Abstract
Oxaliplatin (OXL) is a third-generation chemotherapeutic agent commonly used to treat metastatic digestive tumors, but one of the main limiting complications of OXL is painful peripheral neuropathy. The present study was to examine the inhibitory effects of blocking microRNA-155 (miR-155) in the dorsal horn of the spinal cord on neuropathic pain induced by OXL in rats and the underlying mechanisms. Behavioral test was performed to examine mechanical pain and cold sensitivity in rats. Real-time RT-PCR and ELISA were employed to determine miR-155 and products of oxidative stress 8-isoprostaglandin F2α (8-iso PGF2α) and 8-hydroxy-2′-deoxyguanosine (8-OHdG) in the dorsal horn. Western blot analysis was used to examine expression of Nrf2-antioxidant response element (Nrf2-ARE), NADPH oxidases (NOXs), and transient receptor potential ankyrin 1 (TRPA1). In results, intrathecal administration of miR-155 inhibitor attenuated mechanical allodynia and cold hyperalgesia in rats with OXL therapy and this was accompanied with restoring of impaired Nrf2-ARE in the dorsal horn. A blockade of miR-155 also attenuated expression of NOX subtype 4 (NOX4) and thereby decreased the levels of 8-iso PGF2α/8-OHdG in the dorsal horn of OXL rats. In addition, inhibiting NOX4 decreased products of oxidative stress in the dorsal horn and attenuated upregulation of TRPA1 induced by OXL. In conclusion, data show the critical role of miR-155 in regulating OXL-induced neuropathic pain likely via oxidative stress–TRPA1 signal pathway, indicating that inhibition of miR-155 has potential benefits in preventing neuropathic pain development during intervention of OXL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the most common and distressing symptoms suffered by patients with progression of cancer is pain (Hanna et al. 2013). Cancer pain predominantly arises from a tumor compressing or infiltrating tissue; from nerve and other changes caused by a hormone imbalance or immune response; and/or from treatments and diagnostic procedures (Hanna et al. 2013; Pasetto et al. 2006). It should be noted that chemotherapy and radiotherapy produce painful conditions that persist long after treatment (Hanna et al. 2013; Hoskin 2008; Portenoy 2011). Therefore, how to effectively manage cancer pain related to these therapies becomes an important issue for treatment and management of cancer patients in clinics.
Oxaliplatin (OXL) is an organoplatinum compound, and as a third-generation chemotherapeutic agent, it is commonly used to treat cancer (Bécouarn et al. 2001). Especially, it has a significant activity against advanced and/or metastatic digestive tumors but one of the main limiting complications of OXL is painful neuropathy (Sereno et al. 2014). The signs of neuropathy start with paresthesia, followed by hyperesthesia (Pasetto et al. 2006). Also, a heightened cold sensitivity is observed in cancer patients with OXL treatment (Sereno et al. 2014). Overall, treatment options for these abnormal sensations have been restricted, partly due to a poor understanding of the underlying mechanisms responsible for neuropathic pain induced by chemotherapeutic OXL.
MicroRNAs (miRNAs) are small noncoding endogenous RNA molecules that repress their target mRNA through complementary binding in the message 3′-UTR (Bartel 2009). miRNAs play important roles in multiple physiological processes such as cell death and survival, cellular response to stress, stem cell division, and pluripotency (Sayed and Abdellatif 2011). miRNAs also contribute to disease processes including cancer, cardiovascular diseases, and neurological disorders (Eacker et al. 2009; Farazi et al. 2011; Han et al. 2011). Due to their small size, relative ease of delivery, and sequence specificity in recognizing their targets, miRNAs are promising therapeutic targets with respect to drug development (Gambari et al. 2011).
Among various miRNAs, miRNA-155 (miR-155) has been particularly reported to play a role in numerous physiological and pathological processes (Calame 2007; Elton et al. 2013; Faraoni et al. 2009; O'Connell et al. 2012). miR-155 is involved in chronic immune response by increasing the proliferative response of T cells through the downregulation of lymphocyte-associated antigens (Sonkoly et al. 2010). In autoimmune disorders such as rheumatoid arthritis, a higher expression of miR-155 is presented in patients’ tissues and synovial fibroblasts (Faraoni et al. 2009). In multiple sclerosis, upregulated expression of miR-155 has been found in peripheral and central nervous system–resident myeloid cells, circulating blood monocytes, and activated microglia (Moore et al. 2013). It has been suggested that miR-155 is implicated in inflammation and overexpression of miR-155 leads to chronic inflammatory state in human (O'Connell et al. 2012).
It is well-known that the inflammatory process is involved in neuropathic pain (Clark et al. 2013; Mika et al. 2013). Proinflammatory cytokines (PICs) are elevated in the peripheral and central nervous system after nerve injury and/or inflammation, leading to mechanical and thermal hypersensitization (Moalem and Tracey 2006). Moreover, increases of PICs in the peripheral and central nervous system have been observed during application of chemotherapeutic agents (such as OXL) and the elevation of PICs is accompanied with amplified oxidative stress (Duan et al. 2018; Kannarkat et al. 2007).
Prior studies have indicated that oxidative stress induced by an imbalance in redox homeostasis is critically involved in the induction of neuropathic pain (Jaggi and Singh 2011; Kallenborn-Gerhardt et al. 2013). Oxidative stress occurs due to overproduction of free radicals, i.e., reactive oxygen species (ROS) such as superoxide anion or hydrogen peroxide together with a failure of antioxidant defense mechanisms (Altenhofer et al. 2012). Intracellular accumulation of ROS and disturbances in the cellular redox state are likely to induce neuronal degeneration and sensitization in pain conditions (Salvemini et al. 2011). Prevention of ROS generation, rather than scavenging already formed free radicals, may represent another possibility to target oxidative stress (Altenhofer et al. 2015). Thus, balancing of ROS by antioxidants or free radical scavengers and inhibition of ROS generation is necessary to play a beneficial role in modulating neuropathic pain conditions. Of note, transient receptor potential ankyrin 1 (TRPA1) plays a functional role in regulating neurogenic inflammation resulting from channel activation to compounds including pungent agents, irritant chemicals, and products of oxidative stress (Andersson et al. 2008; Sawada et al. 2008).
