Abstract
Purpose of Review
To review the role of radiation therapy and specifically metastasis-directed stereotactic body radiation therapy (SBRT) in the management of patients with oligometastatic breast cancer with emphasis on potential toxicities and future directions.
Recent Findings
Recent prospective studies have demonstrated encouraging initial results indicating the potential efficacy of metastasis-directed SBRT in the management of patients with oligometastatic disease. However, given potentially significant toxicities associated with metastasis-directed SBRT, additional data in the form of phase III randomized control trials are needed to define the role of SBRT in the management of patients with oligometastatic breast cancer; such studies are currently ongoing.
Summary
While current data are encouraging, additional data are required to determine the benefit of SBRT in patients with oligometastatic breast cancer. Physicians opting to treat patients with metastasis-directed SBRT should ideally do so on protocol.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
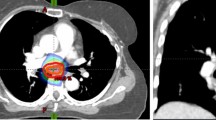
Radiation therapy plays a critical role in the management of patients with early-stage and locally advanced breast cancer. Adjuvant radiation following surgical management provides a well-established locoregional control, and in many cases, mortality, and benefit [1,2,3,4,5,6,7]. Among patients with metastatic breast cancer, radiation therapy is an effective means of palliating symptomatic locoregional [8] and distant disease [9, 10]. While radiation therapy has a proven benefit in the palliation of patients with symptomatic metastases, significant interest has been generated in its potential as a definitive therapy for patients with low burden metastatic disease (oligometastatic). Technological advances in radiation therapy have resulted in stereotactic body radiation therapy (SBRT) (also commonly referred to as stereotactic ablative radiotherapy (SABR)), which describes the conformal delivery of high doses of radiation in few fractions. The advent of SBRT combined with the hope that radiation therapy could provide benefit, beyond symptom relief, to patients with metastatic breast cancer has resulted in the widespread use of metastasis-directed radiation therapy in patients with low-volume metastatic disease [11].
While the concept of using local therapy to prolong the disease-free interval or even potentially cure breast cancer patients with few metastases is enticing, the evidence and potential toxicities of this therapy need to be understood in order to ensure that risks and benefits are adequately weighed. This article aims to review the natural history of oligometastatic breast cancer along with the role of radiation therapy, its management, potential toxicities associated with treatment, and future directions in this area.
A Brief History of Oligometastatic Breast Cancer
Despite significant advances in the management of patients with metastatic breast cancer, long-term cure remains rare among patients with disseminated disease. A population-based analysis of over 1500 patients with metastatic breast cancer treated with doxorubicin- and anthracycline-based chemotherapy demonstrated a sustained complete response in 3.1% at 5 years with 1.6% remaining free of disease at 15 years [12]. As a result, substantial efforts have been made to better understand the natural history of metastatic breast cancer such that its management can be optimized. Halsted originally proposed that metastatic progression occurs in an orderly fashion in which the primary breast tumor first spreads regionally to the draining lymph nodes, where tumor cells accumulate until capacity in the lymph node is reached resulting in cells spilling into the next echelon of draining lymph nodes [13]. Halsted’s model of orderly metastatic progression bolstered the idea that disease control could be achieved through sufficiently aggressive local therapy; this idea was subsequently challenged by the theory that breast cancer metastasizes distantly early in its natural history, which was most famously articulated by Fisher. Fisher’s model of metastatic progression postulated that breast cancer is typically already disseminated at the time of diagnosis, thus eschewing the importance of local therapy in favor of systemic therapy [14]. These theories were subsequently reconciled by Hellman who proposed the spectrum hypothesis postulating that breast cancer can be locoregionally confined or disseminated at time of presentation and that initially locoregionally confined disease may or may not subsequently progress distantly [15]. Shortly thereafter, this model was refined by Hellman and Weichselbaum who proposed the existence of an oligometastatic state in which patients present with a limited amount of disease that has metastasized distantly, but is unlikely to progress rapidly [16].
Since the oligometastatic state was originally proposed by Hellman and Weichselbaum, there has been significant interest in refining the definition of oligometastatic disease and determining optimal methods for detection and management of this population. Although the criteria under which a patient may be considered to have oligometastatic disease has historically varied across the literature, recent consensus guidelines use the term to refer to patients with 1–5 metastases, all of which are amenable to metastasis-directed therapy [17•, 18]. Beyond the number and location of metastases, volume of metastatic disease and rate of metastatic progression have been demonstrated to play an important role in differentiating patients with disease that has metastasized distantly, but is unlikely to progress rapidly versus those who are likely to progress rapidly with polymetastatic disease [16, 19]. Moreover, given the wide variety of clinical scenarios in which a patient may have a low number/volume of metastases that are not progressing rapidly, a consensus classification system for patients with oligometastatic disease has been developed based on the following factors: (1) Whether or not the patient had polymetastatic disease prior to diagnosis of the oligometastatic state (induced oligometastatic disease) or not (genuine oligometastatic disease), (2) among those with genuine oligometastatic disease whether this represents the patient’s initial presentation with oligometastatic disease (de novo oligometastatic disease) or not (repeat oligometastatic disease), (3) among those with de novo oligometastatic disease whether the diagnosis of oligometastatic disease occurred ≤ 6 months (synchronous oligometastatic disease) or > 6 months (metachronous oligometastatic disease) following the diagnosis of the primary cancer, (4) among those with metachronous oligometastatic disease whether oligometastases occur on systemic therapy (metachronous oligoprogressive disease) or off of systemic therapy (metachronous oligorecurrent disease), and (5) among those with repeat/induced oligometastatic disease whether their oligometastatic disease is stable (repeat/induced oligopersistent disease) or progressing (repeat/induced oligoprogressive disease) on systemic therapy [17•].
