Abstract
Despite the fact that malignancies are associated with hematological abnormalities, some clinical studies have been unable to detect such a relation. The aim of our study was to detect the prevalence of pretreatment hematologic abnormalities in patients with common solid tumors and to determine if such a profile could be used for prognostic evaluations. We identified all patients in Cancer Center of Sun Yat-sen University who were diagnosed as solid tumors (breast carcinoma, hepatocellular carcinoma, nasopharyngeal carcinoma, esophageal carcinoma, gastric cancer, cervical carcinoma, endometrial cancer, renal cell carcinoma, and non-small cell lung cancer) between January 2000 and August 2009. All subjects were investigated regarding levels of white blood cells, platelets, and hemoglobin concentration. We identified 3,180 patients with solid tumors and 285 patients with benign diseases for the final analysis. The percentages of leukocytosis, anemia, and thrombocytosis in patients with solid tumors ranged from 4.0% to 25.6%, 3.3% to 29.2%, and 2.1% to 9.7%, respectively. The multivariate Cox analysis revealed that anemia was an independent prognostic factor in patients with breast cancer (P = 0.006), hepatocellular carcinoma (P = 0.002), nasopharyngeal carcinoma (P = 0.008), and esophageal carcinoma (P = 0.001). Leukocytosis was an independent prognostic factor in patients with cervical cancer (P = 0.007). The incidence of hematological abnormalities in Chinese patients with solid tumors was relatively lower than that of the counterparts in the Western countries. A pretreatment anemia or leukocytosis can serve as a useful marker to predict outcome of patients in some of the solid tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although many investigators have suggested a relationship between the hematologic abnormalities and malignant diseases, other studies conflict with their findings. The relationship between elevated platelet count and the malignant tumors was first reported by Reiss et al. in 1872 [1]. Tumor-related thrombocytosis has been reported among patients with types of solid tumors. The ranges of frequencies previously reported in the same disease were inconsistent: 12.0% to 42.5% in gynecologic cancer patients [2–4], 5.83% to 53.0% in lung cancer patients [5–7], and 19.5% to 56.8% in renal cell carcinoma patients [8, 9]. Moreover, it was identified as an adverse prognostic indicator in bronchial cancer patients [10], lung cancer patients [10, 11], gastric cancer patients [12], colorectal cancer patients [11, 13], esophageal cancer patients [14], hepatocellular cancer patients [15], pancreas cancer patients [16], glioblastoma patients [17], renal cell carcinoma patients [18], oral squamous cell carcinoma patients [19], and in different gynecological malignancies and breast cancer patients [2, 20, 21]. But, not as consistently, Hefler noted that thrombocytosis was not an independent predictor of survival for patients with vulvar cancer [21]. It seems that the percentage and the prognostic value of thrombocytosis varies from disease to disease, and even for the same kind of solid tumor, it changes with the geological distribution [5, 6]. A similar phenomenon was found in the condition of anemia and leukocytosis. The incidence rates of anemia and leukocytosis in patients with solid tumors were in a range of 9% to 42.6% [7, 22] and 7.4% to 39.0% [7, 22, 23], respectively.
We have previously [23] shown that the percentages of leukocytosis, anemia, and thrombocytosis were significantly higher in colorectal cancer patients than in patients with benign diseases. Moreover, we found that both pretreatment anemia and thrombocytosis were independent prognostic variables for survival of colorectal cancer patients. However, multivariate Cox regression analysis failed to indicate leukocytosis as a prognostic factor. In order to determine the incidence of hematological abnormalities in Chinese patients with solid tumors, a further study was conducted in patients diagnosed with breast cancer, hepatocellular carcinoma (HCC), nasopharyngeal carcinoma (NPC), esophageal cancer, gastric cancer, cervical cancer, renal cell carcinoma, endometrial carcinoma, and non-small cell lung cancer (NSCLC). All these nine kinds of solid tumors are most common in China. The prognostic value of hematologic abnormalities in these tumors is also investigated.