Accordingly, in this study, we targeted miR-155 by using miR-155 inhibitor and further examined its effects on neuropathic pain induced by OXL. Moreover, in order to determine signal mechanisms leading to neuropathic pain via miR-155, we examined if Nrf2-antioxidant response element (Nrf2-ARE) and oxidative stress-TRPA1 signals are engaged in the effects of miR-155. Since NADPH quinone oxidoreductase-1 (NQO1) is regulated by Nrf2, we also determined the levels of NQO1 to assess effectiveness of Nrf2. We speculated that OXL impairs Nrf2-ARE and Nrf2-regulated NQO1 in the dorsal horn of rats. We also speculated that OXL amplifies oxidative NADPH oxidase (subtype NOX4), and this thereby increases 8-isoprostaglandin F2α (8-iso PGF2α, a product of oxidative stress) and 8-hydroxy-2′-deoxyguanosine (8-OHdG, a biomarker of protein oxidation) and upregulates TRPA1 in the dorsal horn. We hypothesized that intrathecal administration of miR-155 inhibitor recovers Nrf2-NQO1 and attenuates NOX4, leading to decreases of 8-iso PGF2α/8-OHdG and TRPA1. This further attenuates mechanical allodynia and cold hyperalgesia in OXL rats. We further hypothesized that blocking NOX4 decreases 8-iso PGF2α/8-OHdG in the dorsal horn of OXL rats and attenuates TRPA1 and thereby improves neuropathic pain.
Methods
Animal
All animal protocols were in accordance with the guidelines of the International Association for the Study of Pain and approved by the Institutional Animal Care and Use Committee of Jilin University. Adult male Sprague-Dawley rats (200–250 g) were housed in individual cages with free access to food and water and were kept in a temperature-controlled room (25 °C) on a 12/12 h light/dark cycle.
A Model of Neuropathic Pain and Administration of Drugs
Rats were anesthetized by intraperitoneal injection (i.p.) of sodium pentobarbital (60 mg/kg) in order to implant intrathecal catheter for administration of drugs. Briefly, one end of polyethylene-10 tubing was inserted intrathecally through an incision in the cisternal membrane and advanced 7–9 cm caudal until the tip of the catheter was positioned at the lumbar spinal level (L5 to L6). The other end of the intrathecal tubing was sutured to the musculature and skin at the incision site and externalized to the back of the rat.
OXL (Tocris Biosci) was dissolved in a 5% glucose solution at a final concentration of 2 mg/mL. Acute neurotoxicity was induced in rats by a single injection (i.p.) of OXL (6 mg/kg), and mechanical and cold hypersensitivity were fully developed 3 days after its injection (Duan et al. 2018). Control rats received the same volume of i.p. injection of glucose vehicle.
After the end of OXL injection, miR-155 inhibitor (5′AAU UAC GAU UAG CAC UAU CCC CA-3′) and its scramble for negative controls (2 μg, Biomics Biotech, Nantong, China) were given by intrathecal injection each day for 5 consecutive days. NOX1/4 inhibitor GKT137831 (2 μg, Cayman Chem) and TRPA1 inhibitor HC030031 (2 μg, Sigma Co.) were given by individual intrathecal injection each day for 5 consecutive days. In each experiment, a Hamilton microsyringe (250 μL) was connected to the intrathecal tubing to make 100 μL of delivery using a syringe pump over 20 min (5 μL/min; Model Elite, Harvard Apparatus Co.).
Behavioral Test
To quantify the mechanical sensitivity of the hindpaw, rats were placed in individual plastic boxes and allowed to acclimate for > 30 min. Mechanical paw withdrawal threshold (PWT) of rat hindpaw in response to the stimulation of von Frey filaments was determined. A series of calibrated von Frey filaments (ranging from 0.4 to 18 g; BioSeb Co., Vitrolles, France; model Bio-VF-M) were applied perpendicularly to the plantar surface of the hindpaw with an appropriate force to bend the filaments until paw withdrew. Note that the filaments were bent for 5–10 s in our protocols and in general, they can be bent sufficiently for ~ 60 s. In the presence of a response, the filament of next lower force was applied. In the absence of a response, the filament of next greater force was applied. To avoid injury during tests, the cutoff strength of the von Frey filament was 18 g. The tactile stimulus producing a 50% likelihood of withdrawal was determined using the “up-down” method (Chaplan et al. 1994). Each trial was repeated 2 times at approximately 2-min intervals. The mean value was used as the force produced a withdrawal response.
To examine cold sensitivity, Thermal Place Preference System (Coulburn Instruments) was used to perform the thermal place preference test in order to assess a cold avoidance behavior. Two connecting metal plates were surrounded by a plastic enclosure. The first plate was kept at neutral temperature (25 °C), and the second plate was kept at cold temperature (12 °C). The test was performed in darkness and each session lasted 3 min. During the session, the rats were left free to explore both plates. The time spent on the cold plate during the entire session was recorded using an infrared camera connected to a computer to determine cold avoidance behavior. Thus, cold sensitivity was expressed as percentage time spent on the cold plate over 3 min (time on cold plate (seconds)/180 s × %). To better control behavior test, the rats were repeatedly placed on the apparatus with both plates held at room temperature (25 °C) during 3 min 2 days before the beginning of the experiment. Note that rats spent an equal amount of time on each plate under these conditions, suggesting that animals showed no place preference. Also, to avoid learning or any place preference unrelated to cold, the temperatures of the plates were inverted between two consecutive sessions. Two trials were performed for each of dosages and data were averaged. Note that the animal experiments were conducted blindly in this report to prevent experimental bias. In all the behavioral tests, the experimenter had no knowledge about the treatments that the rats had received.
Real-time PCR
The lumbar spinal cord (L5 and L6) was removed and the dorsal horn tissues were obtained under an anatomical microscope. The tissues were processed for the extraction of total RNA (RNeasy Mini Kit; Qiagen, CA). RT-PCR was performed using the TaqmanW Universal PCR Master Mix (Applied Biosys). This mix contains AmpliTaq GoldW DNA Polymerase, AmpEraseW UNG, ROX passive reference, buffer, and dNTPs, as well as gene-specific primers for miR-155 gene. In addition, 18 s rRNA (TaqmanW PDAR) was used as an endogenous control to correct for variations in the samples. RT-PCR was performed in duplicate in 96-well plates containing 2 μL of cDNA. The thermal conditions of the cycles were 50 °C for 2 min, 60 °C for 30 min, and 95 °C for 5 min, and this was followed by 40 cycles at 94 °C for 20 s and 62 °C for 60 s. The data were collected in the ABI PRISM SDS 7000 thermal cycler. Relative quantification of target gene expression was performed using the 2-ΔΔCt comparative method, and the threshold cycle value was defined by the point at which there was a statistically significant detectable increase in fluorescence.