The frequency of oligometastatic disease among patients with metastatic breast cancer remains uncertain, though a review of several first-line systemic therapy trials for patients with metastatic breast cancer found that approximately 50% of enrolled patients initially had two or fewer metastatic sites and up to 75% had four or fewer [18]. Moreover, within a population of women with recurrent disease following definitive treatment for early-stage or locally advanced breast cancer, greater than 25% of patients had 5 or fewer metastases at time of progression [20]. As a result, improved delineation of the optimal management of oligometastatic disease could have important implications for many patients with metastatic breast cancer.
Historical Role of Local Therapy in the Management of Oligometastatic Breast Cancer
Given the inherent limited extent of disease among patients with oligometastatic cancer, the use of local therapy in this population is of significant interest; however, the idea of treating patients with limited metastatic disease with local therapy is by no means new. Weinlechner initially reported the results of a pulmonary metastasectomy following the resection of a chest wall sarcoma in 1882 [21]. Since that time, surgical resection of metastases in patients with low-volume metastatic breast cancer has been reported to be associated with durable long-term control in a significant number of patients [22,23,24,25]. For example, in a cohort of 467 breast cancer patients with pulmonary metastasis treated with metastasectomy between 1960 and 1994, 15-year overall survival was 18% [26]. A subsequent review demonstrated similar findings among other retrospective studies of pulmonary metastasectomy in patient with breast cancer; in line with the oligometastatic paradigm, the majority of long-term survivors in these studies had a solitary pulmonary metastasis [27]. It is also important to note that the reported experience of favorable outcomes following metastasectomy is not limited to pulmonary metastases, with similar results being achieved following resection of distant metastases in other organs and 5-year overall survivals of nearly 40% achieved [27,28,29,30,31,32]. While the available retrospective data has demonstrated encouraging long-term results in breast cancer patients with low-volume metastatic disease treated with metastasectomy, many patients with metastatic breast cancer are not able to undergo metastasectomy as a result of their medical comorbidities and/or disease that is not amenable to resection, resulting in the search for other effective local therapy options. This need combined with advent of SBRT, which allows patients to be treated with precisely delivered, high dose radiation therapy in few fractions of treatment, has made radiation therapy an attractive potential option for metastasis-directed therapy.
Efficacy of SBRT as Metastasis-Directed Therapy
Given its non-invasive nature and relative convenience, SBRT is viewed by many as an attractive potential local therapy option in patients with low-burden metastatic disease. Although local control following SBRT is generally accepted to be quite high, this is often difficult to assess given frequent post-treatment changes [33] and lack of standardized criteria for response evaluation following SBRT; response evaluation criteria in solid tumors (RECIST), which is used to judge objective tumor response rates following systemic therapy, has been applied to patients receiving SBRT to gauge local control, as has PET/CT with variable outcomes [34,35,36,37,38,39].
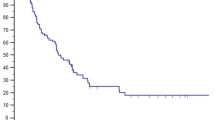
Although the majority of the available literature examining the role of SBRT to metastatic disease is limited by relatively short-term follow-up, there are emerging data indicating that like patients who undergo metastasectomy, patients who are treated with SBRT can experience durable control. The long-term outcomes of a prospective phase II study of 48 women with metastatic breast cancer with 5 or fewer extracranial metastases were recently reported with durable progression-free survival achieved in a significant number of patients. Outcomes in this study were particularly impressive in the subgroup of patients with only osseous metastases, in whom 10-year freedom from widespread progression and overall survival were 67% and 75%, respectively [40•]. While the results of this and similar series examining the role of local therapy in patients with oligometastatic disease are undoubtedly encouraging given historically poor long-term sustained response in patients with metastatic disease treated with systemic therapy alone, the non-randomized nature of these studies raises the question of whether the favorable outcome of these patients is the result of metastasis-directed therapy or merely a by-product of favorable outcomes within the oligometastatic population.
In order to address the question of whether oligometastatic disease is merely a prognostic factor in women with metastatic breast cancer or truly predictive and amenable to improved outcomes with local therapy, randomized data are needed. While randomized data in this area remain scarce, this is beginning to change. The results of SABR-COMET, a phase IIR screening trial, which randomized 99 patients with a controlled primary tumor > 3 months from definitive therapy and 5 or fewer distant metastases (n = 92 with 1–3 metastases, n = 7 with 4–5 metastases) to SBRT or standard of care (SOC) therapy in a 2:1 ratio have been published and recently updated with encouraging long-term results [41••, 42••]. With a median follow-up of 51 months, 5-year progression-free survival was not reached in the SOC arm, but was 17% in patients treated with SBRT (p = 0.001). Moreover, 5-year overall survival was significantly higher in patients treated with SBRT at 42%, compared with 18% in patients treated with SOC therapy alone (p = 0.006) [42••]. While the results of SABR-COMET are undoubtedly exciting, several caveats should be considered in its interpretation, the first of which is its intent as a phase II screening trial. Phase II screening trials are designed to determine whether larger, confirmatory studies should be performed to investigate a hypothesis and use an intentionally permissive p value in order to increase the likelihood that potentially significant outcomes are identified for further testing [43]. Thus, while the study’s finding of a clinically significant improvement in progression-free and overall survival with the addition of SBRT to SOC therapy met statistical significance under the pre-determined threshold of p < 0.20, this design significantly increases the likelihood of incorrectly rejecting a true null hypothesis (i.e., a type I error) and therefore requires confirmation in a phase III trial. Additionally, despite impressive progression-free and overall survival, objective response rates by RECIST were relatively low; however, as discussed by the authors and noted previously, frequent post-treatment changes following SBRT may confound assessment of this [33]. Beyond these factors, imbalances between the SBRT and SOC arms should also be considered when interpreting the results of SABR-COMET. For example, while the proportion of patients with primary breast cancer was relatively similar between the SBRT and SOC arm at 20% and 15%, respectively, other favorable histologies, such as prostate cancer, were significantly more common among patients treated with SBRT (21%) compared with those treated with SOC therapy (6%) [41••, 44]. It should be noted that upon post hoc sensitivity analysis excluding prostate cancer patients, the benefit in overall survival with the addition of SBRT was diminished, though still significant at 5 years (33% vs 16%, p = 0.085) [42••]; however, given the post hoc nature of this analysis, the conclusions that may be derived from this result are not entirely clear. Moreover, attempts to balance the distribution of histologies between groups do not account for the variety of histologies within each group. Given the heterogeneity of the biological behavior of metastatic disease among histologies, it is unclear whether the improved outcomes seen in SABR-COMET are generalizable to all patients with oligometastatic disease or driven by select histologies.
