Abstract
Level V lymph node (LN) dissection has been significantly associated with postoperative shoulder dysfunction as a sequel of spinal accessory nerve (SAN) dysfunction. The aim of study was to determine the role of level V LN dissection in clinically node positive (cN+) oral cavity cancer. We have prospectively evaluated 210 patients of oral cavity squamous cell carcinoma (SCC). During neck dissection, the contents of the level V LN were dissected, labelled, and processed separately from the neck dissection specimen. We studied the prevalence of histopathologic metastasis to level V nodes in clinically node negative (cN0), cN1 and cN2 groups. Potential risk factors for the involvement of level V LN were also analysed. Of 210 cases, 48 were cN0. Out of them 77 % were pN0 and none of cNo (48) patients had level V metastases. Out of 162 cN+ cases, 112 were cN1 and 49 cN2. Amongst cN1 (112) cases, cN1 with palpable level lb LN (99), 60 % had pN0 and none of them had level V LN involvement but cN1 with palpable ll/lll LN (13), 85 % had pN+ and 1 patient had level V LN involvement (8 %). 8 patients from cN2 (49) group had level V LN involvement (16 %). Over all level V LN involvement was 4.3 %. Tongue was the most common site to give rise to level V LN metastases and extra capsular spread (ECS) was present in 100 % patient with level V LN metastases. Thus, we concluded that, apart from cN0, patients with cN1 oral cavity cancer with level lb as only site, carefully selected cases could safely undergo SND. Potential risk factors for level V LN metastases are clinically evident ECS, multiple LN involvement and cN1 with deep jugular chain of LN involvement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head and neck cancer accounts for 10 % of all malignancies worldwide and up to 40 % cancer burden in India [1]. Amongst head and neck cancers oral cavity cancer is the most common and accounting for 30 % of all cases [2]. Squamous cell carcinoma (SCC) is the most common histological type (90 %) of all the oral cavity cancer. Oral cavity cancer is the most common in Indian male with 35 % of total cases and 3rd most common in Indian female with 18 % of total cases [2]. The high incidence of cancer is attributable largely to the habit of chewing betel nuts, tobacco and pan (mixture of tobacco, lime and other substances wrapped in a vegetable leaf). In developing country like India only 10 to 15 % of cases present in localized stages [2].
Metastasis to the regional lymph node (LN) is the single most important prognostic factor in predicting local and distant failure as well as survival. The nodal metastasis reduces the survival by 50 % [3]. The primary treatment of oral cavity cancer is surgical resection with adjuvant chemoradiation therapy reserved for more advance cases, nonresectable disease or patient with significant comorbidities that would preclude surgery. There are certain observations which brought the concept of Selective neck dissection (SND) in the management of neck. First, Regional LN involvement in oral cavity squamous cell carcinoma (SCC) is in predictable and sequentially progressive manner. Level V LN involvement in oral cavity SCC is seldom. Second, despite advances in surgical and adjuvant chemoradition therapy, the diagnosis of oral cavity cancer continues to portend a poor prognosis. This is evidence by the fact that overall 5 year survival has remained essentially unchanged over the past 30 years [4]. Third and most important, level V LN dissection has been significantly associated with postoperative shoulder dysfunction as a sequel of spinal accessory dysfunction in some patients even when the nerve remains intact secondary to traction or with ischemic injury to the nerve [5, 6]. These facts lead to the shift in paradigm of neck management from Radical Neck Dissection (RND) to Modified Radical Neck Dissection (MRND) and subsequently to Selective Neck Dissection (SND). Role of SND in the management of clinically node negative (cN0) oral cavity cancer is undebatable [7, 8]. Still most of the patients of oral cavity cancer with clinically palpable LN (cN+) are subjected to comprehensive lymph node dissection. The aim of this study was to determine the role of level V LN dissection in clinically node positive (N+) oral cavity cancer and to analyse the potential risk factors for level V LN metastasis.
