Abstract
Introduction
Mandibular reconstruction is often challenging. However, the revolution of computer-assisted design and computer-assisted manufacturing (CAD/CAM), virtual surgical planning (VSP) and 3D printing technology have changed this notion.
Patients and Methods
In this article, we have described six case scenarios where various aspects of VSP and 3D printing technology have been utilized for complex mandibular reconstruction procedures, to provide the patients with the best possible outcome in terms of form, function, and aesthetics.
Discussion
Virtual planning for tumour resection and fibula osteotomies and 3D printing of cutting guides and stereolith models have changed the face of mandibular reconstruction techniques. Increased accuracy, rehabilitation of normal anatomical configuration, appropriate dental rehabilitation, decreased intra-operative time and post-operative complications are some of the advantages. In addition, patient-specific implants eliminate the need for a separate donor site. 3D printed titanium cribs or meshes not only provide robustness, but also incorporates additional features that enable bone graft placement and excellent dental rehabilitation.
Conclusion
These modalities show promising results for reconstruction of complex mandibular defects.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Head and neck surgeons are often faced with the challenge of complex mandibular reconstruction surgeries following resection. Mandibular defects can result from resection of various pathologies such as benign or malignant tumours, from post-traumatic bone damage, or from bisphosphonate or medication-related osteonecrosis of the jaw [1]. Reconstruction modalities have evolved with time, with each technique getting better than the previous in terms of precision, function, and aesthetics. Alloplastic implants, most commonly, mandibular reconstruction plates have been widely used for mandibular rehabilitation for a long time [2]. However, freehand adaptation of the plate can create errors and have an adverse effect on the anatomical outcome. This is more so in case of anterior defects where the upper jaw projection is the only reference available to surgeons for plate adaptation; and this subjective visualization can cause errors [3]. Presently, the vascularized fibula free flap is the gold standard for mandibular reconstruction [4]. These free flaps are ideal for segmented defects where one or more osteotomies are required to reconstruct the mandible or defects that include soft tissue [1]. However, the surgical procedure can be challenging even for the most experienced surgeons.
At the end of the day, our goal is to achieve precise reconstruction of the facial contour and orthognathic planes to ensure optimum function and overall quality of life. With this aim in mind, came the revolution of computer-assisted design and computer-assisted manufacturing (CAD/CAM) technology. This technology has greatly improved the functional and aesthetic outcomes of reconstructive procedures [5]. Virtual surgical planning (VSP) and CAD/CAM are used for virtual reconstruction of mandibular defects and restoration of normal anatomical configuration. This enables development of a patient-specific 3D printed model or prototype which can be used as a template for precise and customized pre-operative bending and adaptation of the reconstruction plate, which in turn reduces errors at the time of surgery [3]. VSP can also be used for the fabrication of cutting guides for precise resection of the mandible during surgery as well as surgical guides for precise harvesting and osteotomy of the free fibular graft for the reconstruction of complex segmented defects [1]. Yet another advancement has been patient-specific implants (PSI) which are patient-matched customized reconstruction plates or prostheses. Its popularity is increasing due to its reported precision and ability to overcome many of the drawbacks of conventional techniques [6]. All these advancements have shown favourable outcomes in enhancing patient aesthetics and function, as well as in saving time during surgery [3]. In this case series, we would like to depict a few such mandibular reconstructive procedures that we performed with the aid of VSP and CAD/CAM. We would like to bring to light the advantages of using these technologies during surgical planning and the relatively precise results obtained thereafter, along with a review of literature.
Case Series
Scenario 1
A 48-year-old female was diagnosed with solid ameloblastoma of the right body of mandible. The plan for definitive management was segmental mandibulectomy with adequate margins. We decided to use VSP to define our resection margins pre-operatively. We used a pull through technique and the virtually planned cutting guides helped us carry out mandibular resection with precise pre-defined margins intra-operatively. It not only made the surgery more predictable, but also saved precious intra-operative time.
