Abstract
Background
Positron emission tomography/computed tomography (PET/CT) with 2-deoxy-2-[18F]fluoro-D-glucose (FDG) has become the standard of care for the initial staging and subsequent treatment response assessment of many different malignancies. Despite this success, PET/CT is often supplemented by MRI to improve assessment of local tumor invasion and to facilitate detection of lesions in organs with high background FDG uptake. Consequently, PET/MRI has the potential to expand the clinical value of PET examinations by increasing reader certainty and reducing the need for subsequent imaging. This study evaluates the ability of FDG-PET/MRI to clarify findings initially deemed indeterminate on clinical FDG-PET/CT studies.
Methods
A total of 190 oncology patients underwent whole-body PET/CT, immediately followed by PET/MRI utilizing the same FDG administration. Each PET/CT was interpreted by our institution's nuclear medicine service as a standard-of-care clinical examination. Review of these PET/CT reports identified 31 patients (16 %) with indeterminate findings. Two readers evaluated all 31 PET/CT studies, followed by the corresponding PET/MRI studies. A consensus was reached for each case, and changes in interpretation directly resulting from PET/MRI review were recorded. Interpretations were then correlated with follow-up imaging, pathology results, and other diagnostic studies.
Results
In 18 of 31 cases with indeterminate findings on PET/CT, PET/MRI resulted in a more definitive interpretation by facilitating the differentiation of infection/inflammation from malignancy (15/18), the accurate localization of FDG-avid lesions (2/18), and the characterization of incidental non-FDG-avid solid organ lesions (1/18). Explanations for improved reader certainty with PET/MRI included the superior soft tissue contrast of MRI and the ability to assess cellular density with diffusion-weighted imaging. The majority (12/18) of such cases had an appropriate standard of reference; in all 12 cases, the definitive PET/MRI interpretation proved correct. These 12 patients underwent six additional diagnostic studies to clarify the initial indeterminate PET/CT findings. In the remaining 13 of 31 cases with indeterminate findings on both PET/CT and PET/MRI, common reasons for uncertainty included the inability to distinguish reactive from malignant lymphadenopathy (4/13) and local recurrence from treatment effect (2/13).
Conclusions
Indeterminate PET/CT findings can result in equivocal reads and additional diagnostic studies. PET/MRI may reduce the rate of indeterminate findings by facilitating better tumor staging, FDG activity localization, and lesion characterization. In our study, PET/MRI resulted in more definitive imaging interpretations with high accuracy. PET/MRI also showed potential in reducing the number of additional diagnostic studies prompted by PET/CT findings. Our results suggest that whole-body PET/MRI provides certain diagnostic advantages over PET/CT, promotes more definitive imaging interpretations, and may improve the overall clinical utility of PET.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Positron emission tomography/computed tomography (PET/CT), utilizing the glucose analogue, 2-deoxy-2-[18F]fluoro-D-glucose (FDG), has become the standard of care for the initial staging and subsequent treatment response assessment of many different malignancies [1]. Despite its success, PET/CT is often supplemented by magnetic resonance imaging (MRI) to answer specific clinical questions not adequately addressed by this hybrid modality. For example, colorectal liver metastases, the presence of which can significantly alter clinical management, can be difficult to detect on PET/CT due to high background FDG uptake. Liver MRI including diffusion-weighted imaging (DWI) has already been shown to be more sensitive than PET/CT for hepatic metastases and consequently is routinely ordered in this setting to achieve accurate staging [2]. Likewise, while PET/CT is often obtained to evaluate for distant metastases from cervical cancer, pelvic MRI, with its high soft tissue contrast, provides superior accuracy for local staging [3]. Thus, simultaneous PET/MRI has the potential to provide complete oncologic staging for many different malignancies, including colorectal and cervical cancer, in a single imaging examination.