Patients and methods
Patients
Between January 2000 and August 2009, the medical records of pathology-proven solid tumor patients (including patients with breast cancer, HCC, NPC, esophageal cancer, gastric cancer, cervical cancer, renal cell carcinoma, endometrial carcinoma, and NSCLC) who were diagnosed and received treatment in the Cancer Center of Sun Yat-Sen University were retrospectively analyzed. In addition to these patients, we randomly selected a control group of 285 patients who had benign diseases, including uterine fibroids, breast fibroadenoma, nodular goiter, liver cyst, polycystic kidney, and gallbladder polyps. We excluded patients who received blood transfusion, or had a history of more than one kind of primary cancer.
Blood samples were collected at initial diagnosis 1 day before the treatment. Two-milliliter blood sample was obtained from the peripheral vein and then transported to the hematology laboratory in our cancer center. A full blood count including white blood cells, hemoglobin concentration, and platelet counts was performed, using an electronic particle counting device (Sysmex XE-5000, Japan) before treatment. Other clinical data collected for subsequent analysis included age at diagnosis, gender, tumor staging, and histological grade. Staging was performed according to the tumor node metastasis (TNM) classification of the American Joint Committee on Cancer (AJCC, sixth edition, 2002).
All patients provided written informed consent; we obtained separate consent for use of blood sample. Study approval was obtained from independent ethics committees at Cancer Center of Sun Yat-Sen University. The study was undertaken in accordance with the ethical standards of the World Medical Association Declaration of Helsinki.
Definition of leukocytosis, anemia, and thrombocytosis
Tumor-related leukocytosis was defined as a pretreatment white blood cell count >10 × 109/L without known inflammatory or infectious diseases [21]. A hemoglobin <110 g/L without acute blood loss was defined as tumor-related anemia [24].Thrombocytosis was defined as a pretreatment platelet count >400 × 109/L without known inflammatory conditions [10].
Statistical analysis
The statistical analysis was performed by Statistical Package of Social Sciences 13.0 software. P value <0.05 was considered to be statistically significant. The Kaplan–Meier method was used to estimate the 3-year overall survival. For patients who remained alive, data were censored at the date of the last contact. Kaplan–Meier analysis with log-rank test was used for univariate analysis. Variables showing a trend for association with survival (P < 0.05) were selected in the final multivariate Cox proportional hazards model. The difference of hematologic profile between solid tumors and benign diseases was examined by a chi-square test.
Results
Patient demographics
We identified 3,500 patients with solid tumors in our institution, but excluded 135 patients (3.9%) because of incomplete follow-up, 102 patients (2.9%) because of missing baseline characteristics, and 63 patients (1.8%) because of thrombus and acute or chronic inflammatory diseases (including 25 patients who were taking anticoagulant agents to prevent the coronary heart disease, 20 patients with deep vein thrombosis, 10 patients with pneumonia, three patients with Crohn’s disease, and five patients with tuberculosis). Twelve patients (0.3%) who received transfusion because of severe anemia before coming to our hospital and eight patients (0.2%) with acute blood loss were also excluded. The median follow-up was 31.0 months (range 3.0–115.0 months). The treatments of the reviewed patients were basically planned according to the principles of The National Comprehensive Cancer Network (NCCN) guidelines. The characteristics of the 3,180 patients with solid tumors are shown in Table 1. Until January 2010, there were 689 patients who died from malignant diseases.
