Abstract
Background
Frailty has no single universally accepted definition or method for assessment. It is commonly defined from a physiological perspective as a disruption of homeostatic mechanisms ultimately leading to a vulnerable state. Numerous scoring indices and assessments exist to assist clinicians in determining the frailty status of a patient. The purpose of this review is to discuss the relationship between frailty and perioperative outcomes in surgical patients.
Principal findings
We performed a review to determine the association of frailty with perioperative outcomes in patients undergoing a wide variety of surgical procedures. A scoping literature search was performed to capture studies from MEDLINE®, EMBASE™, and CENTRAL (Cochrane), which resulted in locating 175 studies across the three electronic databases. After an article screening process, 19 studies were found that examined frailty and perioperative outcomes. The studies used a range of assessments to determine frailty status and included patients in a variety of surgical fields. Regardless of surgical population and method of frailty assessment, a relationship existed between adverse perioperative outcomes and frailty status. Frail patients undergoing surgical procedures had a higher likelihood than non-frail patients of experiencing mortality, morbidity, complications, increased hospital length of stay, and discharge to an institution.
Conclusions
Patients undergoing surgery who are deemed frail, regardless of the scoring assessment used, have a higher likelihood of experiencing adverse perioperative outcomes. With the lack of a unified definition for frailty, further research is needed to address which assessment method is most predictive of adverse postoperative outcomes.
Résumé
Contexte
La fragilité ne répond à aucune définition ou méthode d’évaluation universellement acceptée. Elle est couramment définie d’un point de vue physiologique comme une perturbation des mécanismes homéostatiques conduisant finalement à un état de vulnérabilité. De nombreux indices de cotation et d’évaluation existent pour aider les cliniciens à définir l’état de fragilité d’un patient. L’objectif de cette synthèse est de discuter les rapports existant entre la fragilité et les aboutissements périopératoires chez les patients chirurgicaux.
Constatations principales
Nous avons effectué une étude de synthèse afin de préciser l’association entre fragilité et aboutissements périopératoires chez des patients devant subir une grande variété de procédures chirurgicales. Une recherche ciblée de la littérature a été menée dans les bases de données électroniques MEDLINE®, EMBASE™ et CENTRAL (Cochrane) pour identifier les études pertinentes: 175 études ont été localisées. Après un processus de sélection des articles, 19 études portant sur la fragilité et les aboutissements périopératoires ont été conservées. Ces études utilisaient différentes évaluations pour déterminer l’état de fragilité et incluaient des patients dans des domaines chirurgicaux variés. Indépendamment de la population chirurgicale et de la méthode d’évaluation de la fragilité, il existait une relation entre les évènements périopératoires indésirables et le statut de fragilité. Les patients fragiles subissant des procédures chirurgicales avaient une plus grande probabilité que les patients non fragiles d’être confrontés au décès, à une morbidité, à des complications, à un allongement de la durée de séjour et au congé vers un établissement de soins de longue durée.
Conclusions
Les patients subissant une intervention chirurgicale et qui sont jugés fragiles, indépendamment du système d’évaluation utilisé ont une plus grande probabilité d’éprouver des évènements périopératoires indésirables. En l’absence de définition unique de la fragilité, des recherches supplémentaires sont nécessaires pour identifier quelle méthode d’évaluation prédit le mieux la survenue d’aboutissements postopératoires indésirables.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Overview and rationale
Frailty is a distinctive health state related to the aging process that results in a decrease in both reserve and resistance to stressors and ultimately, in vulnerability to adverse outcomes.1 Frailty is estimated to be present in 10% of people over the age of 65 and increases to 25-50% of people over the age of 85.2 Various frailty assessments have been shown to determine whether a patient will exhibit a decline in health in response to medical or surgical stressors.2 Despite this, the multitude of definitions and scoring systems that have been developed for frailty make it difficult for healthcare practitioners to incorporate a standard assessment in clinical care.
In this review, we examine the literature and ultimately aim to determine the clinical utility of frailty as a preoperative assessment. In the Introduction, we discuss the definition of frailty and summarize common frailty assessments, and in the Methods section, we examine and analyze literature that explores the association of frailty with a range of perioperative and surgical outcomes. Lastly, in the Discussion section, we discuss the significance of considering frailty during preoperative assessment. Importantly, while not the main focus of this narrative review, we also provide a basic foundation to assist clinicians in developing an approach for the management of frail older adults undergoing surgery.
What is frailty?
A common theme in examining frailty as a syndrome is an increased vulnerability to stressors as a result of decreased physiological reserve.3-5 This in turn increases the risk of adverse clinical consequences to stressors.6 Indeed, Afilalo et al.7 have classified stressors as falling into the categories of acute or chronic illness as well as due to iatrogenic processes.