Patients and Methods
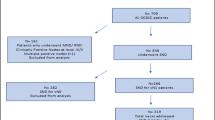
This was a prospective case series conducted in the Department of Surgical Oncology from April 2011 to June 2012. We have prospectively evaluated 210 patients of oral cavity SCC who underwent surgical treatment of the primary lesion along with a simultaneous comprehensive neck dissection in the institute during this period. Inclusion Criteria for the study was primary tumor confined to oral cavity, histological SCC type, patients who underwent surgery in our institute only. Exclusion Criteria for the study was recurrent tumor, either of primary or neck surgery done outside, patients who had taken preoperative chemotherapy or radiotherapy and patients with multiple primary tumors. All patients underwent thorough history taking, clinical examination which included oral cavity examination, indirect laryngoscopic examination, bilateral cervical examination and general examination. In all patient biopsy confirmation was done preoperatively. Patients with early lesions were evaluated by orthopentogram to assess mandibular involvement. Computer Tomography Scan or Magnetic Resonance Imaging were used as a investigation tool to confirm the local operability in indicated patients like in patients with large lesions having trismus, lesion reaching up to retro molar trigone (RMT) and lesions abutting the mandible where marginal mandibulectomy is being planned. Clinical N stage is confirmed by Ultrasonography. All patients were staged clinically using AJCC/TNM classification. During surgery, contents of the level V lymph nodes were dissected, labelled, and processed separately from neck dissection specimen. Analysis of clinical stage, pathological stage and other variables like differentiation, lymphovascular invasion (LVI), total number of LNs, positive LNs, level of involvement and extra capsular spread (ECS) were done. Chart review of the data was done to evaluate potential risk factors for level V LN metastasis.
Results
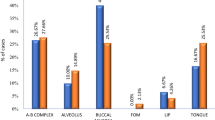
Age range in the study group was 17–78 years with mean age of 44.96 years and a median age of 44 years. The study included 155 males and 55 females (male: female ratio 2.8:1). Out of 210 oral cavity cancers, 92 had cancer of buccal mucosa/RMT (43 %), 64 had cancer of tongue/floor of mouth (31 %), 25 had cancer of alveolar process (12 %), 21 had cancer involving gingivo buccal complex (10 %) and eight had cancer of lip (4 %). Table 1 is showing distribution of primary cancer according to site of origin. Total 210 cases and 226 neck specimens were examined. In total, 5421 lymph nodes were dissected from level I to V. Average nodes per lymph node dissection was 23.98. 1458 of them were in level V with an average yield of 6.9.
Amongst 210 patients 48(23 %) patients were cN0 and 162(77 %) were clinically node positive (cN+). Out of 48 cN0 patients, 77 % were pathologically proven N0 (pN0). 23 % patients were showing occult metastasis in final report. None of the patient with cN0 stage had level V LN metastasis in their final histopathological examination (HPE) report (Table 2).
Out of 162(77 %) clinically N+ patients, 112(69 %) patients were cN1, among them 99 had level lb involvement and 13 had level ll/lll involvement. Out of 162 cN1 patients 61(54 %) patients were pN0, 28(25 %) were pN1 and 23(21 %) were pN2. None of the cN1 patients with level Ib involvement had level V LN metastasis in final report. One out of 13 patients with cN1 with level ll/lll involvement had level V LN metastasis in final HPE report (Table 3) Of note there was significant difference in pathological N stage in two subset of cN1. In patients with cN1 with palpable level lb, 60 % were pN0, 24 % were pN1 and 16 % were pN2. In patients with cN1 with palpable level ll/lll, only 15 % were pN0, 30 % were pN1 and 55 % were pN2.
Out of 162 cN+ patients, 49(30 %) patients were cN2 with 34 with multiple ipsilateral LNs (N2b), 8 patients with LN larger than 3 cm (N2a) and 7 patients with bilateral LN involvement (N2c). 1 patient with cN2b had clinically palpable LN at level V. Out of 49 cN2 patients 17 patients were pN0, 8 patients were pN1 and 24 patients were pN2. Out of 49 cN2 patients, 8 had level V LN metastasis in their final report. All of them belong to pN2b stage (Table 4).
Out of 210 patients, 9 patients (4.3 %) had metastasis to level V LN in the final report. All of them were pN2b stage. No patients had skip metastasis to level V LN in the absence of other nodal involvement in study group. Table 5 is showing comprehensively involvement of level V LN in various clinical nodal situations. All patients with level V LN metastasis had ECS and 8/9 (88.89 %) patients had LVI as shown in Table 6. Amongst oral cavity cancer tongue was the most common site, which give rise to level V LN metastasis.
