Abstract
We have previously described the development of substantial, but reversible obesity in Wistar rats fed with palatable liquid nutrition (Fresubin). In this study, we investigated changes in serum hormone levels, glycemia, fat mass, adipocyte size, and gene expression of adipokines and inflammatory markers in adipose tissue of Wistar rats fed by Fresubin (i) for 5 months, (ii) up to 90 days of age, or (iii) after 90 days of age to characterize metabolic alterations and their reversibility in rats fed with Fresubin. An intra-peritoneal glucose tolerance test was also performed to determine levels of serum leptin, adiponectin, insulin, and C-peptide in 2- and 4-month-old animals. In addition, mesenteric and epididymal adipose tissue weight, adipocyte diameter, and gene expression of pro- and anti-inflammatory adipokines and other markers were determined at the end of the study. Chronic Fresubin intake significantly increased adipocyte diameter, reduced glucose tolerance, and increased serum leptin, adiponectin, insulin, and C-peptide levels. Moreover, gene expression of leptin, adiponectin, CD68, and nuclear factor kappa B was significantly increased in mesenteric adipose tissue of Fresubin fed rats. Monocyte chemotactic protein 1 messenger RNA (mRNA) levels increased in mesenteric adipose tissue only in the group fed Fresubin during the entire experiment. In epididymal adipose tissue, fatty acid binding protein 4 mRNA levels were significantly increased in rats fed by Fresubin during adulthood. In conclusion, chronic Fresubin intake induced complex metabolic alterations in Wistar rats characteristic of metabolic syndrome. However, transition of rats from Fresubin to standard diet reversed these alterations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Along with genetics, environmental factors such as an inappropriate diet and lifestyle habits play a crucial role in the development of obesity. Specifically, hyperphagia, unbalanced macronutrient profiles [4], energy density, and post-ingestion effects of diet represent major factors participating in the development of dietary obesity [31]. The etiopathogenesis of obesity is also tightly connected to metabolic syndrome, which is defined as a cluster of components, such as increased waist circumference, increased triglyceride levels, reduced high-density lipoprotein (HDL) cholesterol levels, increased blood pressure, and increased fasting glucose levels [20].
Rodent models are frequently used for the study of obesity as they readily gain weight when fed high-fat diets [11, 31, 48, 77]. One model for the induction of obesity involves the supplementation of a high-energy diet with a highly palatable liquid diet (Ensure) that induces hyperphagia [48] and overrides the homeostatic control of ingestion by activating neural systems mediating reward and motivation [46]. In our previous paper, we described an obesity model based on feeding of Wistar rats, with the liquid nutrition (Fresubin). We confirmed that increased Fresubin intake results in development of marked obesity in adult rats due to its palatability, liquidity, and macronutrient composition. Importantly, transitioning rats fed by Fresubin since weaning to solid pelleted chow at the age of puberty normalized their body weight [53]. These findings indicate that there is flexibility in the mechanisms responsible for the development of obesity in rats.
The aim of the present study was to characterize potential metabolic changes induced in obese animals fed with Fresubin in detail, so as to identify the mechanisms involved in the development of obesity in animals fed by liquid nutrition. We focused on investigating intervention-related changes in the endocrine system, visceral adipose tissue, and whole body glucose metabolism. We also investigated the effect of chronic Fresubin intake on hormonal status (concentration of leptin, adiponectin, insulin, and C-peptide), glucose tolerance, adiposity, and gene expression of inflammatory signals and markers of adipogenesis in different adipose tissue depots as well as at the systemic level. At the level of gene expression, we examined leptin, adiponectin, cluster of differentiation 68 (Cd68), nuclear factor kappa B (Nfkb), and monocyte chemotactic protein 1 (Mcp1) in mesenteric adipose tissue. Moreover, in epididymal adipose tissue, in addition to leptin and adiponectin, we also examined the expression of glucose transporter 4 (Glut4), peroxisome proliferator-activated receptor γ (Pparg), and fatty acid binding protein 4 (Fabp4). Furthermore, to study the reversibility of metabolic alterations induced by chronic Fresubin intake, the above-mentioned parameters were also investigated in rats fed by Fresubin during either the juvenile period of their lives or in adulthood, respectively.
Materials and methods
Animals
Male Wistar rats from single dams were purchased from Charles River (Germany). After weaning on the 21st day, the rats were housed four per cage and maintained under controlled laboratory conditions (12 h light–dark cycle, lights on at 6:00 a.m., ambient temperature 22 ± 1 °C, and 55 ± 10 % humidity). All experiments were performed between 08:00 and 12:00 h, and all external noises or other stressful stimuli were strictly avoided. The experiments were carried out in accordance with the Council Directive 2010/63EU of the European Parliament and the Council of 22nd September 2010 on the protection of animals used for scientific purposes.
Experimental design and diets
After weaning on the 21st day, rats were randomly divided into four experimental groups based on the type of provided diet: (1) control group (CON, n = 12) receiving standard pelleted chow during the entire study (5 months); (2) liquid nutrition group (LN, n = 12) receiving Fresubin during the entire study; (3) liquid nutrition juvenile group (LNJ, n = 12) receiving Fresubin until the 90th day of age, then transferred to pelleted chow for the rest of the study; and (4) liquid nutrition adult group (LNA, n = 12) receiving pelleted chow until the 90th day of age and then transferred to Fresubin for the rest of the study (Fig. 1). All experimental groups were provided with Fresubin or pelleted chow (as appropriate) and water ad libitum. Body weight, food, and water intake were determined three times per week throughout the study.
A schematic illustration of the experimental design. At the age of 21 days, pups were weaned and separated into a control group (CON) fed by pelleted chow for the entire study, b liquid nutrition group (LN) fed 5 months by Fresubin for the entire study, c liquid nutrition juvenile group (LNJ) fed 70 days by Fresubin and then 60 days by pelleted food, and d liquid nutrition adult group (LNA) fed 70 days by pelleted chow and then 60 days by Fresubin. At the age of 2 and 4 months, an intra-peritoneal glucose tolerance test was performed. At the end of the study, rats were decapitated and blood and adipose tissues were removed for further biochemical analyses
The composition of the diets was as follows: (a) for the standard pelleted chow diet: 11.21 ml of water and 88.79 g of dry substance with 23.04 g of protein, 2.72 g of fat, and 8.49 g of carbohydrate in 100 g, caloric density 1329 kJ/100 g dry substance with 33 % of calories provided as protein, 13 % as lipid, and 9 % as carbohydrate; (b) for liquid nutrition Fresubin: 84 ml of water and 23.9 g of dry substance with 3.8 g of protein, 3.4 g of fat and 13.8 g of carbohydrate in 100 ml, caloric density 1757 kJ/100 g dry substance with 15 % calories provided as protein, 30 % as lipid, and 55 % as carbohydrate (for details, see [53], or http://www.fresenius-kabi.co.uk/4824_4889.htm).
Intra-peritoneal glucose tolerance test
Intra-peritoneal glucose tolerance test (IPGTT) was performed in conscious animals at the age of 2 and 4 months (Fig. 1). Food was withdrawn at 6:00 p.m. on the day before the test (i.e., 14 h before the procedure). Blood samples (0.5 ∼ 0.8 mL) were obtained from the tip of the tail, and blood glucose levels were immediately determined using a glucose reagent strip (One Touch Ultra, LifeScan, USA) and a standard automated glucometer (Accu-Check active, Roche Diagnostics, USA). After baseline blood glucose measurements, animals received an intra-peritoneal injection of 2.0 g glucose/kg body weight (30 % glucose solution in saline). Blood samples (∼0.2 mL) were then collected for measurement of blood glucose concentrations 15, 30, 60, 90, and 120 min after glucose administration. Glucose tolerance was assessed as the area under the glycemic curve (glucose AUC).
Remaining blood samples were kept for 30 min at room temperature and then centrifuged for 20 min at 3000×g at 4 °C. Obtained serum was stored at −80 °C until analysis of leptin, adiponectin, insulin, and C-peptide concentrations by radioimmunoassay.
Blood serum assays
The blood serum acquired during the IPGTT in the age of 2 and 4 months was used for the assessments of following parameters by RIA kits: Rat Leptin RIA kit (Millipore), Rat Adiponectin RIA kit (Millipore), Rat Insulin RIA kit (Millipore), and Rat C-Peptide RIA kit (Millipore). Assays were performed according to the manufacturer’s instructions, and the intra- and inter-assay variations were below 10 %. Intra- and inter-assay coefficients of variations for measurements of leptin and adiponectin were 3.27 and 4.8 %, respectively, for the former, and 4.09 and 7.31 % for the later. In the case of insulin assessment, the variations were 2.86 and 9 %. The coefficients of variation for C-peptide were less than 10 % for both intra- and inter-assay variations.