There are several different models outlining the pathophysiology of how frailty develops and manifests; however, the two more commonly referenced models of frailty are the “phenotype” model described by Fried et al. and the “deficit” model used by Rockwood et al.1,5 In the phenotype model, frailty manifests itself with “declines in lean body mass, strength, endurance, balance, walking performance and low activity”.1 The Fried phenotype assessment evaluates for the presence of such features. In the deficit model, such as in the Canadian Study of Health and Aging (CSHA),5 it was found that “summing the number of impairments” and clinical deficits (which include a large range of symptoms, from an inability to perform activities of daily living to mood disorders) can also determine frailty.5
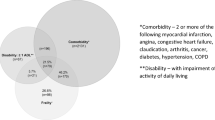
There is an overlap in management approaches for patients who are frail and for those with multimorbidities. The deficit model of frailty encompasses multimorbidity, as it incorporates disease and disability as well as cognitive, psychological, and social factors into the deficits. While not everyone with multimorbidities are labelled frail, once a certain number of morbidities have been reached, a patient can be classified as frail, with more deficits leading to an increased level of frailty.
Regardless of the model of frailty used, it is important for healthcare practitioners to be mindful that exposure to stressors has a profound impact on the health status of patients deemed frail and can be linked to poor outcomes. This is reflected in the fact that frail patients are at an increased risk of adverse events such as delirium,8 procedural complications, disability, mortality, morbidity, slowed recovery,5,7 cardiovascular events, and increased hospital length of stay (LOS).9
Frailty and an aging population
There is little doubt that the older adult population is growing at a rapid rate in North America and worldwide. In the United States, the population of adults aged 65 and older is expected to reach 80 million during the years 2010-2040.10 According to Social Development Canada, approximately one quarter of the population in Canada will be over the age of 65 by the year 2041. Increasing age has a well-defined correlation with frailty status, but aging alone is not necessarily synonymous with frailty.6 Nonetheless, similar features are shared by both frailty and aging. In both states, there is a loss of homeostatic mechanisms to respond to stressors and the manifestation of cellular responses such as apoptosis, cellular senescence, and cellular repair.11 Some studies suggest that factors preceding a frail state come into play before a patient reaches old age.12 As such, frailty can be considered a model for unsuccessful aging.
In a separate report, Rockwood et al. looked to investigate the influence of aging in relation to patients who are fit vs patients who are frail.12 Their study used a frailty index based on an accumulation of deficits whereby a patient’s frailty status was a component of the number of deficits. From this analysis, the authors observed that those who are relatively fit at all ages had a lower risk of death as well as less utilization of healthcare resources. In contrast, increasing frailty indices were associated with higher mortality and more utilization of healthcare services. Studies such as these indicate that, although frailty is often linked to age, there is variation within age groups due to the multifactorial nature of frailty.13 In a prospective Canadian study examining frailty and intensive care unit (ICU) admission in patients aged 50 and older, it was shown that frailty can occur in a relatively younger patient demographic (i.e., those ≥ 50 yr of age).14 It was determined that frailty status in ICU patients aged 50 and older was associated with a greater likelihood of experiencing adverse events such as nosocomial infection and re-intubation, greater in-hospital and ICU LOS, increased in-hospital mortality, and increased risk of mortality 12 months following ICU admission.14
With an increasingly older adult population, it can be assumed that there will be an increasing number of individuals who are frail. In a cohort study looking at frailty and adult lifespan in a Canadian population, it was determined that the prevalence of frailty exhibited an exponential pattern with age.12 Another Canadian study using a Clinical Frailty Scale (CFS) determined that 43.3% of patients in a cohort of 2,305 patients aged 65 yr and older had a score of “vulnerable” or greater.5,6 Interestingly, increased CFS scores were characteristic of being older, female, having problems with ambulation, cognitive impairment, as well as the presence of more comorbidities.5,6
Pathophysiology, association and interaction of factors leading to frailty
It is debatable whether frailty is a process incumbent with normal aging or if it is a distinct pathophysiological process.15 The mechanism of frailty as a pathophysiological process is not fully understood.16 It has been proposed that an interplay of inflammatory processes, endocrine changes, inactivity, and malnutrition leads to sarcopenia and ultimately to a frail status (Figure). Syndromes such as sarcopenia, as well as cachexia, disability, and comorbidity do “dip into the waters” of frailty, as these syndromes are commonly seen together.15 Sarcopenia has a strong connection with a frail state as decreasing muscle mass in the elderly plays a role in the evolution of frailty.1,17 From an endocrine point of view, an enhanced risk of sarcopenia and frailty is seen in relation to having low gonadal hormone levels and insulin-like growth factor-1 (IGF-1), along with high levels of inflammatory mediators, low vitamin D, and being in a pro-coagulative state.16 Poor nutritional intake is also characteristic of both frailty and sarcopenia.18 Clearly, there is an interaction among environmental, genetic, as well as age-related factors that determines frailty.
