Abstract
Background
The purpose of this retrospective study was to test whether the pretreatment hematologic profile can predict the prognosis of patients with head and neck cancer.
Methods
Medical records from 278 patients with head and neck cancer were reviewed, and 270 cases were evaluable. Clinical data including age, gender, stage, pretreatment hematologic profile (including white blood cell, platelet, and differential counts, and hemoglobin level) were recorded. Statistical analyses were performed to determine the prognostic effect of these hematologic indicators, as well as clinical variables. The association between the hematologic indicators and clinical factors was also analyzed.
Results
Pretreatment monocytes >1,000 cells/μl (P = 0.028), hemoglobin <11.0 g/dl (P = 0.022), and platelet count >400 × 103 cells/μl (P = 0.017) were identified as independent prognostic factors in addition to the nodal status and metastasis. A significant correlation between T-stage/monocyte or platelet count and metastasis/platelet count were shown. Monocytosis, anemia, and thrombocytosis were demonstrated to have a cumulative effect on the prognosis of head and neck cancer patients (normal vs. abnormality in one lineage, P = 0.001; abnormality in one vs. more than one lineage, P = 0.005).
Conclusions
A pretreatment hematologic profile can be considered as a useful prognostic marker in patients with head and neck cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head and neck cancer, including cancers originating from the oral cavity, oropharynx, hypopharynx, and larynx, represents the 5th most common cancer in men and the 8th most common cancer in women worldwide (Parkin et al. 2001). Head and neck cancer is one of the major cancers in Taiwan and ranks 4th in male cancer-related deaths (Department of Health, ExecutiveYuan 2004). Greater than 90% of head and neck cancer are squamous cell carcinomas. Multimodality therapies, including surgery, radiotherapy, and chemotherapy are adapted to treat SCCHN. However, the prognosis of advanced head and neck cancers remains poor and more reliable clinical predictors of outcome are needed to select high risk patients who may benefit from receiving more aggressive therapy (Van Belle and Cocquyt 2003).
An abnormal hemogram has been suggested as a sign of dismal prognosis of human cancers due to the implication of pathophysiologic responses to disseminated disease. Tumor-related leukocytosis which is defined as an increasing level of white blood cells has been shown to correlate with poor prognosis in patients with lung caner (Kasuga et al. 2001). Pretreatment anemia is associated with shorter survival for patients with lung carcinoma (Caro et al. 2001), cervical carcinoma (Caro et al. 2001; Dunst et al. 2003), head and neck cancer (Becker et al. 2000; Caro et al. 2001; Rudat et al. 1999; Baghi et al. 2008), lymphoma (Caro et al. 2001), prostate carcinoma (Caro et al. 2001), and esophageal cancer (Rades et al. 2005). Pretreatment thrombocytosis indicating the abnormally high level of platelets, has been reported to be associated with poor prognosis for patients with lung carcinoma (Pedersen and Milman 1996, 2003), glioblastoma (Brockmann et al. 2007), esophageal carcinoma (Shimada et al. 2004), breast cancer (Taucher et al. 2003), gastric carcinoma (Ikeda et al. 2002), hepatocellular carcinoma (Chen et al. 2005), pancreas cancer (Suzuki et al. 2004), renal cell carcinoma (Gogus et al. 2004), and oral squamous cell carcinoma (Lu et al. 2007).
Because a change in the hematologic profile reflects the systemic response to disseminated disease, abnormalities in more than one lineage of blood cells may indicate a more severe disease status. However, reports regarding the cumulative effect of multiple lineage abnormalities on the prognosis of human cancers are still limited. In order to determine whether a pretreatment hematologic profile could be regarded as a useful prognostic marker for SCCHN and if a cumulative effect of abnormalities in multiple lineages of blood cells on cancer prognosis indeed occurs, we analyzed the prognostic significance of a pretreatment hematologic profile in a retrospective cohort of head and neck cancer patients.