The mandibular defect that resulted was a Class IV defect as per Brown’s classification of mandibular defects [7]. It included bilateral canines up to the angle of mandible on the right side. Thus, reconstruction with rehabilitation of precise anatomic configuration was a challenge. We virtually reconstructed the mandibular defect by mirror imaging the intact contralateral mandible. CAD/CAM technology was used to print a customized 3D model of the mandible with normal anatomical contour. We used this model to pre-bend and adapt the titanium reconstruction plate that was used for mandibular reconstruction (Fig. 1). Without having to use freehand adaptation and subjective visualization, intra-operative errors in plate bending were minimized and the patient achieved an accurate anatomical configuration that replicated the unoperated side of her face.
Scenario 2
A 52-year-old female presented with solid ameloblastoma of the left hemi-mandible. Sites for mandibular osteotomies were defined pre-operatively with virtual planning to enable accurate resection. Through a Robson corner splint incision and approach, we carried out left hemi-mandibulectomy with the precise margins. A class IIc Brown’s mandibular defect was obtained. Since the defect was relatively large, we opted for a free fibular reconstruction. Doppler studies were done to study the vessels in the lower limb. Due to financial constraints, fibula cutting guides could not be fabricated. However, VSP was used to reconstruct the defect by mirror imaging the contralateral mandible and a patient-specific stereolithographic model of the mandible with intact anatomical configuration was 3D printed with the help of CAD/CAM. This model was used for pre-operative customized adaptation of the titanium reconstruction plate (Fig. 2). Thus, even though the fibula osteotomies were performed freehand, the precise pre-operative hardware adaptation reduced the margin of error. The surgical results achieved were satisfactory in terms of both form and function.
Scenario 3
Solid ameloblastoma was diagnosed in the right hemi-mandible of a 28-year-old female. Considering the age of the patient, accurate anatomic and functional rehabilitation was of utmost importance. McGregor’s midline lip split incision was placed to carry out hemi-mandibulectomy with the help of prefabricated cutting guides that enabled precise placement of osteotomy cuts. The resultant Brown’s Class IIc defect was planned for vascularized fibular reconstruction. VSP was utilized to accurize the fibular harvest and fibular osteotomies. Fibula cutting guides were virtually fabricated and 3D printed to ensure accurate osteotomies and good bony contact between the segments. The accurately osteotomized fibula was used for precise reconstruction of the complex mandibular defect. The fibula was secured with the help of a titanium reconstruction plate (Fig. 3). The overall result obtained had satisfying aesthetic outcomes with adequate functional and prosthetic rehabilitation.
Scenario 4
A 54-year-old male was diagnosed with solid ameloblastoma of the central mandible. Central segmental mandibulectomy with the help of virtually planned surgical guides was carried out via pull through technique. Free fibular osteocutaneous flap was used to reconstruct the Brown’s Class IV defect that resulted after resection. With the help of VSP and CAD/CAM, fibula cutting guides were fabricated to predefine the osteotomies accurately. In this case, the osteotomies and reconstruction needed to be accurate because it was a large, anterior, segmented defect that required precise contouring and shaping. Thus, the titanium reconstruction plate was pre-bent and adapted on a patient-specific 3D model of the mandible that was mirror imaged to obtain normal anatomical form (Fig. 4). This additional step ensured that there was no error during contouring of the anterior mandibular defect and a highly satisfactory anatomic and functional result was achieved.
Virtual planning of fibula osteotomies for mandibular reconstruction followed by 3D printing of cutting guides for mandibular resection and fibula osteotomy; 3D printing of reconstructed mandible for pre-bending of the reconstruction plate; osteotomized osteocutaneous fibula graft secured to pre-bent reconstruction plate (exact replication of virtual planning can be appreciated); fibula fixed to native mandible
Scenario 5
A 42-year-old male presented with solid ameloblastoma of the left body of mandible. Virtual planning of tumour resection was done, and accurate osteotomies were carried out via a pull through approach. The resultant Brown’s Class IV defect was addressed with a prosthetically driven mandibular reconstruction technique. Three-dimensional virtual models of the patient’s mandible were created to visualize the extent of the defect post-operatively. A custom-made reconstructive titanium milled plate was virtually fabricated to reconstruct the defect. Apart from being patient-specific, this milled plate also had a trough to allow bone graft placement that would permit dental implant rehabilitation. The customized milled plate was 3D printed using CAD/CAM technology and secured to the native mandible using titanium screws (Fig. 5). This accurate reconstructive technique enabled restoration of the native mandibular arch and facial profile, while the provision for dental implant placement enabled functional and prosthetic rehabilitation. The post-operative results achieved were acceptable to both the patient and the surgeons.