Frailty also appears to have an inflammatory component. It is known that preoperative inflammatory and coagulation markers are higher in frail patients.6 These markers include interleukin-6 (IL-6), tumour necrosis factor-alpha, C-reactive protein, coagulation factor VIII, and D-dimer.6,15 With respect to biomarkers, IL-6 may be an important factor, as increased plasma levels have the highest association with frailty.18 Similarly, Afilalo et al. also mention other biomarkers that have a correlation with frailty,7 some of them being markers of inflammation. These included lymphocyte count, memory/naïve CD8 T-cell count, plasminogen activator inhibitor-1, testosterone, insulin-like growth factor-1, albumin, and vitamin D.7
Why measure frailty?
With no widely universal definition of frailty6 and the creation of many frailty scales, it is reasonable to question why frailty is measured. One reason is that frailty “identifies groups of people in need of extra medical attention”.19 Fulop et al. summated that “most important for the concept of frailty is the ability to predict it, so it can be modulated or even prevented”.18 Further rationale for the importance of assessing patient frailty is that such measures can be utilized as a clinical tool for optimizing healthcare policy planning.5 Clinicians can use a patient’s frailty status to help predict adverse consequences, such as the likelihood of mortality or if a patient is likely to require care in an institution.5 In terms of healthcare policy, these measures can be used to help in identifying the need for healthcare services and their allocation.5 The relationship of ICU resources and the older adult population may help support the usefulness of frailty measures, as they can help to determine ICU and long-term prognosis.6
What are common frailty assessments and their criteria?
With no universal criteria for what constitutes a frail patient, multiple frailty assessments and criteria have been generated. We tabulated what we consider to be some common frailty assessments and their respective criteria (Table 1).
Frailty in the surgical setting
Frail patients tend to have worse health in all illness settings.20 Logically, a frail patient will likely not cope well with a major stressor such as surgery. Advanced age has already been shown to be a risk factor for poor surgical outcomes.21 The association of frailty with both age and decreased physiological reserve leads to the opinion that frailty can be determined preoperatively in order to predict the risk of postoperative outcomes. Current preoperative assessments tend to focus on end-organ compromise, whereas frailty is a systemic indicator of overall health and physiological status.20 This potentially makes characterizing frailty a useful tool for predicting both mortality and functional postoperative outcomes. The text that follows describes our search of the literature for studies analyzing frailty status in older adult surgical patients and the relationship of frailty with surgical outcomes.
Methods
In older adult patients about to undergo surgery, do postoperative outcomes differ between patients deemed frail and those deemed not frail?
Frailty has been shown to be a predictor of poor health and response to stressors. This literature search aimed to examine whether preoperative assessments of frailty are linked to worse postoperative outcome. We focused on studies describing an adult (18 years of age and older) surgical population. Studies to be considered had to have a well-defined frailty assessment performed preoperatively with comparisons made between patients deemed frail and those deemed not frail. Studies also had to report specific postoperative outcomes such as mortality, disability, or cost.
Data source and search strategy
In collaboration with a medical librarian (A.S.Z.), a scoping literature search was designed and conducted to capture best-evidence articles and literature regarding frailty, frailty assessments, and perioperative outcomes. The included studies were published during 2009-2014. The following electronic databases were used in the search: MEDLINE®, EMBASE™, and CENTRAL (Cochrane). The search resulted in 175 articles across the three databases.
Article eligibility and selection criteria
From the 175 articles across the three databases, two reviewers (T.B. and A.S.) reviewed articles using a predetermined screening process. Articles were first screened on the basis of title, abstract, and whether or not they were full-text journal articles. In order to be included for data extraction into relevant tables, certain criteria had to be met as discussed previously by the authors. Firstly, articles had to use a well-defined frailty assessment/tool in a surgical population. Secondly, articles had to have a definitively measured perioperative surgical outcome. One author (T.B.) conducted the data extraction by collecting relevant and pertinent information, while another author (A.S.) verified the data extraction. While this review is not a systematic review per se, we adopted many of the PRISMA guidelines for systematic reviews and meta-analyses to strengthen our review.