ELISA Measurement
The dorsal horn tissues (L5 and L6) were obtained under an anatomical microscope. Total protein was extracted by homogenizing the sample in ice-cold immunoprecipitation assay buffer with protease inhibitor cocktail kit. The lysates were centrifuged, and the supernatants were collected for measurements of protein concentrations using a bicinchoninic acid assay reagent kit. The levels of 8-iso PGF2α and 8-OHdG were examined using an ELISA assay kits (Promega Co. and Abcam Co.) according to the provided description. Briefly, polystyrene 96-well microtitel immunoplates were coated with affinity-purified rabbit primary antibodies. Parallel wells were coated with purified rabbit IgG for evaluation of nonspecific signal. After overnight incubation, plates were washed. Then, the diluted samples and 8-iso PGF2α/8-OHdG standard solutions (100 pg/mL–100 ng/mL) were distributed in each plate. The plates were washed and incubated with anti-8-iso PGF2α/8-OHdG galactosidase. Then, the plates were washed and incubated with substrate solution. After incubation, the optical density was measured at 575 nm using an ELISA reader.
Western Blot Analysis
The dorsal horn tissues (L5 and L6) were removed and total protein was extracted and measured. After being denatured, the supernatant samples containing 20 μg of protein were loaded onto gels and electrically transferred to a polyvinylidene fluoride membrane. The membrane was incubated with respective primary antibodies (at 1:500): rabbit anti-Nrf2 (Cat# ab137550, Abcam), anti-NQO1 (Cat# ab34173, Abcam), anti-NOX1 (Cat# ab131088, Abcam)/anti-NOX2 (Cat# ab31092, Abcam)/anti-NOX3 (Cat# ab93388, Abcam)/anti-NOX4 (Cat# ab154244, Abcam), and anti-TRPA1 (Cat#NB110-40763, Novus Bio). The membranes were washed and incubated with an alkaline phosphatase–conjugated anti-rabbit secondary antibody (1:1000). The immunoreactive proteins were detected by enhanced chemiluminescence. The bands recognized by the primary antibody were visualized by exposure of the membrane onto an x-ray film. The membrane was stripped and incubated with anti-β-actin to show equal loading of the protein. Then, the film was scanned and the optical densities of primary antibodies and β-actin bands were determined using the NIH Scion Image Software. Values for densities of immunoreactive bands/β-actin band from the same lane were determined. Each of the values was then normalized to a control sample.
Statistical Analysis
All data were analyzed using one-way measures analysis of variance. Tukey’s post hoc analyses were used to determine differences between groups. For all analyses, differences were considered significant at P < 0.05. Values were presented as means ± standard error of mean. All statistical analyses were performed by using SPSS for Windows version 13.0 (SPSS Inc.).
Results
The Changes of miR-155 After OXL Intervention
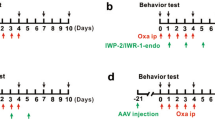
In the present study, a single intraperitoneal injection of OXL was used to induce mechanical and cold hypersensitivity in rats (Fig. 1A) and then, we examined the time course for changes of miR-155 after OXL intervention. Figure 1 B shows a stabilized increase in the levels of miR-155 of the dorsal horn 3–5 days after the beginning of OXL intervention. Based on this result, the time point of day 5 was selected for intrathecal injection miR-155 inhibitor and its scramble, and NOX4 and TRPA1 antagonists for the rest of the experiments.
(A) A schematic diagram showing the schedule giving miR-155 inhibitor, its scrambles, and NOX4 and TRPA1 receptor blockers after administration of OXL (6 mg/kg; a single intraperitoneal injection). miR-155 inhibitor/its scrambles, GKT137831, and HC030031 were administered via intrathecal injection (each day for 5 consecutive days), respectively. (B): showing that the levels of miR-155 expression were increased in the dorsal horn of the spinal cord after administration of OXL and remained at a high level 3 days after OXL. *P < 0.05 vs. its level of pre-injection of OXL (day 0). The number of rats = 6–10 in each group. (C): showing the effectiveness of miR-155 inhibitor. As compared with scramble, administration of miR-155 inhibitor attenuated the levels of miR-155. *P < 0.05 vs. its levels with scramble. The number of rats = 6–8 in each group
In addition, we examine the effectiveness of miR-155 inhibitor used in this study. As compared with scramble, intrathecal administration of miR-155 inhibitor attenuated the levels of miR-155 (Fig. 1C, P < 0.05, inhibitor vs. scramble; n = 6–8 in each group).
Effects of miR-155 Inhibition on Mechanical and Cold Sensitivity
PWT appeared to be less in OXL rats than that in control rats 2–5 days after injection of OXL (Fig. 2A). This figure also demonstrates that PWT was increased 2 days after injection of miR-155 inhibitor in OXL rats, and the effects were observed while miR-155 inhibitor was given for 3–5 days (P < 0.05, OXL rats vs. OXL rats with inhibitor). As compared with miR-155 inhibitor, its scramble did not alter PWT in OXL rats (P > 0.05, OXL rats vs. OXL rats with scramble). In addition, Fig. 2 B shows that OXL injection significantly decreased percentage time spent on the cold plate as compared with controls 2–5 days after OXL. Application of miR-155 inhibitor increased percentage time spent on the cold plate in OXL rats (P < 0.05, OXL rats vs. OXL rats with inhibitor). Likewise, miR-155 inhibitor scramble had no distinct effects on percentage time spent on the cold plate in OXL rats (P > 0.05, OXL rats vs. OXL rats with scramble).
(A) PWT was less in OXL rats than in control rats 2–5 days after its injection. Intrathecal administration of miR-155 inhibitor, but not its scramble, increased PWT in OXL rats 2–5 days after miR-155 inhibitor. (B): showing that time spent on the cold plate was less in OXL rats than in control rats 2–5 days after injection of OXL. miR-155 inhibitor elevated % time spent on the cold plates in OXL rats. mir-155 inhibitor scramble had no effects on % time spent on the cold plates in OXL rats. *P < 0.05, OXL rats vs. control rats. #P < 0.05, OXL rats with inhibitor vs. OXL rats and OXL rats with scramble. The number of rats in each group is also shown
Effects of miR-155 Inhibition on Nrf2-ARE and NOXs
We also examined the protein levels of Nrf2 and Nrf2-regulated NQO1 as well as NOXs in the dorsal horn. Figure 3 A and B show that the protein expression levels of Nrf2 and Nrf2-regulated NQO1 were decreased in the dorsal horn of OXL rats (P < 0.05, OXL rats vs. control rats; n = 8–12 in each group). In contrast, the protein levels of NOX4 in the dorsal horn of OXL rats were upregulated (P < 0.05, OXL rats vs. control rats; n = 8 in each group) as shown in Fig. 3C but no significant differences in NOX1, NOX2, and NOX3 were observed in control rats and OXL rats, i.e., expression of NOX1, NOX2 and NOX3 (normalized to β-actin) was 1.15 ± 0.12, 1.09 ± 0.10, and 1.12 ± 0.13 in the dorsal horn of OXL rats; and 1.01 ± 0.10, 0.97 ± 0.12, and 1.05 ± 0.15 in the dorsal horn of control rats (P > 0.05, OXL vs. control for each NOXs; n = 6–10 in each group). In addition, Fig. 3 A–C demonstrate that miR-155 inhibitor, but not its scramble, improved impairment of Nrf2-NQO1 and attenuated upregulation of NOX4 (P < 0.05, miR-155 inhibitor vs. scramble group; n = 6–12 in each group).
