Abstract
As the most important detoxifying enzymes in liver, glutathione S-transferases (GSTs) can protect hepatocytes against carcinogens. We conducted a large cohort study to investigate the prognostic value of single nucleotide polymorphisms (SNPs) in seven encoding genes of GSTs for hepatocellular carcinoma (HCC). Twelve SNPs were genotyped and correlated with overall survival in 469 HCC patients. The median follow-up time of all patients was 21 (range 3–60) months, and the median survival time was 22 months. By the end of the study, 135 (28.8 %) patients were alive. Only rs4147581 in GSTP1 gene exhibited a significant association with survival of HCC patients (P = 0.006), with its mutant allele bearing a significantly lower risk of death (hazard ratio, 0.71; 95 % confidence interval 0.53–0.90), compared with the homozygous wide-type. A longer median survival time in patients with rs4147581 mutant allele was noticed than those homozygous wide-type (P = 0.03), and there was a marked adverse effect on survival conferred by smoking exposure in these patients. Conclusively, our findings provide supporting evidence for a contributory role of GSTP1 rs4147581 polymorphism in predicting the prognosis of HCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the fifth most common cancer worldwide, accounting for up to 500,000 deaths per year. Nearly half of HCC morbidities and mortalities are projected to occur in China [1], probably due to the chronic infection of hepatitis B virus, a common carcinogen to HCC [2]. Other environmental carcinogens such as aflatoxin or chemical carcinogens are also established as potential contributors to hepatic carcinogenesis [3]. It is therefore reasonable to assume that the metabolizing enzymes responsible for carcinogen detoxification are logical candidate biomarkers to enrich our understanding of molecular hepatic carcinogenesis.
Glutathione S-transferases (protein: GSTs; gene: GSTs) are a broadly expressed family of phase II isoenzymes that protect normal cells against the damages induced by hepatitis B virus or aflatoxin-related hepatocarcinogens [4]. There is a general recognition that loss of detoxification function in GSTs can increase cancer risk [5–7]. In humans, there are several classes of GSTs, viz. α (GSTA), μ (GSTM), π (GSTP), θ (GSTT), and ω (GSTO) [5, 8]. Recently, growing observations have indicated that the effectiveness of the detoxifying properties of GSTs is genetically determined [9] because genetic polymorphisms can produce remarkable changes in the metabolic process of carcinogens and chemotherapeutic agents [10], increase the risk of HCC and other malignances [9, 11–19], and affect the survival status of cancer patients [11–13, 17]. The most widely evaluated genetic polymorphisms are harbored in the coding genes for GSTM1 and GSTT1. However, a literature search has not yet revealed any evidence regarding the association of other GST genes with overall survival of HCC patients.
To fill the gap in knowledge and generate useful information, we previously genotyped several SNPs in GST genes in a cohort of 214 patients and found that polymorphisms of GSTO2 and GSTP1 might be associated with survival in HCC [20, 21]. To confirm or refute the results, an enlarged study was conducted. In the present study, we recruited 469 patients to provide convincing association between genetic polymorphisms in GST genes and the 5-year survival in HCC.
Materials and methods
Ethics
The ethics committee at the First Affiliated Hospital of Xi’an Jiaotong University has reviewed and approved this study. Written informed consent has been obtained from each participant at enrollment.
Study subjects
A total of 469 HCC patients of Han descent were enrolled from the Department of Hepatobiliary Surgery and Department of Cardiology and Periphery Vascular Medicine at the First Affiliated Hospital of Xi’an Jiaotong University between January 2009 and November 2014. Patients were eligible for the study if they met the following criteria: (1) 18 years or older, (2) suffered HCC, the diagnosis of which was based on the National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology, and (3) have no previous history of other types of cancer or cancer-related treatments.