Results
Basic study characteristics
Nineteen articles were used for the purposes of data extraction. The patient populations can be broken down based on type of surgical procedure performed. Four studies involved patients having cardiac valve surgery (including transcatheter aortic valve repplacement).4,22-24 Five studies involved a mix of gastrointestinal surgical patients,25-27 including abdominal21 and other general surgery patients.28 Two studies involved vascular surgical patients29,30 and two involved surgical oncology patients with either gynecological neoplasms31 or gastric adenocarcinoma.32 Two of the studies involved comprehensive surgical populations,33,34 one study involved thoracic surgical patients undergoing lobectomy;35 two studies used a mix of patients undergoing a mix of surgical procedures,20,36 and one study involved patients undergoing a mix of minimally invasive surgical procedures.37 All studies were published during 2009-2014. Table 2 highlights the surgical populations and the association of frailty with perioperative outcomes for the articles included.
Frailty and perioperative surgical outcomes
All included studies showed an association between defined perioperative outcomes and frailty. In eight studies, mortality was a perioperative outcome associated with frailty.4,22,24,25,29,32,33,35 There was a wide variety of odds ratios (OR) for mortality reported in these studies, likely due to the variation in surgical population and frailty assessment used. For example, one study involving cardiac surgical patients reported an OR of 1.10 (95% confidence interval [CI] 1.04 to 1.16),22 while another study conducted in patients undergoing esophagectomy reported a very high OR of 31.84.25 Eight studies showed an association between frailty and the development of postoperative complications.20,21,26,27,31,34,36,37 As with mortality, a wide variety of ORs was reported for the development of complications, likely also due to the variation in surgical population and frailty assessment used. With respect to 30-day postoperative complications, the OR ranged from as low as 1.05 (95% CI 0.94 to 1.17) in older adult abdominal surgical patients21 to as high as 11.70 in patients undergoing emergency general surgery.28 One study using the Groningen Frailty Index (GFI) in vascular surgical patients found that a GFI of ≥ 4 had a significant relationship with the development of postoperative delirium.30
Various studies consistently listed infectious causes as the leading cause of postoperative complications.21,26-28,30 Infection often manifested itself as surgical site infection but also included pneumonia, urinary tract infection (UTI), and septicemia. In addition, those deemed more frail using a modified frailty index (mFI) showed an increased incidence of prolonged ventilation (38.9%) and re-intubation (22.2%).26 Delirium was another common presentation of postoperative complications28,37 and is itself a predictor of increased LOS. Cardiac complications were also noted. There was a significant correlation between myocardial infarctions and increased frailty scores.26 Another common cardiac complication was arrhythmia,27,28,37 which was present in up to 3.6% of patients in some studies.28 These are important complications that anesthesiologists and intensivists may have to manage in the postoperative period.
Three studies looked at increased LOS in relation to frailty26,34,36 as well as other perioperative outcomes. One study using a frailty assessment based on the Fried frailty criteria in older adult patients found that an association between increased LOS and frailty status existed in all types of surgical procedures.34 For example, patients classified as intermediately frail in this study had an incident risk ratio (IRR) of 1.5 (95% CI 1.2 to 1.8) with respect to increased LOS, while those classified as frail had an IRR of 1.7 (95% CI 1.3 to 2.2) with respect to increased LOS. Two studies24,34 examined institutionalization in addition to other perioperative outcomes. In older adult patients undergoing many types of surgeries, odds ratios for discharge to an institution were similar between frail cardiac surgery patients24 and intermediately frail patients34 (OR 3.7; 95% CI 1.8 to 7.7 and OR 3.2; 95% CI 1.0 to 10.0, respectively). Importantly, when an older adult patient was classified as “frail” in a study involving all types of surgeries,34 the OR increased to 20.5 and had a wide 95% CI of 5.5 to 75.7.
Discussion and future directions
Frailty is associated with negative perioperative outcomes
In this review, multiple studies involving a variety of surgical populations identified a relationship between negative perioperative outcomes and frailty status. Even with a multitude of frailty assessments used and variation in surgical populations (Table 3), these studies collectively indicate a consensus that patients deemed to be frail have a higher likelihood of experiencing mortality, morbidity, complications, increased LOS, and discharge to a non-home institution.
Does this review mirror the findings of others?
It is important to emphasize that our findings accurately reflect the findings of previously published studies regarding frailty as an independent risk factor for negative surgical outcomes. Partridge et al. 15 also examined frailty definitions and methods of frailty assessment and their impact in the surgical population. Our review was similar in the sense that a number of frailty assessments were used in a variety of surgical populations. The present review included numerous studies pertaining to frailty assessments and perioperative outcomes in surgical populations.