Effects of OXL on antioxidant response and oxidative stress signal pathways. (A and B): protein expression levels of Nrf2 and NQO1. Top panel and bottom panel are representative bands and averaged data: Nrf2 and NQO1 were decreased in the dorsal horn of OXL rats. As miR-155 inhibitor was given via intrathecal injection, impairment of Nrf2-NQO1 was recovered. *P < 0.05, OXL rats vs. control rats and OXL rats with miR-155 inhibitor. Note that miR-155 inhibitor scramble had no effects. n = 8–12 in each group. (C): showing that protein expression levels of NOX4 were amplified by OXL and the increase of NOX4 was attenuated by miR-155 inhibitor. *P < 0.05, OXL rats vs. control rats and OXL rats with inhibitor. n = 6–10 in each group. (D): OXL amplified the levels of oxidative products 8-iso PGF2α and 8-OHdG in the dorsal horn and miR-155 inhibitor attenuated increases of 8-iso PGF2α and 8-OHdG. *P < 0.05, OXL rats (n = 15) vs. control rats (n = 15) and OXL rats with inhibitor (n = 16). No significant differences in 8-iso PGF2α and 8-OHdG were observed in OXL rats and OXL rats with scramble (P > 0.05 between two groups)
Levels of Oxidative Stress Products
We further examined products of oxidative stress in the dorsal horn of OXL rats and control rats as shown in Fig. 3D. This figure demonstrates that 8-iso PGF2α and 8-OHdG were increased in the dorsal horn of OXL rats as compared with control rats (P < 0.05, OXL vs. controls; n = 15 in each group). As miR-155 inhibitor was given by intrathecal injection, increases of 8-iso PGF2α and 8-OHdG were attenuated in OXL rats (n = 16). Note that miR-155 inhibitor scramble had no effects on increases of 8-iso PGF2α/8-OHdG in the dorsal horn of OXL rats (P > 0.05, OXL rats with scramble/n = 10 vs. OXL rats/n = 15).
Effects of Blocking NOX4 and TRPA1 on Mechanical and Cold Sensitivity
In order to determine engagement of oxidative stress–TRPA1 signal pathways in the effects of miR-155, we examined if blocking spinal NOX4 or TRPA1 can attenuate hypersensitivity of mechanical and cold stimulation induced by OXL. Figure 4 A and B show that OXL decreased PWT and decreased percentage time spent on the cold plate 2–5 days after OXL. As GKT137831 or HC030031 was given by intrathecal injection, decreases in PWT and percentage time spent on the cold plate were largely recovered in OXL rats (P < 0.05, OXL rats vs. OXL rats with GKT137831 or HC030031).
Effects of blocking NOX and TRPA1 on mechanical and cold sensitivity. (A): PWT was less in OXL rats than that in control rats 2–5 days after injection of OXL. Intrathecal injection of GKT137831 attenuated decreases of PWT in OXL rats. Likewise, HC030031 also attenuated decreases of PWT evoked by OXL. (B): showing that % time spent on the cold plate was less in OXL rats as compared with control rats 2–5 days after injection of OXL. GKT137831 and HC030031 attenuated the effects of OXL. *P < 0.05, OXL rats vs. control rats; #P < 0.05, OXL rats vs. OXL rats with GKT137831 or HC030031. The number of rats in each group is also shown. (C): OXL amplified the levels of oxidative products 8-iso PGF2α and 8-OHdG in the dorsal horn. As GKT137831 was given via intrathecal injection, increases of 8-iso PGF2α and 8-OHdG were attenuated. *P < 0.05, OXL rats (n = 12) vs. control rats (n = 10) and OXL rats with GKT137831 (n = 12). (D): the protein levels of TRPA1 were amplified in the dorsal horn tissues of OXL rats and intrathecal administration of GKT137831 decreased upregulation of TRPA1 in the dorsal horn of OXL rats. *P < 0.05, OXL rats (n = 12) vs. control rats (n = 8) and OXL rats with GKT137831 (n = 8)
Effects of Blocking NOX on Oxidative Stress Products and TRPA1 Expression
Figure 4 C demonstrates that intrathecal infusion of GKT137831 attenuated increases of both 8-iso PGF2α and 8-OHdG in the dorsal horn in OXL rats (P < 0.05, OXL rats vs. OXL rats with inhibitor; n = 12 in each group). In addition, Fig. 4 D shows that OXL upregulated protein expression of TRPA1 receptors in the dorsal horn and intrathecal administration of GKT137831 significantly attenuated amplification of TRPA1 induced by OXL (P < 0.05, OXL rats/n = 12 vs. OXL rats with inhibitor/n = 8).
Discussion
In general, miRNAs play a fundamental role in cellular biology. They are critical modulators for a wide range of cellular processes including development, differentiation, proliferation, metabolism, and apoptosis (Ambros 2004; Bartel 2004). miRNAs are small ~ 22 nucleotide RNA sequences that regulate the expression of protein-coding mRNA sequences, often targeting numerous proteins within a particular network or pathway. miRNA targeting is achieved when they are guided to the 3′-UTR of mRNA sequences, where partial or exact complementary base pairing of the miRNA results in degradation or translational inhibition of the target mRNA molecules. Each miRNA is anticipated to bind to more than 200 mRNA target sequences, and as a result, overexpression and/or inhibition of a single miRNA can have a wide effect on cellular function (Chekulaeva and Filipowicz 2009; Winter et al. 2009).