Demographic and clinical data
Demographic data were gathered using a standardized epidemiological questionnaire. Peripheral blood sample (5 mL) was drawn from each eligible patient after an interview. Detailed clinical data were obtained from patients’ medical records and consultation with physicians, including date of diagnosis, smoking behavior, history of hepatitis virus infection and liver cirrhosis, Child–Pugh score, serum alpha-fetoprotein (AFP) level at diagnosis, venous invasion, and clinical staging. Clinical staging was determined by the tumor–node–metastasis (TNM) classification system (UICC /AJCC, 2010). During follow-up, vital status on HCC patients was updated at a 3-month interval by a trained clinical specialist through an on-site interview, direct calling, or medical chart review. Each patient was followed up regularly after therapy until the end of our follow-up period on 3/31/2015. Demographic and clinical characteristics of all HCC patients are shown in Table S1.
SNP selection
All examined SNPs were selected from the NIEHS (National Institute of Environmental Health Sciences, http://snpinfo.niehs.nih.gov/snpinfo/snptag.htm) according to our previous studies [20, 21]. In total, 12 SNPs were selected from seven genes: GSTA1 (rs6917150), GSTA4 (rs385636), GSTM2 (rs638820), GSTM3 (rs1109138, rs7483), GSTO1 (rs2282326, rs17116779), GSTO2 (rs156699, rs7085725, rs157077), and GSTP1 (rs4147581, rs2370141).
Genotyping
Venous blood of each patient was stored in Vacutainer tubes at 4 °C. Genomic DNA was extracted using the E.Z.N.A. Blood DNA Midi Kit (Omega Bio-Tek, Norcross, GA, USA) according to the manufacturer’s instructions. DNA was dissolved in TE buffer (10 mM Tris at PH 7.8, 1 mM EDTA) and then quantified by a measurement of OD260. The final preparation was stored at −20 °C. Genotyping was performed using the Sequenom iPLEX genotyping system (Sequenom Inc, San Diego, CA, USA). The laboratory personnel who performed the genotyping was blinded to the vital status of the patients.
Statistical analysis
All statistical analyses were performed using the SPSS version 21.0 statistical package for Microsoft Windows (SPSS, Chicago, IL, USA). Survival time of HCC patients was defined as the period from the date of first diagnosis to the date of death (clinical endpoint) or last follow-up (censored). The Pearson χ 2 test was used to compare the distributions of demographic and clinical variables by survival status. Hazard ratio (HR) and its 95 % confidence interval (CI) were estimated from a multivariate Cox proportional hazards model, adjusting for age, gender, Child–Pugh score, and TNM stage. Kaplan–Meier curve and log-rank test were used to assess overall survival (OS) differences. Survival tree analysis was performed to classify HCC patients into distinct risk subgroups using the STREE software (http://c2s2.yale.edu/software/stree/). All statistical tests were two-sided, and a P value <0.05 was considered to be statistically significant.
Results
Host characteristics
The median age of 469 patients (383 men and 86 women) was 55 years (mean ± SD 54.3 ± 14.4; range 20–87 years) at the time of HCC diagnosis. Of all study patients, 86.1 % (n = 404) were HBsAg (surface antigen of the hepatitis B virus) positive, 71.2 % (n = 334) had a Child–Pugh score A, and 33.9 % (n = 159) were (current) smokers. There were 55.4 % (n = 260) of patients with tumor size ≥5 cm and 45.8 % (n = 215) with significantly increased serum AFP (≥200 ng/mL). The percentage of patients with TNM stage I + II and stage III was 50.5 % (n = 237) and 49.5 % (n = 232), respectively. The median follow-up time of all patients was 21 months (range 3–60 months). At the latest follow-up, the median survival time for the entire cohort of patients was 22 months, and 135 (28.8 %) patients were alive (Table S1).