Adipose tissue collection and gene expression analysis
At the end of experiment, all rats were killed by decapitation. Mesenteric and epididymal adipose tissue were rapidly removed, weighed, immediately frozen in liquid nitrogen, and then stored at −80 °C until RNA extraction. Total RNA was obtained using TRI REAGENT® (Molecular Research Center, Inc.) following the manufacturer’s protocol. Complementary DNA (cDNA) was synthesized from 1 μg of total RNA using the RevertAid H minus First-Strand cDNA Synthesis Kit (Thermo Fisher Scientific). Semi-quantitative real-time PCR was set up in a total volume of 25 μL containing 30 ng of template cDNA mixed with 12.5 μL of FastStart Universal SYBR Green Master Rox (Roche Diagnostics), 1 μL of specific primer pair set (sequences of used primers are shown in Table 1), and water. Each sample was amplified on a ABI7900HT Fast real-time PCR instrument (Applied Biosystems) under the following conditions: 1 cycle of 2 min at 50 °C, followed by 1 cycle of 10 min at 95 °C, and then 40 cycles of 95 °C for 15 s and 60 °C for 1 min. Data were normalized to glyceraldehyde-3-phosphate dehydrogenase (Gapdh) and/or TATA box binding protein (Tbp) levels and expressed as the relative fold change, calculated using the ΔΔCt method [49]. A melting curve analysis was performed to confirm the specificity of the amplified products.
Preparation of adipocytes and evaluation of their size
Adipocytes were isolated by collagenase digestion from epididymal adipose tissue obtained after decapitation. The tissue was minced in M199 medium (Gibco, Life Technologies) supplemented with 0.5 % bovine serum albumin (BSA, Sigma, St. Louis, MO, USA), 3 mM CaCl2, and 2 mg mL−1 collagenase II (Sigma). After a 30-min collagenase digestion at 37 °C, the digested tissue was centrifuged for 1 min 100×g at 25 °C and the stromal-vascular fraction was removed. Floating adipocytes were washed twice in M199 medium supplemented with 0.5 % BSA and 3 mM CaCl2 by centrifugation at 100×g for 1 min at 25 °C, then filtered through 200-μm nylon mesh and finally centrifuged at 100×g for 1 min at 25 °C. The cell suspension was placed in a Bürker cell chamber and examined by light microscopy (for details, see [76]) using a Leica DMLS microscope equipped with a Power Shot S40 (Canon, Japan). At least ten random visual fields were photographed for every rat adipocyte suspension. The diameter of the cells was measured from the image of their planar surface. At least 100 cells from each adipocyte suspension were evaluated.
Statistical analysis
All statistical analyses were performed using GraphPad Prism program version 5.02 (GraphPad Software). Statistical analysis was performed by one-way ANOVA followed by Bonferroni’s post hoc test to determine significant differences in adipose tissue mass, adipocyte diameter, and messenger RNA (mRNA) levels of leptin, adiponectin, Cd68, Nfkb, Glut4, Pparg, Fabp4, and Mcp1. Significant differences in body weight gain, serum leptin, adiponectin, insulin, C-peptide levels, and the results of the IPGTT were determined by two-way ANOVA using factors of time and diet followed by Bonferroni’s post hoc test. The results are expressed as means ± SEM and represent an average of 7–12 animals. P < 0.05 was taken as indicative of statistical significance for the tests.
Results
Body weight, fat mass, and adipocyte size
The body weight of rats was monitored throughout the experiment. At the age of 2 months (5 weeks after beginning on Fresubin diet), the liquid nutrition-fed rats (LN) had significantly lower body weight than the pelleted chow-fed LNA rats (P < 0.05) and a tendency toward lower body weight was found also in the Fresubin fed LNJ rats (P > 0.05).
Furthermore, the body weight of LN rats increased over time and was significantly higher than the body weight of chow-fed CON and LNJ rats (P < 0.001) at the age of 4 months (14 weeks after the beginning of Fresubin consumption). Similar differences were also found at the age of 4 months in the LNA group, which was switched from chow to Fresubin for 1 month at the age of 90 days (P < 0.001). This condition persisted till the end of the experiment at the age of 5 months (LN vs. CON P < 0.01; LN vs. LNJ P < 0.001; LNA vs. CON, LNJ P < 0.001; Fig. 2a).
Body weight at the age of 2, 4, and 5 months (a), absolute mass of white (mesenteric and epididymal) adipose tissue at the age of 2, 4, and 5 months (b), relative mass of white (mesenteric and epididymal) adipose tissue at the age of 2, 4, and 5 months (c), diameter of adipocyte isolated from epididymal adipose tissue (d), and representative photographs of adipocytes (e) isolated from epididymal adipose tissue of rats fed by pelleted chow (CON), liquid nutrition (LN), liquid nutrition in juvenility (LNJ), or liquid nutrition in adulthood (LNA). Each value is displayed as mean ± SEM (n = 12 for each group). Statistical significance between groups (Bonferroni post-tests) CON vs. LN: **P < 0.01, ***P < 0.001; CON vs. LNA: ††† P < 0.001; LN vs. LNJ: +++ P < 0.001; LNA vs. LNJ: ### P < 0.001; LN vs. LNA: Δ P < 0.05
As we described in our previous study, at the time of Fresubin consumption, all rats had significantly increased energy intake, as well as carbohydrate and lipid intake (P < 0.001). In contrast, due to a relatively low protein content of Fresubin (approximately 15 % compared to 33 % in pellet chow), significantly decreased protein intake at the time of Fresubin intake was observed in rats fed with liquid nutrition in comparison with the CON rats fed with chow diet (P < 0.001). For details, see [53].
At the end of the experiment, the amount of mesenteric and epididymal adipose tissue was significantly higher in LN and LNA rats compared to the chow-fed CON and LNJ rats (P < 0.001; Fig. 2b, c). Moreover, intake of liquid nutrition resulted in a statistically significant increase in adipocyte diameter in epididymal adipose tissue of LN (P < 0.001) and LNA (P < 0.001) rats compared to the CON and LNJ groups (Fig. 2d, e).
Intra-peritoneal glucose tolerance test
At the age of 2 months, no significant differences in fasting plasma glucose concentrations were observed between the groups. However, in the LN and LNJ rats, we found a tendency to have a higher area under the glycemic curve (glucose AUC) suggesting reduced tolerance to intra-peritoneal glucose load compared to CON and LNA groups (P < 0.0001, r = 0.8904; Fig. 3a, c). We also found a significantly higher rise in glucose concentrations in the LN and LNJ compared to CON and LNA rats only during the 15-min interval after the intra-peritoneal glucose load (LN vs. CON P < 0.05; LN vs. LNA P < 0.001; LNJ vs. LNA P < 0.01; Fig. 3a).
Response of plasma glucose levels to intra-peritoneal glucose tolerance test at the age of 2 months (a), at the age of 4 months (b), and glucose area under the curve (AUC; mmol min/L) at the age of 2 and 4 months of rats fed with pelleted chow (CON), liquid nutrition (LN), liquid nutrition in juvenility (LNJ), or liquid nutrition in adulthood (LNA). Each value is displayed as mean ± SEM (n = 12 for each group). Statistical significance between groups (Bonferroni post-tests) CON vs. LN: *P < 0.05, **P < 0.01, ***P < 0.001; CON vs. LNA: † P < 0.05, †† P < 0.01, ††† P < 0.001; LN vs. LNJ: ++ P < 0.01; LNA vs. LNJ: ## P < 0.01; LN vs. LNA: ΔΔΔ P < 0.001
Also, at the age of 4 months, there was no significance between group differences in fasting plasma glucose concentrations. However, after administration of the intra-peritoneal glucose load, LN rats showed significantly increased glucose concentrations from 15 to 90 min during the IPGTT compared to CON (Fig. 3b). Similarly, the LNA group had increased glucose concentrations during the whole 2-h test compared to CON (Fig. 3b). Compared to the LNJ group, significant differences were found only at the 15-min interval (LN vs. LNJ P < 0.01; LNA vs. LNJ P < 0.05; Fig. 3b). Furthermore, both Fresubin-fed groups (LN, LNA) had a significantly higher area under the glycemic curve compared to CON rats as revealed by two-way ANOVA (P < 0.01; Fig. 3c).