Patients and methods
Patient population and treatment of SCCHN
The medical records of 278 pathology-proven head and neck cancer patients who were diagnosed and received treatment in Taipei Veterans General Hospital between July 2003 and July 2007 were retrospectively analyzed. Clinical information collected for subsequent analysis included age at diagnosis, gender, primary tumor site, pretreatment tumor staging, and the pretreatment hematologic profile (white blood cells with differential count, hemoglobin level, and platelet counts). The American Joint Committee on Cancer (AJCC) staging system (sixth edition) was applied in our study (Greene et al. 2002). The AJCC staging is based on the evaluation of the T, N and M components: the T stage is divided into fours major parts (T1–T4), expressing increasing size or spread of the primary tumor (Greene and Leslie 2008); the N stage is also divided into four parts (N0–N3), indicating the absence or increasing numbers of tumor involved in the regional nodes; whereas the M stage identifies the absence (M0) or the presence (M1) of distant metastases including lymph nodes that are not regional. To facilitate the statistical analysis, we grouped the patients into different T (T1 + T2 vs. T3 + T4), N (N0 vs. N+, i.e., N1–3) and M status (M0 vs. M1). Subjects with medical conditions associated with reactive leukocytosis or thrombocytosis (e.g., acute or chronic inflammatory diseases) or anemia caused by acute blood loss were excluded from this retrospective study (n = 8). The remaining 270 cases include 246 males and 24 females with a median age 56.5 years (range 36–89 years). The median follow-up was 24 months (range 0–63.5 months).Among these 270 evaluable cases, 253 patients received definitive treatment, including primary chemoradiotherapy (CRT), surgery alone, or surgery plus postoperative radiotherapy/CRT. For patients with distant metastasis on initial presentation (n = 17), palliative chemotherapy was arranged for symptomatic relief. The characteristics of the 270 head and neck cancer patients are shown in Table 1.
Definition of tumor-related leukocytosis, monocytosis, anemia, and thrombocytosis
Tumor-related leukocytosis was defined as a pretreatment white blood cell (WBC) count >10 × 103 cells/μl without known inflammatory or infectious diseases, and tumor-related thrombocytosis was defined as a pretreatment platelet count >400 × 103 cells/μl without known inflammatory conditions (Kasuga et al. 2001; Pedersen and Milman 2003; Brockmann et al. 2007; Sugitani et al. 2001). To determine whether monocytosis is a prognostic marker of head and neck cancer, a monocyte count >1,000 cells/μl was defined as monocytosis. A hemoglobin <11 g/dl without acute blood loss was defined as tumor-related anemia (Becker et al. 2000; Dunst et al. 2003).
Statistical analysis
All statistical analyses were performed by Statistical Package of Social Sciences 13.0 software (SPSS, Inc. Chicago, IL). A P value < 0.05 was considered to be statistically significant. The Kaplan–Meier estimate was used for survival analysis and the log-rank test was selected to compare the cumulative survival durations in different patient groups (i.e., the univariate survival analysis; Peto and Pike 1973). To test the independent prognostic effect of variables which showed significance in separated analysis by log-rank test, the Cox’s proportional hazards model (i.e., the multivariate survival analysis; Cox 1972) was applied for variables with a P value < 0.05 in the log-rank test. The relative risk of survival analysis indicates the risk of death with reference to the first item of each analysis. The association between the abnormality of the pretreatment hemogram (leukocytosis, monocytosis, anemia, and thrombocytosis) and clinical factors was examined by a chi-square test.
Results
Abnormalities of pretreatment hemograms are associated with a worse outcome and advanced disease of head and neck cancer
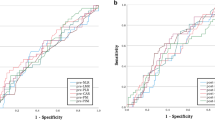
Univariate survival analysis was performed to test the prognostic significance of clinical variables in 270 head and neck cancer cases, and the following seven factors were shown to have an adverse impact on survival: advanced T disease (P = 0.002), nodal involvement (P = 0.002), distant metastasis (<0.001), leukocytosis (WBC > 10.0 × 103 cells/μl; P = 0.031), monocytosis (monocytes > 1,000 cells/μl; P < 0.001), anemia (Hb < 11 g/dl; P = 0.001), and thrombocytosis (platelets > 400 × 103 cells/μl, P < 0.001) (Table 1). These results suggest that abnormalities of all three lineages of blood cells before treatment indicate a worse prognosis of head and neck cancers.