Prognostic significance
Cox proportional hazards regression model was constructed to identify the prognostic factors for OS of HCC patients. First, univariate analysis and Kaplan–Meier analysis showed that younger age (≤55 years) [HR (95 % CI) 0.46 (0.42–0.66); p < 0.001], male gender [0.59 (0.45–0.78); p < 0.001], non-smoking behavior [0.88 (0.79–0.99); p = 0.03], and early TNM stage (I + II) [0.67 (0.60–0.75); p = 0.001] were protective factors against death in HCC patients (Table 1 and Fig. 1). HBsAg status, cirrhosis, Child–Pugh score, serum AFP, and tumor size were not associated with clinical outcome (P > 0.05) (Table 1). Furthermore, multivariate analysis revealed that age (P < 0.001), gender (P = 0.001), and TNM stage (P < 0.001) were independent prognostic predictors for OS of HCC patients (Table 1), and low Child–Pugh score [0.59 (0.44–0.80); p = 0.001) exhibited an independent association with longer survival time.
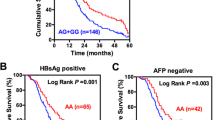
GST polymorphisms and HCC clinical outcomes
Of the 12 SNPs examined, only rs4147581 in GSTP1 was significantly associated with OS of HCC patients under the dominant model of inheritance (Table 2). Patients carrying at least one mutant allele of rs4147581 had a significantly decreased risk of death [HR (95 % CI) 0.76 (0.61–0.95)] when compared with those homozygous wild type (P = 0.02). Kaplan–Meier analysis showed a significantly longer median survival time in patients with the mutant allele of rs4147581 than those without (24.1 vs. 20.9 months; log rank P = 0.02) (Fig. 2a).
GSTP1 rs4147581 and OS in low-risk HCC patients
The impact of GSTP1 rs4147581 on OS of HCC patients who were stratified by demographic and clinicopathological characteristics is shown in Table 3. There was a significant reduction in death risk conferred by rs4147581 in male patients [HR (95 % CI) 0.74 (0.58–0.94); P = 0.02], in non-smokers [0.74 (0.56–0.97); p = 0.03], in patients with AFP <200 ng/mL [0.65 (0.48–0.88); p = 0.01], and in patients with clinical stage I + II [0.61 (0.43–0.85); p = 0.01]. As indicated in Fig. 2b–e, log-rank tests further found significant differences in OS between the mutant allele carriers and the wild-type homozygous carriers of rs4147581 in male gender, non-smokers, low AFP (<200 ng/mL), or early stage (TNM I + II) (P = 0.02, 0.03, 0.02, and <0.001, respectively).
Smoking and OS in rs4147581 mutant allele carriers
As shown in Table S2, there was a significant difference in the genotype distributions of GSTP1 rs4147581 in patients with vs. without smoking behavior (P = 0.01), as well as in patients classified by smoking quantity (P = 0.02) (Fig. 3a). Patients carrying the mutant allele of rs4147581 were overrepresented in non-smokers relative to smokers. To investigate the interactive role of rs4147581 and smoking habit in HCC progression, Kaplan–Meier curves for patients with the mutant allele across different smoking exposures are depicted in Fig. 3. Overall survival of rs4147581 mutant allele carriers was adversely affected by smoking exposure (Fig. 3c, e). In contrast, the association between smoking exposure and clinical outcome was not significant among patients homozygous for the wild type (Fig. 3b, d).
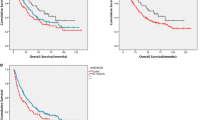
Survival tree analysis
A survival tree analysis was carried out to explore the potential prognostic value of rs4147581 (Fig. 4). The top splitting factor was TNM stage, followed by age and rs4147581, resulting in four terminal node tree (Fig. 4a). The median survival time was 16.6 months for terminal node 1 (HCC patients with stage III) and 19.7 months for terminal node 2 (patients with stage I + II and age >55 years). In younger HCC patients (age ≤55 years) with stage I + II, rs4147581 mutant allele carriers had a better clinical outcome with a median survival time of 29.0 months when compared with those homozygous wild type (P < 0.001; Fig. 4b).