Scenario 6
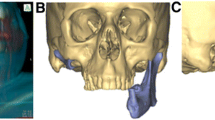
A 22-year-old male was diagnosed with odontogenic keratocyst of the right mandibular body and ramus. Considering the extent of the lesion and underlying muscle involvement, hemi-mandibulectomy with disarticulation was carried out with the help of prefabricated surgical guides. A Roux Trotter lip split approach was used and a Brown’s Class 1c defect resulted after resection. The patient’s age was the primary factor that drove us towards VSP and PSI. Virtual images of the mandibular defect after resection were created. The defect was virtually reconstructed with a patient-matched mandibular body component as well as a fully functional temporomandibular joint component. The titanium body and condylar construct, and ultra-high molecular weight polyethylene (UHMWPE) glenoid fossa component were 3D printed and secured using titanium screws intra-operatively (Fig. 6). Being customized, the intra-operative fit was accurate. This patient-specific approach ensured flawless form and aesthetics due to its excellent contour and superior functional qualities owing to its custom-made design.
Discussion
The mandibular structure is complex due to its contours, angles, change in trabecular patterns and various muscle attachments. All these factors have made reconstruction of mandibular defects challenging for maxillofacial surgeons [8]. At the same time, ablative mandibular defects post resection negatively affects the patient’s well-being and social functioning, apart from affecting aesthetics, speech, mastication, and deglutition. Conventional methods of mandibular reconstruction have included reconstruction plate fixation, rehabilitation with non-vascularized block bone grafts and vascularized free flaps. However, each of them comes with their own set of disadvantages. Reconstruction plates are mainly useful for reconstruction of lateral defects and not those including the condylar component or anterior defects due to the complex contour in these areas [9]. Freehand on-table plate adaptation leads to inability to achieve accurate anatomic contour which further predisposes the native mandible to stress shielding effect and leads to complications such as bone resorption, hardware fracture, hardware exposure, infection and eventually hardware failure [2]. An additional problem is the challenge of prosthodontic rehabilitation. The use of non-vascularized bone grafts is limited to small lateral defects less than 6–7 cm in length. Accurate contouring is difficult for anterior defects, composite defects, and defects involving the condylar unit. There is a limitation in the amount of bone height that can be harvested which makes prosthodontic rehabilitation challenging. There is also a high risk of osteonecrosis if the patient is to be subjected to radiotherapy [10]. Although mandibular reconstruction with free fibula flaps is the gold standard currently, there is a steep learning curve, and the technique remains challenging to most. Subjective visualization and inaccurate osteotomies on the operating table can create contour errors. Second donor site and long operating time resulting in flap ischaemia are other complications [8].
The introduction of VSP, CAD/CAM and 3D printing technology have helped to alleviate the drawbacks related to conventional techniques to a large extent. The combination of precise pre-operative planning and accurate intra-operative execution has resulted in lesser errors, better surgical outcomes and decreased surgical time [8]. Three-dimensional CT-based virtual resection or subtraction of the defect followed by mandibular reconstruction by mirror imaging the contralateral side gives an accurate idea about the extent of the defect, an idea about structures that can be salvaged and those that need to be resected, and finally what the ideal contour of the mandible should be post-operatively [3, 11]. 3D printing the virtually reconstructed mandible gives us stereolith models that can be used for various purposes. Pre-resection 3D models can be used for three-dimensional understanding of the lesion, estimating the intra-operative challenges as well as for educational purposes. The virtually reconstructed mandibles with normal anatomy play a bigger role; they can be used for accurate pre-bending or adaptation of reconstruction plates pre-operatively. These well-contoured reconstruction plates pre-bent on a patient-specific stereolith model have shown to prevent various complications such as mental or gonial over-projection, torque on the condylar head and malocclusion [1, 8]. Further, pre-bending can be done with nearby structures such as inferior alveolar nerve canal, dentition or lower border kept in mind, thereby preventing intra-operative injury to these vital structures [3]. It also reduces intra-operative time and cumbersome on-table plate adaptation based on eyeballing [11].