Frailty assessments and the scoring indices of the included studies
Each study used a defined frailty assessment and/or scoring index in a surgical population (Table 3). Methods for obtaining frailty scores as part of an assessment tool or scoring index were collected through a variety of questionnaires, physical function tests, and laboratory biomarkers. The majority of the frailty assessments used were replicas or modifications of the more commonly used and validated frailty assessments that we have cited earlier (See Table 1). To highlight some of the more common assessments, five studies used a replica or modification of the Fried frailty criteria;23,27,31,34,37 two studies used a replica or modification of the CSHA-FI based on an accumulation of deficits (where the more deficits accumulated the more frail the patient),21,33 and four studies used a mFI.25,28,29,35 The other studies utilized a range of frailty assessments, as outlined in Table 3. Clearly, there is a lack of consensus for a clear definition of frailty and for the best assessment tool to use in determining frailty status. More specifically, future research should focus on determining which assessment of frailty is best at predicting postoperative outcomes.
Clinical significance and future research directives
The results of our review provide important information for healthcare professionals in a variety of settings. Indeed, our findings are pertinent for healthcare providers involved in the care and evaluation of a patient before, during, and after surgery (perioperative period). It is of vital importance that perioperative healthcare providers understand that frailty has a link to the development of negative postoperative outcomes. As stated by authors in a paper regarding outcomes and their importance to perioperative elderly care, “increased healthcare usage by the elderly (particularly the frail “oldest old”) requires reciprocal, coordinated continuity of care between community, hospital and rehabilitation services, if patients are to be managed safely, inexpensively and with dignity”.38 Our findings are also important for healthcare researchers. From our findings, it seems that, irrespective of the assessment of frailty used, frail patients are associated with more poor postoperative outcomes. Future research should focus on evaluating how frailty can be modified in a patient once it is identified so that preventative strategies or minimization of negative perioperative adverse events can be achieved. An example of work in this field is the study by Arthur et al. 39 which shows that patients attending a preoperative exercise program prior to coronary artery bypass graft (CABG) procedures have better outcomes in quality of life (QoL) and hospital LOS. Similar research should be conducted on frail patients to determine if preoperative intervention can minimize, or even reverse, the effects of having a frail status.
A gold standard frailty assessment has yet to be established. This was clearly shown by the wide range of frailty assessments utilized in the articles examined. Creation of a unified frailty assessment methodology would prove invaluable in the hospital setting. Regarding surgery, research should examine which components of frailty are most associated with poor surgical outcome. For example, Afilalo et al. 9 compared various frailty assessments with postoperative outcomes, and determined that gait speed was the most statistically significant predictor of mortality and morbidity (OR 2.63; 95% CI 1.17 to 5.90). Continued research in this area could prove frailty status to be a valuable preoperative assessment tool in the future.
How best to manage the frail patient
Ultimately, clinicians want to be able to use this information to provide optimal healthcare for patients. Currently, however, definitive criteria are lacking on how best to manage the “frail patient”. This is partly due to the heterogeneous nature of frailty. Nevertheless, treatments that address the conditions often associated and occurring with frailty can serve as guidelines for managing a frail patient.
Frailty is a multidimensional condition involving many organ systems.40 Nutrition is an important factor in all aging patients, but seemingly more so in frail patients. Frail patients often exhibit anemia and hypoalbuminemia, two potential markers of poor nutrition.40,41 In addition, nutrition plays a role in sarcopenia, which is often seen with frailty and tested in frailty assessments through physical function tests such as gait speed, get up and go, and grip strength. Literature recommendations have cited that increasing protein intake in community-dwelling older adults can combat the disability associated with sarcopenia,40,41 which is a “surrogate marker of frailty”.40 The surgical literature has also recommended early enteric feeding for patients who are undergoing colorectal surgery or a cystectomy.40,42,43 Postoperative nutrition guidelines such as this can also be applied to frail patients undergoing these types of operations.
Exercise is another proposed aspect of management that may help to improve perioperative and postoperative outcomes in frail surgical patients. Studies have shown that exercise intervention can improve functional outcomes, balance, and gait speed.40 The concept of “prehabilitation” is likely to become an area of increasing interest within the frailty literature as it may optimize the risk profile of frail surgical patients. Preoperative exercise programs have already shown to be beneficial in regard to postoperative outcomes. In a pilot randomized controlled trial of prehabilitation for elective CABG patients, patients participating in the “prehab” exercise program improved their physical fitness as evaluated through a preoperative six-minute walk and 5-m gait speed test, and this improvement was preserved in the postoperative period.44 In an orthopedic study, preoperative exercise programs prior to total joint arthroplasty improved physical function testing postoperatively compared with baseline.45 Preoperative exercise programs address the physical components of frailty and sarcopenia and would seem to be beneficial. Research is beginning to emerge on the effects of prehabilitation in a variety of patients.45,46 A randomized controlled trial, termed the PREHAB (Preoperative REhabilitation for reduction of Hospitalization After coronary Bypass and valvular surgery – NCT02219815) study is currently underway and looking at the effects of prehabilitation on frail patients undergoing cardiac surgery.