Discussion
In this study, we assessed the impact of 12 well-selected polymorphisms within seven promising genes on the 5-year survival of HCC in a large Chinese cohort. The most important finding is that polymorphism rs4147581 in GSTP1 gene was significantly associated with overall survival of 469 HCC patients. Moreover, this polymorphism might be an independent prognostic marker for HCC, especially in the male and non-smokers, as well as patients with a lower serum AFP level, and early clinical stage.
GSTP1 is a member of glutathione S-transferase family and acts as a part of the protective system against a wide range of potentially harmful cytotoxic compounds. Previous studies have demonstrated that GSTP1 genetic defects contribute to an increased risk and poor clinical outcome of various malignancies, such as esophageal cancer [22], colorectal cancer [11], glioma [13], breast cancer [9, 23], prostate cancer [24], and ovarian cancer [12, 25]. Loss of GSTP1 has been suggested to increase the risk of DNA damage and mutation and consequently lead to HCC carcinogenesis and progression [7]. However, little is known to date about the genetic effect of GSTP1 on HCC risk and prognosis. Chen et al. [16] reported that GSTP1 gene polymorphisms might contribute to an increased risk of HCC in Taiwanese, reinforcing the hypothesis that the GSTP1 gene is a logical candidate for cancer progression. In our previous study, we have identified a common polymorphism rs4147581 in GSTP1 as a primary factor to predict the clinical outcome of HCC patients [20]. The potential contribution of rs4147581 to OS of HCC was further consolidated by an enlarged cohort that was conducted in the present study.
Although the exact mechanism by which GSTP1 rs4147581 polymorphism exerts its effect on clinical outcome remains largely unknown, there are several biological hints from medical literature. According to the public genotyping (GSE28127) and gene expression (GSE22058) datasets from National Center for Biotechnology Information (NCBI) Gene Expression Omnibus (GEO) database (http://www.ncbi.nlm.nih.gov/geo/), the wild-type allele of rs4147581 polymorphism was observed to be associated with lower GSTP1 expression [20]. In addition, as reflected by the eQTL (expression quantitative trait loci) analysis (http://www.sanger.ac.uk/resources/software/genevar/), the GSTP1 expression differs significantly according to rs4147581 genotypes. Furthermore, a recent study reported a close relation between GSTP1 rs4147581 polymorphism and smoking-related DNA methylation [26], which resulted in downregulation of GSTP1 in liver cancer cell lines or tumor tissues [7, 27, 28]. On the basis of these observations, we therefore developed a hypothesis that, if involved, rs4147581 variant might upregulate GSTP1 expression through inhibiting DNA methylation, which might at least in part explain the marked survival advantage across its genotypes observed in this cohort study.
As a metabolizing enzyme, GSTP1 has been extensively investigated in the activation and detoxification of procarcinogens in tobacco smoke [14, 29]. As expected, we observed a close relationship between GSTP1 rs4147581 variant and smoking behavior in HCC patients. Further stratification by smoking quantity, our findings supported a protective role of rs4147581 mutant allele in non-smoking patients. It is of interest to note that carriers of rs4147581 mutant allele who had prolonged survival time were more susceptible to smoking exposure. All these observations indicated that patients who carried the rs4147581 mutant allele might benefit from smoking cessation, which may guide those patients to make a wise decision.
Several possible limitations should be acknowledged. First, our findings in Han Chinese may not be generalizable to other ethnic or racial groups. Second, the moderate sample size after stratification precluded further interaction explorations between GSTP1 genetic alterations and environmental risk factors. Third, our study presents limited evidence for revealing the functional mechanism of GSTP1 polymorphism, which needs further investigation in future experimental studies.
In conclusion, we demonstrate the first epidemiological evidence supporting a contributory role of GSTP1 rs4147581 polymorphism in predicting HCC prognosis in a large cohort. If validated, this polymorphism may potentially serve as a simple non-invasive predictive biomarker for clinical outcome of HCC in the future.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology. 2012;142:1264–73. e1261.
