Abstract
Background
Disorders of the temporomandibular joint (TMJ) are frequent and are usually associated with other disorders of the facial skeleton. Surgery might be needed to correct TMJ anatomy and function and, in cases where pathologies coexist, a two-stage corrective surgery might be needed. However, the current fashion of single-stage procedures is feasible with the aid of new technologies such as computer-assisted surgery (CAS). This is a step forward toward performing complex procedures such as a TMJ replacement with simultaneous orthognathic surgery. CAS allows designing patient-fitted prosthesis and more predictable and accurate surgeries. Moreover, intraoperative development can be controlled in real time with intraoperative navigation, and postoperative results can be measured and compared afterwards.
Aims
The primary purpose of this article is to present the protocol used in our institution for orthognathic surgery associated with unilateral and bilateral TMJ replacement with patient-fitted prostheses guided with CAS.
Materials and methods
We present two cases to illustrate our protocol and its results.
Results
In the first case, the difference in millimeters between planning and surgical outcomes was 1.72 mm for the glenoid component and 2.16 mm for the condylar prosthesis; for the second case, differences in the right side were 2.59 mm for the glenoid component and 2.06 mm for the ramus, and in the left side, due to the anatomy the difference was a little greater, without clinical significance
Conclusion
Combined surgery of the midface and mandible with total TMJ replacement is feasible and beneficial for the patient. CAS facilitates the planning and design of custom-fit prosthesis and execution of these procedures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Disorders of the temporomandibular joint (TMJ) are frequent and generally coexist with other abnormalities of the maxillofacial skeleton [1,2,3]. When surgical correction is required, single-stage procedures are feasible and beneficial for patients [1, 4,5,6,7]. Surgical corrective goals may be achieved with adequate planning and surgical execution, preoperative virtual planning (PVP), 3D model printing and intraoperative virtual navigation (IVN) which are useful tools that facilitate treatment of complex disorders. Such tools, generically called “computer-assisted surgery” (CAS); primary endpoint is achieving more predictable and precise postoperative results [8, 9]. They facilitate simple procedures, like removal of a foreign body, as well as complex ones such as those performed for facial trauma, correction of craniomaxillary dysmorphisms, orthognathic surgery, oncological resections or TMJ replacements [10,11,12].
PVP allows to virtually design osteotomies and prostheses, while INV is useful for implementing decisions made during PVP and guiding the surgeon during surgery by providing continuous imaging assessment of the anatomy. Additionally, 3D printing is used to make splints, prostheses and 3D models [11].
The goal of this study is to present the protocol used in our institution for orthognathic surgery associated to unilateral and bilateral TMJ replacement with customized prostheses, performed in a single stage procedure with computer assistance; we present two cases to illustrate this protocol and its results. As secondary aim, we wish to assess the accuracy of the procedure and postoperative clinical course.
Protocol Presentation
In both patients, the general treatment aims were to achieve harmony in the mid- and lower thirds of the face, adequate vertical dimension and facial projection, and general functional rehabilitation, including TMJ (Table 1).
Orthognathic surgery and total TMJ replacement, unilateral and bilateral, were performed in a single surgical stage. Preoperative planning was performed with a 64 slice-high resolution computed tomography (CT) of the craniofacial skeleton and neck, without contrast enhancement (Multislice 64, Aquilion, Toshiba Medical Solutions, Erlangen, Germany); the CT scan protocol includes 1-mm sections, obtained with the patient in occlusion and a wax up model in centric relation to determine the condylar location.
Despite the retrospective nature of this study, it was approved by the hospital’s institutional review board (IRB). We have read and followed the guidelines stated in the Helsinki Declaration when treating these patients and preparing this article. The IRB stated no need of informed consent for the developing of this paper.