In addition to the potential diagnostic advantages afforded by combining PET and MRI, PET/MRI may reduce the likelihood that a patient undergoing whole-body PET imaging will require a second imaging examination to evaluate a finding deemed indeterminate at initial recognition. For example, indeterminate liver lesions identified on PET/CT are often referred to MRI for definitive characterization, resulting in additional time and expense. One group has already evaluated the effects of PET/MRI on the frequencies of incidental lesions in the abdomen, finding that significantly fewer incidental lesions were classified as indeterminate on PET/MRI compared with PET/CT [4]. A different group of investigators evaluating the clinical impact of whole-body PET/MRI versus whole-body PET/CT in an oncology population found that the former identified significantly more findings that altered clinical management [5]. In light of these prior studies, the aims of our study were threefold: (1) to assess the rate of indeterminate findings on clinical FDG-PET/CT at our institution and their impact on clinical management; (2) to determine whether PET/MRI, acquired for these same patients, would have yielded more definitive interpretations (i.e., fewer indeterminate reads); and (3) to estimate the impact that utilizing PET/MRI instead of PET/CT as the primary imaging examination could have had on clinical management (e.g., avoidance of surgery or biopsy, fewer follow-up imaging studies, etc.).
Methods
Patient Characteristics
A total of 190 oncology patients provided informed consent to participate in an Institutional Review Board-approved study pertaining to the optimization of clinical PET/MRI protocols (Table 1). The most common clinical indications for PET imaging were the initial staging and the subsequent restaging of malignancy. Fasting for at least 4 hours and blood glucose levels ≤150 mg/dl were required for PET imaging. Patients received a mean weight-based FDG dose of 14.4 mCi (range 5.2 – 23.8 mCi).
Image Acquisition
All patients underwent standard-of-care PET/CTs on a Biograph 40 PET/CT or mCT (Siemens Healthcare; Erlangen, Germany), immediately followed by PET/MRI utilizing the same FDG administration. CT images were obtained without intravenous contrast according to our standard institutional protocol, for both anatomic correlation of PET findings and attenuation correction. The following CT parameters were used: 120 kV, 110 mAs (effective, Siemens CareDose), 5 mm slice thickness, 4 mm slice spacing. PET data were acquired using 5-6 bed positions, depending on patient height, to achieve standard coverage from the skull base through the proximal thighs. Emission times were 2-3 min per bed position. For patients also undergoing imaging of the head/neck region or of the distal lower extremities, additional PET bed positions were required. For PET/CT acquisition, the mean time interval between FDG injection and the beginning of imaging (FDG uptake time) was 62 min (standard deviation ± 15 min; range 50-97 min).
Following completion of the PET/CT, patients then underwent PET/MRI on an integrated Biograph mMR scanner (Siemens Healthcare; Erlangen, Germany). Images were obtained according to either a whole-body protocol or a locally focused protocol, depending on the patient’s underlying diagnosis and the needs of our clinical research facility in terms of calibrating various acquisition conditions. The details of our institution’s standard PET/MRI protocols have been previously published [6]. As a result, MR sequences varied from patient to patient. Commonly employed sequences are described in Table 2.
The T1W Dixon volumetric interpolated breath-hold examination (VIBE) sequence was acquired in a two-point fashion (using two different echo times) to generate in/opposed-phase images for attenuation correction, with a standard four-class segmentation algorithm (soft tissue, fat, lung, air). Other sequences were obtained for anatomic correlation of the PET findings. For the standard skull base through proximal thighs protocol, PET data were acquired using 4-5 bed positions, depending on patient height. Emission times were 3-4 min per bed position. As with PET/CT, some patients also underwent dedicated imaging of the lower extremities or head/neck region, requiring additional PET bed positions. For patients scanned according to one of several locally focused protocols, fewer than 4-5 PET bed positions were necessary. The mean FDG uptake time for PET/MRI was 127 min (standard deviation ± 16 min; range 102-157 min). Once PET/MRI began, the mean MR acquisition time was 59 min (standard deviation ± 19 min; range 10-125 min).