Gross-Steinmeyer K, Eaton DL. Dietary modulation of the biotransformation and genotoxicity of aflatoxin b(1). Toxicology. 2012;299:69–79.
Chasseaud LF. The role of glutathione and glutathione S-transferases in the metabolism of chemical carcinogens and other electrophilic agents. Adv Cancer Res. 1979;29:175–274.
Lee WH, Morton RA, Epstein JI, Brooks JD, Campbell PA, Bova GS, et al. Cytidine methylation of regulatory sequences near the pi-class glutathione S-transferase gene accompanies human prostatic carcinogenesis. Proc Natl Acad Sci U S A. 1994;91:11733–7.
Niu D, Zhang J, Ren Y, Feng H, Chen WN. Hbx genotype d represses gstp1 expression and increases the oxidative level and apoptosis in hepg2 cells. Mol Oncol. 2009;3:67–76.
Zhang YJ, Chen Y, Ahsan H, Lunn RM, Chen SY, Lee PH, et al. Silencing of glutathione S-transferase p1 by promoter hypermethylation and its relationship to environmental chemical carcinogens in hepatocellular carcinoma. Cancer Lett. 2005;221:135–43.
Daniel V. Glutathione S-transferases: gene structure and regulation of expression. Crit Rev Biochem Mol Biol. 1993;28:173–207.
Curran JE, Weinstein SR, Griffiths LR. Polymorphisms of glutathione S-transferase genes (gstm1, gstp1 and gstt1) and breast cancer susceptibility. Cancer Lett. 2000;153:113–20.
Watson MA, Stewart RK, Smith GB, Massey TE, Bell DA. Human glutathione S-transferase p1 polymorphisms: relationship to lung tissue enzyme activity and population frequency distribution. Carcinogenesis. 1998;19:275–80.
Stoehlmacher J, Park DJ, Zhang W, Groshen S, Tsao-Wei DD, Yu MC, et al. Association between glutathione S-transferase p1, t1, and m1 genetic polymorphism and survival of patients with metastatic colorectal cancer. J Natl Cancer Inst. 2002;94:936–42.
Howells RE, Dhar KK, Hoban PR, Jones PW, Fryer AA, Redman CW, et al. Association between glutathione-S-transferase gstp1 genotypes, gstp1 over-expression, and outcome in epithelial ovarian cancer. Int J Gynecol Cancer. 2004;14:242–50.
Okcu MF, Selvan M, Wang LE, Stout L, Erana R, Airewele G, et al. Glutathione S-transferase polymorphisms and survival in primary malignant glioma. Clin Cancer Res. 2004;10:2618–25.
Wenzlaff AS, Cote ML, Bock CH, Land SJ, Schwartz AG. Gstm1, gstt1 and gstp1 polymorphisms, environmental tobacco smoke exposure and risk of lung cancer among never smokers: a population-based study. Carcinogenesis. 2005;26:395–401.
White DL, Li D, Nurgalieva Z, El-Serag HB. Genetic variants of glutathione S-transferase as possible risk factors for hepatocellular carcinoma: a huge systematic review and meta-analysis. Am J Epidemiol. 2008;167:377–89.
Chen YL, Tseng HS, Kuo WH, Yang SF, Chen DR, Tsai HT. Glutathione S-transferase p1 (gstp1) gene polymorphism increases age-related susceptibility to hepatocellular carcinoma. BMC Med Genet. 2010;11:46.
Kilburn L, Okcu MF, Wang T, Cao Y, Renfro-Spelman A, Aldape KD, et al. Glutathione S-transferase polymorphisms are associated with survival in anaplastic glioma patients. Cancer. 2010;116:2242–9.
Sergentanis TN, Economopoulos KP. Gstt1 and gstp1 polymorphisms and breast cancer risk: a meta-analysis. Breast Cancer Res Treat. 2010;121:195–202.