There are three important aspects of virtual planning for mandibular resection followed by free fibular reconstruction: (a) accurate resection of mandibular defect, (b) precise osteotomy of fibular segments, and (c) placement of fibular segments in the predetermined position [12]. Based on the 3D CT scans, the surgeon can plan the mandibular resection pre-operatively. Cutting guides can be virtually designed based on the planned resection and 3D printed to precisely guide the osteotomy cuts intra-operatively. Further, the 3D scans of the fibula can be virtually cut into the desired pattern to reconstruct the mandibular defect anatomically. The fibular cutting guides thus obtained will have precise angulations to accurately osteotomize the bone to ensure good bone contact between segments. The precisely segmented fibula can then be fixed in their pre-defined positions to the native mandible and reconstruct complex segmented defects [13]. A customized pre-bent reconstruction plate on a 3D model can further augment the results. These features have increased accuracy of reconstruction, reduced operative time and graft ischaemia time, improved ease of use, and enhanced patient satisfaction [4, 14,15,16]. The ideal locations of future dental implants can also be determined enabling superior prosthetic rehabilitation [17]. The use of these technologies in our cases definitely enhanced our surgical outcomes. Restoration of appropriate height, width and projection of the face boosted the patients’ confidence and our encouragement.
Traditional autografts have certain disadvantages such as failure due to poor blood supply, susceptibility to infection, long operative time, two surgical sites, insufficient bone height or width making dental rehabilitation problematic, difficulty in reconstructing the condylar unit and bone resorption with time [15]. PSI is a well-accepted solution to these drawbacks. These implants are virtually designed via a patient-matched compensation for the bone loss based on the symmetry of the contralateral side. Biocompatible materials such as titanium are used to manufacture and print the customized 3D design in a CAD/CAM milling machine. 3D printing is accurate and is specific to the patient three-dimensionally. This ensures meticulous surgical procedure, accurate facial symmetry, and aesthetic results even for geometrically complex defects, less operative time, avoidance of second surgical site, and lesser blood loss [15]. For our patient, along with a titanium body and condylar construct, we also milled a patient-matched polyethylene glenoid fossa component that gave a better result to the patient in terms of aesthetics as well as joint function.
To make mandibular reconstructions more robust, titanium cribs or mesh plates are often used. These implants are designed virtually and custom-made for the patient based on 3D CT images. The advantages of these implants are accurate reconstruction of the lower border, rigidity and robustness of reconstruction, and ability to reinforce the native mandible by placing autologous bone grafts in the trough. The presence of the plate also prevents graft resorption during the healing phase [18]. The porous nature of the mesh allows tissue colonization by ingrowth from surrounding tissues thereby enhancing tissue integration [19]. Ultimately, the adequate height of the prosthesis and bone graft help in ideal dental implant planning. Disadvantages of such prostheses include its high cost and chances of hardware exposure. Our patient who underwent mandibular reconstruction with a patient-specific titanium crib has been on follow-up with no complications so far.
Despite these advancements and precautions, there may still be inevitable intra-operative errors during osteotomies or plate bending. To combat this and make VSP more accurate, 3D images from intra-operative CT scans have been superimposed on pre-operative CT images to allow real-time intra-operative correction of fibula or plate malposition [20]. Similarly, navigation software systems can be used for intra-operative navigation during maxillofacial reconstruction to enhance surgical accuracy and outcomes [21]. Another advancement is the “jaw in a day” concept where free fibula reconstruction with virtually fabricated cutting guides, immediate dental implant placement and complete dental rehabilitation are all carried out in one surgery, in 1 day [22]. Computer tomographic angiography perforator localization technique can be integrated with VSP of osteocutaneous free fibula grafts to precisely and accurately localize perforators intra-operatively [23]. Such advancements are continually paving the way for a brighter future in maxillofacial reconstructive surgery.