Discussion
As more surgeons accept the surgical and oncological feasibility of removing involved lymph nodes along with surrounding fibro fatty tissue without removal of important uninvolved structure like spinal accessory nerve, the surgical management of node positive neck has became matter of judgement. Management of neck varies from selective neck dissection to radical neck dissection. Selective neck dissection consists of removal of only nodal groups, which are at highest risk for containing metastases, according to location of primary tumor. The concept of selective neck dissection is based on the clinical observation that SCC of upper digestive tract metastases to the cervical LN in a predictable and sequentially progressive pattern [9]. Various studies have proved the adequacy of selective LN dissection in clinically N0 patients of oral cavity cancer. Review of the literature reveals that the efficacy of selective neck dissection is comparable to comprehensive lymphadenectomy for treatment of the cN0 neck [7, 8]. Pitman et al. have previously demonstrated similar regional recurrence rates between selective neck dissection and comprehensive neck dissection in cN0 oral cavity cancer [10]. Thus, role of selective neck dissection in the management of clinically N0 oral cavity cancer is undebatable. Moreover, apart from controlling the occult metastases, it provides valuable pathological information for staging and for addition of further adjuvant therapy without compromising the oncological safety.
Andre et al. shown that with SND when performed in elective setting risk of ipsilateral nodal recurrence was 5 %, but when performed in patients with cN+ patients ipsilateral nodal recurrence was 9–15 % [11]. He further shown that incidence of occult metastasis in the cN0 patients were 24 %. In our study incidence of occult metastasis in the cN0 patients were 23 %.
Ambrosch et al. evaluated the efficacy of SND in a retrospective study of 503 patients of SCC of the upper aero digestive tract as elective and therapeutic treatment and shown that local control after SND was comparable to MRND and application of SND should be extended to advanced nodal disease [12]. In another study, Kowalski et al. evaluated the feasibility of SOHND in cN1 and cN2a oral cancer patients and shown that in patients with cN1 or cN2a at level l up to 54.7 % were pathologically N0 [13]. In present study subset analysis shown that, cN1 with level lb as an only palpable node, 60 % were pN0. These observations reflect the high incidence of palpable level lb LN in oral cavity cancer often just inflammatory in nature. Only 1 out of 13 patients (8 %) with cN1 with level ll/lll involvement had level V metastasis in final report. Devidson et al. in his results shown that incidence of level V metastasis in oral cavity cancer was around 3 % [14]. In our study, 4.3 % patients had metastasis to level V LN.
Byers et al. evaluated the pattern of regional recurrence after SND for cN+ cases, and shown that there was increase in loco regional control with the use of PORT [15]. In his study, regional recurrence for pN1 was 5 % with PORT Vs 35 % without PORT. Anderson et al. further shown loco regional control after SND with PORT in clinically as well pathological node positive patients of 94 % at 2 year [16]. PORT was given for ECS and multiple nodal involvement in that study.
Pellitteri et al. Shown bigger role for SND in selected cases with primary SCC of the upper aero digestive tract even with multiple LN positive cervical disease [17]. But in our study, all patients with level V LN involvement had pN2b, and patients with cN2b level V LN involvement were 16 %. Hence in our study, multiple palpable LN was considered potential risk factor.
John et al. shown in his study that amongst all oral cavity cancers, cancer of tongue and floor of mouth were the most common to have level V metastases [9]. In our observation, tongue was the most common site, which gives rise to level V LN metastasis.
The presence of ECS of tumor has been explored in numerous studies that demonstrated that tumor extension beyond the capsule of lymph node worsen the prognosis. Johnson et al. reported that < 40 % of the patients with histological evidence of ECS were free of disease 24 months after therapy [3]. Fertilo et al. has reported that macroscopically recognizable ECS carries a prognosis worse than that of microscopic spread [18]. In our study, all patients with HPE suggestive of level V LN metastasis had ECS. Hence, clinically evident ECS like, LN size > 3 cm (N2a), LN fixed with mandible, skin or adjacent structures, matted nodal mass were considered potential risk factors in our study.
Conclusion
In the management of patients with clinically node negative oral cavity cancer, selective neck dissection is the standard of care. In patients with clinically N2 and N3 oral cavity cancers comprehensive neck dissection is essential in order to achieve good loco-regional control.