The incidence rate of pretreatment hematologic abnormalities in solid tumors
The percentage of leukocytosis, anemia, and thrombocytosis in the whole group of patients were 11.7% (371/3,180), 12.8% (406/3,180), and 5.6% (177/3,180), respectively, while for the patients with benign diseases, it was 8.1% (23/285), 6.0% (17/285), and 3.5% (10/285), respectively. More in detail, the incidence of hematologic abnormality in patients with solid tumors is shown in Table 2, and the difference of hematologic profile abnormalities between patients with solid tumors and benign diseases was also compared. Patients with NSCLC cancer had a significant higher percentage of leukocytosis (25.6%) and thrombocytosis (8.4%) than the benign disease patients, while only 4.0% of breast cancer patients present leukocytosis, significantly lower than the benign disease patients. Moreover, the percentages of thrombocytosis and anemia in patients with gastric cancer, cervical cancer, and endometrium cancer were all significantly higher than patients with benign disease, which were 7.1% and 29.2%, 7.5% and 21.4%, and 9.7% and 22.6%, respectively. The percentages of hematological abnormalities in patients with HCC, NPC, esophageal cancer, and renal cell carcinoma were significantly indifferent from that of patients with benign diseases.
Influence of pretreatment hematologic profile on survival
The median overall survival for patients with breast cancer, HCC, NPC, esophageal cancer, gastric cancer, cervical cancer, renal cell carcinoma, endometrial carcinoma, and NSCLC were 29.1 months (range from 3.0 to 107.0 months), 16.4 months (range from 3.0 to 51.6 months), 30.5 months (range from 3.2 to 89.6 months), 16.9 months (range from 3.0 to 74.7 months), 49.5 months (3.0 to 171.0 months), 29.8 months (range from 3.0 to 80.3 months), 29.2 months (range from 3.0 to 77.2 months), 28.0 months (range from 3.3 to 50.0 months), and 12.6 months (range from 3.0 to 36.0 months), respectively. Table 3 showed the influence of hematologic abnormalities on the 3-year-long overall survival in solid tumor patients. The 3-year-long overall survival of the patients who had breast cancer associated leukocytosis, thrombocytosis, and anemia were significantly lower than that of the patients without any hematological abnormalities (81.3% vs. 91.9%, P = 0.04; 80.0% vs. 92.0%, P = 0.014; and 84.0% vs. 92.2%, P = 0.02). The 3-year-long overall survival of the patients who had NPC associated leukocytosis, thrombocytosis, and anemia were significantly lower than that of the patients without any hematological abnormalities (79.9% vs. 87.4%, P = 0.01; 62.5% vs. 87.4%, P < 0.001; and 40.9% vs. 87.6%, P < 0.001). Furthermore, patients with leukocytosis in HCC and cervical cancer also had a lower 3-year-long overall survival than patients without leukocytosis (16.6% vs. 50.7%, P < 0.001 for HCC; 57.8% vs. 87.4%, P < 0.001 for cervical cancer). Patients with anemia in HCC, esophageal cancer, endometrium cancer, renal cell carcinoma, and NSCLC had a lower 3-year-long overall survival than patients without anemia (19.0% vs. 49.4%, P < 0.001 for HCC; 40.9% vs. 87.6%, P < 0.001 for NPC; 40.0% vs. 53.9%, P = 0.015 for esophageal cancer; 83.3% vs. 95.8% P = 0.021 for endometrial carcinoma; 75.0% vs. 94.8%, P = 0.002 for renal cell carcinoma; 0% vs. 69.0%, P = 0.04 for NSCLC). However, patients with hematologic abnormalities in gastric cancer did not show a survival difference with patients without hematologic abnormalities.
The multivariate Cox analysis
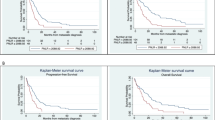
To test the independent prognostic effects of these clinical factors, Cox’s proportional hazard model was applied. Variables showing a trend for association with survival (P < 0.05) were selected in the final multivariate Cox proportional hazards model. The results revealed that anemia was an independent prognostic factor in patients with breast cancer (P = 0.006), HCC (P = 0.002), NPC (P = 0.008), and esophageal carcinoma (P = 0.001). Leukocytosis was an independent prognostic factor in patients with cervical cancer (P = 0.007). The survival curve was shown in Fig. 1. But, thrombocytosis was not confirmed as an independent prognostic factor in the given nine kinds of solid tumor patients.