Case 1
The patient is a 49-year-old lady with a history of recurred condylar hyperplasia, referred due to progressive occlusion dysfunction and lateral deviation of the mandible. On physical examination, her skeletal class was type I, with a slight occlusion overjet and lateral deviation. Metabolic condylar activity was assessed in three bone SPECT exams at 8-month intervals, which showed a 16% difference between both condyles and a CT of the facial skeleton with a 16.3 × 13.6 mm bone lesion, associated to arthrosis of the TMJ and no condyle excursion with open mouth technique. Orthodontic treatment was implemented for presurgical alignment and leveling of dental arches and subsequently perform a total TMJ replacement associated to a sagittal osteotomy of both ramuses. For orthodontic planning, VTO (visual treatment objective) and 3D images were used (PVP).
The VTO and PVP showed a maxillary canted occlusal plane that limited transverse rotation of the mandible (Fig. 1a); therefore, it was decided to combine the bilateral mandibular osteotomies with a type I Le Fort osteotomy. The surgical objectives were:
-
A 3 mm advancement in the maxilla with a 2 mm impaction in the right side and no impaction in the left side.
-
Bilateral sagittal osteotomy of the mandible for transverse rotation
-
Centralization of the lower midline.
-
Total right-sided TMJ replacement.
The PVP was performed with assistance of the MediCAS Software Virtual Platform.
-
1.
Frontal and lateral photographs of the patient were obtained by the orthodontist in the office, with a natural head position and a marker located in the right side of the image.
-
2.
A 3D reconstruction of the patient’s facial skeleton was performed (skin and bone) and a bite plaster model based on the CT.
-
3.
With the use of specific tools, the position of the head was reoriented in the three spatial axes, matching the frontal and lateral photographs, correcting pitch, yaw and roll. Subsequently, reference lines were traced: a true vertical line, an intercanthal line and a true horizontal line (Fig. 1b).
-
4.
The patient’s bite model was fused with his/her CT (match).
-
5.
A 3D reconstruction of the inferior dental nerve was obtained.
-
6.
A Le Fort I osteotomy and bilateral sagittal ramus osteotomies were virtually performed (Fig. 1b, c). The lower view allowed assessing the left mandibular basal bone.
-
7.
The VTO movements were applied to the 3D model (Fig. 1c).
-
8.
The intermediate and final splints were designed.
-
9.
A patient-fitted TMJ prosthesis was designed and manufactured (Fig. 2a); the glenoid component was made of ultra-high molecular weight polyethylene (UHMWPE), using at least 6 2.0-mm screws for fixation (Fig. 2b, c). The mandibular component was built in titanium, and at least 8, 2.4-mm screws were used for fixation (Fig. 2d).
3D Printing
The splint was printed in photopolymerizable resin (Stratasys Object 30 printer), the biomodels of the upper and lower maxillaries in powder (3D system Pro Jet 360 printer), the prosthetic models (Stratasys F 270 printer) in PLA (polylactic acid), and the final prosthesis in titanium with a high molecular weight polyethylene glenoid component.
Intraoperative Navigation
For the IVN, the navigator used was a Stryker Navigator, Chart II, Freiburg, Germany.
-
1.
Two 3-mm pins were placed in the chin, to position the active navigation pointer using an Ortholock™ fixation system.
-
2.
A correspondence system between the 3D image and the actual patient’s anatomy was employed, with 4 reference points, and the surface was refined with approximately 40 additional points.
-
3.
The PVP was implemented using the navigation pointer to delineate the osteotomy lines, drill the base of the skull and to position the screws in the glenoid and condylar prostheses.
Surgical Procedure
Through lateral preauricular and retromandibular approaches, the TMJ and mandibular ramus were exposed, and the integrity of the VII cranial nerve and its branches was confirmed with neurostimulation.
A Le Fort I osteotomy was performed in the maxilla, with fixation using an intermediate splint, plus bilateral sagittal osteotomy of the mandibular rami and their fixation with three bicortical screws, using the definitive splint.