On the whole, the results of SABR-COMET are encouraging and bolster the results of smaller, disease-specific, phase II studies that demonstrate progression-free survival benefits among patients treated with SBRT to low-volume metastatic disease [45•, 46•, 47•, 48•]. However, unlike these smaller, disease-specific, phase II studies, in which SBRT was well-tolerated with minimal toxicity and no grade 4–5 events, toxicity among patients treated on SABR-COMET was non-trivial.
SBRT-Related Toxicity
Given that the benefit of metastasis-directed SBRT in patients with oligometastatic breast cancer remains uncertain at this point, the risks of such treatment must be carefully assessed in the event that it is to be utilized. On SABR-COMET, treatment-related grade 2 or higher adverse events was significantly more common among patients treated with SBRT (29%) compared with those treated with SOC therapy only (9%). Moreover, 3 patients (5%) treated with SBRT experienced grade 5 treatment-related adverse events (one patient with radiation pneumonitis, one patient with a post-treatment pulmonary abscess, and one patient with a subdural hemorrhage after surgical repair of an SBRT-related perforated gastric ulcer), while no patients in the SOC arm experienced treatment-related death [41••]. The toxicity seen among patients treated with metastasis-directed SBRT on SABR-COMET gives reason for significant contemplation regarding the role of SBRT in the oligometastatic population; however, additional emerging data suggests that with rigorous quality control, metastasis-directed SBRT can be performed safely. NRG-BR001, a phase I trial which evaluated the safety of multisite SBRT, enrolled 42 patients with oligometastatic breast, prostate, and non-small cell lung cancer. On BR001, 8 grade 3 adverse events, which occurred 125–556 days from the start of SBRT in 7 patients, were deemed to likely be related to protocol therapy; however, no protocol-defined dose-limiting toxicities were observed with 100% quality assurance compliance [49•].
What Is the Current Role of Metastasis-Directed SBRT in the Management of Patients with Oligometastatic Breast Cancer?
Although the data supporting the efficacy of metastasis-directed SBRT in patients with oligometastatic disease has grown considerably in recent years, many caveats exist limiting its application to patients with oligometastatic breast cancer at this time. Of the aforementioned prospective, phase II trials that support the role of metastasis-directed SBRT in patients with oligometastatic disease only SABR-COMET included patients with breast cancer. Beyond, the aforementioned concerns about overstating the implications of SABR-COMET given its phase II screening design, lack of stratification by histology is a significant issue which further limits the ability to infer that metastasis-directed SBRT benefits oligometastatic breast cancer patients. Moreover, even among women with metastatic breast cancer, outcomes vary widely based upon a number of clinical and pathologic factors [12, 50, 51] that need to be considered when evaluating the data supporting the role of metastasis-directed SBRT in patients with oligometastatic breast cancer.
In line with the oligometastatic paradigm, the prognostic importance of metastatic burden in patients with metastatic breast cancer has been demonstrated repeatedly. Notably, within a large cohort of women treated with anthracycline-based chemotherapy for metastatic breast cancer, women with 5 or fewer metastases had a median survival of 146 weeks, which was significantly longer than median survivals of 96 weeks, 80 weeks, and 62 weeks, in women with 6–12, 13–20, and greater than 20 metastases, respectively [15]. Similarly, within a population of women with recurrent disease following definitive treatment for early-stage or locally advanced breast cancer, in which median time to distant recurrence was approximately 30 months, median survival following recurrence was significantly longer in patients with limited metastatic recurrence compared with those with widespread failure.. Within this population, patients with 1–5 metastases had a median survival of 108 months and a 5-year actuarial survival of 60% compared with a median survival of 22 months and a 5-year actuarial survival of 12% in patients with more than 5 metastases at time of progression [20]. It is also important to note that although recent consensus guidelines describe oligometastatic patients as having 1–5 metastases [17•], it is not entirely clear whether patients within this population vary based upon number of metastases. For example, on SABR-COMET, although patients with 1–5 metastases were eligible for enrollment, the vast majority of patients had 1–3 metastases (n = 92 with 1–3 metastases, n = 7 with 4–5 metastases) [42••]. Moreover, specific to oligometastatic breast cancer, there is data supporting the prognostic importance of a solitary metastasis compared with multiple metastases [40•, 41••, 52] further supporting the importance of metastatic burden in patients with metastatic breast cancer.