Univariate analysis of patients with different status of pretreatment hematologic profile. a Survival curve of breast cancer patients according to the condition of hemoglobin. Hemoglobin <110 vs. ≥110 g/L (3-year-long overall survival, 84.0% vs. 92.2%, P = 0.02). b Survival curve of hepatocellular carcinoma patients according to the condition of hemoglobin. Hemoglobin <110 vs. ≥110 g/L (3-year-long overall survival, 19.0% vs. 49.4%, P < 0.001). c Survival curve of nasopharyngeal carcinoma patients according to the condition of hemoglobin. Hemoglobin <110 vs. ≥110 g/L (3-year-long overall survival, 40.9% vs. 87.6%, P < 0.001). d Survival curve of esophageal carcinoma patients according to the condition of hemoglobin. Hemoglobin <110 vs. ≥110 g/L (3-year-long overall survival, 40.0% vs. 53.9%, P = 0.015). e Survival curve of cervical cancer patients according to the condition of white blood cell. White blood cell >10 × 109 vs. ≤10 × 109 cells/L (3-year-long overall survival, 57.8% vs. 87.4%, P < 0.001)
Discussion
It is the first report about the distribution of hematologic abnormalities in patients with malignant diseases in China. We found that the incidence of leukocytosis, thrombocytosis, and anemia varied in the different malignant diseases patients, and it ranged from 4.0% to 25.6%, 2.1% to 9.7%, and 3.3% to 29.2%, respectively. The incidence of hematologic abnormalities of patients with solid tumors in China was relatively lower than the previous reports in other countries. More than 50% of the patients with lung cancer or renal cell carcinoma were reported to have pretreatment thrombocytosis in European or American countries [5, 9]. The interpretation of the difference is open to question. Hideaki Shimade once showed [14] that in Japan, if they set the cut-off platelet count as higher than 400 × 109/L, which was commonly agreed, thrombocytosis was present only in 5.1% of the esophageal carcinoma. It was relatively lower than the previous reports, and the author suspected that the difference relied in the types of solid tumors. So, they defined the thrombocytosis as a platelet count higher than 293 × 109/L for the esophageal carcinoma, which was the mean plus one standard deviation of platelet count in healthy control. Using this definition, the incidence rate of thrombocytosis was 21.1%. Here, we proposed that ethnic and racial background could be one possible explanation. It is reported that only 5.83% of NSCLC patients in Japan [6] had pretreatment thrombocytosis, which was also lower than the reports in European countries or American. One of the limitations of the previous studies was that no incidence of hematologic abnormalities in patients with non-malignant diseases was provided. It is totally possible that people without malignant diseases in countries with high incidence of hematologic abnormalities in malignant diseases also have high incidence of leukocytosis, thrombocytosis, and anemia. Further studies are needed to confirm our hypothesis. In our study, the comparison of hematologic abnormalities between patients with solid tumor and benign diseases was provided, and we found that only 8.1%, 3.5%, and 6.0% of the benign disease patients present leukocytosis, thrombocytosis, and anemia, respectively.
Not all the patients with solid tumors had a significant higher rate of hematologic abnormalities than the benign diseases. Only patients with NSCLC had a higher rate of leukocytosis than benign diseases. As for thrombocytosis and anemia, we are surprised to find out that thrombocytosis appeared with anemia together, except in NSCLC. Although patients with gastric cancer, cervical cancer, and endometrial carcinoma were in a high risk of bleeding, Jale Matindir thought that [22] this was rarely severe enough to cause anemia, while cytokines induced by tumors, such as interleukins, interferon gamma, and tumor necrosis factors, can induce hemolysis, suppress erythropoiesis, and inhibit the response of erythroid progenitor cells to erythropoietin [25, 26]. Other probable explanations include disorders of iron metabolism [27]. Absolute or relative erythropoietin deficiency seems to be the final pathway leading to anemia in patients with solid tumors [28]. Erytropoietin may be involved in the development of thrombocytosis associated with tumor anemia and has been shown to promote platelet formation in rats [28]. This may explain the high correlation between thrombocytosis and anemia.
