visual control parallel to the paraspinous muscles at an almost flat angle to the skin directed cranially. With the medial port serving as the camera port, dissection (using bipolar scissors- LigaSure® 5 mm blunt tip 37 cm) begins by targeting the superior pole of the kidney rather than the adrenal gland itself. The aim is to resect the adrenal gland en bloc with its surrounding fat off of the upper pole of its corresponding kidney. Dissection is directed medially (3 O’clock to 9 O’clock) along the upper pole of the kidney on the right side whereas on the left side it is directed in the reverse direction (9 O’clock to 3 O’clock). On the right, the adrenal arteries are seen crossing the posterior aspect of the inferior vena cava (IVC). Once divided and the gland lifted up, the confluence of the right adrenal vein and the IVC is exposed, and the vein could be divided. On the left, once the adrenal arteries in the area medial to the upper pole of the kidney are divided, the adrenal vein typically joined by the inferior phrenic vein becomes exposed. The vein is divided and its stump could serve as means of retraction to continue the dissection. The resected gland is then delivered via an endobag through the middle port. Larger lesions may require morcellation. The field is then irrigated and inspected for adequate hemostasis. Drain placement is not a routine requirement. Finally, port sites are closed with absorbable sutures. A video demonstrating a left-sided PRA is provided here (Video).
Results
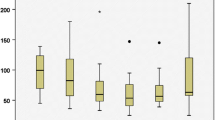
All of the 14 procedures were completed retroperitonoscopically without the need to convert to an alternative technique. The operative time (surgeon’s time; from incision to closure) ranged between 35 and 150 min (mean 87.5 min). A sharp drop in operative time occurred following the 6th procedure performed. The drop in operative time was progressive thereafter, and after 10 cases performed it became under an hour (Fig. 1). No adverse intraoperative events occurred, and in none of the procedures was placement of a drain required. Postoperative morbidity and mortality rates were zero. All patients resumed oral intake and ambulated following full recovery from anesthesia. The mean length of hospital stay was 3 days (range 2–6 days).
Discussion
Surgery is partly science and partly art. Therefore, proper acquisition of both theoretical and technical knowledge related to a surgical procedure is one of the keys to its successful introduction into one’s practice. In PRA unfamiliarity of surgeons with the relevant retroperitoneal anatomy, and the ergonomics and detailed executional steps of the procedure may discourage its adoption. This could be dealt with through a step-wise educational approach that involves observing an expert surgeon-mentor followed by mentored-hands on experience. At the authors’ centre a surgical team (GM, LF, and SB) experienced in laparoscopic adrenalectomy followed this strategy collaborating with Dr Martin Walz who popularized and advanced the procedure. Surgeons may also be reluctant to adopt PRA due to misconceptions regarding the consequences of the high-pressure retroperitoneal insufflation, and delayed control of the adrenal veins. It has been demonstrated, however, that intraperitoneal and retroperitoneal CO2 insufflation evoke different cardiovascular changes, and that high retroperitoneal insufflation pressure does not cause significant hemodynamic changes and is well tolerated [8, 9]. High-pressure retroperitoneal insufflation is also theoretically incriminated for a higher risk of venous thromboembolic disease and gas embolism. Nevertheless, these potential complications have not been reported in literature [1–6]. In PRA division of the adrenal vein is done towards the end of the procedure. This contradicts the vein-first dogma. Controlling the vein first especially in cases of pheochromocytoma was considered as the golden rule to prevent catecholamine surges related to gland manipulation. However, it has been demonstrated that delayed division of the vein is as safe as dividing it first [10–12]. Delayed division of the adrenal vein does not significantly increase hemodynamic changes during endoscopic adrenalectomy be it via LTA or PRA.
Another key to successful introduction of a new surgical technique is selectivity. A learning curve is a graphical representation of the relationship between performance and experience in four phases. Accordingly, performance tends to improve with experience, and one of the measures used for its assessment is operative time [13]. In PRA, it has been demonstrated that factors that significantly prolong operative time include: right-sided procedures, male sex, lesions >3 cm in size, and pheochromocytomas. Furthermore, the effect of these factors (except for the first) on operative time does not seem to revert even after attaining proficiency performing the procedure [1, 10]. The patients selected in the introductory phase of the authors’ experience almost fit the profile of an ideal case with the majority of patients being normal weight females with relatively small left sided lesions (no pheochromocytomas). Obesity itself is not a contraindication to PRA. However, super-obesity (BMI >45 kg/m2) is [14]. In super-obese individuals abdominal viscera compress the retroperitoneum limiting the available working space, and high-pressure insufflation (even around 30 mmHg) is unlikely to compensate for this set back. Although this series is considered too small to draw proper conclusions, there was a sharp drop in operating time after the sixth procedure. The first case was operated in 150 min and the last two cases were performed in 45 and 35 min by the same surgical team (SB, LF and GB); a single surgeon served as the primary operator in all 14 cases. This is probably attributed to PRA’s direct anatomical access to the adrenal gland, and the target-oriented dissection it allows, avoiding mobilization of adjacent structures and in turn allowing a rapid learning curve (Fig. 1). These factors also account for the safety of the procedure. In this series, no intraoperative adverse events such as a peritoneal or pleural leak, vascular injury, gas embolism or hemodynamic instability were encountered. Postoperatively, none of the patients developed venous thromboembolic disease or hyperesthesia of the abdominal wall (subcostal nerve palsy); the latter being probably attributed to the proper technique of port placement. Postoperative mortality was zero. The conversion rate in this series was zero as well, and this is further testimony to the importance of a step-wise educational strategy in adopting a new surgical technique, and adhering to selection criteria. Finally, the introduction of oral intake and the ability of patients to ambulate shortly after the intervention are attributed to the lack of violation of the peritoneal cavity and are considered important additional advantages of a retroperitonoscopic approach over a laparoscopic one. A potential limitation of this study is the small number of procedures performed. A larger number of procedures are required to demonstrate reproducibility of the favorable results, and report a proper learning curve consisting of four phases.