The patient was placed in intermaxillary fixation (IMF) using the intermediate splint designed with PVP. Primary and surface registrations of the mandible were performed; the pins were located in the chin. The medial pterygoid, masseter and temporal muscles were detached, and coronoidectomy plus condylectomy were performed according to the planning. The TMJ was exposed, and the capsule and articular meniscus were resected. Primary and surface registrations of the glenoid fossa were performed. Drilling of the base of the skull was performed with IVN assistance, avoiding the middle cranial fossa. The prosthesis was positioned and fixation to the zygomatic arch was performed with at least 6, 2.0-mm screws. A third registration stage followed and at least 8, 2.4-mm screws were used to fix the mandibular component. The IMF was removed and the condyle’s position was checked with opening and closure movements of the mandible. Before concluding the procedure, IVN was used to compare intraoperative execution to PVP.
Case 2
A 29-year-old man without a significant medical history was referred because of abnormal occlusion and sleep apnea. On physical examination his skeletal class was type II with an open bite; the centric relationship of condyles cannot be achieved manually with occlusion. A panoramic X-ray and CT of the facial skeleton showed bilateral condylar resorption. A bone SPECT confirmed the diagnosis. A MRI evidenced absence of corticalization in both condyles. His diagnosis was rheumatoid arthritis.
The goals of VTO were:
-
A 9 mm advancement of the upper maxillary
-
An 8 mm superior impaction for correction of gummy smile
-
A 1 mm correction of the superior midline from right to left
-
A 7 mm mandibular autorotation
-
A 10 mm advancement for genioplasty
-
Total bilateral TMJ replacement
In this patient, preoperative planning and intraoperative sequences were similar to those followed in the previous case. The main difference was that this patient required bilateral TMJ replacement, and therefore, a bilateral approach was used. In terms of registration, a skull post replaced the pins.
No immediate complications occurred, and both patients started rehabilitation the first day post surgery; they were discharged on postoperative days 4 and 7 respectively.
Measurement of Accuracy
Measurements were performed overlapping pre- and postoperative CT scans; for all screws implanted, the head center of the position planned was compared to the actual position.
Results
The difference in mm was 1.72 mm for the glenoid component and 2.16 mm for the condylar prosthesis or mandibular component in the first case (Fig. 3). In the second case, differences in the right side were 2.59 for the glenoid component and 2.06 for the ramus, and in the left side due to the anatomy the difference was greater (3.03 mm for the glenoid component and 6.30 mm for the ramus), although not clinically significant (Fig. 4).
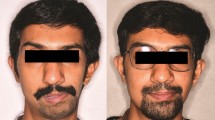
No joint abnormalities were reported in the long-term follow-up (42 months for the first patient and 16 months for the second patient). Both patients objectively recovered mouth opening and occlusion (32 and 30 mm, respectively) and mild lateralization movements improved subjectively (Figs. 5, 6).
Discussion
The prevalence of TMJ dysfunction in the general population may vary, and reports range between 5 and 30% [13]. Several of these disorders have an indication of total TMJ replacement, among them condylar hyperplasia, benign or malignant articular neoplasias, keratocysts, trauma, idiopathic condylar resorption, ankylosis, connective tissue diseases, arthritis, etc. Clinically, they may present or be associated to myofascial pain, otalgia, malocclusion, headaches, sleep apnea, etc. [1, 2, 6, 7].
Joint replacement entails restoring function and consequently, an improvement in patient´s quality of life, allowing them to return to their social activities, with less pain, better mouth opening and easier feeding [14, 15]. Regarding quality of life, Mercuri et al. [16] described an 85% improvement compared to their condition prior to TMJ replacement. Additionally, replacement with alloplastic prostheses prevents morbidity of the donor site and maintains a stable occlusion [15, 16].
Disorders of the TMJ are not isolated, and often coexist with other abnormalities of the facial skeleton; therefore, simultaneous correction of both malformations in a single-stage surgical procedure may prove beneficial for the patient [4,5,6,7]. Nadershah et al. [2] considered that the main indications for concomitant surgery are for patients who failed conservative treatment and patients with advanced TMJ condylar resorption or active TMJ pathologic conditions like condylar hyperplasia, osteochondroma, who require surgical TMJ treatment.