Till now, less is known about the association of pretreatment peripheral white blood cells and prognosis in patients with malignant diseases. Tumor-related leukocytosis is considered to be an important paraneoplastic syndrome [24]. Kasuga et al. reported that lung carcinoma cells autonomously produced hematopoietic cytokines, including granulocyte colony stimulating factor (G-CSF), granulocyte–macrophage colony stimulating factor (GM-CSF), and interleukin-6 [29]. These cytokines can hence stimulate the proliferation of leukocytes [29]. Several studies have also demonstrated that leukocytosis induced by G-CSF, and GM-CSF is closely associated with tumor progression and is a poor prognostic factor for lung and colon cancer [29, 30]. But, in the present study, we only found that leukocytosis was an independent risk factor for cervical cancer patients.
Anemia is a well-established poor prognostic factor in several types of cancers [31]. Our study showed that anemia was a strong predictor of shorter survival in patients with breast cancer (P = 0.006), HCC (P = 0.002), NPC (P = 0.008), and esophageal carcinoma (P = 0.001). It was reported that pretreatment anemia was associated with shorter survival in numerous carcinoma patients, including lung carcinoma [31], cervical carcinoma [31, 32], head and neck cancer [31, 33], lymphoma [31], prostate carcinoma [34], and esophageal cancer [34]. Severe anemia was associated with poor tumor oxygenation. Intratumoral hypoxia is an important factor in activation of hypoxia-inducible factor-1, which can promote tumor metastasis [35].
The multivariate analysis in our study did not confirm the prognostic role of thrombocytosis in patients with the nine kinds of solid tumors, which is conflicted with previous reports (Table 4). The discrepancy between our study and the previous reports, in which thrombocytosis represent a key prognostic variable, may be explained in several ways. First, as we mentioned before, the incidence rate of thrombocytosis at the time of diagnosis was lower than previous studies. This means that the exact number of patients with thrombocytosis was small; therefore, a larger group of patients was needed to get a significant survival difference at the consideration of statistics. Second, the retrospective nature of our study may limit us to address a casual relationship between thrombocytosis and poor survival of patients with solid tumors.
In conclusion, our study is the first to demonstrate the incidence of hematologic abnormalities in patients with common solid tumors. Moreover, it suggests that abnormalities in the hematologic profile are an important sign of more severe disease. A pretreatment anemia or leukocytosis can serve as a useful marker to predict outcome of patients in some of the solid tumors. The limitation of current study is in its retrospective analysis setting. It remains questionable whether hematological profile abnormality is simply an end result of tumor growth or the underlying killer causing mortality. Several other limitations may apply to our findings. The impact of various treatments related outcome could not be evaluated in this study. Although the present study only focuses on survival, hematological abnormalities may have a stronger effect on disease recurrence. Therefore, separate analyses are needed to elucidate the prognostic significance of these variables in recurrence prediction. Confirming the prognostic effect of pretreatment hematologic profile in studies with prospective design is mandatory. Despite these and other limitations, our data provide an important insight into the patients of solid tumors with hematologic abnormalities in China.
References
Tranum BL, Haut A. Thrombocytosis: platelet kinetics in neoplasia. J Lab Clin Med. 1974;84:615–9.
Li AJ, Madden AC, Cass I, Leuchter RS, Lagasse LD, Karlan BY. The prognostic significance of thrombocytosis in epithelial ovarian carcinoma. Gynecol Oncol. 2004;92:211–4.
Lerner DL, Walsh CS, Cass I, Karlan BY, Li AJ. The prognostic significance of thrombocytosis in uterine papillary serous carcinomas. Gynecol Oncol. 2007;104:91–4.