Needless to say, accurate mandibular reconstruction using VSP and 3D printing requires meticulous planning. The CT scan of the facial skeleton should be of high resolution and the image slices should be as thin as possible, preferably < 1 mm. If a fibula reconstruction is planned, it is advisable to get a CT angiography of the lower limbs to detect the anatomy of the blood vessels. The 3D file is then extracted from the Digital Imaging and Communications in Medicine (DICOM) data and prepared for VSP in a STL file format which can be readable to a printer. During VSP, the mandibular section with the pathology is identified and resected on workable 3D virtual models. The appropriate fibula is selected and the mandible is reconstructed in segments following the desired curvature of the bone by mirroring the contralateral healthy mandible on a software. In case of anterior mandible or bilateral mandibular defects, digital image library in accordance to the patient’s facial proportions is used to obtain the appropriate mandibular shape and contour [9]. The images of the reconstruction are shared with the operating surgeon, and after confirmation, the designing is completed. The surgical guides are then designed as per the formulated plan. The fibula segments are repositioned back onto the native fibula in the 3D file and the measurements are shared along with images of the guides for re-confirmation. Finally, the items are printed in a CAD/CAM milling machine by a process called slicing, where the model is sliced into layers of predetermined thickness by special slicing software that is characteristic for each 3D printing machine. As these slices are stacked on top of each other, it gives shape and form to the part being printed [24]. Titanium implants are printed such that at least three screw holes are present on either side of the defect and there is a minimum distance of 5 mm between them, between the screw holes and the lower border and between the screw holes and resection margins [9]. Additionally, 3D models of the virtually reconstructed mandible can be printed to help in better understanding of the local anatomy and precise pre-bending of hardware. The printed items are cleaned, polished and their fit is checked prior to dispatch. Documents including invoice, sterilization protocol and details of planning and design are also shared with the surgeon. Thus, thorough planning, meticulous execution and efficient collaboration with the operating surgeon are vital steps required to make these surgeries successful.
As always, every novel invention comes with its own set of limitations. The current printing technologies in use are fused deposition modelling (FDM), stereolithography (SLA), selective laser sintering (SLS), and Polyjet [24]. FDM can be appreciated for its high speed, simplicity, and reasonable cost; however, it is plagued by poor mechanical characteristics and layer-by-layer appearance that produces inferior surface quality [25]. SLA is one of the most widely used 3D printing technologies and was implemented in all our cases. Although it replicates the finer details and allows good surface finish, these models are brittle, discolour over time and are susceptible to heat, moisture and chemicals [24]. Being durable and tough, SLS can be used for functional and production part fabrication. However, this technology is faced with a lack of choice of materials and difficulty in achieving finer details due to the powder sintering process, leaving a rough and porous surface that is difficult to polish and paint24. With Polyjet, it is possible to achieve smooth surfaces with fine details, which can also be painted. Although they provide a wider range of material options, most of the materials lack mechanical properties such as durability and “stepping effect” due to the layered build process [24]. Biomaterials in 3D printing can be broadly grouped as metals, polymers, ceramics and composites. Due to excellent mechanical properties such as strength, ease of fabrication and sterilization, metals are most widely used for fabrication of maxillofacial reconstruction prostheses, as was used by us in the form of titanium. However, they are susceptible to corrosion, aseptic loosening and possess excessive modulus of elasticity. Polymers also have suitable mechanical strength, bur are difficult to sterilize [25]. Our cutting guides were fabricated with polylactic acid (PLA) polymer. While ceramics have high strength, corrosion resistance and biocompatibility, they are difficult to mould and can leach into body fluids. Finally, composites are expensive and have laborious manufacturing processes despite having good mechanical strength and corrosion resistance [25].
Cost is a major factor to consider when it comes to 3D printing technology. It costs to invest in new technology; capital equipment, training and process development can increase the price of the final product, which is a cost that must be borne by the patient. This often becomes a challenge for the patient, especially for those with a lower socio-economic background. However, significant focus is now being placed on developing low-cost printers, which would make this technology more accessible. A few other disadvantages of 3D printing technology are frequent loss of accuracy resulting in intra-operative errors, limited material availability, large machine size, bulk of post-processing procedures, inability to mass produce which slows down production volume, elimination of labour and counterfeits and copyright infringements [8, 15]. For those working in the 3D printing industry, there are also potential hazards, such as breathing in of harmful chemicals especially when the printing material is a powder, skin contact with harmful materials such as metal powders or solvents, and burns from the high temperatures of printers. Dealing with flammable and combustible materials increases the chances of fire and explosion [26]. With efficient tackling of limitations and proper care and precautions in place, VSP and 3D printing technology is truly the present and future of maxillofacial reconstruction.