Such complex approach requires an adequate PVP and precise surgical execution. The development of PVP software and assistance with IVN has improved the results in selected craniomaxillofacial surgery, like the ones described above. Many authors have assessed the benefits of using these technologies and agreed that the combination of PVP and IVN delivers more accurate and predictable postoperative results when translating virtual surgery to the operating room [4, 5, 9, 17,18,19]. Besides, the design and development of customized prostheses with the use of these tools improves fitting and osseointegration, thus resulting in less friction and micromovements, better stability and possibly longer mean durability [20]. For the first case presented, the prosthesis was designed and manufactured according to planning, by Biomet ® (Jacksonville, Florida, USA), and for the second case, it was designed at our institution and manufactured by KeyMed Devices ® (Buenos Aires, Argentina). Long-term results have shown adequate fitting with subjective improvement in the quality of life in both patients.
TMJ replacement and orthognathic surgery in a single stage has been well-described [1, 4, 5, 7, 21,22,23,24], but none have reported the use of IVN (Table 2). However, all agree that virtual planning is a valuable contribution to surgical accuracy and predictability. Movahed et al. [4] described their staged protocol and concluded that the use of CAS in this type of procedures shortens the laboratory work previous to surgery (fabrication of prostheses, and for setting the stereolithic models) and surgical times and increases accuracy. Wolford [1], from the same study group, presented posteriorly their experience with similar conclusions; they underscore that single stage surgery may be performed but requires expert surgeons as well as precise and careful diagnosis and planning. Also, they addressed that TMJ should always be treated first. Mohaved et al. [4] also noticed that there are yet some areas to develop, such as the elimination of dental models by using laser scanning, in order to recontour the rami and fossae and to perform accurate maxillary surgical movements using CAS technology. In our patients, PVP was performed with mediCAS planner ® (www.medicas3d.com), estimating the necessary advancements and impactions for the upper maxillary in each patient and defining the location of the inferior dental nerve and its relation with the sagittal ramus osteotomies and the overlaps and gaps between them in the inferior view. The PVP also determined the location and fixation means of prosthetic components. Contrary to Wolford’s approach [1], in our patients the orthognathic surgery was performed prior to TMJ replacement, and we associate IVN for further reliability.
A successful IVN requires an accurate registration; in our experience, similar to other authors, fixed fiducial points are the more stable markers for navigation [12, 17, 19, 25, 26]. We have used bone landmarks for primary and secondary registrations, avoiding soft tissue areas. In the first case, registration was performed three times, relocating the pins each time; in the second case we decided to change the type of navigation pointer to a skull post and the patient was set in IMF; as a result, the registration was made only twice, navigating the maxilla and mandible at the same time. It is worth noticing that registration accuracy is defined by the difference, in millimeters, between the virtual and real coordinate [27], so that the accuracy of optical navigation should be between 0.4 and 1 mm to decrease the margin of error and ensure precision; registration errors can occur but the range of acceptable error is less than 1 mm [25, 27]. Under this statement, we performed the registration on both patients.
The use of IVN allows transferring the surgical plan to the patient [10, 12, 19, 25]. Intraoperatively, it was useful to avoid injuring the base of the skull while drilling the temporal fossa and to perform the osteotomies of the coronoid process and condyle. It was also helpful to drill the mandibular basal bone excess in unilateral condylar hyperplasia and also to correctly positioning and fixating the prosthesis. Additionally, as described in the literature, it allowed confirming, during surgery, the agreement between planning and surgical execution [8, 12, 25].
A postoperative CT scan was used to evaluate the surgical outcomes by comparing and matching the PVP with the post-operative results. According to Levine et al. [8], excellent accuracy is achieved within 1–5 mm. Azarmehr et al. [26], considered a maximum difference of 2 mm between planning and actual results. This difference is accepted in order to call an orthognathic surgery successful (success criterion). In our case, the postoperative outcome had a minimal difference with no functional impairments.
Among the disadvantages of PVP and IVN are the long learning curve (about 30–40 h are required) and their cost [25]. By contrast, prospective studies have shown that, particularly in orthognathic surgery, 3D planning versus the conventional technique decreases duration of the procedure; thus, it is time saving [4, 28]. Therefore, in spite of the learning time required; it will eventually decrease the total procedure time.