To fully demonstrate the correlation between hematologic profile (WBC count, monocyte count, hemoglobin, platelets) and TNM staging, statistical analysis to evaluate the correlation between T/N/M status and hematologic variables was performed. A significant correlation between T-stage/monocyte count, T-stage/platelet count, and M stage/platelet count were shown (Table 2). Taken together, these results suggest that abnormalities of pretreatment hemogram not only indicate a worse prognosis but also correlate with an advanced disease of head and neck cancers.
Pretreatment monocytosis, but not leukocytosis, is an independent prognostic factor
To test the independent prognostic effect of these clinical factors, Cox’s proportional hazard model was applied. The results demonstrated that when TMN status, and leukocytosis, anemia, and thrombocytosis were tested first, leukocytosis and T status were not independent prognostic factors. However, if we substituted leukocytosis with monocytosis in multivariate survival analysis, the following five variables were shown to be independent prognostic factors (Table 3): nodal involvement (P = 0.014); metastasis (P = 0.043); monocytosis (P = 0.028); anemia (P = 0.02), and thrombocytosis (P = 0.003). These results indicate that an abnormal pretreatment hemogram, including pretreatment monocytosis, anemia, and thrombocytosis, are important prognostic indicators for head and neck cancers. Pretreatment monocytosis demonstrates a more significant impact on patient survival than leukocytosis.
Cumulative effect of monocytosis, anemia, and thrombocytosis on the prognosis of head and neck cancer patients
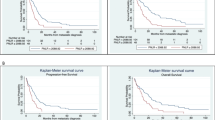
Because an abnormal hemogram may reflect the systemic responses to advanced disease, we speculate that abnormalities in more than one lineage may be associated with a more severe disease. We therefore divided patients into three groups according to the number of abnormalities in the lineages of the blood cells. The results demonstrated that the increased number of abnormal lineages of blood cells, the worse prognosis was observed (Fig. 1, normal vs. abnormality in one lineage, P = 0.001; abnormality in one vs. more than one lineage, P = 0.005). This important result indicates the cumulative effect of an abnormal hemogram on the prognosis of head and neck cancer patients.
Patients who had more abnormalities in the complete blood count had shorter survival. Each finding scored 1: monocytes > 1,000 cells/μl, Hb < 11 g/dl or Plt > 400 × 103 cells/μl. Other findings scored 0: monocytes < 1,000 cells/μl, Hb > 11 g/dl or Plt < 400 × 103 cells/μl. The sum of numbers was calculated and patients were divided into three groups. (score 0 vs. score 1 vs. scores 2 and 3). Score 0 versus score 1, P = 0.001; score 1 vs. scores 2 and 3, P = 0.005
Abnormal hemogram provides additive effect on prognosis in advanced T or N cases
Subgroup analyses were performed to identify if the hematologic profile had additional effect in advanced tumor stage patients. The results showed that monocytosis, anemia, and thrombocytosis were still poor prognostic factors in advanced T stage (T3 + T4) and nodal involvement groups (N+) groups (Figs. 2 and 3, respectively). However, a similar effect was not observed in patient with distant metastasis due to the limited case number with metastasis (n = 17) (data not shown). The independent prognostic effect of monocytosis, anemia, and thrombocytosis was confirmed by Cox’s proportional hazard model in patients with T3 + T4 disease or nodal involvement (data not shown). These results indicate that the pretreatment hematologic profile indeed carries an additive effect to TNM stage on prognosis in patients with head and neck cancers.
The follow-up patients who had pretreatment hemogram abnormalities
Sixty-eight patients had at least one abnormal lineage of blood cells before treatment. Twenty-four patients (35.3%) are still alive and free from disease, 14 patients (20.6%) are still alive, but have had disease recurrence or metastasis, 29 patients (42.6%) died due to cancer or its related complications, and 1 patient (1.4%) died due to liver cirrhosis. Comparing these cases with patients with normal hemograms, a significant increased proportion died of disease (42.6 vs. 21.3%, P < 0.001) and alive with recurrence/metastasis (20.6 vs. 16.3%, P = 0.058) was observed.