Additionally, oligometastatic disease can occur under a variety of different clinical scenarios, as previously described [17•]. The prognostic significance of oligometastatic disease may vary significantly among these different scenarios and should be considered when attempting to determine the role of metastasis-directed SBRT in a patient with oligometastatic breast cancer. The majority of the data demonstrating a benefit with metastasis-directed SBRT is limited to patients with de novo oligometastatic disease, in whom the oligometastatic state has typically been demonstrated to be the most important prognostically. Among patients with de novo metastatic disease, outcomes may vary significantly depending upon the timing of their presentation with metastatic disease [53, 54]. In a series of over 3500 women with metastatic breast cancer treated between 1992 and 2007, patients with synchronous metastatic disease had a median survival of 39 months, which was significantly longer than the median survival of patients with metachronous disease at 27 months [53]. Among those with metachronous disease, prolonged disease-free survival was associated with improved outcomes and within the subpopulation of patients with disease-free intervals greater than 5 years, median survival did not differ significantly from the cohort of patients with synchronous metastatic disease. Although the majority of the data investigating outcomes in oligometastatic breast cancer exists in patients with de novo disease, oligoprogression has been demonstrated to be important prognostically a well. Recently presented retrospective data from a cohort of over 1000 women with metastatic breast cancer demonstrated an oligoprogression rate of approximately 30% [55]. Within this cohort, oligoprogression was twice as common among HER2+ patients compared with TNBC and HR+/HER2− patients. Moreover, the oligoprogressive population experienced significantly better 3-year overall survival (72%) compared with the diffusely progressive population (37%) [55] suggesting the prognostic importance of oligometastatic disease beyond the de novo setting.
The site of metastasis is another important consideration in patients with oligometastatic breast cancer. While the location of a patient’s metastatic disease directly impacts the risk of adverse events associated with metastasis-directed SBRT, site of metastasis has also been demonstrated to be important prognostically. As previously discussed, in a prospective phase II study of 48 women with oligometastatic breast cancer treated with SBRT, patients with bone-only metastases experienced significantly better progression-free and overall survival compared with those with non-bone-only disease [40•]. While the cohort of patients with bone-only disease in this study was small, other studies have previously reported similar findings [56].
Beyond factors specific to patients with oligometastatic disease, a number of clinical factors such as age and performance status have been demonstrated to have important prognostic implications in patients with metastatic breast cancer [57]. Moreover, receptor status is not only profoundly important prognostically among metastatic breast cancer patients but also is the primary factor that determines systemic therapy options [12, 50, 51, 58,59,60]. Given the significant heterogeneity that exists not only among histologies but also within the population of patients with oligometastatic breast cancer, data that takes into account these potential covariates is needed in order to better establish the role of metastasis-directed SBRT.
Although preliminary data supporting metastasis-directed SBRT in patients with oligometastatic disease is indeed encouraging, the benefit of this remains uncertain. Given uncertain benefit combined with non-trivial rates of toxicity, further validation in the form of phase III randomized controlled trials should be obtained prior to widespread adoption of metastasis-directed SBRT in oligometastatic breast cancer patients. Prospective validation of the role of metastasis-directed therapy is especially important in oligometastatic breast cancer given the aforementioned clinical and pathologic factors, which result in significant heterogeneity within this population and have the potential to confound the results of studies examining metastasis-directed SBRT if not appropriately taken into account. Despite this, metastasis-directed SBRT has already become frequently utilized for patients with oligometastatic disease in many clinics. In an international survey of over 1000 radiation oncologists, 61% of respondents stated that they routinely use SBRT to treat patients with 3 or fewer metastases, with 59% of those who do use SBRT in this setting stating that they plan to begin doing so in the near future [11]. The widespread utilization of metastasis-directed SBRT combined with the aforementioned questions that remain regarding the efficacy and safety of metastasis-directed SBRT in oligometastatic breast cancer patients has led some to speculate that forthcoming data could potentially result in medical reversal depending upon the results of ongoing clinical trials [61].
Future Directions in the Management of Oligometastatic Breast Cancer
First and foremost, evidence in the form of phase III randomized control trials is needed in order to definitively determine whether patients with oligometastatic disease benefit from metastasis-directed SBRT. Several ongoing phase III randomized control trials investigating the role of metastasis-directed therapy are enrolling patients with oligometastatic breast cancer with two ongoing trials that are restricted to breast cancer only, with as shown in Table 1. NRG-BR002 (NCT02364557) randomizes patients with locally controlled metastatic breast cancer with 1–4 metastases, all of which are amenable to locally therapy, to SOC systemic therapy versus SOC systemic therapy in addition to ablative therapy (either surgery or SBRT) to all sites of metastasis. Given the aforementioned heterogeneity within the oligometastatic breast cancer population, it is an important note that the trial is stratified by number of metastases (1 vs. > 1) as well as receptor status and first-line systemic therapy (yes versus no). Similarly, STEREO-SEIN (NCT02089100) randomizes patients with de novo oligometastatic breast cancer with 1–5 metastases to SOC systemic therapy with or without SBRT to all sites of metastasis. These and potentially additional randomized trials will be crucial in further defining the role of metastasis-directed local therapy in patients with oligometastatic breast cancer.
Beyond the need for validation in the form of phase III randomized controlled trials, better means of identifying patients with oligometastatic disease are needed. Inherent to the oligometastatic paradigm is the idea that some patients with metastatic disease have a limited amount of disease that has metastasized distantly, but is unlikely to progress rapidly to a polymetastatic state. Beyond the presented clinical data, molecular and genomic data supporting the presence of an oligometastatic state continue to grow [62,63,64,65,66]. As the understanding of the biologic principles underling metastasis continues to evolve, there is increasing potential for the identification of biomarkers associated with the oligometastatic state. Currently, microRNA expression profiles associated the development of oligometastatic disease have been identified to be unique from those associated with development of polymetastatic disease [19, 67]. Pending further prospective validation, these and other biomarkers have the potential to differentiate patients with metastatic breast cancer who are unlikely to progress distantly rapidly and therefore are more likely to benefit from local therapy from those who are likely to quickly develop polymetastatic disease and in turn are less likely to benefit from local therapy. Circulating tumor cells have also been demonstrated to be of prognostic importance in patients with metastatic breast cancer and have the potential to serve as a biomarker for response to treatment following SBRT [68].