Major efforts have focused on understanding how miRNAs are induced in the cell, with an overall aim to reveal their effects on targeted proteins and understanding which miRNAs or panels of miRNAs are dysregulated in disease or under pathophysiological conditions (Ambros 2004; Bartel 2004; Chekulaeva and Filipowicz 2009; Winter et al. 2009). In the similar way, the purpose of our current study was to determine the role played by miR-155 in regulating oxidative insult which induces neuropathic pain during intervention of OXL. Thus, we examined the protein expression of NOX4 and further examined the levels of oxidative products 8-iso PGF2α/8-OHdG in the dorsal horn of OXL rats. Our results demonstrated that NOX4 is likely to be targeted by miR-155 since intrathecal administration of miR-155 inhibitor attenuated the protein levels of NOX4 expression. In addition, Nrf2-ARE is one of targeted signal pathways by miR-155 since we showed that impairment of Nrf2-ARE signal was restored by miR-155 inhibitor. These results are consistent with the findings reported by recent studies, suggesting the effects of miR-155 on oxidative damage through Nrf2 mechanisms in various tissues (Chen et al. 2019; Qiu and Zhang 2018; Yang et al. 2018). Taken together, it is speculated that NOX4 and Nrf2 genes are likely targeted by miR-155 for exaggerating oxidative stress.
The role of oxidative stress in chemotherapy-induced peripheral neuropathy has been studied. As a non-specific ROS scavenger, N-tert-butyl-α-phenylnitrone was reported to inhibit the development of chemotherapy-induced mechanical hypersensitivity (Fidanboylu et al. 2011). In particular, the antioxidant compound silibinin was reported to attenuate the development and maintenance of OXL-induced mechanical and thermal hypersensitivity (Di Cesare Mannelli et al. 2012). In addition, the painful peripheral neuropathy induced by OXL was prevented by the antioxidant effects of flavonoids rutin and quercetin in the dorsal horn (Azevedo et al. 2013). Nonetheless, impairment of mitochondrial and cellular endogenous antioxidant pathways in the peripheral nerves has been observed after diverse chemotherapy including OXL (Waseem et al. 2018). In our current study, we showed that OXL impaired expression of Nrf2-NQO1 in the dorsal horn. Of note, we further demonstrated the effectiveness of intrathecal administration of miR-155 inhibitor and then miR-155 inhibitor improved impairment of this antioxidant signal pathways after OXL intervention and this thereby attenuated mechanical allodynia and cold hyperalgesia.
In addition to antioxidants and/or free radical scavengers, it is interesting to determine the effects of decreasing ROS generation on OXL-induced mechanical and cold hypersensitivity. One source of ROS production is the enzyme family of NOX. The rodent genome encodes four genes that contain the catalytic NOX subunit, namely NOX1, NOX2, NOX3, and NOX4 (Altenhofer et al. 2012). This electron-transferring subunit is constitutively inactive in resting cells and generates ROS only upon activation, e.g., after noxious stimuli (Salvemini et al. 2011). While NOX2 activation is predominantly associated with innate immunity–mediated host defense and NOX1 with blood pressure control and related vascular mechanisms (Gavazzi et al. 2006; Lam et al. 2010), NOX4 was shown highly expressed under stress conditions in the central nervous system (Suzuki et al. 2012). Evidence has also identified activation of NOX4 as a causative factor that contributes to inflammation or neuropathic pain in the nervous system (Kallenborn-Gerhardt et al. 2012). In the current study, we determined levels of NOX1, NOX2, NOX3, and NOX4 in the dorsal horn of OXL rats. We observed that NOX4 was upregulated after injection of OXL. Moreover, intrathecal administration of miR-155 inhibitor attenuated upregulation of NOX4 in the dorsal horn.
It is noted that TRPA1 has a functional role in regulating pain and neurogenic inflammation resulting from channel activation to a variety of compounds (Andersson et al. 2008; Sawada et al. 2008). TRPA1 appears in peripheral and central nervous systems and is engaged in the development of mechanical hypersensitivity and painfully cold temperatures (Kwan et al. 2006; Story et al. 2003). Additional studies further indicate that TRPA1 mediates mechanical and cold hypersensitivity induced by chemotherapeutic agents (Nassini et al. 2015; Zhao et al. 2012). Thus, we examined the role of TRPA1 in the engagement of the effects of OXL on oxidative stress in the dorsal horn. We found that blocking NOX4 or TRPA1 in the dorsal horn attenuated mechanical and cold hypersensitivity in OXL rats and blocking NOX4 also attenuated expression of TRPA1 in the dorsal horn, suggesting OXL-oxidative stress signal activates TRPA1.
Our current data showed that OXL amplified expression of TRPA1 in the dorsal horn. Interestingly, intrathecal injection of GKT137831 attenuated upregulation of TRPA1. The effects of GKT137831 were linked to the inhibitory effects of NOX4 on products of oxidative stress 8-iso PGF2α and 8-OHdG because we observed that intrathecal injection of GKT137831 also decreased those oxidative stress products in the dorsal horn. Of note, ROS are considered as endogenously generated molecule mediators during oxidative stress and/or inflammation and TRPA1 is responding to ROS (Andersson et al. 2008; Sawada et al. 2008). Thus, it is well reasoned that increases of 8-iso PGF2α and 8-OHdG induced by OXL upregulated TRPA1 expression in the dorsal horn in the current study.
Accumulated studies have suggested that a variety of miRNAs play critical roles in regulating pain processing within experimental models and clinical pain disorders (Andersen et al. 2014). It has been reported that miR-203 is involved in regulating neuropathic pain development through targeting Rap1a and its downstream signal pathways MEK/ERK (Li et al. 2015). miR-21 is increased by nerve injury, and inhibition of miR-21 attenuates neuropathic pain in a rat model (Sakai and Suzuki 2013). Increased miR-195 by peripheral nerve injury aggravates neuropathic pain by inhibiting autophagy (Shi et al. 2013). A recent study suggests that inhibition of miR-155 decreases the levels of IL-1β, IL-6, and TNF-α in the dorsal horn in a rat neuropathic pain model of chronic constriction injury (Tan et al. 2015). Consistent with these findings, we demonstrated that OXL amplifies miR-155 expression in the dorsal horn of rats and miR-155 inhibitor can attenuate OXL-enhanced NOX4-TRPA1 signal pathways leading to improvement of neuropathic pain. Nonetheless, more investigations are warranted to delineate the networks of miRNAs in regulating neuropathic pain development.