Among patients of oral cavity cancer with clinical N1 disease, patients with clinically palpable level ll or lll LN comprehensive neck dissection is appropriate as there are high risk of level V lymph node metastasis in such patients. Patients with clinically N1 oral cavity cancer with level lb as only site, carefully selected patients can safely undergo selective neck dissection.
Potential risk factors for level V lymph node metastases are: clinically evident extra capsular spread like lymph node size > 3 cm, lymph node fixed with mandible, skin or adjacent structures, matted lymph node, multiple lymph node involvement, cN1 with deep jugular chain of lymph node involvement and tongue/floor of mouth as a primary site.
These are the interim results of an ongoing study and we hope to derive robust evidence by comparing selective neck dissections to comprehensive neck dissections in addressing neck in patients with clinically node positive oral cavity cancer.
References
Parkin DM, Pisani P, Ferlay J (1999) Global cancer statistics. CA Cancer J Clin 49:33–64
Sankaranarayanan R (1998) Head and Neck cancer: a global prospective on epidemiology and prognosis. Anticancer Res 18:4779–4786
Johnson JT (1995) Cervical LN metastases. Arch Otolaryngol 111:534–537
Moore S, Jhonson A, Pierce A (2006) The epidemiology of mouth cancer. Oral Dis 6:65–74
Cheng PT, Hao SP, Lin YH, Yeh AR (2000) Objective comparison of shoulder dysfunction after three neck dissection techniques. Ann Otol Rhinol Laryngol 109(8):761–766
Pieter UD, Paul CV (2001) Incidence of shoulder pain after neck dissection: a clinical explorative study for risk factors. Head & Neck 23(11):947–953
Sefik Hosal A, Ricardo LC (2000) Selective neck dissection in the management of clinically N0 neck. Laryngoscope 110(12):2037–2040
Ferlito A, Rinaldo A (1998) Selective lateral neck dissection for laryngeal cancer with limited metastatic disease: is it indicated? J Laryngol Otol 112:1031–1033
John WW, Diana HE (2003) Elective management of the clinically negative neck in patients with oral tongue cancer. Arch Otolaryngol Head Neck Surg 129(1):83–88
Pitman KT, Johnson JT, Myers EN (1997) Effectiveness of selective neck dissection for management of the clinically negative neck. Arch Otolaryngol Head Neck Surg 123:917–922
André LC, Luiz PK (2000) Ipsilateral neck cancer recurrences after elective supraomohyoid neck dissection. Arch Otolaryngol Head Neck Surg 126(3):410–412
Ambrosch P, Kron M, Pradier O, Steiner W (2001) Efficacy of selective neck dissection: a review of 503 cases of elective and therapeutic treatment of the neck in squamous cell carcinoma of the upper aerodigestive tract. Otolaryngol Head Neck Surg 124:180–187
Kowalski LP, Carvalho AL (2002) Feasibility of supraomohyoid neck dissection in N1 and N2a oral cancer patients. Head Neck 24:921–92
Davidson BJ, Culkarny V, Delacure MD, Shah JP (1993) Posterior triangle metastases of squamous cell carcinoma of the upper aerodigestive tract. Am J Surg 166:395–398
Byers RM, Clayman GL (1999) Selective neck dissections for squamous carcinoma of the upper aerodigestive tract: Patterns of regional failure. Head & Neck 21(6):499–505
Anderson PE, Warren F, Spiro J, Shah JP et al (2002) Results of selective neck dissection in management of the node-positive neck. Arch Otolaryngol Head Neck Surg 128:1180–4
Pellitteri PK, Robbins KT, Neuman T (1997) Expanded application of selective neck dissection with regard to nodal status. Head & Neck 19(4):260–265
Fertilo A, Rinaldo A (2002) Prognostic significance of microscopic and macroscopic extracapsular spread from metastatic tumor in cervical lymph nodes. Oral Oncol 38:747–751
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Parikh, D.G., Chheda, Y.P., Shah, S.V. et al. Significance of Level V Lymph Node Dissection in Clinically Node Positive Oral Cavity Squamous Cell Carcinoma and Evaluation of Potential Risk Factors for Level V Lymph Node Metastasis. Indian J Surg Oncol 4, 275–279 (2013). https://doi.org/10.1007/s13193-013-0241-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-013-0241-z