In regard to performing both procedures simultaneously, it is worth noting that it prolongs overall intraoperative time, which could eventually be related to infectious complications [29]. Despite this, in our cases, no infections were reported. However, we are aware of this important issue and our aim is to shorten surgical time in the near future.
Conclusion
Complex surgeries of the midface and mandible simultaneously performed with total TMJ replacement are feasible and beneficial for the patient, but their success will depend mainly on an appropriate planning and intraoperative execution. These are complex procedures, usually in the context of a marked distortion of the usual anatomy; hence, the use of PVP, 3D printing and IVN may facilitate their execution.
Availability of Data and Materials
All data are available.
Code Availability
MediCAS Software Virtual Platform.
References
Wolford LM (2016) Computer-assisted surgical simulation for concomitant temporomandibular joint custom-fitted total joint reconstruction and orthognathic surgery. Atlas Oral Maxillofac Surg Clin N Am 24:55–66
Nadershah M, Mehra P (2015) Orthognathic surgery in the presence of temporomandibular dysfunction: what happens next? Oral Maxillofac Surg Clin N Am 27:11–26
Kim S, Keith DA (2018) Combined or staged temporomandibular joint and orthognathic surgery for patients with internal derangement and dentofacial deformities. Oral Maxillofac Surg Clin N Am 30:351–354
Movahed R, Teschke M, Wolford LM (2013) Protocol for concomitant temporomandibular joint custom-fitted total joint reconstruction and orthognathic surgery utilizing computer-assisted surgical simulation. J Oral Maxillofac Surg 71:2123–2129
Gupta RJ, Silva R, Connelly ST (2019) Bilateral temporomandibular joint reconstruction and maxillomandibular advancement for concomitant temporomandibular joint degeneration and obstructive sleep apnea. Atlas Oral Maxillofac Surg Clin N Am 27:43–52
Nale JC (2014) Orthognathic surgery and the temporomandibular joint patient. Oral Maxillofac Surg Clin N Am 26:551–564
Movahed R, Wolford LM (2015) Protocol for concomitant temporomandibular joint custom-fitted total joint reconstruction and orthognathic surgery using computer-assisted surgical simulation. Oral Maxillofac Surg Clin N Am 27:37–45
Levine JP, Patel A, Saadeh PB, Hirsch DL (2012) Computer-aided design and manufacturing in craniomaxillofacial surgery: the new state of the art. J Craniofac Surg 23:288–293
Gateno J, Xia JJ, Teichgraeber JF, Christensen AM, Lemoine JJ, Liebschner MAK et al (2007) Clinical feasibility of computer-aided surgical simulation (CASS) in the treatment of complex cranio-maxillofacial deformities. J Oral Maxillofac Surg 65:728–734
Bell RB (2010) Computer planning and intraoperative navigation in cranio-maxillofacial surgery. Oral Maxillofac Surg Clin N Am 22:135–156
DeLong MR, Gandolfi BM, Barr ML, Datta N, Willson TD, Jarrahy R (2019) Intraoperative image-guided navigation in craniofacial surgery: review and grading of the current literature. J Craniofac Surg 30:465–472
Yu H, Shen SG, Wang X, Zhang L, Zhang S (2013) The indication and application of computer-assisted navigation in oral and maxillofacial surgery-Shanghai’s experience based on 104 cases. J Craniomaxillofac Surg 41:770–774
Proffit WR, Fields HW, Sarver DM (2014) Contemporary orthodontics—e-book. Elsevier Health Sciences, Amsterdam
Kunjur J, Niziol R, Matthews NS (2016) Quality of life: patient-reported outcomes after total replacement of the temporomandibular joint. Br J Oral Maxillofac Surg 54:762–766
Alakailly X, Schwartz D, Alwanni N, Demko C, Altay MA, Kilinc Y et al (2017) Patient-centered quality of life measures after alloplastic temporomandibular joint replacement surgery. Int J Oral Maxillofac Surg 46:204–207