Discussion
In the present study, we found that monocytosis (P = 0.028), anemia (P = 0.022), and thrombocytosis (P = 0.017) were independent risk factors for head and neck cancer patients (Table 3). Furthermore, our data demonstrated that patients with an abnormality in more than one series of blood cells was associated with a worse outcome (normal vs. abnormality in one lineage, P = 0.001; abnormality in one vs. more than one lineage, P = 0.005; Fig. 1). This study is the first to report the cumulative effect of abnormalities in more than one lineage of blood cells on the prognosis of head and neck cancers.
Tumor-related leukocytosis is considered an important paraneoplastic syndrome. Kasuga et al. reported that lung carcinoma cells autonomously produce hematopoietic cytokines, such as granulocyte colony stimulating factor (G-CSF), granulocyte–macrophage colony stimulating factor (GM-CSF), and interleukin-6, which can in turn stimulate the proliferation of leukocytes (Kasuga et al. 2001). Several studies have also demonstrated that G-CSF- and GM-CSF-induced leukocytosis is closely associated with tumor progression and is a poor prognostic factor for lung and colon cancer (Uemura et al. 2006; Kasuga et al. 2001; Mroczko et al. 2007). However, our study revealed that monocytosis, but not leukocytosis, was an independent prognostic factor for patients with head and neck cancers (P = 0.028, Table 3); this is the first report regarding the prognostic significance of monocytosis in head and neck cancer patients. A possible explanation for this observation is that monocytosis might be associated with the increased number of bone marrow-derived myelomonocytic cells, which can stabilize the tumor vasculature (Ahn and Brown 2008; De Palma et al. 2003; Lyden et al. 2001). Bone marrow-derived myelomonocytic cells may infiltrate the tumor and differentiate into tumor-associated macrophages, which release many angiogenic factors, including vascular endothelial growth factor, tumor necrosis factor alpha, and matrix metalloproteinase-9 (Dirkx et al. 2006; Lewis and Pollard 2006; Yang et al. 2004). Pollard (2004) also found that the presence of increasing numbers of tumor-associated macrophages was associated with poor prognosis in cancers.
Anemia is a well-established poor prognostic factor in several types of cancers (Caro et al. 2001). Becker et al. reported that severe anemia is associated with poor tumor oxygenation (Becker et al. 2000). Intratumoral hypoxia is an important factor in radioresistance (Hockel et al. 1996) and activation of hypoxia-inducible factor-1 (HIF-1) promotes tumor metastasis (Yang et al. 2008). Platelets can release vascular endothelial growth factor (VEGF) to promote tumor angiogenesis and to create a hyper-permeable environment for the extravasations of circulating tumor cells (Patruno et al. 2008; Verheul et al. 2000). This result confirms the prognostic role of thrombocytosis in head and neck cancers, which is consistent with previous reports (Lu et al. 2007).
The limitation of current study is in its retrospective analysis: the treatment modalities were not uniform and randomized. The impact of various treatments related outcome could not be evaluated in this study. Confirming the prognostic effect of pretreatment hematologic profile in studies with prospective design is mandatory.
In conclusion, our study is the first to demonstrate that monocytosis is a prognostic factor for patients with head and neck cancer. Abnormalities in more than one lineage of blood cells has a cumulative effect on the prognosis. This suggests that abnormalities in more than one lineage of blood cells is an important sign of more severe disease because changes in the pretreatment hematologic profile may reflect systemic responses to disseminated cancer. We therefore suggest that a pretreatment hematologic profile can serve as a useful marker to predict outcome of patients with head and neck cancer.