Image Analysis
Our institution’s nuclear medicine physicians interpreted all 190 PET/CTs as standard-of-care clinical examinations and generated corresponding reports. For our retrospective study, a single investigator reviewed the reports for these examinations, and 53 patients (28 %) with indeterminate findings were identified. Medical records were reviewed to determine the impact on management arising from these indeterminate findings (e.g., biopsy, additional imaging, endoscopy, etc). All PET/CT and PET/MRI examinations for these patients were transferred into the MIM software package (MIM Software, Inc.; Cleveland, OH) for viewing. Two board-certified radiologists, one specializing in nuclear medicine (J.M.) and one specializing in body MRI (K.F.), were provided with basic clinical information for each case, including oncologic diagnosis, treatment history, and indication for PET imaging. These readers, blinded to follow-up imaging and clinical outcomes for each patient, jointly reviewed the PET/CT examination for each patient to confirm the presence of indeterminate findings. The readers then jointly interpreted the corresponding PET/MRI examination. A consensus was reached for each case, both before and after the addition of the PET/MRI data. Changes in interpretation directly resulting from PET/MRI review were recorded and categorized. When available, follow-up imaging and subsequent biopsy or surgery results served as the standard of reference.
Results
Aim 1: Frequency of Indeterminate PET/CT Findings
Of the 190 total patients, 53 cases with indeterminate findings were identified. Twenty-one cases were excluded due to incomplete anatomic coverage of the corresponding PET/MRI (e.g., some oncologic patients underwent cardiac PET/MRI as part of an optimization protocol; hence, extrathoracic PET/CT findings were not captured by PET/MRI). The PET/CT images for the remaining 32 cases were jointly reviewed by our two-reader team. One additional case was excluded because both reviewers felt that the reportedly indeterminate finding was in fact definitive for malignancy on PET/CT. A total of 31 cases were confirmed to have indeterminate findings in keeping with those described in the PET/CT reports issued by our institution’s clinical PET service. The distribution of malignancies for these 31 patients is shown in Table 1. Indeterminate findings on the clinical PET/CT interpretation resulted in recommendations for biopsy, additional imaging, or additional diagnostic tests in 12 of the 31 cases. Table 3 (six of 13 cases) and Table 4 (six of 18 cases) list these 12 cases individually.
Aim 2: Clarification of Indeterminate PET/CT Findings by PET/MRI
For 13 of the 31 cases with indeterminate findings on PET/CT, the consensus interpretation reached by the two-reader team was unchanged by subsequent review of the corresponding PET/MRI. Interpretations for the cases in which PET/MRI provided no additional diagnostic value are shown in Table 3. Reasons for persistent uncertainly included inability to distinguish reactive from malignant lymphadenopathy (4/13) and difficulty in differentiating between local tumor recurrence and treatment effect (2/13). Additional diagnostic tests were prompted by the indeterminate PET/CT findings in six of these 13 cases, resulting in a diagnosis of malignancy in only one of these six cases (Table 3).
In contrast, for 18 of the 31 cases (58 %) with indeterminate findings on PET/CT, PET/MRI did ultimately alter the initial imaging interpretation. The initial PET/CT interpretations and consensus interpretations after review of the corresponding PET/MRI are shown in Table 4. The most common change in interpretation involved the differentiation of malignant from benign causes of increased FDG uptake (15/18); the lack of an MRI correlate resulted in a consensus of inflammation rather than malignancy in 12 of these 15 cases, while the visibility of a correlate on DWI led to a consensus of metastatic disease in three of these 15 cases. PET/MRI also allowed for better anatomic localization of increased FDG activity (2/18) and for definitive diagnosis of a benign cyst rather than an indeterminate solid lesion (1/18).