Conclusion
Given its non-invasive nature and relative convenience, SBRT has the potential to be an attractive option for metastasis-directed therapy in patients with oligometastatic breast cancer. While small prospective studies have demonstrated the potential benefit of SBRT in patients with oligometastatic disease [40•, 41••, 42••], additional evidence in the form of phase III randomized control trials is needed in order to definitively determine whether patients with oligometastatic disease benefit from metastasis-directed SBRT and specifically which, if any, oligometastatic breast cancer patients benefit from metastasis-directed SBRT. Table 1 lists the currently ongoing phase III trials open to patients with metastatic breast cancer that are investigating the role of metastasis-directed therapy. Ideally, physicians opting to treat patients with oligometastatic breast cancer using metastasis-directed SBRT should do so on protocol. When not possible, clinicians should carefully weigh the uncertain potential benefits of metastasis-directed SBRT against the risk of toxicity.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Early Breast Cancer Trialists' Collaborative G. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365(9472):1687–717. https://doi.org/10.1016/S0140-6736(05)66544-0.
Early Breast Cancer Trialists’ Collaborative G, Darby S, McGale P, Correa C, Taylor C, Arriagada R, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011;378(9804):1707–16. https://doi.org/10.1016/S0140-6736(11)61629-2.
Ebctcg MP, Taylor C, Correa C, Cutter D, Duane F, et al. Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet. 2014;383(9935):2127–35. https://doi.org/10.1016/S0140-6736(14)60488-8.
Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347(16):1233–41. https://doi.org/10.1056/NEJMoa022152.
Overgaard M, Hansen PS, Overgaard J, Rose C, Andersson M, Bach F, et al. Postoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. Danish Breast Cancer Cooperative Group 82b Trial. N Engl J Med. 1997;337(14):949–55. https://doi.org/10.1056/NEJM199710023371401.
Overgaard M, Jensen MB, Overgaard J, Hansen PS, Rose C, Andersson M, et al. Postoperative radiotherapy in high-risk postmenopausal breast-cancer patients given adjuvant tamoxifen: Danish Breast Cancer Cooperative Group DBCG 82c randomised trial. Lancet. 1999;353(9165):1641–8. https://doi.org/10.1016/S0140-6736(98)09201-0.
Ragaz J, Jackson SM, Le N, Plenderleith IH, Spinelli JJ, Basco VE, et al. Adjuvant radiotherapy and chemotherapy in node-positive premenopausal women with breast cancer. N Engl J Med. 1997;337(14):956–62. https://doi.org/10.1056/NEJM199710023371402.
Yee C, Alayed Y, Drost L, Karam I, Vesprini D, McCann C, et al. Radiotherapy for patients with unresected locally advanced breast cancer. Ann Palliat Med. 2018;7(4):373–84. https://doi.org/10.21037/apm.2018.05.13.
Chow E, Harris K, Fan G, Tsao M, Sze WM. Palliative radiotherapy trials for bone metastases: a systematic review. J Clin Oncol. 2007;25(11):1423–36. https://doi.org/10.1200/JCO.2006.09.5281.
Dennis K, Makhani L, Zeng L, Lam H, Chow E. Single fraction conventional external beam radiation therapy for bone metastases: a systematic review of randomised controlled trials. Radiother Oncol. 2013;106(1):5–14. https://doi.org/10.1016/j.radonc.2012.12.009.
Lewis SL, Porceddu S, Nakamura N, Palma DA, Lo SS, Hoskin P, et al. Definitive stereotactic body radiotherapy (SBRT) for extracranial oligometastases: an international survey of >1000 radiation oncologists. Am J Clin Oncol. 2017;40(4):418–22. https://doi.org/10.1097/COC.0000000000000169.
Greenberg PA, Hortobagyi GN, Smith TL, Ziegler LD, Frye DK, Buzdar AU. Long-term follow-up of patients with complete remission following combination chemotherapy for metastatic breast cancer. J Clin Oncol. 1996;14(8):2197–205. https://doi.org/10.1200/JCO.1996.14.8.2197.
Halsted WS. I. The results of radical operations for the cure of carcinoma of the breast. Ann Surg. 1907;46(1):1–19. https://doi.org/10.1097/00000658-190707000-00001.
Fisher B. Laboratory and clinical research in breast cancer--a personal adventure: the David A. Karnofsky memorial lecture. Cancer Res. 1980;40(11):3863–74.
Karnofsky HS, Lecture M. Natural history of small breast cancers. J Clin Oncol. 1994;12(10):2229–34. https://doi.org/10.1200/JCO.1994.12.10.2229.
Hellman S, Weichselbaum RR. Oligometastases. J Clin Oncol. 1995;13(1):8–10. https://doi.org/10.1200/JCO.1995.13.1.8.
• Guckenberger M, Lievens Y, Bouma AB, Collette L, Dekker A, de Souza NM, et al. Characterisation and classification of oligometastatic disease: a European Society for Radiotherapy and Oncology and European Organisation for Research and Treatment of Cancer consensus recommendation. Lancet Oncol. 2020;21(1):e18–28. https://doi.org/10.1016/S1470-2045(19)30718-1Recently published ESTRO/EORTC consensus guidelines for the classification of different clinical states falling under the umbrella term “oligometastatic disease.”.