Exercise in the postoperative period also represents a window of opportunity that may help to improve outcomes associated with frailty in the surgical patient. In a review conducted by Jack et al. addressing postoperative exercise training in the older adult patient, they stated “…there is now convincing evidence that physical fitness is associated with outcome following major surgery; less-fit patients having a greater risk of complications and death”.47 While this is specific to the elderly, we deduce that early mobilization and postoperative exercise programs are just as, if not more, important in the recovery of a frail surgical patient.
We also recommend that clinicians, whether surgeon, anesthesiologist, nurse, or other therapist, seek out a comprehensive geriatric assessment and model of care in the appropriate patient population. Firstly, it is important that clinicians familiarize themselves with frailty and assessment criteria. As there is no single definition for frailty, we cannot recommend one specific assessment over another, as they will vary depending on location and resource availability. Nevertheless, we recommend including a physical function component in any assessment, particularly as gait speed was shown to have the highest association with mortality in postoperative CABG patients.9 The multisystem nature of frailty appears to make management of this patient population challenging for the clinical team, as defined criteria are lacking that exemplify the gold standard model of care. Nevertheless, in a study by Ganz et al., the authors proposed a model of care for providing high-quality care for vulnerable elders. This model aims to identify and improve outcomes such as health-related QoL, function, longevity, and disease control. In this model, there are three core realms to improve these outcomes: communication between the patient and caregiver, a personal care plan, and coordination of care between healthcare providers.48 A co-management model where all providers of healthcare share responsibilities is useful for managing the frail patient who has undergone a major surgical stressor. This necessitates sufficient access to other clinical experts, such as geriatricians, rehabilitation therapists, nurse specialists, and case managers, while establishing links to the community.48
Conclusion
Our review shows that frailty, as measured using a variety of tools and assessments, shows a negative relationship with respect to perioperative adverse outcomes in a variety of surgical populations. Using some measurement of frailty is useful in a clinician’s preoperative assessment as it can capture functional domains often missed by traditional preoperative risk scores. Frailty in a patient has consistently been shown to be an independent risk factor in the development of adverse postoperative outcomes such as mortality, morbidity, discharge to institution, and increased hospital LOS.15 Perioperative knowledge of the frailty status of a very ill patient may also have implications for decision-making regarding end of life and palliative care49 and may lead to more effective shared decision-making among patients, their families, and the clinical team.14 Frailty can thus have a prognostic value as medical interventions not considered beneficial for improving health can possibly be withdrawn or minimized if so desired by patients, loved ones, and caregivers.49 Preoperative frailty measures can help to identify any modifiable factors in a patient that, if enhanced, are more likely to lead to a successful outcome.15
Further study is needed to evaluate how best to minimize frailty status in the older adult patient, whether via preoperative intervention or postoperative rehabilitation. Current suggestions for the management of frail patients include optimizing nutritional status, widespread use of preoperative and postoperative exercise programs, and a well-outlined model of care to familiarize the healthcare team with the frailty assessment being used.
Key points
-
At present, frailty has no single universal definition or method for assessment/scoring.
-
Frailty is a multifactorial and complex health state representing an interplay among physiologic, endocrine, genetic, inflammatory, and age-related factors.
-
With age being a strong risk factor for frailty and an ever-increasing aging population presenting for surgery, it is important for perioperative clinicians to be knowledgeable about frailty as it is frequently seen in older adult patients.
-
Frailty exists in patients undergoing many types of surgical interventions, and regardless of the method use in its assessment, it is linked to adverse perioperative outcomes.
-
Future research is needed to determine if the evaluation of frailty status should be part of routine perioperative care and if the effects of being frail can be minimized.
References
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001; 56: M146-56.
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet 2013; 381: 752-62.
Brown NA, Zenilman ME. The impact of frailty in the elderly on the outcome of surgery in the aged. Adv Surg 2010; 44: 229-49.
Afilalo J, Mottillo S, Eisenberg MJ, et al. Addition of frailty and disability to cardiac surgery risk scores identifies elderly patients at high risk of mortality or major morbidity. Circ Cardiovasc Qual Outcomes 2012; 5: 222-8.
Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005; 173: 489-95.
Bagshaw SM, McDermid RC. The role of frailty in outcomes from critical illness. Curr Opin Crit Care 2013; 19: 496-503.
Afilalo J, Alexander KP, Mack MJ, et al. Frailty assessment in the cardiovascular care of older adults. J Am Coll Cardiol 2014; 63: 747-62.