Aim 3: Verification of PET/MRI Interpretations and Effects on Clinical Management
The consensus interpretation after PET/MRI review was confirmed to be correct by subsequent imaging, pathology, or surgery for 12 of the 18 cases in which PET/MRI altered the initial PET/CT interpretation (Table 4). The remaining six cases had no suitable follow-up available to serve as a standard of reference. The potential impact of PET/MRI on clinical management is also reflected in the number of unnecessary additional tests that may have been avoided with PET/MRI. For patients in whom the PET/MRI yielded a more definitive interpretation, six of 18 patients underwent potentially unnecessary additional testing as a result of the PET/CT reading (Table 4). The PET/MRI interpretations for all six of these cases were confirmed to be correct by the standard of reference.
Discussion
Indeterminate PET/CT findings can result in equivocal interpretations, potentially reducing the clinical utility of PET. Moreover, indeterminate PET/CT findings often require additional imaging (e.g., MRI, ultrasound, contrast-enhanced CT) for further characterization, thereby delaying clinical decision-making, increasing medical expenses, and resulting in additional inconvenience to the patient. In some scenarios, such indeterminate findings even result in invasive procedures such as biopsies or surgical resections. In light of the superb soft tissue contrast of MRI and its ability to assess cellular density with DWI [7], we anticipated that PET/MRI might reduce indeterminate PET/CT findings by facilitating more conclusive lesion characterization.
As expected, our study found that PET/MRI review resulted in more definitive interpretations of indeterminate PET/CT findings for the majority (18 of 31; 58 %) of cases. These results are in keeping with those of a study of 173 oncology patients by Schaarschmidt et al. that compared the numbers of incidental abdominal lesions for PET/CT versus PET/MRI [4]. While PET/MRI identified more incidental abdominal lesions than PET/CT (635 v. 407, p < 0.001), there were also significantly fewer incidental lesions categorized as indeterminate by PET/MRI than by PET/CT (27 v. 91, p <0.001). Notably, in this study, the CT component was contrast-enhanced, suggesting that PET/MRI would likely have performed even better in this regard when evaluated against the standard noncontrast PET/CT protocols used by many institutions. For the remaining 13 of 31 patients in our study with indeterminate reads on both PET/CT and PET/MRI, the uncertain findings were sufficiently concerning and/or clinically relevant to the referring physicians to prompt further work-up in just six of 13 cases; furthermore, in only one of these six cases was malignancy found as a consequence of that evaluation. This result highlights the importance of viewing PET data in the broader clinical context and acting only on uncertain findings that are anticipated to make a significant difference in patient management.
Of the 18 cases in our study for which PET/MRI resulted in a more definitive interpretation than PET/CT, 12 cases (67 %) had adequate clinical information available to serve as a standard of reference. Importantly, the PET/MRI interpretation proved to be correct for all 12 of these cases (100 % accuracy). Most commonly (eight of 12 cases), the lack of an anatomic correlate on MRI in a region of increased FDG uptake resulted in a definitive PET/MRI diagnosis of inflammation, instead of the malignancy versus inflammation interpretation from the corresponding PET/CT (Fig. 1). These cases speak to the increased confidence and accuracy with which PET/MRI allows readers to exclude an underlying malignancy in an area of indeterminate FDG uptake, likely due largely to the intrinsically higher soft tissue contrast of MRI. Similarly, several other studies, citing the high soft tissue contrast of MRI, have already suggested that PET/MRI may outperform PET/CT in the initial local tumor (T) staging of head/neck squamous cell carcinoma [8] and gynecologic malignancy [3, 9], as well as in detecting intra-pelvic recurrence of gynecologic tumors [10] and diagnosing osseous metastases from various primary tumors [11]. This particular advantage of MRI may also reduce the false positive rate of PET/MRI relative to PET/CT, thereby limiting the number of unnecessary additional imaging studies or biopsies, as discussed below. Of course, PET/MRI has not proven superior to PET/CT for all organ systems. For example, one study has found no significant difference between PET/MRI and PET/CT in terms of staging accuracy for non-small cell lung cancer [12]. Similarly, another set of authors noted that PET/CT outperformed PET/MRI in the detection of non-FDG-avid and small (i.e., <5 mm) pulmonary nodules [13].