Salama JK, Chmura SJ. Surgery or ablative radiotherapy for breast cancer oligometastases. Am Soc Clin Oncol Educ Book. 2015:e8–15. doi:https://doi.org/10.14694/EdBook_AM.2015.35.e8.
Lussier YA, Khodarev NN, Regan K, Corbin K, Li H, Ganai S, et al. Oligo- and polymetastatic progression in lung metastasis(es) patients is associated with specific microRNAs. PLoS One. 2012;7(12):e50141. https://doi.org/10.1371/journal.pone.0050141.
Dorn PL, Meriwether A, LeMieux M, Weichselbaum RR, Chmura SJ, Hasan Y. Patterns of distant failure and progression in breast cancer: implications for the treatment of oligometastatic disease. Int J Radiat Oncol Biol Phys. 2011;81(2):S643.
van Dongen JA, van Slooten EA. The surgical treatment of pulmonary metastases. Cancer Treat Rev. 1978;5(1):29–48. https://doi.org/10.1016/s0305-7372(78)80004-8.
McDonald ML, Deschamps C, Ilstrup DM, Allen MS, Trastek VF, Pairolero PC. Pulmonary resection for metastatic breast cancer. Ann Thorac Surg. 1994;58(6):1599–602. https://doi.org/10.1016/0003-4975(94)91639-x.
Meimarakis G, Ruttinger D, Stemmler J, Crispin A, Weidenhagen R, Angele M, et al. Prolonged overall survival after pulmonary metastasectomy in patients with breast cancer. Ann Thorac Surg. 2013;95(4):1170–80. https://doi.org/10.1016/j.athoracsur.2012.11.043.
Planchard D, Soria JC, Michiels S, Grunenwald D, Validire P, Caliandro R, et al. Uncertain benefit from surgery in patients with lung metastases from breast carcinoma. Cancer. 2004;100(1):28–35. https://doi.org/10.1002/cncr.11881.
Staren ED, Salerno C, Rongione A, Witt TR, Faber LP. Pulmonary resection for metastatic breast cancer. Arch Surg. 1992;127(11):1282–4. https://doi.org/10.1001/archsurg.1992.01420110024006.
Friedel G, Pastorino U, Ginsberg RJ, Goldstraw P, Johnston M, Pass H, et al. Results of lung metastasectomy from breast cancer: prognostic criteria on the basis of 467 cases of the International Registry of Lung Metastases. Eur J Cardiothorac Surg. 2002;22(3):335–44. https://doi.org/10.1016/s1010-7940(02)00331-7.
Pagani O, Senkus E, Wood W, Colleoni M, Cufer T, Kyriakides S, et al. International guidelines for management of metastatic breast cancer: can metastatic breast cancer be cured? J Natl Cancer Inst. 2010;102(7):456–63. https://doi.org/10.1093/jnci/djq029.
Abbott DE, Cantor SB, Hu CY, Aloia TA, You YN, Nguyen S, et al. Optimizing clinical and economic outcomes of surgical therapy for patients with colorectal cancer and synchronous liver metastases. J Am Coll Surg. 2012;215(2):262–70. https://doi.org/10.1016/j.jamcollsurg.2012.03.021.
Pawlik TM, Izzo F, Cohen DS, Morris JS, Curley SA. Combined resection and radiofrequency ablation for advanced hepatic malignancies: results in 172 patients. Ann Surg Oncol. 2003;10(9):1059–69. https://doi.org/10.1245/aso.2003.03.026.
Pocard M, Pouillart P, Asselain B, Falcou MC, Salmon RJ. Hepatic resection for breast cancer metastases: results and prognosis (65 cases). Ann Chir. 2001;126(5):413–20. https://doi.org/10.1016/s0003-3944(01)00526-0.
Sadot E, Lee SY, Sofocleous CT, Solomon SB, Gonen M, Kingham TP, et al. Hepatic resection or ablation for isolated breast cancer liver metastasis: a case-control study with comparison to medically treated patients. Ann Surg. 2016;264(1):147–54. https://doi.org/10.1097/SLA.0000000000001371.
Yoshimoto M, Tada T, Saito M, Takahashi K, Uchida Y, Kasumi F. Surgical treatment of hepatic metastases from breast cancer. Breast Cancer Res Treat. 2000;59(2):177–84. https://doi.org/10.1023/a:1006398401352.
Huang K, Dahele M, Senan S, Guckenburger M, Rodrigues G, Ward A, et al. Radiographic changes after lung stereotactic ablative radiotherapy (SABR) -- can we distinguish fibrosis from recurrence? A systematic review of the literature. Pract Radiat Oncol. 2013;3(2 Suppl 1):S11–2. https://doi.org/10.1016/j.prro.2013.01.039.
Arnett ALH, Mou B, Owen D, Park SS, Nelson K, Hallemeier CL, et al. Long-term clinical outcomes and safety profile of SBRT for centrally located NSCLC. Adv Radiat Oncol. 2019;4(2):422–8. https://doi.org/10.1016/j.adro.2019.01.002.
Mohammed N, Grills IS, Wong CY, Galerani AP, Chao K, Welsh R, et al. Radiographic and metabolic response rates following image-guided stereotactic radiotherapy for lung tumors. Radiother Oncol. 2011;99(1):18–22. https://doi.org/10.1016/j.radonc.2011.03.003.
Solanki AA, Weichselbaum RR, Appelbaum D, Farrey K, Yenice KM, Chmura SJ, et al. The utility of FDG-PET for assessing outcomes in oligometastatic cancer patients treated with stereotactic body radiotherapy: a cohort study. Radiat Oncol. 2012;7:216. https://doi.org/10.1186/1748-717X-7-216.