The neuronal cells in the spinal dorsal horn express TRPA1, and intracellular miRNAs are key regulators of gene expression (Park et al. 2014; Tai et al. 2008). In involvement of pain, extracellular miRNAs play a role in neuronal activation and sensory behaviors via toll-like receptor-7 (TLR7) and its coupling to TRPA1 ion channel (Park et al. 2014). Specifically, inhibition of miR-155 in the spinal cord diminished mechanical allodynia and thermal hyperalgesia in rats with chronic constriction injury (Tan et al. 2015). In addition, overexpression of NOX4 is observed in the neuronal and microglial cells after the spinal cord injury (Bermudez et al. 2016; Im et al. 2012). Both changes of Nrf2 and NQO1 are found in the neuron after the spinal cord injury (Li et al. 2016; Liu et al. 2018). Nonetheless, we observed that downregulated Nrf2-NQO1 and amplified NOX4-TRPA1 at the spinal level are engaged in neuropathic pain induced by OXL in the current study. Inhibition of miR-155 at the spinal cord levels improves neuropathic pain via those signal mediators. Deletion of miR-155 in the primary sensory neurons is also an interesting target to improve neuropathic pain after the spinal cord injury (Gaudet et al. 2016).
Although OXL increased TRPA1 expression in the dorsal horn likely through NOX4, it should be noted that some oxidative stress products are known to activate and/or increase other signal mediators rather than TRPA1. For example, the previous findings demonstrate that accumulation of extracellular oxidative protein products stimulates NOX-dependent ROS production, which activate extracellular signal-regulated kinase (ERK)1/2 and p38 mitogen-activated protein kinase (MAPK), and thereby induce cell apoptosis by activating Caspase 3 and poly(ADP-ribose) polymerase (PARP)-1 (Ding et al. 2017; Sun et al. 2016).
In conclusion, OXL impairs Nrf2-antioxidant response and Nrf2-regulated NQO1 in the dorsal horn of rats whereas OXL can amplify NOX4. This process thereby leads to increases of products of oxidative stress 8-iso PGF2α and 8-OHdG in the dorsal horn. Intrathecal administration of miR-155 inhibitor improves impaired antioxidant response and exaggerated oxidative stress signal and thereby attenuates mechanical allodynia and cold hyperalgesia. OXL also increases expression of TRPA1 in the dorsal horn. Inhibition of oxidative stress signal by intrathecal injection of NOX1/4 blocker attenuates TRPA1 expression with decreasing 8-iso PGF2α and 8-OHdG and thereby attenuates allodynia and cold hyperalgesia induced by OXL. We have revealed specific signal pathways of miR-155 engagement in amplified products of oxidative stress and upregulation of TRPA1 in the dorsal horn of rats with mechanical allodynia and cold hyperalgesia after OXL intervention. Overall, our data suggest that inhibition of miR-155 has potential benefits in preventing neuropathic pain development during OXL intervention.
References
Altenhofer S et al (2012) The NOX toolbox: validating the role of NADPH oxidases in physiology and disease. Cell Mol Life Sci 69:2327–2343. https://doi.org/10.1007/s00018-012-1010-9
Altenhofer S, Radermacher KA, Kleikers PW, Wingler K, Schmidt HH (2015) Evolution of NADPH oxidase inhibitors: selectivity and mechanisms for target engagement. Antioxid Redox Signal 23:406–427. https://doi.org/10.1089/ars.2013.5814
Ambros V (2004) The functions of animal microRNAs. Nature 431:350–355. https://doi.org/10.1038/nature02871
Andersen HH, Duroux M, Gazerani P (2014) MicroRNAs as modulators and biomarkers of inflammatory and neuropathic pain conditions. Neurobiol Dis 71:159–168. https://doi.org/10.1016/j.nbd.2014.08.003
Andersson DA, Gentry C, Moss S, Bevan S (2008) Transient receptor potential A1 is a sensory receptor for multiple products of oxidative stress. J Neurosci 28:2485–2494. https://doi.org/10.1523/jneurosci.5369-07.2008
Azevedo MI, Pereira AF, Nogueira RB, Rolim FE, Brito GAC, Wong DVT, Lima-Júnior RCP, de Albuquerque Ribeiro R, Vale ML (2013) The antioxidant effects of the flavonoids rutin and quercetin inhibit oxaliplatin-induced chronic painful peripheral neuropathy. Mol Pain 9:53. https://doi.org/10.1186/1744-8069-9-53
Bartel DP (2004) MicroRNAs: genomics, biogenesis, mechanism, and function. Cell 116:281–297
Bartel DP (2009) MicroRNAs: target recognition and regulatory functions. Cell 136:215–233. https://doi.org/10.1016/j.cell.2009.01.002
Bécouarn Y, Agostini C, Trufflandier N, Boulanger V (2001) Oxaliplatin: available data in non-colorectal gastrointestinal malignancies. Crit Rev Oncol Hematol 40:265–272. https://doi.org/10.1016/S1040-8428(01)00169-X
Bermudez S, Khayrullina G, Zhao Y, Byrnes KR (2016) NADPH oxidase isoform expression is temporally regulated and may contribute to microglial/macrophage polarization after spinal cord injury. Mol Cell Neurosci 77:53–64. https://doi.org/10.1016/j.mcn.2016.10.001
Calame K (2007) MicroRNA-155 function in B cells. Immunity 27:825–827. https://doi.org/10.1016/j.immuni.2007.11.010
Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL (1994) Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods 53:55–63
Chekulaeva M, Filipowicz W (2009) Mechanisms of miRNA-mediated post-transcriptional regulation in animal cells. Curr Opin Cell Biol 21:452–460. https://doi.org/10.1016/j.ceb.2009.04.009
Chen H, Liu Gao MY, Zhang L, He FL, Shi YK, Pan XH, Wang H (2019) MicroRNA-155 affects oxidative damage through regulating autophagy in endothelial cells. Oncol Lett 17:2237–2243. https://doi.org/10.3892/ol.2018.9860
Clark AK, Old EA, Malcangio M (2013) Neuropathic pain and cytokines: current perspectives. J Pain Res 6:803–814. https://doi.org/10.2147/jpr.s53660