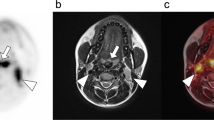
PET/MRI clarification of indeterminate PET/CT findings via superior soft tissue contrast. A 29-year-old woman with newly diagnosed squamous cell carcinoma of the cervix status-post loop electrosurgical excision procedure (LEEP) presented for initial staging. PET/CT (a, d) and PET/MRI (b-c, e-f) examinations were performed. Transaxial CT images (a) obtained near the level of the external cervical os (ECO) revealed a subcentimeter hypodensity (arrow), which corresponded to a focus of increased FDG uptake (arrow) on transaxial CT images with PET fusion (d). It was unclear whether this hypodensity represented a small soft tissue mass versus a small amount of fluid at the ECO. Consequently, this finding was interpreted as residual malignancy versus inflammation from the recent LEEP. The subsequent PET/MRI examination also showed increased FDG uptake (arrow) near the ECO on transaxial SPACE images with PET fusion (e). However, transaxial (b) and sagittal (c) SPACE images clearly demonstrated that this focus of hypodensity on CT corresponded to T2-hyperintense fluid within the ECO (arrowheads). No discrete soft tissue mass was appreciated on SPACE. Similarly, contrast-enhanced transaxial VIBE images (f) revealed a focal area of hypointensity (arrow) rather than an enhancing soft tissue mass. Overall, PET/MRI review resulted in an interpretation of “no cervical mass to indicate residual disease,” a conclusion corroborated by a repeat cervical biopsy 3 weeks later that was negative for malignancy
Compared with PET/CT, PET/MRI has been shown by Catalano et al. to have significantly higher rates of actionable findings that substantially alter clinical management [5]. While mostly due to failures of PET/CT to detect certain PET/MRI findings, the results of Catalano et al. were also partly attributable to cases in which PET/MRI interpretations were more definitive than PET/CT interpretations. In our study, six of the 18 patients with indeterminate findings on PET/CT but not on PET/MRI underwent dedicated work-ups of these findings, as prompted by the PET/CT interpretations. Because these diagnostic evaluations would likely not have been triggered by interpretations of the corresponding PET/MRIs, these six patients could have been (correctly) spared three additional imaging studies, two biopsies, and one colonoscopy. While our sample size is small, the rates of indeterminate PET/CT findings in this study generally mirror those encountered in our clinical practice. The additional diagnostic studies prompted by such indeterminate PET/CT findings can have a considerable impact when viewed on the larger population scale. Thus, if used as a primary all-in-one modality for the whole-body evaluation of oncologic conditions, PET/MRI may decrease the number of unnecessary diagnostic tests performed as a result of PET imaging; such a reduction has the potential to result in cost savings, improved patient comfort/convenience, and greater diagnostic efficiency. Further research is still needed to provide more robust evidence for these particular advantages of PET/MRI over PET/CT.
DWI constitutes an additional advantage of PET/MRI over PET/CT in the diagnosis and exclusion of malignancy in regions of abnormal FDG uptake. In our study, there were three cases (though only one of which had an adequate standard of reference for confirmation) in which DWI findings resulted in a definitive PET/MRI diagnosis of malignancy, instead of an interpretation on PET/CT of inflammation versus malignancy (Fig. 2). The value of incorporating DWI into whole-body staging protocols has already been demonstrated for the metastatic evaluation of organs with high background FDG uptake [14] and for the initial staging of newly diagnosed lymphoma [15]. Overall, our observations, in conjunction with the results of these other studies, indicate that DWI may play an important role in making sense of otherwise indeterminate PET findings.