Leung JM, Tsai TL, Sands LP. Brief report: preoperative frailty in older surgical patients is associated with early postoperative delirium. Anesth Analg 2011; 112: 1199-201.
Afilalo J, Eisenberg MJ, Morin JF, et al. Gait speed as an incremental predictor of mortality and major morbidity in elderly patients undergoing cardiac surgery. J Am Coll Cardiol 2010; 56: 1668-76.
Adams P, Ghanem T, Stachler R, Hall F, Velanovich V, Rubinfeld I. Frailty as a predictor of morbidity and mortality in inpatient head and neck surgery. JAMA Otolaryngol Head Neck Surg 2013; 139: 783-9.
Fedarko NS. The biology of aging and frailty. Clin Geriatr Med 2011; 27: 27-37.
Rockwood K, Song X, Mitnitski A. Changes in relative fitness and frailty across the adult lifespan: evidence from the Canadian National Population Health Survey. CMAJ 2011; 183: E487-94.
Saxton A, Velanovich V. Preoperative frailty and quality of life as predictors of postoperative complications. Ann Surg 2011; 253: 1223-9.
Bagshaw SM, Stelfox HT, McDermid RC, et al. Association between frailty and short- and long-term outcomes among critically ill patients: a multicentre prospective cohort study. CMAJ 2014; 186: E95-102.
Partridge JS, Harari D, Dhesi JK. Frailty in the older surgical patient: a review. Age Ageing 2012; 41: 142-7.
Topinkova E. Aging, disability and frailty. Ann Nutr Metab 2008; 52(Suppl 1): 6-11.
Landi F, Cruz-Jentoft AJ, Liperoti R, et al. Sarcopenia and mortality risk in frail older persons aged 80 years and older: results from ilSIRENTE study. Age Ageing 2013; 42: 203-9.
Fulop T, Larbi A, Witkowski JM, et al. Aging, frailty and age-related diseases. Biogerontology 2010; 11: 547-63.
Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc 2012; 60: 1487-92.
Robinson TN, Wu DS, Pointer L, Dunn CL, Cleveland JC Jr, Moss M. Simple frailty score predicts postoperative complications across surgical specialties. Am J Surg 2013; 206: 544-50.
Cohen RR, Lagoo-Deenadayalan SA, Heflin MT, et al. Exploring predictors of complication in older surgical patients: a deficit accumulation index and the Braden Scale. J Am Geriatr Soc 2012; 60: 1609-15.
Sundermann S, Dademasch A, Praetorius J, et al. Comprehensive assessment of frailty for elderly high-risk patients undergoing cardiac surgery. Eur J Cardiothorac Surg 2011; 39: 33-7.
Green P, Woglom AE, Genereux P, et al. The impact of frailty status on survival after transcatheter aortic valve replacement in older adults with severe aortic stenosis: A single-center experience. JACC Cardiovasc Interv 2012; 5: 974-81.
Ganapathi AM, Englum BR, Hanna JM, et al. Frailty and risk in proximal aortic surgery. J Thorac Cardiovasc Surg 2014; 147: 186-91.e1.
Hodari A, Hammoud ZT, Borgi JF, Tsiouris A, Rubinfeld IS. Assessment of morbidity and mortality after esophagectomy using a modified frailty index. Ann Thorac Surg 2013; 96: 1240-5.
Lasithiotakis K, Petrakis J, Venianaki M, et al. Frailty predicts outcome of elective laparoscopic cholecystectomy in geriatric patients. Surg Endosc 2013; 27: 1144-50.
Tan KY, Kawamura YJ, Tokomitsu A, Tang T. Assessment for frailty is useful for predicting morbidity in elderly patients undergoing colorectal cancer resection whose comorbidities are already optimized. Am J Surg 2012; 204: 139-43.
Farhat JS, Velanovich V, Falvo AJ, et al. Are the frail destined to fail? Frailty index as predictor of surgical morbidity and mortality in the elderly. J Trauma Acute Care Surg 2012; 72: 1526-30.
Karam J, Tsiouris A, Shepard A, Velanovich V, Rubinfeld I. Simplified frailty index to predict adverse outcomes and mortality in vascular surgery patients. Ann Vasc Surg 2013; 27: 904-8.
Pol RA, van Leeuwen BL, Visser L, et al. Standardised frailty indicator as predictor for postoperative delirium after vascular surgery: a prospective cohort study. Eur J Vasc Endovasc Surg 2011; 42: 824-30.
Courtney-Brooks M, Tellawi AR, Scalici J, et al. Frailty: an outcome predictor for elderly gynecologic oncology patients. Gynecol Oncol 2012; 126: 20-4.