Hormonal status
At the age of 2 months, the Fresubin-fed LN and LNJ rats showed lower body weight despite significantly elevated serum levels of leptin (LN vs. CON P < 0.05; LN vs. LNA P < 0.01; LNJ vs. CON, LNA P < 0.001) and adiponectin (LN vs. CON P < 0.001; LN vs. LNA P < 0.01; LNJ vs. CON, LNA P < 0.001) compared to the chow-fed CON and LNA groups (Fig. 4a, b). Fasting serum insulin and C-peptide levels did not differ between the groups (Fig. 4c, d).
Serum leptin (a), adiponectin (b), insulin (c), and C-peptide (d) concentrations at the age of 2 and 4 months in rats fed by pelleted chow (CON), liquid nutrition (LN), liquid nutrition in juvenility (LNJ), or liquid nutrition in adulthood (LNA). Each value is displayed as mean ± SEM (n = 7–10 for each group). Statistical significance between groups (Bonferroni post-tests) CON vs. LN: *P < 0.05, **P < 0.01, ***P < 0.001; CON vs. LNA: ††† P < 0.001; LN vs. LNJ: ++ P < 0.01, +++ P < 0.001; LNA vs. LNJ: # P < 0.05, ## P < 0.01, ### P < 0.001; LN vs. LNA: ΔΔ P < 0.01; LNJ vs. CON: ‡‡‡ P < 0.001
At the age of 4 months, significantly increased body weigh in LN rats was accompanied by higher serum leptin (LN vs. CON, LNJ P < 0.001), adiponectin (LN vs. CON, LNJ P < 0.0001), insulin (LN vs. CON P < 0.05; LN vs. LNJ P < 0.01), and C-peptide levels (LN vs. CON P < 0.01; LN vs. LNJ P < 0.001) compared to the chow-fed CON and LNJ rats. Similar differences were found in Fresubin-fed LNA rats, which showed significantly increased leptin (LNA vs. CON, LNJ P < 0.001), adiponectin (LNA vs. CON, LNJ P < 0.001), insulin (LN vs. LNJ P < 0.05), and C-peptide levels (LN vs. LNJ P < 0.01) compared to chow-fed CON and LNJ groups (Fig. 4a–d).
When comparing values obtained at the age of 2 and 4 months, the diet switch for the LNJ group (from Fresubin to chow) resulted in a decrease of 13.3 % in leptin, 41 % in adiponectin, and 29.1 % in insulin, along with a 10.5 % increase in C-peptide levels. On the other hand, continual intake of Fresubin in the LN group caused an increase of 287 % in leptin, 9.7 % in adiponectin, 281 % in insulin, and 152 % in C-peptide levels. Similarly, the diet switch (from chow to Fresubin) in the LNA group resulted in an increase of 453 % in leptin, 55 % in adiponectin, 136 % in insulin, and 77 % in C-peptide levels.
Gene expression in adipose tissues
The Fresubin-fed LN rats showed significantly increased gene expression of leptin, adiponectin, Cd68, Nfkb, and Mcp1 genes in mesenteric adipose tissue, compared to chow-fed CON and LNJ rats (Fig. 5a–e). In the LNA group, gene expression of leptin, adiponectin, Cd68, and Nfkb were also significantly increased (Fig. 5a–c), whereas Mcp1 mRNA levels showed only a tendency to be increased (Fig. 5e).
Gene expression of leptin (a) and adiponectin (b), cluster of differentiation 68 (Cd68; c), nuclear factor kappa B (Nfkb; d), and monocyte chemotactic protein 1 (Mcp1; e) in mesenteric adipose tissue of rats fed by pelleted chow (CON), liquid nutrition (LN), liquid nutrition in juvenility (LNJ), or liquid nutrition in adulthood (LNA). Each value is displayed as mean ± SEM (n = 7–10 for each group). Statistical significance between groups (Bonferroni post-tests) CON vs. LN: **P < 0.01, ***P < 0.001; CON vs. LNA: † P < 0.05, ††† P < 0.001; LN vs. LNJ: ++ P < 0.01, +++ P < 0.001; LNA vs. LNJ: # P < 0.05, ## P < 0.01, ### P < 0.001
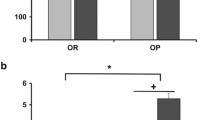
A tendency toward an increased expression of leptin mRNA and a decreased expression of Glut4 mRNA was found in epididymal adipose tissue in the LN and LNA groups (Fig. 6a, c) but it did not reach statistical significance (P > 0.05). Furthermore, only a slight reduction of adiponectin and Pparg mRNA levels was found in LN group (Fig. 6b, d). Significantly increased levels of Fabp4 mRNA were found only in the LNA group compared to the other three experimental groups (P < 0.001; Fig. 6f).
Gene expression of leptin (a), adiponectin (b), glucose transporter 4 (Glut4; c), peroxisome proliferator-activated receptor γ (Pparg; d), and fatty acid binding protein (Fabp4; e) in epididymal adipose tissue of rats fed by pelleted chow (CON), liquid nutrition (LN), liquid nutrition in juvenility (LNJ), or liquid nutrition in adulthood (LNA). Each value is displayed as mean ± SEM (n = 7–10 for each group). Statistical significance between groups (Bonferroni post-tests) CON vs. LNA: ††† P < 0.001; LNA vs. LNJ: ### P < 0.001; LNA vs. LN: ΔΔΔ P < 0.001
Discussion
In the present study, we investigated the long-term effects on metabolism of feeding Wistar rats a liquid diet (Fresubin) by analyzing selected endocrine parameters in the serum as well as by measuring selected morphologic, metabolic, endocrine, and immune parameters in mesenteric and epididymal adipose tissues. Moreover, by including a group fed first by Fresubin and then by chow, we were able to also investigate the reversibility of metabolic alterations induced by the liquid nutrition diet.
We found that long-term consumption of Fresubin led to substantial development of obesity with both increased absolute and relative adipose tissue mass along with altered adipose tissue morphology as demonstrated by increased adipocyte diameter. We also found impaired glucose tolerance, increased serum leptin and adiponectin levels, as well as increased gene expression of leptin, adiponectin, Cd68, Nfkb, and Mcp1 in adipose tissue, indicating development of significant and complex metabolic alterations in response to Fresubin intake.
Fresubin intake alters plasma levels of adipokines
Several studies have shown that the blood concentration of many adipokines, hormones, and acute-phase proteins is altered in human obesity [21]. Furthermore, plasma leptin is elevated, whereas plasma adiponectin is reduced in obese humans and animal models [14, 22, 62, 75]. Here, we showed that Fresubin consumption leads to significant elevation in circulating leptin and adiponectin levels as increased levels of both hormones were detected in all groups of rats during the time duration of Fresubin consumption.
The diet composition, feeding pattern, and type of experimental species might influence plasma leptin concentrations [66]. In the study of Naderali et al., 16 weeks of feeding rats a fat-enriched, glucose-enriched diet resulted in pronounced obesity, signified by a 2-fold increase in fat pad masses and a >3-fold increase in plasma leptin concentrations [57]. Also, in a model of high-fat diet-induced obesity, Kim and Park observed the accumulation of visceral fats along with hyperleptinemia, insulin resistance, and overexpression of the leptin gene in epididymal adipose tissue after 9 weeks of a high-fat diet in male Sprague–Dawley rats [42].
Interestingly, we observed increased leptin concentrations even in the 2-month-old LNJ (99 % higher leptin levels compared to CON) and LN (72 % higher leptin levels compared to CON) rats, which had slightly lower body weight than did the chow-fed CON and LNA rats. It is known that circulating leptin levels reflect the energy and nutritional state of the organism. In a previous study, Archer et al. focused on juvenile diet-induced obesity, using 4-week-old rats fed a solid, high-energy diet and observed an unexpected phenotype of reduced body weight but with increased adiposity. They speculated that ingestion of a high-energy pelleted diet that is energy-dense but with relatively low protein content (15 %) leads to overconsumption so as to meet the demands of growing rats. According to them, when given an appropriate choice, rats select a diet that contains at least 17 % of proteins [3]. Also, Hariri and Thibault pointed out the importance of maintaining the animals’ minimal nutrient requirements, especially for protein, vitamins, and minerals, so as to eliminate the possibility of overconsumption to fulfill these nutrient needs [31]. The Fresubin used in our study has a protein content of 15 %, thus we can hypothesize that the phenotype and body composition of our juvenile rats was the same as in the above-mentioned study of Archers.