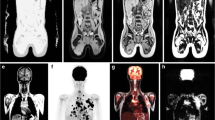
PET/MRI clarification of indeterminate PET/CT findings by DWI. A 50-year-old woman with newly diagnosed anal/rectal carcinoma presented for initial staging. PET/CT (a, d) and PET/MRI (b-c, e-f) examinations were performed. Transaxial CT images (a) with PET fusion (d) revealed multiple subcentimeter lymph nodes, increased in number but not in size, within the presacral fat (oval). The lymph nodes were too small to resolve on the PET images. These findings were deemed indeterminate, and a differential of malignant versus reactive lymphadenopathy was provided. Similarly, the subsequent PET/MRI examination showed multiple tiny lymph nodes in the presacral fat on transaxial HASTE images (b) but no definite PET correlate on the transaxial HASTE images with PET fusion (e). In contrast, transaxial DWI (c) and the apparent diffusion coefficient (ADC) map (f) demonstrated multiple small foci of restricted diffusion (arrows) within the presacral fat, corresponding to the lymph nodes identified on HASTE and CT images. In light of the conspicuity of these lymph nodes on DWI, review of the PET/MRI resulted in a more definitive diagnosis of nodal metastatic disease. The patient was treated with pelvic radiation and systemic chemotherapy. Subsequent imaging showed no evidence of residual malignancy
Another benefit of integrated PET/MRI over PET/CT is the robust set of MRI-based strategies for the motion correction of PET images, including respiratory navigation and deformable registration algorithms [16, 17]. In our study, we identified two cases in which a focus of increased FDG uptake on PET/CT localized to an organ or lymph node station uncommonly involved by the patient’s primary malignancy; these sites of FDG uptake were consequently deemed indeterminate (Fig. 3). In contrast, on the corresponding PET/MRI examinations, these FDG-avid foci instead localized to different, more expected anatomic structures, resulting in more definitive interpretations. In both cases, the PET/MRI interpretation was subsequently confirmed by the standard of reference. Along these lines, a study of 13 patients with known metastatic lesions comparing spatial registration between PET images and anatomic images found significantly less misregistration on integrated PET/MRI than on PET/CT [18]. This reduction in registration errors may result in more definitive and accurate image interpretations.
PET/MRI clarification of indeterminate PET/CT findings due to better spatial registration of PET images. An 81-year-old woman with retroperitoneal liposarcoma status-post resection and right radical nephrectomy presented for restaging. PET/CT (a, c) and PET/MRI (b, d) examinations were performed. Transaxial CT images (a) with PET fusion (c) revealed a focus of increased FDG uptake in the spleen (arrow) without any clear CT correlate. This splenic lesion was called indeterminate given that the spleen would be an atypical location for a liposarcoma metastasis. Differential considerations included metastatic disease versus an inflammatory or infectious process. On the subsequent PET/MRI, transaxial post-contrast VIBE images (b) with PET fusion (d) showed an enhancing, hypermetabolic lymph node near the splenic hilum (arrow) but no splenic lesion. This finding suggested that the PET images from the PET/CT examination had been misregistered to the CT images. This focus of increased FDG uptake within an enhancing lymph node was felt to be more consistent with a nodal metastasis than an infectious/inflammatory process. Subsequent PET imaging continued to show no splenic lesions
Our study has several limitations that should be recognized. The number of cases with indeterminate PET/CT findings was relatively low. In practice, the utility of PET/CT is hindered by frequent false positives. Our results and those of others [4] suggest that the rate of false positive reads may be reduced with PET/MRI. However, because six of the 18 cases in which PET/MRI altered the original PET/CT interpretation lacked an adequate standard of reference, our study may underestimate the rate at which PET/MRI results in false positive interpretations. Additionally, the constellation of malignancies included in our analysis was dependent on our institutional referral patterns, which may have contributed to sampling bias, thereby reducing the generalizability of our results. Our retrospective study design involved only a single team of two readers, precluding analysis of interobserver variability. This design reflects our current practice model, as well as that of several other institutions, for interpreting PET/MRI examinations. Because cases were identified on the basis of the PET/CT interpretation, we were unable to address the complementary question of whether PET/CT is likewise capable of clarifying findings initially deemed indeterminate on PET/MRI. Finally, all PET/MRI examinations were performed after the corresponding PET/CT examination, introducing systematic differences in FDG uptake time; however, the resulting differences in FDG distribution between PET/MRI and PET/CT were not identified as the reason for offering a more definitive interpretation on PET/MRI for any of the analyzed cases.