Takenaka R, Shibamoto Y, Miyakawa A, Hashizume C, Baba F. The fate of residual tumor masses that persist after stereotactic body radiotherapy for solitary lung nodules: will they recur? Clin Lung Cancer. 2016;17(5):406–11. https://doi.org/10.1016/j.cllc.2015.12.003.
Taremi M, Hope A, Dahele M, Pearson S, Fung S, Purdie T, et al. Stereotactic body radiotherapy for medically inoperable lung cancer: prospective, single-center study of 108 consecutive patients. Int J Radiat Oncol Biol Phys. 2012;82(2):967–73. https://doi.org/10.1016/j.ijrobp.2010.12.039.
Timmerman R, Paulus R, Galvin J, Michalski J, Straube W, Bradley J, et al. Stereotactic body radiation therapy for inoperable early stage lung cancer. JAMA. 2010;303(11):1070–6. https://doi.org/10.1001/jama.2010.261.
• Milano MT, Katz AW, Zhang H, Huggins CF, Aujla KS, Okunieff P. Oligometastatic breast cancer treated with hypofractionated stereotactic radiotherapy: some patients survive longer than a decade. Radiother Oncol. 2019;131:45–51. https://doi.org/10.1016/j.radonc.2018.11.022Prospective non-randomized phase II study of women with oligometastatic breast cancer treated with metastasis-directed SBRT demonstrating durable progression-free and overall survival.
•• Palma DA, Olson R, Harrow S, Gaede S, Louie AV, Haasbeek C, et al. Stereotactic ablative radiotherapy versus standard of care palliative treatment in patients with oligometastatic cancers (SABR-COMET): a randomised, phase 2, open-label trial. Lancet. 2019;393(10185):2051–8. https://doi.org/10.1016/S0140-6736(18)32487-5SABR-COMET – Prospective, randomized phase II screening trial examining the role of metastasis-directed SBRT in patients with oligometastatic disease across histologies. Metastasis-directed SBRT was associated with an improvement in overall survival in this phase II screening trial.
•• Palma DA, Olson R, Harrow S, Gaede S, Louie AV, Haasbeek C et al. Stereotactic ablative radiotherapy for the comprehensive treatment of oligometastatic cancers: long-term results of the SABR-COMET phase II randomized trial. J Clin Oncol. 2020:JCO2000818. doi:https://doi.org/10.1200/JCO.20.00818. Recently published 5-year update of SABR-COMET. With extended follow-up the overall survival benefit associated with metastasis-directed SBRT was noted to be durable and to increase in magnitude.
Rubinstein LV, Korn EL, Freidlin B, Hunsberger S, Ivy SP, Smith MA. Design issues of randomized phase II trials and a proposal for phase II screening trials. J Clin Oncol. 2005;23(28):7199–206. https://doi.org/10.1200/JCO.2005.01.149.
Hong JC, Ayala-Peacock DN, Lee J, Blackstock AW, Okunieff P, Sung MW, et al. Classification for long-term survival in oligometastatic patients treated with ablative radiotherapy: a multi-institutional pooled analysis. PLoS One. 2018;13(4):e0195149. https://doi.org/10.1371/journal.pone.0195149.
• Gomez DR, Tang C, Zhang J, Blumenschein GR Jr, Hernandez M, Lee JJ, et al. Local consolidative therapy vs. maintenance therapy or observation for patients with oligometastatic non-small-cell lung cancer: long-term results of a multi-institutional, phase II, randomized study. J Clin Oncol. 2019;37(18):1558–65. https://doi.org/10.1200/JCO.19.00201Prospective, randomized phase II trial evaluating the role of metastasis-directed SBRT in oligometastatic non-small cell lung cancer.
• Iyengar P, Wardak Z, Gerber DE, Tumati V, Ahn C, Hughes RS, et al. Consolidative radiotherapy for limited metastatic non-small-cell lung cancer: a phase 2 randomized clinical trial. JAMA Oncol. 2018;4(1):e173501. https://doi.org/10.1001/jamaoncol.2017.3501Prospective, randomized phase II trial evaluating the role of metastasis-directed SBRT in oligometastatic non-small cell lung cancer.
• Ost P, Reynders D, Decaestecker K, Fonteyne V, Lumen N, De Bruycker A, et al. Surveillance or metastasis-directed therapy for oligometastatic prostate cancer recurrence: a prospective, randomized, multicenter phase II trial. J Clin Oncol. 2018;36(5):446–53. https://doi.org/10.1200/JCO.2017.75.4853STOMP – prospective, randomized phase II trial evaluating the role of metastasis-directed SBRT in oligometastatic prostate cancer.
• Phillips R, Shi WY, Deek M, Radwan N, Lim SJ, Antonarakis ES, et al. Outcomes of observation vs stereotactic ablative radiation for oligometastatic prostate cancer: the ORIOLE phase 2 randomized clinical trial. JAMA Oncol. 2020. https://doi.org/10.1001/jamaoncol.2020.0147ORIOLE – prospective, randomized phase II trial evaluating the role of metastasis-directed SBRT in oligometastatic prostate cancer.
• Chmura SJ, Winter K, Salama JK, Robinson CG, Pisansky TM, Borges V, et al. Phase I trial of stereotactic body radiation therapy (SBRT) to multiple metastatic sites: a NRG oncology study. Int J Radiat Oncol Biol Phys. 2018;102(3):S68–S9. https://doi.org/10.1016/j.ijrobp.2018.06.187NRG-BR001 – phase I trial testing the hypothesis that multisite metastasis-directed SBRT could be safely delievered. SBRT was delievered to a median of three metastases with no protocol-defined dose-limiting toxicities.