Di Cesare Mannelli L, Zanardelli M, Failli P, Ghelardini C (2012) Oxaliplatin-induced neuropathy: oxidative stress as pathological mechanism. Protective effect of silibinin. J Pain 13:276–284. https://doi.org/10.1016/j.jpain.2011.11.009
Ding R, Sun B, Liu Z, Yao X, Wang H, Shen X, Jiang H, Chen J (2017) Advanced oxidative protein products cause pain hypersensitivity in rats by inducing dorsal root ganglion neurons apoptosis via NADPH oxidase 4/c-Jun N-terminal kinase pathways. Front Mol Neurosci 10:195. https://doi.org/10.3389/fnmol.2017.00195
Duan Z, Su Z, Wang H, Pang X (2018) Involvement of pro-inflammation signal pathway in inhibitory effects of rapamycin on oxaliplatin-induced neuropathic pain. Mol Pain 14:1744806918769426. https://doi.org/10.1177/1744806918769426
Eacker SM, Dawson TM, Dawson VL (2009) Understanding microRNAs in neurodegeneration. Nat Rev Neurosci 10:837–841. https://doi.org/10.1038/nrn2726
Elton TS, Selemon H, Elton SM, Parinandi NL (2013) Regulation of the MIR155 host gene in physiological and pathological processes. Gene 532:1–12. https://doi.org/10.1016/j.gene.2012.12.009
Faraoni I, Antonetti FR, Cardone J, Bonmassar E (2009) miR-155 gene: a typical multifunctional microRNA. Biochim Biophys Acta 1792:497–505. https://doi.org/10.1016/j.bbadis.2009.02.013
Farazi TA, Spitzer JI, Morozov P, Tuschl T (2011) miRNAs in human cancer. J Pathol 223:102–115. https://doi.org/10.1002/path.2806
Fidanboylu M, Griffiths LA, Flatters SJ (2011) Global inhibition of reactive oxygen species (ROS) inhibits paclitaxel-induced painful peripheral neuropathy. PLoS One 6:e25212. https://doi.org/10.1371/journal.pone.0025212
Gambari R, Fabbri E, Borgatti M, Lampronti I, Finotti A, Brognara E, Bianchi N, Manicardi A, Marchelli R, Corradini R (2011) Targeting microRNAs involved in human diseases: a novel approach for modification of gene expression and drug development. Biochem Pharmacol 82:1416–1429. https://doi.org/10.1016/j.bcp.2011.08.007
Gaudet AD, Mandrekar-Colucci S, Hall JCE, Sweet DR, Schmitt PJ, Xu X, Guan Z, Mo X, Guerau-de-Arellano M, Popovich PG (2016) miR-155 deletion in mice overcomes neuron-intrinsic and neuron-extrinsic barriers to spinal cord repair. J Neurosci 36:8516–8532. https://doi.org/10.1523/jneurosci.0735-16.2016
Gavazzi G, Banfi B, Deffert C, Fiette L, Schappi M, Herrmann F, Krause KH (2006) Decreased blood pressure in NOX1-deficient mice. FEBS Lett 580:497–504. https://doi.org/10.1016/j.febslet.2005.12.049
Han M, Toli J, Abdellatif M (2011) MicroRNAs in the cardiovascular system. Curr Opin Cardiol 26:181–189. https://doi.org/10.1097/HCO.0b013e328345983d
Hanna, Magdi, Zylicz, Ben Z (2013) Cancer pain. Springer
Hoskin PJ (2008) Radiotherapy. In: Clinical pain management: cancer pain. Hodder Arnold, London, pp 251–255
Im YB, Jee MK, Choi JI, Cho HT, Kwon OH, Kang SK (2012) Molecular targeting of NOX4 for neuropathic pain after traumatic injury of the spinal cord. Cell Death Dis 3:e426. https://doi.org/10.1038/cddis.2012.168
Jaggi AS, Singh N (2011) Therapeutic targets for the management of peripheral nerve injury-induced neuropathic pain. CNS Neurol Disord Drug Targets 10:589–609
Kallenborn-Gerhardt W, Schroder K, del Turco D, Lu R, Kynast K, Kosowski J, Niederberger E, Shah AM, Brandes RP, Geisslinger G, Schmidtko A (2012) NADPH oxidase-4 maintains neuropathic pain after peripheral nerve injury. J Neurosci 32:10136–10145. https://doi.org/10.1523/jneurosci.6227-11.2012
Kallenborn-Gerhardt W, Schroder K, Geisslinger G, Schmidtko A (2013) NOXious signaling in pain processing. Pharmacol Ther 137:309–317. https://doi.org/10.1016/j.pharmthera.2012.11.001
Kannarkat G, Lasher EE, Schiff D (2007) Neurologic complications of chemotherapy agents. Curr Opin Neurol 20:719–725. https://doi.org/10.1097/WCO.0b013e3282f1a06e
Kwan KY, Allchorne AJ, Vollrath MA, Christensen AP, Zhang DS, Woolf CJ, Corey DP (2006) TRPA1 contributes to cold, mechanical, and chemical nociception but is not essential for hair-cell transduction. Neuron 50:277–289. https://doi.org/10.1016/j.neuron.2006.03.042
Lam GY, Huang J, Brumell JH (2010) The many roles of NOX2 NADPH oxidase-derived ROS in immunity. Semin Immunopathol 32:415–430. https://doi.org/10.1007/s00281-010-0221-0
Li H, Huang Y, Ma C, Yu X, Zhang Z, Shen L (2015) MiR-203 involves in neuropathic pain development and represses Rap1a expression in nerve growth factor differentiated neuronal PC12 cells. Clin J Pain 31:36–43. https://doi.org/10.1097/ajp.0000000000000070
Li W, Jiang D, Li Q, Yao S, Sun X, Yang Y, Meng Z, Liu W (2016) Lipopolysaccharide-induced preconditioning protects against traumatic spinal cord injury by upregulating Nrf2 expression in rats. Life Sci 162:14–20. https://doi.org/10.1016/j.lfs.2016.08.008
Liu X, Gu X, Yu M, Zi Y, Yu H, Wang Y, Xie Y, Xiang L (2018) Effects of ginsenoside Rb1 on oxidative stress injury in rat spinal cords by regulating the eNOS/Nrf2/HO-1 signaling pathway. Exp Ther Med 16:1079–1086. https://doi.org/10.3892/etm.2018.6286
Mika J, Zychowska M, Popiolek-Barczyk K, Rojewska E, Przewlocka B (2013) Importance of glial activation in neuropathic pain. Eur J Pharmacol 716:106–119. https://doi.org/10.1016/j.ejphar.2013.01.072
Moalem G, Tracey DJ (2006) Immune and inflammatory mechanisms in neuropathic pain. Brain Res Rev 51:240–264. https://doi.org/10.1016/j.brainresrev.2005.11.004
Moore CS, Rao VT, Durafourt BA, Bedell BJ, Ludwin SK, Bar-Or A, Antel JP (2013) miR-155 as a multiple sclerosis-relevant regulator of myeloid cell polarization. Ann Neurol 74:709–720. https://doi.org/10.1002/ana.23967