References
Ahn GO, Brown JM (2008) Matrix metalloproteinase-9 is required for tumor vasculogenesis but not for angiogenesis: role of bone marrow-derived myelomonocytic cells. Cancer Cell 13:193–205. doi:10.1016/j.ccr.2007.11.032
Baghi M, Wagenblast J, Hambek M, Moertel S, Gstoettner W, Strebhardt K, Knecht R (2008) Pre-treatment haemoglobin level predicts response and survival after TPF induction polychemotherapy in advanced head and neck cancer patients. Clin Otolaryngol 33:245–251. doi:10.1111/j.1749-4486.2008.01702.x
Becker A, Stadler P, Lavey RS, Hänsgen G, Kuhnt T, Lautenschläger C, Feldmann HJ, Molls M, Dunst J (2000) Severe anemia is associated with poor tumor oxygenation in head and neck squamous cell carcinomas. Int J Radiat Oncol Biol Phys 46:459–466. doi:10.1016/S0360-3016(99)00384-3
Brockmann MA, Giese A, Mueller K et al (2007) Preoperative thrombocytosis predicts poor survival in patients with glioblastoma. Neuro-oncol 9:335–342. doi:10.1215/15228517-2007-013
Caro JJ, Salas M, Ward A et al (2001) Anemia as an independent prognostic factor for survival in patients with cancer: a systemic, quantitative review. Cancer 91:2214–2221. doi:10.1002/1097-0142(20010615)91:12<2214::AID-CNCR1251>3.0.CO;2-P
Chen CC, Chang JY, Liu KJ et al (2005) Hepatocellular carcinoma associated with acquired von Willebrand disease and extreme thrombocytosis. Ann Oncol 16:988–989. doi:10.1093/annonc/mdi171
Cox DR (1972) Regression models and life tables. J R Stat Soc Ser 34:187–220
De Palma M, Venneri MA, Roca C et al (2003) Targeting exogenous genes to tumor angiogenesis by transplantation of genetically modified hematopoietic stem cells. Nat Med 9:789–795. doi:10.1038/nm871
Department of Health (2004) The Executive Yuan cancer registry annual report in Taiwan area. Department of Health, ExecutiveYuan, ROC
Dirkx AE, Oude Egbrink MG, Wagstaff J et al (2006) Monocyte/macrophage infiltration in tumors: modulators of angiogenesis. J Leukoc Biol 80:1183–1196. doi:10.1189/jlb.0905495
Dunst J, Kuhnt T, Strauss HG et al (2003) Anemia in cervical cancers: impact on survival, patterns of relapse, and association with hypoxia and angiogenesis. Int J Radiat Oncol Biol Phys 56:778–787. doi:10.1016/S0360-3016(03)00123-8
Gogus C, Baltaci S, Filiz E et al (2004) Significance of thrombocytosis for determining prognosis in patients with localized renal cell carcinoma. Urology 63:447–450. doi:10.1016/j.urology.2003.10.039
Greene FL, Leslie HS (2008) The staging of cancer: a retrospective and prospective appraisal. CA Cancer J Clin 58:180–190. doi:10.3322/CA.2008.0001
Greene FL, Page DL, Fleming ID et al (2002) AJCC cancer staging manual, 6th edn. Springer, New York
Hockel M, Schlenger K, Mitze M et al (1996) Hypoxia and radiation response in human tumors. Semin Radiat Oncol 6:3–9. doi:10.1016/S1053-4296(96)80031-2
Ikeda M, Furukawa H, Imamura H et al (2002) Poor prognosis associated with thrombocytosis in patients with gastric cancer. Ann Surg Oncol 9:287–291
Kasuga I, Makino S, Kiyokawa H et al (2001) Tumor-related leukocytosis is linked with poor prognosis in patients with lung carcinoma. Cancer 92:2399–2405. doi:10.1002/1097-0142(20011101)92:9<2399::AID-CNCR1588>3.0.CO;2-W
Lewis CE, Pollard JW (2006) Distinct role of macrophages in different tumor microenvironments. Cancer Res 66:605–612. doi:10.1158/0008-5472.CAN-05-4005
Lu CC, Chang KW, Chou FC et al (2007) Association of pretreatment thrombocytosis with disease progression and survival in oral squamous cell carcinoma. Oral Oncol 43:283–288. doi:10.1016/j.oraloncology.2006.03.010
Lyden D, Hattori K, Dias S et al (2001) Impaired recruitment of bone-marrow-derived endothelial and hematopoietic precursor cells blocks tumor angiogenesis and growth. Nat Med 7:1194–1201. doi:10.1038/nm1101-1194