Clark GM, Sledge GW Jr, Osborne CK, McGuire WL. Survival from first recurrence: relative importance of prognostic factors in 1,015 breast cancer patients. J Clin Oncol. 1987;5(1):55–61. https://doi.org/10.1200/JCO.1987.5.1.55.
Dawood S, Broglio K, Gonzalez-Angulo AM, Buzdar AU, Hortobagyi GN, Giordano SH. Trends in survival over the past two decades among white and black patients with newly diagnosed stage IV breast cancer. J Clin Oncol. 2008;26(30):4891–8. https://doi.org/10.1200/JCO.2007.14.1168.
Milano MT, Zhang H, Metcalfe SK, Muhs AG, Okunieff P. Oligometastatic breast cancer treated with curative-intent stereotactic body radiation therapy. Breast Cancer Res Treat. 2009;115(3):601–8. https://doi.org/10.1007/s10549-008-0157-4.
Dawood S, Broglio K, Ensor J, Hortobagyi GN, Giordano SH. Survival differences among women with de novo stage IV and relapsed breast cancer. Ann Oncol. 2010;21(11):2169–74. https://doi.org/10.1093/annonc/mdq220.
den Brok WD, Speers CH, Gondara L, Baxter E, Tyldesley SK, Lohrisch CA. Survival with metastatic breast cancer based on initial presentation, de novo versus relapsed. Breast Cancer Res Treat. 2017;161(3):549–56. https://doi.org/10.1007/s10549-016-4080-9.
Bazan JG, Holbrook A, Jhawar S, White JR. P4–12-03. Patterns of progression in metastatic breast cancer: does oligoprogression exist? San Antonio Breast Cancer Symposium. 2019.
Lobbezoo DJ, van Kampen RJ, Voogd AC, Dercksen MW, van den Berkmortel F, Smilde TJ, et al. Prognosis of metastatic breast cancer subtypes: the hormone receptor/HER2-positive subtype is associated with the most favorable outcome. Breast Cancer Res Treat. 2013;141(3):507–14. https://doi.org/10.1007/s10549-013-2711-y.
Yamamoto N, Katsumata N, Watanabe T, Omuro Y, Ando M, Narabayashi M, et al. Clinical characteristics of patients with metastatic breast cancer with complete remission following systemic treatment. Jpn J Clin Oncol. 1998;28(6):368–73. https://doi.org/10.1093/jjco/28.6.368.
Hortobagyi GN, Smith TL, Legha SS, Swenerton KD, Gehan EA, Yap HY, et al. Multivariate analysis of prognostic factors in metastatic breast cancer. J Clin Oncol. 1983;1(12):776–86. https://doi.org/10.1200/JCO.1983.1.12.776.
Emi Y, Kitamura K, Shikada Y, Kakeji Y, Takahashi I, Tsutsui S. Metastatic breast cancer with HER2/neu-positive cells tends to have a morbid prognosis. Surgery. 2002;131(1 Suppl):S217–21. https://doi.org/10.1067/msy.2002.119580.
Ismail-Khan R, Bui MM. A review of triple-negative breast cancer. Cancer Control. 2010;17(3):173–6. https://doi.org/10.1177/107327481001700305.
Drazer MW, Salama JK, Hahn OM, Weichselbaum RR, Chmura SJ. Stereotactic body radiotherapy for oligometastatic breast cancer: a new standard of care, or a medical reversal in waiting? Expert Rev Anticancer Ther. 2016;16(6):625–32. https://doi.org/10.1080/14737140.2016.1178577.
Chiang AC, Massague J. Molecular basis of metastasis. N Engl J Med. 2008;359(26):2814–23. https://doi.org/10.1056/NEJMra0805239.
Gupta GP, Massague J. Cancer metastasis: building a framework. Cell. 2006;127(4):679–95. https://doi.org/10.1016/j.cell.2006.11.001.
Nguyen DX, Massague J. Genetic determinants of cancer metastasis. Nat Rev Genet. 2007;8(5):341–52. https://doi.org/10.1038/nrg2101.
Yachida S, Jones S, Bozic I, Antal T, Leary R, Fu B, et al. Distant metastasis occurs late during the genetic evolution of pancreatic cancer. Nature. 2010;467(7319):1114–7. https://doi.org/10.1038/nature09515.
Li Y, Tang ZY, Ye SL, Liu YK, Chen J, Xue Q, et al. Establishment of cell clones with different metastatic potential from the metastatic hepatocellular carcinoma cell line MHCC97. World J Gastroenterol. 2001;7(5):630–6. https://doi.org/10.3748/wjg.v7.i5.630.
Lussier YA, Xing HR, Salama JK, Khodarev NN, Huang Y, Zhang Q, et al. MicroRNA expression characterizes oligometastasis(es). PLoS One. 2011;6(12):e28650. https://doi.org/10.1371/journal.pone.0028650.
Cristofanilli M, Budd GT, Ellis MJ, Stopeck A, Matera J, Miller MC, et al. Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N Engl J Med. 2004;351(8):781–91. https://doi.org/10.1056/NEJMoa040766.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Turchan has nothing to disclose. Dr. Chmura reports personal fees from RefleXion Medical, other from Astellas Pharma, and grants from Merck and BMS outside the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors. All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Radiation Oncology
Rights and permissions
About this article
Cite this article
Turchan, W.T., Chmura, S.J. Radiation Therapy in the Management of Oligometastatic Breast Cancer: Current Evidence and Future Directions. Curr Breast Cancer Rep 12, 266–274 (2020). https://doi.org/10.1007/s12609-020-00383-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-020-00383-y