Based on results of several studies, it is generally accepted that in obese humans, particularly those with visceral obesity, levels of plasma adiponectin are reduced, and this reduction is greater in men than in women [30, 35, 38, 69]. Several factors may participate in these findings, including the pro-inflammatory factors such as TNF-α, IL-6, as well as hypoxia which suppress the expression of adiponectin in adipocytes, resulting in decreased adiponectin levels in obese and/or diabetic rodents and humans as well as in the obese rhesus monkey model [38, 44, 57]. Despite the aforementioned facts, there are published data showing paradoxical hyperadiponectinemia in states resembling metabolic syndrome, e.g., in states of severe insulin resistance due to genetically defective insulin receptors [72], in patients with Laron syndrome, a growth hormone insensitivity characterized by dwarfism, profound obesity, and hyperlipidemia [40], as well as in the spontaneously hypertensive rat (SHR) characterized by excessive weight, dyslipidemia, glucose intolerance, and insulin resistance [68].
Unexpectedly, our findings also point toward persisting hyperadiponectinemia even in the obese state, as in the 4-month-old obese LN rats (Fresubin consumption for 14 weeks) show 136 % higher adiponectin levels and how our obese LNA rats (Fresubin consumption for 1 month) show 106 % higher adiponectin levels when compared to CON rats. As adiponectin is a unique hormone with anti-diabetic, anti-inflammatory, and anti-atherogenic effects, the observed hypersecretion of adiponectin in the obese hyperinsulinemic Fresubin-fed rats may represent a compensatory response maintaining systemic insulin sensitivity as suggested by Semple et al. [72] and/or it could result from the diet composition itself.
On the basis of their study, Naderali et al. proposed that the lipid profile of the plasma and/or the constituents of the diet consumed by rats might contribute to adiponectin levels more than obesity per se [57]. In their study, Wistar rats were fed either standard laboratory chow or given a fat and glucose-enriched diet (diet-fed) for either 2 days or 16 weeks. After 2 days, total body weight, fat pad masses, and plasma levels of leptin were comparable between the two groups. However, there was a significant decrease in plasma adiponectin levels. After 16 weeks, diet-fed rats had significantly higher body weight, fat pad mass, and plasma levels of leptin and adiponectin compared with chow-fed controls. The authors confirmed the presence of increased expression of the leptin gene in the epididymal fat, but on the other hand, there was significantly decreased expression of adiponectin mRNA. According to the authors, an unexpected higher level of plasma adiponectin in the face of decreased adiponectin mRNA levels in dietary-obese rats suggests the possible existence of post-transcriptional control mechanism(s) for circulating adiponectin levels in obese rats. This may involve decreased metabolism and/or excretion of circulating adiponectin protein under non-physiological conditions such as obesity [57]. Similar conclusions were also deduced in the study of Rodriguez et al. who confirmed hyperadiponectinemia, overexpression of adiponectin in adipose tissue, and increased mRNA levels of adiponectin receptors in skeletal muscle of overweight, hypertensive, hyperglycemic, and hyperinsulinemic SHR rats [68]. The authors suggest that the mechanism responsible for the elevated circulating adiponectin concentrations includes decreased renal adiponectin clearance, or an elevated synthesis in adipose tissue pointing toward the presence of an adiponectin-resistant state. Similarly, recent studies have reported adiponectin resistance as a consequence of impaired adiponectin response due to defective AMP-activated protein kinase (AMPK) signaling in the liver and muscle of high-fat diet-fed rodents [6, 56], and in the skeletal muscle of obese and diabetic subjects [5, 9], which contributes to the development of insulin resistance [68]. To summarize, the increased expression rate of the adiponectin gene and circulating adiponectin concentrations in the liquid nutrition-fed obese, hyperleptinemic and hyperinsulinemic rats probably reflects the consequence of impaired adiponectin functions. Furthermore, it can be hypothesized that hyperadiponectinemia could be a compensatory mechanism preserving proper oxidation of lipids and maintaining insulin sensitivity.
Some dietary factors, such as soy protein, fish oils, and linoleic acid, are suggested to increase plasma adiponectin levels [38]. As Fresubin contains soy protein and mono- and polyunsaturated fatty acids, it could contribute to the increased adiponectin levels, even after obesity onset. Also, Naderali et al. reported that either plasma triacyglycerol and non-esterified fatty acid levels or the composition of the diet might affect adipose tissue, thereby dysregulating adiponectin production and/or its clearance [57].
In this study, we measured mRNA expression of leptin and adiponectin in two types of adipose depots, mesenteric and epididymal. In the mesenteric adipose depots of LN and LNA rats, we found significantly enhanced transcription of both genes compared to the control diet-fed CON and LNJ. These increased transcription rates probably contributed to the elevated circulating plasma leptin and adiponectin levels. We can hypothesize that this increased transcription could be related to enhanced adipocyte differentiation and hypertrophy of adipocytes. In the epididymal depots, no significant differences in leptin and adiponectin expression were found between groups. This is in agreement with other authors showing that as a heterogenous organ, adipose tissue is distributed in different anatomical sites, with different features and functions. This might be associated with a different pattern of expression of genes involved in lipid metabolism [28, 59]. According to Reseland et al., leptin mRNA levels vary in different adipose depots in rodents [66]. Also in their study carried out on the Zucker fatty rat, Krskova et al. [43] reported differences in adiponectin and leptin gene expression in epididymal and retroperitoneal adipose tissue. They assumed that this might be related to the different ratios of hypertrophic to hyperplastic adipocyte content in these two fat depots. Palou et al. carried out a study on 3-month-old rats and characterized the patterns of expression of key genes involved in lipogenesis, lipolysis, and fatty acid oxidation. They found different patterns of expression related to the morphologic and metabolic differences between internal adipose tissue depots [59].
Fresubin intake induced insulin resistance
Several authors have reported elevated basal plasma insulin levels and resistance to the metabolic effects of insulin in obesity [17, 31]. Independent of obesity, high-fat feeding in-and-of-itself contributes to impaired glucose tolerance and insulin resistance, which has been shown in both human and animal studies [31, 67, 78, 79]. Several studies confirmed that a cafeteria diet (high-salt, high-sugar, high-fat, low-fiber, energy-dense, and palatable food) promotes voluntary hyperphagia, which results in rapid weight gain, increased fat pad mass, and pre-diabetic parameters such as glucose and insulin intolerance [12, 33, 54, 70]. In our study, the IPGTT was carried out twice during the experiment, at which time both glycemia and the levels of circulating insulin were assessed. The IPGTT at 2 months revealed no significant differences among the dietary groups. However, in 4-month-old rats, the increased glycemia and AUC levels clearly indicate a progression of impaired glucose tolerance in the Fresubin-fed LN and LNA rats. This could be the result of progressing weight gain, and obesity is accompanied by low-grade inflammation and insulin resistance. Several studies demonstrated that diet-induced obesity (DIO) rats on a high-fat diet are characterized by a decline in glucose tolerance and insulin secretion. They also showed that glucose intolerance in these rats deteriorated with age; however, they never developed frank diabetes [50, 61]. The absence of diabetes was also noted in Wistar rats during long-term fat feeding [15]. Levin and Dunn-Meynel reported elevated insulin levels in DIO rats after either consuming a high-energy diet or a high-energy diet supplemented with the palatable liquid nutrition Ensure for 10 weeks [47]. In a short-term study of Yang et al. in C57BL/6J mice, a high-fat, high-sucrose diet consumed for 2 or 4 weeks caused a significant 2.2- and 1.1-fold increase in plasma insulin levels, respectively, compared to the control group [82]. Our data related to insulinemia showed that at the age of 2 months (5 weeks of Fresubin consumption), no differences in circulating insulin levels were found between the chow-fed and liquid nutrition-fed rats. However, at the age of 4 months, the LN rats (consuming Fresubin for 14 weeks) had 173 % higher plasma insulin levels and the LNA rats (consuming Fresubin for 1 month) had 116 % higher insulin levels than chow-fed control rats. This observed hyperinsulinemia could represent a compensatory mechanism in order to counteract any decreased insulin sensitivity.
We suggest that the simultaneous occurrence of hyperleptinemia, hyperinsulinemia, and impaired glucose tolerance in obese adult LN and LNA rats could be explained by the theories of leptin resistance and dysregulated adipo-insular axis [41]. It is possible that chronically elevated leptin levels led to the development of leptin resistance with the breakdown of leptin signaling in the hypothalamus and pancreatic β cells. This led along with disinhibition of food intake and subsequent hyperphagia, to the dysregulation of the adipo-insular axis and to the failure of leptin’s suppressive effect on insulin secretion, resulting in chronic hyperinsulinemia. Additionally, hyperinsulinemia exacerbates adipogenesis, thereby increasing leptin production. This positive leptin–insulin feedback loop may, according to Kieffer and Habener (2000), be an important factor in the pathogenesis of obesity-associated diabetes mellitus [41].