Nassini R, Fusi C, Materazzi S, Coppi E, Tuccinardi T, Marone IM, de Logu F, Preti D, Tonello R, Chiarugi A, Patacchini R, Geppetti P, Benemei S (2015) The TRPA1 channel mediates the analgesic action of dipyrone and pyrazolone derivatives. Br J Pharmacol 172:3397–3411. https://doi.org/10.1111/bph.13129
O'Connell RM, Rao DS, Baltimore D (2012) MicroRNA regulation of inflammatory responses. Annu Rev Immunol 30:295–312. https://doi.org/10.1146/annurev-immunol-020711-075013
Park CK, Xu ZZ, Berta T, Han Q, Chen G, Liu XJ, Ji RR (2014) Extracellular microRNAs activate nociceptor neurons to elicit pain via TLR7 and TRPA1. Neuron 82:47–54. https://doi.org/10.1016/j.neuron.2014.02.011
Pasetto LM, D’Andrea MR, Rossi E, Monfardini S (2006) Oxaliplatin-related neurotoxicity: how and why? Crit Rev Oncol Hematol 59:159–168. https://doi.org/10.1016/j.critrevonc.2006.01.001
Portenoy RK (2011) Treatment of cancer pain. Lancet 377:2236–2247. https://doi.org/10.1016/s0140-6736(11)60236-5
Qiu L, Zhang Y (2018) miR-155 modulates cockroach allergen- and oxidative stress-induced cyclooxygenase-2 in asthma. J Immunol 201:916–929. https://doi.org/10.4049/jimmunol.1701167
Sakai A, Suzuki H (2013) Nerve injury-induced upregulation of miR-21 in the primary sensory neurons contributes to neuropathic pain in rats. Biochem Biophys Res Commun 435:176–181. https://doi.org/10.1016/j.bbrc.2013.04.089
Salvemini D, Little JW, Doyle T, Neumann WL (2011) Roles of reactive oxygen and nitrogen species in pain. Free Radic Biol Med 51:951–966. https://doi.org/10.1016/j.freeradbiomed.2011.01.026
Sawada Y, Hosokawa H, Matsumura K, Kobayashi S (2008) Activation of transient receptor potential ankyrin 1 by hydrogen peroxide. Eur J Neurosci 27:1131–1142. https://doi.org/10.1111/j.1460-9568.2008.06093.x
Sayed D, Abdellatif M (2011) MicroRNAs in development and disease. Physiol Rev 91:827–887. https://doi.org/10.1152/physrev.00006.2010
Sereno M, Gutiérrez-Gutiérrez G, Gómez-Raposo C, López-Gómez M, Merino-Salvador M, Tébar FZ, Rodriguez-Antona C, Casado E (2014) Oxaliplatin induced-neuropathy in digestive tumors. Crit Rev Oncol Hematol 89:166–178. https://doi.org/10.1016/j.critrevonc.2013.08.009
Shi G, Shi J, Liu K, Liu N, Wang Y, Fu Z, Ding J, Jia L, Yuan W (2013) Increased miR-195 aggravates neuropathic pain by inhibiting autophagy following peripheral nerve injury. Glia 61:504–512. https://doi.org/10.1002/glia.22451
Sonkoly E, Janson P, Majuri ML, Savinko T, Fyhrquist N, Eidsmo L, Xu N, Meisgen F, Wei T, Bradley M, Stenvang J, Kauppinen S, Alenius H, Lauerma A, Homey B, Winqvist O, Ståhle M, Pivarcsi A (2010) MiR-155 is overexpressed in patients with atopic dermatitis and modulates T-cell proliferative responses by targeting cytotoxic T lymphocyte-associated antigen 4. J Allergy Clin Immunol 126:581–589.e581-520. https://doi.org/10.1016/j.jaci.2010.05.045
Story GM, Peier AM, Reeve AJ, Eid SR, Mosbacher J, Hricik TR, Earley TJ, Hergarden AC, Andersson DA, Hwang SW, McIntyre P, Jegla T, Bevan S, Patapoutian A (2003) ANKTM1, a TRP-like channel expressed in nociceptive neurons, is activated by cold temperatures. Cell 112:819–829
Sun B, Ding R, Yu W, Wu Y, Wang B, Li Q (2016) Advanced oxidative protein products induced human keratinocyte apoptosis through the NOX-MAPK pathway. Apoptosis 21:825–835. https://doi.org/10.1007/s10495-016-1245-2
Suzuki Y, Hattori K, Hamanaka J, Murase T, Egashira Y, Mishiro K, Ishiguro M, Tsuruma K, Hirose Y, Tanaka H, Yoshimura S, Shimazawa M, Inagaki N, Nagasawa H, Iwama T, Hara H (2012) Pharmacological inhibition of TLR4-NOX4 signal protects against neuronal death in transient focal ischemia. Sci Rep 2:896. https://doi.org/10.1038/srep00896
Tai C, Zhu S, Zhou N (2008) TRPA1: the central molecule for chemical sensing in pain pathway? J Neurosci 28:1019–1021. https://doi.org/10.1523/jneurosci.5237-07.2008
Tan Y, Yang J, Xiang K, Tan Q, Guo Q (2015) Suppression of microRNA-155 attenuates neuropathic pain by regulating SOCS1 signalling pathway. Neurochem Res 40:550–560. https://doi.org/10.1007/s11064-014-1500-2
Waseem M, Kaushik P, Tabassum H, Parvez S (2018) Role of mitochondrial mechanism in chemotherapy-induced peripheral neuropathy. Curr Drug Metab 19:47–54. https://doi.org/10.2174/1389200219666171207121313
Winter J, Jung S, Keller S, Gregory RI, Diederichs S (2009) Many roads to maturity: microRNA biogenesis pathways and their regulation. Nat Cell Biol 11:228–234. https://doi.org/10.1038/ncb0309-228
Yang ZB, Chen WW, Chen HP, Cai SX, Lin JD, Qiu LZ (2018) MiR-155 aggravated septic liver injury by oxidative stress-mediated ER stress and mitochondrial dysfunction via targeting Nrf-2. Exp Mol Pathol 105:387–394. https://doi.org/10.1016/j.yexmp.2018.09.003
Zhao M, Isami K, Nakamura S, Shirakawa H, Nakagawa T, Kaneko S (2012) Acute cold hypersensitivity characteristically induced by oxaliplatin is caused by the enhanced responsiveness of TRPA1 in mice. Mol Pain 8:55. https://doi.org/10.1186/1744-8069-8-55
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
All animal protocols were in accordance with the guidelines of the International Association for the Study of Pain and approved by the Institutional Animal Care and Use Committee of Jilin University.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Miao, F., Wang, R., Cui, G. et al. Engagement of MicroRNA-155 in Exaggerated Oxidative Stress Signal and TRPA1 in the Dorsal Horn of the Spinal Cord and Neuropathic Pain During Chemotherapeutic Oxaliplatin. Neurotox Res 36, 712–723 (2019). https://doi.org/10.1007/s12640-019-00039-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12640-019-00039-5