Conclusion
PRA is a minimally invasive and maximally effective procedure performed via a minimal access. It can be rapidly, safely and effectively introduced into surgical practice following a well organized preparatory phase. The authors believe that the additional advantages it offers will allow it to gain considerable popularity and become the surgeon’s preferred tool for managing adrenal pathology.
References
Walz MK, Alesina PF, Wenger FA, Deligiannis A, Szuczik E, Petersenn S, Ommer A, Groeben H, Peitgen K, Janssen OE, Philipp T, Neumann HP, Schmid KW, Mann K (2006) Posterior retroperitoneoscopic adrenalectomy–results of 560 procedures in 520 patients. Surgery 140:943–948. doi:10.1016/j.surg.2006.07.039
Perrier ND, Kennamer DL, Bao R, Jimenez C, Grubbs EG, Lee JE, Evans DB (2008) Posterior retroperitoneoscopic adrenalectomy: preferred technique for removal of benign tumors and isolated metastases. Ann Surg 248:666–674. doi:10.1097/SLA.0b013e31818a1d2a
Berber E, Tellioglu G, Harvey A, Mitchell J, Milas M, Siperstein A (2009) Comparison of laparoscopic transabdominal lateral versus posterior retroperitoneal adrenalectomy. Surgery 146:621–625. doi:10.1016/j.surg.2009.06.057
Lee CR, Walz MK, Park S, Park JH, Jeong JS, Lee SH, Kang SW, Jeong JJ, Nam KH, Chung WY, Park CS (2012) A comparative study of the transperitoneal and posterior retroperitoneal approaches for laparoscopic adrenalectomy for adrenal tumors. Ann Surg Oncol 19:2629–2634. doi:10.1245/s10434-012-2352-0
Barczyński M, Konturek A, Nowak W (2014) Randomized clinical trial of posterior retroperitoneoscopic adrenalectomy versus lateral transperitoneal laparoscopic adrenalectomy with a 5-year follow-up. Ann Surg 260:740–747. doi:10.1097/SLA.0000000000000982
Chai YJ, Woo JW, Kwon H, Choi JY, Kim SJ, Lee KE (2016) Comparative outcomes of lateral transperitoneal adrenalectomy versus posterior retroperitoneoscopic adrenalectomy in consecutive patients: a single surgeon’s experience. Asian J Surg. 39:74–80. doi:10.1016/j.asjsur.2015.04.005
Bakkar S, Materazzi G (2016) Posterior retroperitonoscopic adrenalectomy; how to do it—pears and secretes. J Minim Invasive Surg Sci 5(4):e42362. doi:10.17795/minsurgery-42362
Giebler RM, Walz MK, Peitgen K, Scherer RU (1996) Hemodynamic changes after retroperitoneal CO2 insufflation for posterior retroperitoneoscopic adrenalectomy. Anesth Analg 82:827–831
Giebler RM, Behrends M, Steffens T, Walz MK, Peitgen K, Peters J (2000) Intraperitoneal and retroperitoneal carbon dioxide insufflation evoke different effects on caval vein pressure gradients in humans: evidence for the starling resistor concept of abdominal venous return. Anesthesiology 92:1568–1580
Bonjer HJ, van der Harst E, Steyerberg EW, de Herder WW, Kazemier G, Mohammedamin RS, Bruining HA (1998) Retroperitoneal adrenalectomy: open or endoscopic? World J Surg 22:1246–1249
Zhang X, Lang B, Ouyang JZ, Fu B, Zhang J, Xu K, Wang BJ (2007) Ma X (2007) Retroperitoneoscopic adrenalectomy without previous control of adrenal vein is feasible and safe for pheochromocytoma. Urology 69:849–853. doi:10.1016/j.urology.01.078
Vassiliou MC, Laycock WS (2009) Laparoscopic adrenalectomy for pheochromocytoma: take the vein last? Surg Endosc 23:965–968. doi:10.1007/s00464-008-0264-7
Bakkar S, Materazzi G, Biricotti M, De Napoli L, Conte M, Galleri D, Aghababyan A, Miccoli P (2016) Minimally invasive video-assisted thyroidectomy (MIVAT) from A to Z. Surg Today 46:255–259. doi:10.1007/s00595-015-1241-0
Walz MK, Peitgen K, Walz MV, Hoermann R, Saller B, Giebler RM, Jockenhövel F, Philipp T, Broelsch CE, Eigler FW, Mann K (2001) Posterior retroperitoneoscopic adrenalectomy: lessons learned within five years. World J Surg 25:728–734
Acknowledgements
The authors thank Dr Walz for his devotion to evidence-based surgical innovation, and for sharing his time and experience mentoring the procedure. Dr Marco Biricotti’s work in preparing the video is also highly appreciated.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This work was approved by the Ethics Committee at the University Hospital of Pisa, Pisa-Italy.
Informed consent
For this type of study formal consent is not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bakkar, S., Materazzi, G., Fregoli, L. et al. Posterior retroperitonoscopic adrenalectomy; a back door access with an unusually rapid learning curve. Updates Surg 69, 235–239 (2017). https://doi.org/10.1007/s13304-017-0437-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-017-0437-9