We have also assessed the circulating levels of C-peptide, which is formed in the biosynthesis of insulin in the pancreatic β cells of Langerhans and released in equimolar amounts to the portal circulation [27, 84]. The levels of C-peptide reflected insulin levels during the assessments at 2 and 4 months. These data are in agreement with the observed impaired glucose tolerance in adult liquid nutrition-fed rats (LN, LNA), as it was shown that patients with insulin resistance and early type 2 diabetes exhibit elevated levels of C-peptide [8]. Altogether, these results show that there are age-dependent differences affecting circulating insulin levels and the progression of glucose intolerance and/or insulin resistance in our model of liquid nutrition-induced obesity in rats.
Fresubin intake induced pro-inflammatory milieu in the adipose tissue
Adipose tissue can expand through adipocyte hypertrophy and/or hyperplasia [31]. During the progression of obesity, adipocyte hypertrophy precedes hyperplasia for the requirement of additional energy storage [32, 65, 76]. Marked increase in adipocyte size in response to Fresubin was observed also in our study. There is evidence that adipocyte hypertrophy is a strong predictor of the adipose tissue macrophage content. However, the mechanisms underlying the potential relationship between adipocyte size and macrophage infiltration seem to be multifactorial [32]. Hypertrophied adipocytes are characterized by higher lipolytic activity [52], which might be the trigger for macrophage infiltration [32]. As stated by Jernas et al., larger adipocytes display an altered adipokine profile toward increased secretion of chemoattractant and immune-related proteins, which could promote macrophage activation and migration into adipose tissue [37]. In our study, significantly higher levels of Cd68, Mcp1, and Nfkb mRNA, the markers of pro-inflammatory M1 macrophages, were found in the mesenteric adipose tissue of rats fed by Fresubin throughout the entire study (19 weeks). In addition, in LN rats we found increased gene expression of Emr-1 (protein expressed on macrophages; data not shown) in fat tissue, indicating macrophage infiltration. In the LNA rats, which consumed Fresubin only during adulthood (for 9 weeks), we found a significant increase in the expression of Cd68 and Nfkb and a trend toward an increase in Mcp1 levels. Therefore, we suppose that in our model of Fresubin-induced obesity, a low-grade inflammation may be present in the hypertrophied adipose tissue; however, the onset (weaning in LN and LNJ group vs. adulthood in LNA group) and duration of Fresubin intake (9 weeks in LNJ/LNA group vs. 19 weeks in LN group) are crucial factors. This is in accordance with the findings of Yu et al. in male C57BL/6 mice fed a high-fat diet for 12 weeks. They examined the expression of chemokines and macrophage markers and found that the expression of Mcp1 and Cd68 mRNA significantly increased in all types of adipose tissue (mesenteric, epididymal, renal, and subcutaneous) of the obese mice compared with non-obese counterparts [85]. Also, Xu et al. reported a dramatic up-regulation of Mcp1 expression in the epididymal fat pad in mice after 16 weeks on a high-fat diet [81]. Similarly, Chen et al. reported an elevated adipose expression of Mcp1 in response to high-fat diet [16]. An increase in the MCP-1 levels in the visceral fat tissue has also been found in obese humans [10]. It is known that leptin activates some pro-inflammatory pathways, including a stimulatory effect on the production of MCP-1 [44]. Therefore, we suggest that the increased leptin expression, as well as circulating leptin levels, might have a stimulatory effect on Mcp1 expression in adipocytes. To examine the role of adipose tissue macrophages in insulin resistance, Di Gregorio et al. examined expression of Cd68 in human adipose tissue and found a significant inverse relation between Cd68 mRNA and insulin sensitivity [19]. Elevated Cd68 mRNA levels found in LN and LNA groups are in accordance with these findings.
Many studies have characterized obesity, metabolic syndrome, and diabetes as a state of metabolically driven low-grade chronic inflammation [23, 24, 64]. Accumulated macrophages are important sources of many cytokines in adipose tissue [19, 23]. Numerous theories have been proposed that may explain macrophage recruitment into adipose tissue in the obese state, including increased adipocyte size and necrosis, local hypoxia, and nutritional endotoxemia [32]. There is also evidence that chronic inflammation promotes the development of insulin resistance and other metabolic disturbances by stimulating NF-κB pathways in adipocytes and liver [29, 34]. Another contributing factor might be the increased levels of free fatty acids (FFA) released from enlarged adipocytes in obesity. It has been demonstrated that saturated fatty acids can act as ligands for toll-like receptor 4 and induce the activation of the NF-κB pathway, which is accompanied by a release of inflammatory cytokines from macrophages [26]. Increased gene expression of Nfkb found in mesenteric adipose tissue of LN and LNA groups support the role of adipose-derived inflammation as a factor contributing to alteration of glucose tolerance in obese individuals.
Fresubin intake alters metabolism in adipose tissue
We also focused on the expression of selected markers of adipogenesis, namely Glut4, Pparg, and Fabp4 in epididymal adipose depot. A slightly reduced expression of the Glut4 and Pparg genes was found in both liquid nutrition-fed groups of rats (LN and LNA), while in the case of Fabp4, we detected a significant up-regulation of gene expression in LNA rats. Our findings concerning Glut4 are in accordance with several studies. For example, a reduction in the GLUT4 content of insulin-sensitive tissues has been reported in several models of genetically [39, 71] or pharmacologically [60] treated obese animals [73]. The same results have been achieved in diet-induced obesity models. High-fat feeding is known to cause insulin resistance and reduction of Glut4 expression in adipose tissue and skeletal muscle [74] and it is dependent on both the composition and initiation of the diet [36]. We can hypothesize that longer Fresubin consumption could have an even more pronounced impact on Glut4 expression while playing a significant role in the physical deterioration associated with obesity by insulin resistance and of course, aging.
PPAR-γ is generally accepted as a master transcriptional regulator of lipid as well as glucose metabolism [7, 83]. Inhibition of PPAR-γ function by inflammatory cytokines such as TNF-α may contribute to pathogenesis of many diseases, such as insulin resistance, atherosclerosis, and inflammation [83]. There is an interesting evidence that the nuclear receptor PPAR-γ might be affected by the composition of fatty acids in the diet, as n-3 and n-6 fatty acids are ligands for PPAR-α and PPAR-γ [18, 66]. However, the existing data are still controversial, as it seems that polyunsaturated fatty acids of the n-6 and n-3 series are not equipotent in promoting adipogenesis in vitro and adipose tissue development in vivo [1]. There are specific differences in the action of n-3 and n-6 fatty acids when applied in different cell lines or different fat depots of the body. According to Muhlhausler et al., polyunsaturated fatty acids (PUFAs) of the n-3 and n-6 classes have the ability to influence the rate of lipid accumulation, while n-3 PUFAs inhibit and n-6 PUFAs promote lipid accumulation [55]. This effect results from modulation of the expression of the key lipogenic transcription factor, sterol regulatory element binding protein 1-c (SREBP1c), which is inversely related to the concentration of n-3 PUFAs, and positively related to n-6 PUFA concentration. Importantly, it was found that fat depots in different anatomical locations have different degrees of responsiveness to altered levels of n-3 and n-6 ratio in the body, with effects being more pronounced in the omental adipose tissue compared to the visceral retroperitoneal depot. Interestingly, they did not find any differences in the expression of Pparg mRNA between the dietary treatments [55]. The activation of the proadipogenic transcription factor, Pparg, and thereby stimulation of adipocyte differentiation/proliferation through n-6 arachidonic acid was also demonstrated by Massiera et al. in their study [51]. Some of the below discussed studies found a reduction of Pparg expression after n-3 administration, and on the contrary, others confirmed increased expression of this gene. Reseland et al. observed a reduction in Pparg expression in cell cultures of the human trophoblast cell line (BeWo) incubated with n-3 polyunsaturated fatty acids (EPA, DHA) that was also accompanied by a reduction in leptin expression [66]. It was also found that n-3 fatty acids suppress PPAR responses in MCF-7 human breast cancer cells, whereas the same n-3 fatty acids stimulate trans-activation of a PPAR response element in HepG2 tumor cells [45]. Also, the previous findings of Al-Hasani and Joost suggest that the n-3 fatty acids act to increase PPAR-γ activity in white adipose tissue, and that this is associated with increased insulin sensitivity [2]. We can hypothesize that the reduction of Pparg mRNA seen in the LN and LNA rats was triggered due to the fatty acid composition of Fresubin, of which saturated fatty acids make up 8.8 %, monounsaturated fatty acids make up 64.7 %, and polyunsaturated fatty acids 26.5 % (members of n-3 represented by α-linolenic acid, eicosapentaenoic acid, docosahexaenoic acid, and one member of n-6 linoleic acid). The ratio of n-6/n-3 in Fresubin was 2.3/1. Some studies indicated that the balance of n-3 and n-6 fatty acids in the diet is most likely a very important factor, as there is the possibility that n-3 fatty acids could act to suppress the adipogenic and lipogenic effects of n-6 fatty acids [1]. Whether this was the case also in our experiment remains questionable, as this issue was not the main objective of the study. Beside the effect of PUFAs, the inhibitory effect of inflammation (increased expression of inflammatory markers MCP-1, CD68, TNF-α, and NF-κB) on Pparg expression and adipocyte differentiation seems more significant.