Mercuri LG, Edibam NR, Giobbie-Hurder A (2007) Fourteen-year follow-up of a patient-fitted total temporomandibular joint reconstruction system. J Oral Maxillofac Surg 65:1140–1148
Lin H-H, Chang H-W, Wang C-H, Kim SG, Lo L-J (2015) Three-dimensional computer-assisted orthognathic surgery: experience of 37 patients. Ann Plast Surg 74(Suppl 2):S118–S126
Zinser MJ, Sailer HF, Ritter L, Braumann B, Maegele M, Zöller JE (2013) A paradigm shift in orthognathic surgery? A comparison of navigation, computer-aided designed/computer-aided manufactured splints, and “classic” intermaxillary splints to surgical transfer of virtual orthognathic planning. J Oral Maxillofac Surg 71(2151):e1–21
Lin H-H, Lo L-J (2015) Three-dimensional computer-assisted surgical simulation and intraoperative navigation in orthognathic surgery: a literature review. J Formos Med Assoc 114:300–307
Sidebottom AJ, Gruber E (2013) One-year prospective outcome analysis and complications following total replacement of the temporomandibular joint with the TMJ Concepts system. Br J Oral Maxillofac Surg 51:620–624
Ryu J, Cho J, Kim HM (2016) Bilateral temporomandibular joint replacement using computer-assisted surgical simulation and three-dimensional printing. J Craniofac Surg 27:e450–e452
Cascone P, Vellone V, Ramieri V, Basile E, Tarsitano A, Marchetti C (2018) Reconstruction of the adult hemifacial microsomia patient with temporomandibular joint total joint prosthesis and orthognathic surgery. Case Rep Surg 2018:2968983
Rahman F, Celebi AA, Louis PJ, Kau CH (2019) A comprehensive treatment approach for idiopathic condylar resorption and anterior open bite with 3D virtual surgical planning and self-ligated customized lingual appliance. Am J Orthod Dentofac Orthop 155:560–571
Hills AJ, Ahmed N, Matthews NS (2014) Concurrent bilateral total temporomandibular joint replacement surgery and conventional maxillary osteotomy utilizing virtual surgical planning web-based technology. J Craniofac Surg 25:954–956
Bobek SL (2014) Applications of navigation for orthognathic surgery. Oral Maxillofac Surg Clin N Am 26:587–598
Azarmehr I, Stokbro K, Bell RB, Thygesen T (2017) Surgical navigation: a systematic review of indications, treatments, and outcomes in oral and maxillofacial surgery. J Oral Maxillofac Surg 75:1987–2005
Strong EB, Bradley Strong E, Rafii A, Holhweg-Majert B, Fuller SC, Metzger MC (2008) Comparison of 3 optical navigation systems for computer-aided maxillofacial surgery. Arch Otolaryngol Head Neck Surg. https://doi.org/10.1001/archotol.134.10.1080
Wrzosek MK, Peacock ZS, Laviv A, Goldwaser BR, Ortiz R, Resnick CM et al (2016) Comparison of time required for traditional versus virtual orthognathic surgery treatment planning. Int J Oral Maxillofac Surg 45:1065–1069
Mercuri LG (2012) Avoiding and managing temporomandibular joint total joint replacement surgical site infections. J Oral Maxillofac Surg 70:2280–2289
Acknowledgements
We would like to thank Mr. Axel Mancino, for his invaluable help among the whole process of planning, designing and mainly during intraoperative navigation.
Funding
No fundings were used for the developing of this paper.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. NLG and LB performed material preparation, data collection and analysis. NLG wrote the first draft of the manuscript, and all authors commented on previous versions of the manuscript. ALR contribuition was substantial in terms of odontologic preparation and patients’ follow-up. GN, MF and LR made substantial contribution regarding technical and surgical procedures. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gomez, N.L., Boccalatte, L.A., Lopez Ruiz, Á. et al. Total Temporomandibular Joint Replacement and Simultaneous Orthognathic Surgery Using Computer-Assisted Surgery. J. Maxillofac. Oral Surg. 20, 394–403 (2021). https://doi.org/10.1007/s12663-020-01422-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-020-01422-y