Gungor T, Kanat-Pektas M, Sucak A, Mollamahmutoglu L. The role of thrombocytosis in prognostic evaluation of epithelial ovarian tumors. Arch Gynecol Obstet. 2009;279:53–6.
Pedersen LM, Milman N. Diagnostic significance of platelet count and other blood analyses in patients with lung cancer. Oncol Rep. 2003;10:213–6.
Tomita M, Shimizu T, Hara M, Ayabe T, Onitsuka T. Prognostic impact of thrombocytosis in resectable non-small cell lung cancer. Interact Cardiovasc Thorac Surg. 2008;7:613–5.
Gislason T, Nou E. Sedimentation rate, leucocytes, platelet count and haemoglobin in bronchial carcinoma: an epidemiological study. Eur J Respir Dis. 1985;66:141–6.
Erdemir F, Kilciler M, Bedir S, Ozgok Y, Coban H, Erten K. Clinical significance of platelet count in patients with renal cell carcinoma. Urol Int. 2007;79:111–6.
Symbas NP, Townsend MF, El-Galley R, Keane TE, Graham SD, Petros JA. Poor prognosis associated with thrombocytosis in patients with renal cell carcinoma. BJU Int. 2000;86:203–7.
Pedersen LM, Milman N. Prognostic significance of thrombocytosis in patients with primary lung cancer. Eur Respir J. 1996;9:1826–30.
Costantini V, Zacharski LR, Moritz TE, Edwards RL. The platelet count in carcinoma of the lung and colon. Thromb Haemost. 1990;64:501–5.
Ikeda M, Furukawa H, Imamura H, Shimizu J, Ishida H, Masutani S, et al. Poor prognosis associated with thrombocytosis in patients with gastric cancer. Ann Surg Oncol. 2002;9:287–91.
Monreal M, Fernandez-Llamazares J, Pinol M, Julian JF, Broggi M, Escola D, et al. Platelet count and survival in patients with colorectal cancer—a preliminary study. Thromb Haemost. 1998;79:916–8.
Shimada H, Oohira G, Okazumi S, Matsubara H, Nabeya Y, Hayashi H, et al. Thrombocytosis associated with poor prognosis in patients with esophageal carcinoma. J Am Coll Surg. 2004;198:737–41.
Chen CC, Yang CF, Yang MH, Lee KD, Kwang WK, You JY, et al. Pretreatment prognostic factors and treatment outcome in elderly patients with de novo acute myeloid leukemia. Ann Oncol. 2005;16:1366–73.
Suzuki K, Aiura K, Kitagou M, Hoshimoto S, Takahashi S, Ueda M, et al. Platelets counts closely correlate with the disease-free survival interval of pancreatic cancer patients. Hepatogastroenterology. 2004;51:847–53.
Brockmann MA, Giese A, Mueller K, Kaba FJ, Lohr F, Weiss C, et al. Preoperative thrombocytosis predicts poor survival in patients with glioblastoma. Neuro Oncol. 2007;9:335–42.
Gogus C, Baltaci S, Filiz E, Elhan A, Beduk Y. Significance of thrombocytosis for determining prognosis in patients with localized renal cell carcinoma. Urology. 2004;63:447–50.
Lu CC, Chang KW, Chou FC, Cheng CY, Liu CJ. Association of pretreatment thrombocytosis with disease progression and survival in oral squamous cell carcinoma. Oral Oncol. 2007;43:283–8.
Taucher S, Salat A, Gnant M, Kwasny W, Mlineritsch B, Menzel RC, et al. Impact of pretreatment thrombocytosis on survival in primary breast cancer. Thromb Haemost. 2003;89:1098–106.
Hefler L, Mayerhofer K, Leibman B, Obermair A, Reinthaller A, Kainz C, et al. Tumor anemia and thrombocytosis in patients with vulvar cancer. Tumour Biol. 2000;21:309–14.
Metindir J, Bilir DG. Preoperative hemoglobin and platelet count and poor prognostic factors in patients with endometrial carcinoma. J Cancer Res Clin Oncol. 2009;135:125–9.