Mroczko B, Groblewska M, Wereszczynska-Siemiatkowska U et al (2007) Serum macrophage-colony stimulating factor levels in colorectal cancer patients correlate with lymph node metastasis and poor prognosis. Clin Chim Acta 380:208–212. doi:10.1016/j.cca.2007.02.037
Parkin DM, Bray F, Ferlay J et al (2001) Estimating the world cancer burden: Globocan 2000. Int J Cancer 94:153–156. doi:10.1002/ijc.1440
Patruno R, Arpaia N, Gadaleta CD et al (2008) VEGF concentration from plasma activated platelets rich correlates with microvascular density and grading in canine mast cell tumour spontaneous model. J Cell Mol Med 13:555–561. doi:10.1111/j.1582-4934.2008.00355.x
Pedersen LM, Milman N (1996) Prognostic significance of thrombocytosis in patients with primary lung cancer. Eur Respir J 9:1826–1830. doi:10.1183/09031936.96.09091826
Pedersen LM, Milman N (2003) Diagnostic significance of platelet count and other blood analyses in patients with lung cancer. Oncol Rep 10:213–216
Peto R, Pike MC (1973) Conservatism of the approximation sigma (O-E)2-E in the logrank test for survival data or tumor incidence data. Biometrics 29:579–584. doi:10.2307/2529177
Pollard JW (2004) Tumour-educated macrophages promote tumour progression and metastasis. Nat Rev Cancer 4:71–78. doi:10.1038/nrc1256
Rades D, Schild SE, Bahrehmand R et al (2005) Prognostic factors in the nonsurgical treatment of esophageal carcinoma with radiotherapy or radiochemotherapy: the importance of pretreatment hemoglobin levels. Cancer 103:1740–1746. doi:10.1002/cncr.20952
Rudat V, Dietz A, Schramm O et al (1999) Prognostic impact of total tumor volume and hemoglobin concentration on the outcome of patients with advanced head and neck cancer after concomitant boost radiochemotherapy. Radiother Oncol 53:119–125. doi:10.1016/S0167-8140(99)00119-X
Shimada H, Oohira G, Okazumi S et al (2004) Thrombocytosis associated with poor prognosis in patients with esophageal carcinoma. J Am Coll Surg 198:737–741. doi:10.1016/j.jamcollsurg.2004.01.022
Sugitani I, Kasai N, Fujimoto Y et al (2001) Prognostic factors and therapeutic strategy for anaplastic carcinoma of the thyroid. World J Surg 25:617–622. doi:10.1007/s002680020166
Suzuki K, Aiura K, Kitagou M et al (2004) Platelets counts closely correlate with the disease-free survival interval of pancreatic cancer patients. Hepatogastroenterology 51:847–853
Taucher S, Salat A, Gnant M et al (2003) Impact of pretreatment thrombocytosis on survival in primary breast cancer. Thromb Haemost 89:1098–1106
Uemura Y, Kobayashi M, Nakata H et al (2006) Effects of GM-CSF and M-CSF on tumor progression of lung cancer: roles of MEK1/ERK and AKT/PKB pathways. Int J Mol Med 18:365–373
Van Belle SJ, Cocquyt V (2003) Impact of haemoglobin levels on the outcome of cancers treated with chemotherapy. Crit Rev Oncol Hematol 47:1–11. doi:10.1016/S1040-8428(03)00093-3
Verheul HM, Jorna AS, Hoekman K et al (2000) Vascular endothelial growth factor-stimulated endothelial cells promote adhesion and activation of platelets. Blood 96:4216–4221
Yang L, DeBusk LM, Fukuda K et al (2004) Expansion of myeloid immune suppressor Gr+ CD11b+ cells in tumor-bearing host directly promotes tumor angiogenesis. Cancer Cell 6:409–421. doi:10.1016/j.ccr.2004.08.031
Yang MH, Wu MZ, Chiou SH et al (2008) Direct regulation of TWIST by HIF-1alpha promotes metastasis. Nat Cell Biol 10:295–305. doi:10.1038/ncb1691
Acknowledgments
This work was partially supported by the Taiwan Clinical Oncology Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, MH., Chang, P.MH., Chen, PM. et al. Prognostic significance of a pretreatment hematologic profile in patients with head and neck cancer. J Cancer Res Clin Oncol 135, 1783–1790 (2009). https://doi.org/10.1007/s00432-009-0625-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-009-0625-1