Xu Z, Zhu H, Luk JM, Wu D, Gu D, Gong W, et al. Clinical significance of sod2 and gstp1 gene polymorphisms in Chinese patients with gastric cancer. Cancer. 2012;118:5489–96.
Qu K, Liu SS, Wang ZX, Huang ZC, Liu SN, Chang HL, et al. Polymorphisms of glutathione S-transferase genes and survival of resected hepatocellular carcinoma patients. World J Gastroenterol. 2015;21:4310–22.
Wang Z, Qu K, Huang Z, Xu X, Zhang J, Zhang L, et al. Glutathione S-transferase o2 gene rs157077 polymorphism predicts response to transarterial chemoembolization in hepatocellular carcinoma. 2015.
Zhao Y, Wang F, Shan S, Zhao Y, Qiu X, Li X, et al. Genetic polymorphism of p53, but not gstp1, is association with susceptibility to esophageal cancer risk—a meta-analysis. Int J Med Sci. 2010;7:300–8.
Yang G, Shu XO, Ruan ZX, Cai QY, Jin F, Gao YT, et al. Genetic polymorphisms in glutathione-S-transferase genes (gstm1, gstt1, gstp1) and survival after chemotherapy for invasive breast carcinoma. Cancer. 2005;103:52–8.
Agalliu I, Lin DW, Salinas CA, Feng Z, Stanford JL. Polymorphisms in the glutathione S-transferase m1, t1, and p1 genes and prostate cancer prognosis. Prostate. 2006;66:1535–41.
Nagle CM, Chenevix-Trench G, Spurdle AB, Webb PM. The role of glutathione-S-transferase polymorphisms in ovarian cancer survival. Eur J Cancer. 2007;43:283–90.
Breton CV, Byun HM, Wenten M, Pan F, Yang A, Gilliland FD. Prenatal tobacco smoke exposure affects global and gene-specific DNA methylation. Am J Respir Crit Care Med. 2009;180:462–7.
Zhong S, Tang MW, Yeo W, Liu C, Lo YM, Johnson PJ. Silencing of gstp1 gene by cpg island DNA hypermethylation in hbv-associated hepatocellular carcinomas. Clin Cancer Res. 2002;8:1087–92.
Ding S, Gong BD, Yu J, Gu J, Zhang HY, Shang ZB, et al. Methylation profile of the promoter cpg islands of 14 “drug-resistance” genes in hepatocellular carcinoma. World J Gastroenterol. 2004;10:3433–40.
Munaka M, Kohshi K, Kawamoto T, Takasawa S, Nagata N, Itoh H, et al. Genetic polymorphisms of tobacco- and alcohol-related metabolizing enzymes and the risk of hepatocellular carcinoma. J Cancer Res Clin Oncol. 2003;129:355–60.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (Grant Nos. 81201549, 81272644, 81402022, and 81472247) and the Project of Innovative Research Team for Key Science and Technology in Shaanxi province (Grant No. 2013KCJ-23).
Conflicts of interest
There is no competing financial interest among the authors.
Authors’ contributions
Yuelang Zhang and Xiaoqun Dong were responsible for experimental design and supervised the study. Zhixin Wang, Kai Qu, Zichao Huang, and Susun Liu developed methodology. Zhixin Wang, Kai Qu, Sinan Liu, Hulin Chang, Xinsen Xu, Ting Lin, Yamin Liu, and Chang Liu carried out the experiments. Zhixin Wang, Kai Qu, and Wenquan Niu performed data analysis and prepared the figures and tables. Zhixin Wang, Kai Qu, Wenquan Niu, and Xiaoqun Dong wrote, reviewed, and revised the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Zhixin Wang and Kai Qu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Wang, Z., Qu, K., Niu, W. et al. Glutathione S-transferase P1 gene rs4147581 polymorphism predicts overall survival of patients with hepatocellular carcinoma: evidence from an enlarged study. Tumor Biol. 37, 943–952 (2016). https://doi.org/10.1007/s13277-015-3871-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3871-7