Fabp4 is expressed in adipocytes and macrophages, and modulates the inflammatory and metabolic response [87]. Expression of Fabp4 is highly induced during adipocyte differentiation and is transcriptionally controlled by PPAR-γ agonists, fatty acids, and insulin. It has been reported that increased circulating FABP4 levels are associated with obesity, insulin resistance, type-2 diabetes, hypertension, cardiac dysfunction, and atherosclerosis [24, 58, 80]. In obese humans, FABP4 levels are significantly increased compared to the lean controls, and serum FABP4 levels are positively correlated with waist circumference, blood pressure, and insulin resistance [80]. Deficiency of FABP4 partially protects mice against the development of insulin resistance associated with genetic or diet-induced obesity [13, 25]. In our study, significantly elevated Fabp4 mRNA levels were found solely in the Fresubin fed LNA rats. We can hypothesize that this increased expression of Fabp4 results from the marked obesity accompanied by the increased fat mass and adipocyte hypertrophy in LNA rats. As the function of FABP4 is to carry the fatty acids from the cytoplasm to the nucleus where they act as PPAR-γ ligands, the increased fatty acid metabolism should be considered significant [43]. Our data indicate that the age at which Fresubin intake started as well as duration of Fresubin intake are crucial factors responsible for observed increase of Fabp4 mRNA levels. However, this issue needs further elucidation. The trend toward “down-regulation” of Fabp4 expression found in the obese LN group could, according to Queipo-Ortuno et al., result from possible adipose tissue dysfunction leading to metabolic disorders [63]. These authors found down-regulation of Fabp4 mRNA in obese patients and speculate that low Fabp4 expression in adipose tissue could lead to lower free fatty acid transport to β-oxidation, resulting in FFA accumulation that may exceed the adipose tissue storage capacity. This excess fat is then transported to non-adipose tissues such as the liver, where the initial response is to facilitate storage in the form of triacylglycerides, but the limited capacity quickly becomes saturated. As lipid excess produces toxic reactive species promoting lipotoxicity [63], high adipose tissue Fabp4 expression may have a protective role, controlling the availability of FFA and their metabolites in the cytoplasm [63, 86].
Conclusions
To the best of our knowledge, this is the first study investigating the metabolic effects of liquid nutrition used as a full replacement for solid, pelleted food in rats. Our long-term study has demonstrated that liquid nutrition Fresubin fed Wistar rats develop marked visceral obesity with adipocyte hypertrophy accompanied by impaired glucose tolerance, hyperleptinemia, hyperinsulinemia, hyperadiponectinemia, increased C-peptide levels, and an altered gene expression profile of visceral adipose tissue marked by up-regulated expression of inflammatory markers (Cd68, Mcp1, Nfkb) and altered expression of selected markers of adipogenesis (Glut4, Pparg, Fabp4) indicating the development of metabolic syndrome. The observed hyperadiponectinemia represents an interesting finding and points toward the possibility of adiponectin resistance in Fresubin-fed obese rats. The attributes of Fresubin, such as palatability, fluidity, macronutrient composition, lower caloric density than the solid chow diet, along with ease of ingestion, digestion, and absorption play an important role in the development of the above-mentioned phenotype and the hyperphagia. Chronic Fresubin feeding may therefore represent a suitable model of metabolic syndrome. Importantly, Fresubin-induced metabolic alterations are reversible as the transition from Fresubin to standard pelleted chow is accompanied by normalization of values of determined factors and metabolic alterations clearly showing a high flexibility of metabolism depending on the type of consumed diet.
References
Ailhaud G, Massiera F, Weill P, Legrand P, Alessandri JM, Guesnet P (2006) Temporal changes in dietary fats: role of n-6 polyunsaturated fatty acids in excessive adipose tissue development and relationship to obesity. Prog Lipid Res 45:203–236
Al-Hasani H, Joost HG (2005) Nutrition-/diet-induced changes in gene expression in white adipose tissue. Best Pract Res Clin Endocrinol Metab 19:589–603
Archer ZA, Corneloup J, Rayner DV, Barrett P, Moar KM, Mercer JG (2007) Solid and liquid obesogenic diets induce obesity and counter-regulatory changes in hypothalamic gene expression in juvenile Sprague–Dawley rats. J Nutr 137:1483–1490
Archer ZA, Mercer JG (2007) Brain responses to obesogenic diets and diet-induced obesity. Proc Nutr Soc 66:124–130
Bandyopadhyay GK, Yu JG, Ofrecio J, Olefsky JM (2006) Increased malonyl-CoA levels in muscle from obese and type 2 diabetic subjects lead to decreased fatty acid oxidation and increased lipogenesis; thiazolidinedione treatment reverses these defects. Diabetes 55:2277–2285
Barnea M, Shamay A, Stark AH, Madar Z (2006) A high-fat diet has a tissue-specific effect on adiponectin and related enzyme expression. Obesity (Silver Spring) 14:2145–2153
Berger J, Moller DE (2002) The mechanisms of action of PPARs. Annu Rev Med 53:409–435
Bhatt MP, Lim YC, Ha KS (2014) C-peptide replacement therapy as an emerging strategy for preventing diabetic vasculopathy. Cardiovasc Res 104:234–244
Bruce CR, Mertz VA, Heigenhauser GJ, Dyck DJ (2005) The stimulatory effect of globular adiponectin on insulin-stimulated glucose uptake and fatty acid oxidation is impaired in skeletal muscle from obese subjects. Diabetes 54:3154–3160
Bruun JM, Lihn AS, Pedersen SB, Richelsen B (2005) Monocyte chemoattractant protein-1 release is higher in visceral than subcutaneous human adipose tissue (AT): implication of macrophages resident in the AT. J Clin Endocrinol Metab 90:2282–2289
Buettner R, Scholmerich J, Bollheimer LC (2007) High-fat diets: modeling the metabolic disorders of human obesity in rodents. Obesity (Silver Spring) 15:798–808
Caimari A, Oliver P, Keijer J, Palou A (2010) Peripheral blood mononuclear cells as a model to study the response of energy homeostasis-related genes to acute changes in feeding conditions. OMICS 14:129–141
Cao H, Maeda K, Gorgun CZ, Kim HJ, Park SY, Shulman GI, Kim JK, Hotamisligil GS (2006) Regulation of metabolic responses by adipocyte/macrophage fatty acid-binding proteins in leptin-deficient mice. Diabetes 55:1915–1922
Clement K, Langin D (2007) Regulation of inflammation-related genes in human adipose tissue. J Intern Med 262:422–430
Chalkley SM, Hettiarachchi M, Chisholm DJ, Kraegen EW (2002) Long-term high-fat feeding leads to severe insulin resistance but not diabetes in Wistar rats. Am J Physiol Endocrinol Metab 282:E1231–E1238
Chen A, Mumick S, Zhang C, Lamb J, Dai H, Weingarth D, Mudgett J, Chen H, MacNeil DJ, Reitman ML, Qian S (2005) Diet induction of monocyte chemoattractant protein-1 and its impact on obesity. Obes Res 13:1311–1320
de Ferranti S, Mozaffarian D (2008) The perfect storm: obesity, adipocyte dysfunction, and metabolic consequences. Clin Chem 54:945–955
Deckelbaum RJ, Worgall TS, Seo T (2006) n-3 fatty acids and gene expression. Am J Clin Nutr 83:1520S–1525S