Qiu MZ, Yuan ZY, Luo HY, Ruan DY, Wang ZQ, Wang FH, et al. Impact of pretreatment hematologic profile on survival of colorectal cancer patients. Tumour Biol. 2010;31:255–60.
Chen MH, Chang PM, Chen PM, Tzeng CH, Chu PY, Chang SY, et al. Prognostic significance of a pretreatment hematologic profile in patients with head and neck cancer. J Cancer Res Clin Oncol. 2009;135:1783–90.
Dowlati A, R'Zik S, Fillet G, Beguin Y. Anaemia of lung cancer is due to impaired erythroid marrow response to erythropoietin stimulation as well as relative inadequacy of erythropoietin production. Br J Haematol. 1997;97:297–9.
Spivak JL. Cancer-related anemia: its causes and characteristics. Semin Oncol. 1994;21:3–8.
DeRienzo DP, Saleem A. Anemia of chronic disease: a review of pathogenesis. Tex Med. 1990;86:80–3.
Moliterno AR, Spivak JL. Anemia of cancer. Hematol Oncol Clin North Am. 1996;10:345–63.
Kasuga I, Makino S, Kiyokawa H, Katoh H, Ebihara Y, Ohyashiki K. Tumor-related leukocytosis is linked with poor prognosis in patients with lung carcinoma. Cancer. 2001;92:2399–405.
Mroczko B, Groblewska M, Wereszczynska-Siemiatkowska U, Okulczyk B, Kedra B, Laszewicz W, et al. Serum macrophage-colony stimulating factor levels in colorectal cancer patients correlate with lymph node metastasis and poor prognosis. Clin Chim Acta. 2007;380:208–12.
Caro JJ, Salas M, Ward A, Goss G. Anemia as an independent prognostic factor for survival in patients with cancer: a systemic, quantitative review. Cancer. 2001;91:2214–21.
Dunst J, Kuhnt T, Strauss HG, Krause U, Pelz T, Koelbl H, et al. Anemia in cervical cancers: impact on survival, patterns of relapse, and association with hypoxia and angiogenesis. Int J Radiat Oncol Biol Phys. 2003;56:778–87.
Baghi M, Wagenblast J, Hambek M, Moertel S, Gstoettner W, Strebhardt K, et al. Pre-treatment haemoglobin level predicts response and survival after tpf induction polychemotherapy in advanced head and neck cancer patients. Clin Otolaryngol. 2008;33:245–51.
Rades D, Schild SE, Bahrehmand R, Zschenker O, Alberti WA, Rudat VR. Prognostic factors in the nonsurgical treatment of esophageal carcinoma with radiotherapy or radiochemotherapy: the importance of pretreatment hemoglobin levels. Cancer. 2005;103:1740–6.
Yang MH, Wu MZ, Chiou SH, Chen PM, Chang SY, Liu CJ, et al. Direct regulation of twist by hif-1alpha promotes metastasis. Nat Cell Biol. 2008;10:295–305.
Acknowledgments
This work was funded by National Natural Science Foundation of China grant 30672408, Guangzhou Bureau of Science and Technology grant 2006Z3-E0041, and Sun Yat-sen University 985 Program Initiation Fund (China). We thank Professor Qing Liu in the Epidemiology Department for his suggestion in the statistical analysis. Besides, we thank the staff members in the Department of Medical Oncology, NPC Oncology, Gastric Surgery Oncology, Thoracic Surgery Oncology, Hepatocellular Surgery Oncology, and Gynecology Oncology at Sun Yat-sen University Cancer Center for their assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Qiu, Mz., Xu, Rh., Ruan, Dy. et al. Incidence of anemia, leukocytosis, and thrombocytosis in patients with solid tumors in China. Tumor Biol. 31, 633–641 (2010). https://doi.org/10.1007/s13277-010-0079-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-010-0079-8