Conclusion
Computer-assisted surgery, involving pre-operative VSP, intra-operative cutting and reconstruction guides and 3D printing have contributed majorly to surgical practice, especially when it comes to reconstructive procedures. Patient and surgeon satisfaction on obtaining appropriate form, function and aesthetics is the primary driving factor towards constant discovery, advancement, and improvement in this field.
References
Weitz J, Bauer FJ, Hapfelmeier A, Rohleder NH, Wolff KD, Kesting MR (2016) Accuracy of mandibular reconstruction by three-dimensional guided vascularised fibular free flap after segmental mandibulectomy. Br J Oral Maxillofac Surg 54(5):506–510
Zhou L, Wang P, Han H, Li B, Wang H, Wang G, Zhao J, Liu Y, Wu W (2014) Prototyped grafting plate for reconstruction of mandibular defects. J Cranio-Maxillofacial Surg 42(8):1723–1729
Alalawy H, Abdulnabi HA (2022) The use of virtual surgical planning and 3D printing in reconstruction of a mandibular symphesial defect, challenges and gains: a case report. Adv Oral Maxillofacial Surg 5:100235
Bartier S, Mazzaschi O, Benichou L, Sauvaget E (2021) Computer-assisted versus traditional technique in fibular free-flap mandibular reconstruction: a CT symmetry study. Eur Ann Otorhinolaryngol Head Neck Dis 138(1):23–27
Tarsitano A, Ceccariglia F, Bevini M, Breschi L, Felice P, Marchetti C (2023) Prosthetically guided mandibular reconstruction using a fibula free flap: three-dimensional Bologna plate, an alternative to the double-barrel technique. Int J Oral Maxillofac Surg 52(4):436–441. https://doi.org/10.1016/j.ijom.2022.08.006
Li DTS, Leung YY (2023) Patient-specific implants in orthognathic surgery. Oral Maxillofac Surg Clin North Am 35(1):61–69. https://doi.org/10.1016/j.coms.2022.06.004
Brown JS, Barry C, Ho M, Shaw R (2016) A new classification for mandibular defects after oncological resection. Lancet Oncol 17(1):e23-30
Mahendru S, Jain R, Aggarwal A, Aulakh HS, Jain A, Khazanchi RK, Sarin D (2020) CAD-CAM vs conventional technique for mandibular reconstruction with free fibula flap: a comparison of outcomes. Surg Oncol 34:284–291
Bedogni A, Bettini G, Bedogni G, Menapace G, Sandi A, Michelon F, Di Carlo R, Franco P, Saia G (2021) Safety of boneless reconstruction of the mandible with a CAD/CAM designed titanium device: the replica cohort study. Oral Oncol 112:105073
Marechek A, AlShare A, Pack S, Demko C, Quereshy FA, Baur D (2019) Nonvascularized bone grafts for reconstruction of segmental mandibular defects: is length of graft a factor of success? J Oral Maxillofac Surg 77(12):2557–2566
Gil RS, Roig AM, Obispo CA, Morla A, Pagès CM, Perez JL (2015) Surgical planning and microvascular reconstruction of the mandible with a fibular flap using computer-aided design, rapid prototype modelling, and precontoured titanium reconstruction plates: a prospective study. Br J Oral Maxillofac Surg 53(1):49–53
Zhang L, Liu Z, Li B, Yu H, Shen SG, Wang X (2016) Evaluation of computer-assisted mandibular reconstruction with vascularized fibular flap compared to conventional surgery. Oral Surg Oral Med Oral Pathol Oral Radiol 121(2):139–148
Foley BD, Thayer WP, Honeybrook A, McKenna S, Press S (2013) Mandibular reconstruction using computer-aided design and computer-aided manufacturing: an analysis of surgical results. J Oral Maxillofac Surg 71(2):e111–e119
Rodby KA, Turin S, Jacobs RJ, Cruz JF, Hassid VJ, Kolokythas A, Antony AK (2014) Advances in oncologic head and neck reconstruction: systematic review and future considerations of virtual surgical planning and computer aided design/computer aided modeling. J Plast Reconstr Aesthet Surg 67(9):1171–1185