Di Gregorio GB, Yao-Borengasser A, Rasouli N, Varma V, Lu T, Miles LM, Ranganathan G, Peterson CA, McGehee RE, Kern PA (2005) Expression of CD68 and macrophage chemoattractant protein-1 genes in human adipose and muscle tissues: association with cytokine expression, insulin resistance, and reduction by pioglitazone. Diabetes 54:2305–2313
Eckel RH, Alberti KG, Grundy SM, Zimmet PZ (2010) The metabolic syndrome. Lancet 375:181–183
Fain JN (2010) Release of inflammatory mediators by human adipose tissue is enhanced in obesity and primarily by the nonfat cells: a review. Mediat Inflamm 2010:513948
Ferrante AW Jr (2007) Obesity-induced inflammation: a metabolic dialogue in the language of inflammation. J Intern Med 262:408–414
Furuhashi M, Fucho R, Gorgun CZ, Tuncman G, Cao H, Hotamisligil GS (2008) Adipocyte/macrophage fatty acid-binding proteins contribute to metabolic deterioration through actions in both macrophages and adipocytes in mice. J Clin Invest 118:2640–2650
Furuhashi M, Saitoh S, Shimamoto K, Miura T (2014) Fatty acid-binding protein 4 (FABP4): pathophysiological insights and potent clinical biomarker of metabolic and cardiovascular diseases. Clin Med Insights Cardiol 8:23–33
Furuhashi M, Tuncman G, Gorgun CZ, Makowski L, Atsumi G, Vaillancourt E, Kono K, Babaev VR, Fazio S, Linton MF, Sulsky R, Robl JA, Parker RA, Hotamisligil GS (2007) Treatment of diabetes and atherosclerosis by inhibiting fatty-acid-binding protein aP2. Nature 447:959–965
Galic S, Oakhill JS, Steinberg GR (2010) Adipose tissue as an endocrine organ. Mol Cell Endocrinol 316:129–139
Ghorbani A, Shafiee-Nick R (2015) Pathological consequences of C-peptide deficiency in insulin-dependent diabetes mellitus. World J Diabetes 6:145–150
Giorgino F, Laviola L, Eriksson JW (2005) Regional differences of insulin action in adipose tissue: insights from in vivo and in vitro studies. Acta Physiol Scand 183:13–30
Goran MI, Alderete TL (2012) Targeting adipose tissue inflammation to treat the underlying basis of the metabolic complications of obesity. Nestle Nutr Inst Workshop Ser 73:49–60, discussion p61-46
Greenberg AS, Obin MS (2006) Obesity and the role of adipose tissue in inflammation and metabolism. Am J Clin Nutr 83:461S–465S
Hariri N, Thibault L (2010) High-fat diet-induced obesity in animal models. Nutr Res Rev 23:270–299
Heilbronn LK, Liu B (2014) Do adipose tissue macrophages promote insulin resistance or adipose tissue remodelling in humans? Horm Mol Biol Clin Investig 20:3–13
Heyne A, Kiesselbach C, Sahun I, McDonald J, Gaiffi M, Dierssen M, Wolffgramm J (2009) An animal model of compulsive food-taking behaviour. Addict Biol 14:373–383
Hotamisligil GS (2006) Inflammation and metabolic disorders. Nature 444:860–867
Hotta K, Funahashi T, Bodkin NL, Ortmeyer HK, Arita Y, Hansen BC, Matsuzawa Y (2001) Circulating concentrations of the adipocyte protein adiponectin are decreased in parallel with reduced insulin sensitivity during the progression to type 2 diabetes in rhesus monkeys. Diabetes 50:1126–1133
Im SS, Kwon SK, Kim TH, Kim HI, Ahn YH (2007) Regulation of glucose transporter type 4 isoform gene expression in muscle and adipocytes. IUBMB Life 59:134–145
Jernas M, Palming J, Sjoholm K, Jennische E, Svensson PA, Gabrielsson BG, Levin M, Sjogren A, Rudemo M, Lystig TC, Carlsson B, Carlsson LM, Lonn M (2006) Separation of human adipocytes by size: hypertrophic fat cells display distinct gene expression. FASEB J 20:1540–1542
Kadowaki T, Yamauchi T, Kubota N, Hara K, Ueki K, Tobe K (2006) Adiponectin and adiponectin receptors in insulin resistance, diabetes, and the metabolic syndrome. J Clin Invest 116:1784–1792
Kahn BB, Pedersen O (1992) Tissue-specific regulation of glucose transporters in different forms of obesity. Proc Soc Exp Biol Med 200:214–217
Kanety H, Hemi R, Ginsberg S, Pariente C, Yissachar E, Barhod E, Funahashi T, Laron Z (2009) Total and high molecular weight adiponectin are elevated in patients with Laron syndrome despite marked obesity. Eur J Endocrinol 161:837–844
Kieffer TJ, Habener JF (2000) The adipoinsular axis: effects of leptin on pancreatic beta-cells. Am J Physiol Endocrinol Metab 278:E1–E14
Kim YJ, Park T (2008) Genes are differentially expressed in the epididymal fat of rats rendered obese by a high-fat diet. Nutr Res 28:414–422
Krskova K, Eckertova M, Kukan M, Kuba D, Kebis A, Olszanecki R, Suski M, Gajdosechova L, Zorad S (2012) Aerobic training lasting for 10 weeks elevates the adipose tissue FABP4, Gialpha, and adiponectin expression associated by a reduced protein oxidation. Endocr Regul 46:137–146
Kwon H, Pessin JE (2013) Adipokines mediate inflammation and insulin resistance. Front Endocrinol (Lausanne) 4:71
Lee JY, Hwang DH (2002) Docosahexaenoic acid suppresses the activity of peroxisome proliferator-activated receptors in a colon tumor cell line. Biochem Biophys Res Commun 298:667–674
Levin BE (2005) Factors promoting and ameliorating the development of obesity. Physiol Behav 86:633–639
Levin BE, Dunn-Meynell AA (2002) Defense of body weight depends on dietary composition and palatability in rats with diet-induced obesity. Am J Physiol Regul Integr Comp Physiol 282:R46–R54
Levin BE, Richard D, Michel C, Servatius R (2000) Differential stress responsivity in diet-induced obese and resistant rats. Am J Physiol Regul Integr Comp Physiol 279:R1357–R1364
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(−Delta Delta C(T)) Method. Methods 25:402–408
Madsen AN, Hansen G, Paulsen SJ, Lykkegaard K, Tang-Christensen M, Hansen HS, Levin BE, Larsen PJ, Knudsen LB, Fosgerau K, Vrang N (2010) Long-term characterization of the diet-induced obese and diet-resistant rat model: a polygenetic rat model mimicking the human obesity syndrome. J Endocrinol 206:287–296
Massiera F, Saint-Marc P, Seydoux J, Murata T, Kobayashi T, Narumiya S, Guesnet P, Amri EZ, Negrel R, Ailhaud G (2003) Arachidonic acid and prostacyclin signaling promote adipose tissue development: a human health concern? J Lipid Res 44:271–279
Michaud A, Boulet MM, Veilleux A, Noel S, Paris G, Tchernof A (2014) Abdominal subcutaneous and omental adipocyte morphology and its relation to gene expression, lipolysis and adipocytokine levels in women. Metabolism 63:372–381
Mikuska L, Vrabcova M, Lackovicova L, Ukropec J, Hegedusova N, Slavkovsky P, Hubka P, Mravec B (2013) Long-term liquid nutrition intake and development of obesity: differences between young and adult rats. Endocr Regul 47:85–92
Morris MJ, Chen H, Watts R, Shulkes A, Cameron-Smith D (2008) Brain neuropeptide Y and CCK and peripheral adipokine receptors: temporal response in obesity induced by palatable diet. Int J Obes (Lond) 32:249–258
Muhlhausler BS, Cook-Johnson R, James M, Miljkovic D, Duthoit E, Gibson R (2010) Opposing effects of omega-3 and omega-6 long chain polyunsaturated Fatty acids on the expression of lipogenic genes in omental and retroperitoneal adipose depots in the rat. J Nutr Metab. doi:10.1155/2010/927836
Mullen KL, Smith AC, Junkin KA, Dyck DJ (2007) Globular adiponectin resistance develops independently of impaired insulin-stimulated glucose transport in soleus muscle from high-fat-fed rats. Am J Physiol Endocrinol Metab 293:E83–E90