Conclusions
Despite its proven utility for whole-body staging, oncologic PET/CT is often supplemented by locally focused MRI, both routinely to improve staging accuracy and as needed to answer specific clinical questions. Consequently, whole-body PET/MRI has the potential to provide more definitive reads and hence to prompt fewer additional imaging tests, biopsies, or even surgical resections. Our study found that PET/MRI provides such clarification in more than half of cases with inconclusive imaging features on PET/CT. PET/MRI proved more capable of differentiating malignancy from inflammation, precisely localizing PET findings to appropriate anatomic structures, and characterizing certain incidental lesions. Furthermore, the more definitive interpretations resulting from PET/MRI review of initially indeterminate PET/CT findings were accurate in all cases that had an adequate standard of reference. The final impact of PET/MRI was a potentially substantial reduction in unnecessary additional diagnostic tests, though our study may underestimate the false positive rate of PET/MRI. Overall, our results suggest that whole-body PET/MRI provides certain diagnostic advantages over PET/CT, promotes more definitive imaging interpretations, and may increase the clinical value of PET imaging.
Abbreviations
- ADC:
-
apparent diffusion coefficient
- CT:
-
computed tomography
- DWI:
-
diffusion-weighted imaging
- ECO:
-
external cervical os
- FA:
-
flip angle
- FDG:
-
2-deoxy-2-[18F]fluoro-D-glucose
- FOV:
-
field of view
- FS:
-
fat saturation
- HASTE:
-
half-Fourier acquisition single-shot turbo spin echo
- PET:
-
positron emission tomography
- Q-fat sat:
-
quick fat saturation mode
- SPACE:
-
sampling perfection with application of optimized contrasts using different flip angle evolution
- ST:
-
slice thickness
- T1W:
-
T1-weighted
- T2W:
-
T2-weighted
- TE:
-
time to echo
- TR:
-
time to repetition
- TSE:
-
turbo spin echo
- VIBE:
-
volumetric interpolated breath-hold examination
References
Fletcher JW, Djulbegovic B, Soares HP, Siegel B, Lowe VJ, Lyman GH, et al. Recommendations on the use of 18F-FDG PET in oncology. J Nucl Med. 2008;49:480–508.
Coenegrachts K, De Geeter F, ter Beek L, Walgraeve N, Bipat S, Stoker J, et al. Comparison of MRI (including SS SE-EPI and SPIO-enhanced MRI) and FDG-PET/CT for the detection of colorectal liver metastases. Eur Radiol. 2009;19:370–9.
Kitajima K, Suenaga Y, Ueno Y, Kanda T, Maeda T, Deguchi M, et al. Fusion of PET and MRI for staging of uterine cervical cancer: comparison with contrast-enhanced (18)F-FDG PET/CT and pelvic MRI. Clin Imaging. 2014;38:464–9.
Schaarschmidt BM, Grueneisen J, Heusch P, Gomez B, Umutlu L, Ruhlmann V, et al. Does 18F-FDG PET/MRI reduce the number of indeterminate abdominal incidentalomas compared with 18F-FDG PET/CT? Nucl Med Commun. 2015;36:588–95.
Catalano OA, Rosen BR, Sahani DV, Hahn PF, Guimaraes AR, Vangel MG, et al. Clinical impact of PET/MR imaging in patients with cancer undergoing same-day PET/CT: initial experience in 134 patients—a hypothesis-generating exploratory study. Radiology. 2013;269:857–69.
Fowler KJ, McConathy J, Narra VR. Whole-body simultaneous positron emission tomography (PET)-MR: optimization and adaptation of MRI sequences. J Magn Reson Imaging. 2014;39:259–68.
Thoeny HC, De Keyzer F. Extracranial applications of diffusion-weighted magnetic resonance imaging. Eur Radiol. 2007;17:1385–93.