Tegels JJ, de Maat MF, Hulsewe KW, Hoofwijk AG, Stoot JH. Value of geriatric frailty and nutritional status assessment in predicting postoperative mortality in gastric cancer surgery. J Gastrointest Surg 2014; 18: 439-46.
Velanovich V, Antoine H, Swartz A, Peters D, Rubinfeld I. Accumulating deficits model of frailty and postoperative mortality and morbidity: its application to a national database. J Surg Res 2013; 183: 104-10.
Makary MA, Segev DL, Pronovost PJ, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg 2010; 210: 901-8.
Tsiouris A, Hammoud ZT, Velanovich V, Hodari A, Borgi J, Rubinfeld I. A modified frailty index to assess morbidity and mortality after lobectomy. J Surg Res 2013; 183: 40-6.
Dasgupta M, Rolfson DB, Stolee P, Borrie MJ, Speechley M. Frailty is associated with postoperative complications in older adults with medical problems. Arch Gerontol Geriatr 2009; 48: 78-83.
Revenig LM, Canter DJ, Master VA, et al. A prospective study examining the association between preoperative frailty and postoperative complications in patients undergoing minimally invasive surgery. J Endourol 2014; 28: 476-80.
Peden CJ, Grocott MP. National research strategies: what outcomes are important in peri-operative elderly care? Anaesthesia 2014; 69(Suppl 1): 61-9.
Arthur HM, Daniels C, McKelvie R, Hirsh J, Rush B. Effect of a preoperative intervention on preoperative and postoperative outcomes in low-risk patients awaiting elective coronary artery bypass graft surgery. A randomized, controlled trial. Ann Intern Med 2000; 133: 253-62.
Revenig LM, Ogan K, Guzzo TJ, Canter DJ. The use of frailty as a surgical risk assessment tool in elderly patients. Curr Geriatr Rep 2014; 3: 1-7.
Waters DL, Baumgartner RN, Garry PJ, Vellas B. Advantages of dietary, exercise-related, and therapeutic interventions to prevent and treat sarcopenia in adult patients: an update. Clin Interv Aging 2010; 5: 259-70.
Andersen HK, Lewis SJ, Thomas S. Early enteral nutrition within 24h of colorectal surgery versus later commencement of feeding for postoperative complications. Cochrane Database Syst Rev 2006; 4: CD004080.
Lewis SJ, Andersen HK, Thomas S. Early enteral nutrition within 24 h of intestinal surgery versus later commencement of feeding: a systematic review and meta-analysis. J Gastrointest Surg 2009; 13: 569-75.
Sawatzky JA, Kehler DS, Ready AE, et al. Prehabilitation program for elective coronary artery bypass graft surgery patients: a pilot randomized controlled study. Clin Rehabil 2014; 28: 648-57.
Desmeules F, Hall J, Woodhouse LJ. Prehabilitation improves physical function of individuals with severe disability from hip or knee osteoarthritis. Physiother Can 2013; 65: 116-24.
Brown K, Loprinzi PD, Brosky JA, Topp R. Prehabilitation influences exercise-related psychological constructs such as self-efficacy and outcome expectations to exercise. J Strength Cond Res 2014; 28: 201-9.
Jack S, West M, Grocott MP. Perioperative exercise training in elderly subjects. Best Pract Res Clin Anaesthesiol 2011; 25: 461-72.
Ganz DA, Fung CH, Sinsky CA, Wu S, Reuben DB. Key elements of high-quality primary care for vulnerable elders. J Gen Intern Med 2008; 23: 2018-23.
Koller K, Rockwood K. Frailty in older adults: implications for end-of-life care. Cleve Clin J Med 2013; 80: 168-74.
Acknowledgement
We sincerely acknowledge the PREHAB investigators for their support.
Funding
Navdeep Tangri is supported by the KRESCENT New Investigator Award and the MHRC Establishment Award. The KRESCENT New Investigator Award is a joint initiative of the Canadian Institute of Health Research, the Kidney Foundation of Canada, and the Canadian Society of Nephrology.
Conflicts of interest
None declared.
Disclosures
Dr. Rakesh Arora has an unrestricted educational grant from Pfizer Canada Inc. for work unrelated to the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Co-first authors: Thomas Beggs and Aresh Sepehri
Co-senior authors: Navdeep Tangri and Rakesh C. Arora
Rights and permissions
About this article
Cite this article
Beggs, T., Sepehri, A., Szwajcer, A. et al. Frailty and perioperative outcomes: a narrative review. Can J Anesth/J Can Anesth 62, 143–157 (2015). https://doi.org/10.1007/s12630-014-0273-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-014-0273-z