Naderali EK, Estadella D, Rocha M, Pickavance LC, Fatani S, Denis RG, Williams G (2003) A fat-enriched, glucose-enriched diet markedly attenuates adiponectin mRNA levels in rat epididymal adipose tissue. Clin Sci (Lond) 105:403–408
Ota H, Furuhashi M, Ishimura S, Koyama M, Okazaki Y, Mita T, Fuseya T, Yamashita T, Tanaka M, Yoshida H, Shimamoto K, Miura T (2012) Elevation of fatty acid-binding protein 4 is predisposed by family history of hypertension and contributes to blood pressure elevation. Am J Hypertens 25:1124–1130
Palou M, Priego T, Sanchez J, Rodriguez AM, Palou A, Pico C (2009) Gene expression patterns in visceral and subcutaneous adipose depots in rats are linked to their morphologic features. Cell Physiol Biochem 24:547–556
Papa PC, Seraphim PM, Machado UF (1997) Loss of weight restores GLUT 4 content in insulin-sensitive tissues of monosodium glutamate-treated obese mice. Int J Obes Relat Metab Disord 21:1065–1070
Paulsen SJ, Jelsing J, Madsen AN, Hansen G, Lykkegaard K, Larsen LK, Larsen PJ, Levin BE, Vrang N (2010) Characterization of beta-cell mass and insulin resistance in diet-induced obese and diet-resistant rats. Obesity (Silver Spring) 18:266–273
Pou KM, Massaro JM, Hoffmann U, Vasan RS, Maurovich-Horvat P, Larson MG, Keaney JF Jr, Meigs JB, Lipinska I, Kathiresan S, Murabito JM, O'Donnell CJ, Benjamin EJ, Fox CS (2007) Visceral and subcutaneous adipose tissue volumes are cross-sectionally related to markers of inflammation and oxidative stress: the Framingham Heart Study. Circulation 116:1234–1241
Queipo-Ortuno MI, Escote X, Ceperuelo-Mallafre V, Garrido-Sanchez L, Miranda M, Clemente-Postigo M, Perez-Perez R, Peral B, Cardona F, Fernandez-Real JM, Tinahones FJ, Vendrell J (2012) FABP4 dynamics in obesity: discrepancies in adipose tissue and liver expression regarding circulating plasma levels. PLoS One 7:e48605
Rajala MW, Scherer PE (2003) Minireview: the adipocyte—at the crossroads of energy homeostasis, inflammation, and atherosclerosis. Endocrinology 144:3765–3773
Ravussin E, Smith SR (2002) Increased fat intake, impaired fat oxidation, and failure of fat cell proliferation result in ectopic fat storage, insulin resistance, and type 2 diabetes mellitus. Ann N Y Acad Sci 967:363–378
Reseland JE, Haugen F, Hollung K, Solvoll K, Halvorsen B, Brude IR, Nenseter MS, Christiansen EN, Drevon CA (2001) Reduction of leptin gene expression by dietary polyunsaturated fatty acids. J Lipid Res 42:743–750
Riccardi G, Giacco R, Rivellese AA (2004) Dietary fat, insulin sensitivity and the metabolic syndrome. Clin Nutr 23:447–456
Rodriguez A, Catalan V, Becerril S, Gil MJ, Mugueta C, Gomez-Ambrosi J, Fruhbeck G (2008) Impaired adiponectin-AMPK signalling in insulin-sensitive tissues of hypertensive rats. Life Sci 83:540–549
Ryo M, Nakamura T, Kihara S, Kumada M, Shibazaki S, Takahashi M, Nagai M, Matsuzawa Y, Funahashi T (2004) Adiponectin as a biomarker of the metabolic syndrome. Circ J 68:975–981
Sampey BP, Vanhoose AM, Winfield HM, Freemerman AJ, Muehlbauer MJ, Fueger PT, Newgard CB, Makowski L (2011) Cafeteria diet is a robust model of human metabolic syndrome with liver and adipose inflammation: comparison to high-fat diet. Obesity (Silver Spring) 19:1109–1117
Seino Y, Yamamoto T, Koh G (1992) Insulin and glucose transporter gene expression in obesity and diabetes. Proc Soc Exp Biol Med 200:210–213
Semple RK, Halberg NH, Burling K, Soos MA, Schraw T, Luan J, Cochran EK, Dunger DB, Wareham NJ, Scherer PE, Gorden P, O'Rahilly S (2007) Paradoxical elevation of high-molecular weight adiponectin in acquired extreme insulin resistance due to insulin receptor antibodies. Diabetes 56:1712–1717
Seraphim PM, Nunes MT, Machado UF (2001) GLUT4 protein expression in obese and lean 12-month-old rats: insights from different types of data analysis. Braz J Med Biol Res 34:1353–1362
Sevilla L, Guma A, Enrique-Tarancon G, Mora S, Munoz P, Palacin M, Testar X, Zorzano A (1997) Chronic high-fat feeding and middle-aging reduce in an additive fashion Glut4 expression in skeletal muscle and adipose tissue. Biochem Biophys Res Commun 235:89–93
Trayhurn P, Wood IS (2004) Adipokines: inflammation and the pleiotropic role of white adipose tissue. Br J Nutr 92:347–355
Ukropec J, Penesova A, Skopkova M, Pura M, Vlcek M, Radikova Z, Imrich R, Ukropcova B, Tajtakova M, Koska J, Zorad S, Belan V, Vanuga P, Payer J, Eckel J, Klimes I, Gasperikova D (2008) Adipokine protein expression pattern in growth hormone deficiency predisposes to the increased fat cell size and the whole body metabolic derangements. J Clin Endocrinol Metab 93:2255–2262
Van Heek M, Compton DS, France CF, Tedesco RP, Fawzi AB, Graziano MP, Sybertz EJ, Strader CD, Davis HR Jr (1997) Diet-induced obese mice develop peripheral, but not central, resistance to leptin. J Clin Invest 99:385–390
Woods SC, D'Alessio DA, Tso P, Rushing PA, Clegg DJ, Benoit SC, Gotoh K, Liu M, Seeley RJ (2004) Consumption of a high-fat diet alters the homeostatic regulation of energy balance. Physiol Behav 83:573–578
Woods SC, Seeley RJ, Rushing PA, D'Alessio D, Tso P (2003) A controlled high-fat diet induces an obese syndrome in rats. J Nutr 133:1081–1087
Xu A, Wang Y, Xu JY, Stejskal D, Tam S, Zhang J, Wat NM, Wong WK, Lam KS (2006) Adipocyte fatty acid-binding protein is a plasma biomarker closely associated with obesity and metabolic syndrome. Clin Chem 52:405–413
Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, Sole J, Nichols A, Ross JS, Tartaglia LA, Chen H (2003) Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest 112:1821–1830
Yang ZH, Miyahara H, Takeo J, Katayama M (2012) Diet high in fat and sucrose induces rapid onset of obesity-related metabolic syndrome partly through rapid response of genes involved in lipogenesis, insulin signalling and inflammation in mice. Diabetol Metab Syndr 4:32
Ye J (2008) Regulation of PPARgamma function by TNF-alpha. Biochem Biophys Res Commun 374:405–408
Yosten GL, Maric-Bilkan C, Luppi P, Wahren J (2014) Physiological effects and therapeutic potential of proinsulin C-peptide. Am J Physiol Endocrinol Metab 307:E955–E968
Yu R, Kim CS, Kwon BS, Kawada T (2006) Mesenteric adipose tissue-derived monocyte chemoattractant protein-1 plays a crucial role in adipose tissue macrophage migration and activation in obese mice. Obesity (Silver Spring) 14:1353–1362
Zeyda M, Stulnig TM (2009) Obesity, inflammation, and insulin resistance--a mini-review. Gerontology 55:379–386
Zhang M, Zhu W, Li Y (2014) Small molecule inhibitors of human adipocyte fatty acid binding protein (FABP4). Med Chem 10:339–347
Acknowledgments
This research was supported by European Regional Development Fund Research and Development Grant (ITMS 26240120015). The grant support had no role in the design, analysis, or writing of this article. We wish to thank Dr. Goldstein of ScienceDocs (www.sciencedocs.com/) for the editing of this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interests.
Additional information
Livia Mikuska and Michaela Vrabcova participated equally.
Rights and permissions
About this article
Cite this article
Mikuska, L., Vrabcova, M., Tillinger, A. et al. Chronic liquid nutrition intake induces obesity and considerable but reversible metabolic alterations in Wistar rats. J Physiol Biochem 72, 225–243 (2016). https://doi.org/10.1007/s13105-016-0472-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13105-016-0472-x