Ismail MB, Darwich K (2022) Reconstruction of large mandibular bone defects extended to the condyle using patient-specific implants based on CAD-CAM technology and 3D printing. Adv Oral Maxillofacial Surg 5:100229
Qaisi M, Zheng W, Al Azzawi T, Murphy J (2022) Patient specific bony and soft-tissue fibular reconstruction: perforator virtual surgical planning technique. Adv Oral Maxillofacial Surg 8:100363
Salinero L, Boczar D, Barrow B, Berman ZP, Diep GK, Trilles J, Howard R, Chaya BF, Rodriguez Colon R, Rodriguez ED (2022) Patient-centred outcomes and dental implant placement in computer-aided free flap mandibular reconstruction: a systematic review and meta-analysis. Br J Oral Maxillofac Surg 60(10):1283–1291. https://doi.org/10.1016/j.bjoms.2022.09.006
Sato H, Tanaka M, Inada T, Yamaguchi K, Katada R, Shirota T (2022) Reconstruction with an individualized titanium mesh cage following wide excision of a mandibular tumor under an intraoperative navigation system: a case series. Oral Maxillofacial Surg Cases 8(2):100258
Qassemyar Q, Assouly N, Temam S, Kolb F (2017) Use of a three-dimensional custom-made porous titanium prosthesis for mandibular body reconstruction. Int J Oral Maxillofac Surg 46(10):1248–1251
Lin CH, Hsu CH, Adarsh K, Hsu CM, Wu CM (2022) Real-time intraoperative computed tomography can accurize virtual surgical planning on the double-barrel fibular flap for mandibular reconstruction. J Plast Reconstr Aesthet Surg 75(8):2702–2705. https://doi.org/10.1016/j.bjps.2022.02.083
Soh HY, Hu LH, Yu Y, Wang T, Zhang WB, Peng X (2022) Navigation-assisted maxillofacial reconstruction: accuracy and predictability. Int J Oral Maxillofac Surg 51(7):874–882
Qaisi M, Kolodney H, Swedenburg G, Chandran R, Caloss R (2016) Fibula jaw in a day: state of the art in maxillofacial reconstruction. J Oral Maxillofac Surg 74(6):1284-e1
Ettinger KS, Morris JM, Alexander AE, Nathan JM, Arce K (2022) Accuracy and precision of the computed tomographic angiography perforator localization technique for virtual surgical planning of composite osteocutaneous fibular free flaps in head and neck reconstruction. J Oral Maxillofac Surg 80(8):1434–1444. https://doi.org/10.1016/j.joms.2022.03.018
Tsioukas V, Pikridas C, Karolos IA (2020) Challenges, opportunities, and limitations in 3D printing. 3D Print Appl Med Surg, pp 151–155.
Eshkalak SK, Ghomi ER, Dai Y, Choudhury D, Ramakrishna S (2020) The role of three-dimensional printing in healthcare and medicine. Mater Des 194:108940
Centers for Disease Control and Prevention. The National Institute for Occupational Safety and Health (NIOSH). https://www.cdc.gov/niosh/index.htm
Acknowledgements
We thank Osteo3DTM for helping us with virtual surgical planning and providing stereolith models. We thank CTARS – (Center for Technology Assisted Reconstructive Surgery) and Zimmer Biomet for printing the Patient Specific Implants.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Surgical procedures and material preparation were performed by AK, JT, GS, and ATK. The first draft of the manuscript was written by MS, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
Institutional Ethics Committee approval was not required for this article.
Informed Consent
Informed consent was obtained from all individual participants included in the article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kudva, A., Thomas, J., Saha, M. et al. Mandibular Reconstruction Modalities Using Virtual Surgical Planning and 3D Printing Technology: A Tertiary Care Centre Experience. J. Maxillofac. Oral Surg. (2024). https://doi.org/10.1007/s12663-024-02112-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12663-024-02112-9