Kanda T, Kitajima K, Suenaga Y, Konishi J, Sasaki R, Morimoto K, et al. Value of retrospective image fusion of 18F-FDG PET and MRI for preoperative staging of head and neck cancer: comparison with PET/CT and contrast-enhanced neck MRI. Eur J Radiol. 2013;82:2005–10.
Kitajima K, Suenaga Y, Ueno Y, Kanda T, Maeda T, Takahashi S, et al. Value of fusion of PET and MRI for staging of endometrial cancer: comparison with 18F-FDG contrast-enhanced PET/CT and dynamic contrast-enhanced pelvic MRI. Eur J Radiol. 2013;82:1672–6.
Kitajima K, Suenaga Y, Ueno Y, Kanda T, Maeda T, Makihara N, et al. Value of fusion of PET and MRI in the detection of intra-pelvic recurrence of gynecological tumor: comparison with 18F-FDG contrast-enhanced PET/CT and pelvic MRI. Ann Nucl Med. 2014;28:25–32.
Eiber M, Takei T, Souvatzoglou M, Mayerhoefer ME, Fürst S, Gaertner FC, et al. Performance of whole-body integrated 18F-FDG PET/MR in comparison to PET/CT for evaluation of malignant bone lesions. J Nucl Med. 2014;55:191–7.
Huellner MW, Barbosa F d. G, Husmann L, Pietsch CM, Mader CE, Burger IA, et al. TNM staging of NSCLC: Comparison of PET/MR and PET/CT. J Nucl Med. 2015.
Lee KH, Park CM, Lee SM, Lee JM, Cho JY, Paeng JC, et al. Pulmonary nodule detection in patients with a primary malignancy using hybrid PET/MRI: is there value in adding contrast-enhanced MR imaging? PLoS One. 2015;10:e0129660.
Reiner CS, Stolzmann P, Husmann L, Burger IA, Hüllner MW, Schaefer NG, et al. Protocol requirements and diagnostic value of PET/MR imaging for liver metastasis detection. Eur J Nucl Med Mol Imaging. 2014;41:649–58.
Van Ufford HMEQ, Kwee TC, Beek FJ, van Leeuwen MS, Takahara T, Fijnheer R, et al. Newly diagnosed lymphoma: initial results with whole-body T1-weighted, STIR, and diffusion-weighted MRI compared with 18F-FDG PET/CT. AJR Am J Roentgenol. 2011;196:662–9.
Ouyang J, Li Q, El Fakhri G. Magnetic resonance-based motion correction for positron emission tomography imaging. Semin Nucl Med. 2013;43:60–7.
Würslin C, Schmidt H, Martirosian P, Brendle C, Boss A, Schwenzer NF, et al. Respiratory motion correction in oncologic PET using T1-weighted MR imaging on a simultaneous whole-body PET/MR system. J Nucl Med. 2013;54:464–71.
Rakheja R, DeMello L, Chandarana H, Glielmi C, Geppert C, Faul D, et al. Comparison of the accuracy of PET/CT and PET/MRI spatial registration of multiple metastatic lesions. AJR Am J Roentgenol. 2013;201:1120–3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
TJF – None; KJF – Research Support, Bracco Group; JM – Research Support, Eli Lilly & Co.; Research Consultant, General Electric Healthcare; Research Consultant, Blue Earth Diagnostics Ltd.; Research Consultant, Siemens AG; FD – None
Ethical Statement
The study was approved by an institutional review board or equivalent and has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All subjects in the study gave written informed consent or the institutional review board waived the need to obtain informed consent.
Rights and permissions
About this article
Cite this article
Fraum, T.J., Fowler, K.J., McConathy, J. et al. Indeterminate Findings on Oncologic PET/CT: What Difference Does PET/MRI Make?. Nucl Med Mol Imaging 50, 292–299 (2016). https://doi.org/10.1007/s13139-016-0405-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13139-016-0405-1