Abstract
This study evaluated the effects of simulated gastrointestinal conditions (SGIC) on combined potentially probiotic Limosilactobacillus fermentum 296 (~ 10 log CFU/mL), quercetin (QUE, 160 mg), and/or resveratrol (RES, 150 mg) as the bioactive components of novel nutraceuticals. Four different nutraceuticals were evaluated during exposure to SGIC and analyzed the plate counts and physiological status of L. fermentum 296, contents and bioaccessibility of QUE and RES, and antioxidant capacity. Nutraceuticals with QUE and RES had the highest plate counts (4.94 ± 0.32 log CFU/mL) and sizes of live cell subpopulations (28.40 ± 0.28%) of L. fermentum 296 after SGIC exposure. An index of injured cells (Gmean index, arbitrary unit defined as above 0.5) indicated that part of L. fermentum 296 cells could be entered the viable but nonculturable state when the nutraceuticals were exposed to gastric and intestinal conditions while maintaining vitality. The nutraceuticals maintained high contents (QUE ~ 29.17 ± 0.62 and RES ~ 23.05 mg/100 g) and bioaccessibility (QUE ~ 41.0 ± 0.09% and RES ~ 67.4 ± 0.17%) of QUE and RES, as well as high antioxidant capacity (ABTS assay ~ 88.18 ± 1.16% and DPPH assay 75.54 ± 0.65%) during SGIC exposure, which could be linked to the protective effects on L. fermentum 296 cells. The developed nutraceuticals could cross along the gastrointestinal tract with high concentrations of functioning potentially probiotic cells and bioavailable phenolic compounds to exert their beneficial impacts on consumer health, being an innovative strategy for the co-ingestion of these bioactive components.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Probiotics are live microorganisms capable of conferring a health benefit on the host when consumed in adequate doses [1]. These benefits are beyond gastrointestinal health and include improvements in immune and neurological functions [2, 3]. Probiotics must survive the adverse conditions encountered in the human gastrointestinal tract to reach and colonize the intestine and exert the claimed effects on the host [4]. Gastric acidity, bile acids, and digestive enzymes are among the adverse conditions found in the gastrointestinal tract that can damage the integrity of probiotic cells [5]. The combined ingestion of phenolic compounds, such as quercetin (QUE) and resveratrol (RES), has been cited as a strategy to maintain the viability of probiotics through gastrointestinal tract passage [6].
QUE and RES belong to the flavanols and stilbenes families, respectively, being found in various fruit and vegetables [7]. These phenolic compounds are commonly used as dietary supplements primarily due to their strong antioxidant capacity and associated anti-inflammatory and anticancer properties, and protection from cardiovascular and neurodegenerative diseases [8,9,10]. Additionally, QUE and RES have been shown to protect probiotic lactobacilli when challenged with low pH and high concentrations of bile salts in the human gastrointestinal tract, besides improving some in vitro properties related to their probiotic functionality [6].
Nutraceuticals are natural products that provide beneficial health effects, including disease prevention and treatment [11]. An early study showed that nutraceuticals were suitable vehicles for the co-ingestion of the potentially probiotic Limosilactobacillus fermentum 296, QUE, and/or RES. These formulations maintained high viable cell counts of L. fermentum 296, high contents of QUE and RES, and antioxidant capacity during long-term storage [12, 13], besides causing beneficial alterations in the composition and metabolic activity of human intestinal microbiota during in vitro colonic fermentation [14]. However, investigations on the capability of these nutraceuticals to maintain their bioactive components up to reaching the final part of the gastrointestinal tract and exert the expected functionality on the consumers’ health are still lacking.
This study has hypothesized that these novel nutraceuticals combining L. fermentum 296, QUE, and/or RES maintain high concentrations of their bioactive components and, consequently, the potential functionalities during exposure to human gastrointestinal tract conditions. To test this hypothesis, the effects of conditions mimicking the human gastrointestinal tract on the viable cell counts and physiological status of L. fermentum 296, the contents and bioaccessibility of QUE and RES, and the antioxidant capacity of these nutraceuticals were evaluated.
Material and Methods
Potentially Probiotic Strain and Preparation of Nutraceuticals
Limosilactobacillus fermentum 296 was isolated from strawberry pulp processing by-product composed of mashed seed, peel, and pulp remnants and characterized as a potential probiotic strain [15, 16], as well as a candidate for the prevention of diet-induced hypercholesterolemia and hypertriglyceridemia [17, 18]. L. fermentum 296 stocks were kept at − 20 °C in de Mann, Rogosa, and Sharpe (MRS) broth (HiMedia, Mumbai, India) with glycerol (20% v/v; Sigma-Aldrich, St. Louis, MA, USA). Previous to the use, the strain was anaerobically cultivated (AnaeroGen, Oxoid Anaerogen Anaerobic System, Hampshire, UK) in MRS broth (37 °C, 20–24 h), harvested (4000 × g, 10 min, 4 °C), and washed two times with sterile saline solution (NaCl 0.85 g/100 mL, 4000 × g, 10 min, 4 °C), and resuspended in sterile distilled water to obtain a cell suspension with an optical density reading (625 nm) of 2.0 and viable cell counts of approximately 10 log CFU/mL.
Freshly prepared suspensions of L. fermentum 296 (1 mL) were mixed with commercial fructooligosaccharides (FOS, 20% w/v; F8052, Sigma-Aldrich, St. Louis, MA, USA) [12, 14] as a cryoprotectant. The suspensions were frozen (− 80 °C, 24 h) and freeze-dried (vacuum pressure of < 138 μHG, freeze-drying rate of 1 mm/h, and temperature of − 55 °C ± 2 °C) for 40 h with a bench-top lyophilizer (Liotop, Model L-101, São Carlos, SP, Brazil) (LfF). Other three different nutraceuticals were prepared from LfF: (i) LfF + QUE (160 mg; Sigma-Aldrich) (LfFQ); ii) LfF + RES (150 mg; Sigma-Aldrich) (LfFR); and (iii) LfF + QUE (160 mg) + RES (150 mg) (LfFQR). The concentrations of QUE and RES used to prepare the nutraceuticals were chosen considering their safety and efficacy in promoting health benefits [19, 20]. The nutraceuticals were stored (4 ± 0.5 °C) in sterile amber screw-capped vials and maintained in desiccators with silica gel for relative humidity control [12]. The different nutraceuticals were tested separately in the experiments.
Exposure of Nutraceuticals to Simulated Gastrointestinal Conditions
Immediately after freeze-drying, the nutraceuticals were rehydrated with 10 mL of sterile distilled water for 15 min (25 ± 0.5 °C) in glass flasks (50 mL) under aerobic conditions. The simulations of gastrointestinal tract conditions were done in continuous steps mimicking the oral, gastric, and intestinal phases under aerobic conditions. The oral phase was simulated with α-amylase (100 U/mL) diluted in 1 mM CaCl2, pH 6.9 adjusted with 1 M NaHCO3, and exposure of 2 min with mechanical agitation (200 rpm, 37 °C ± 1 °C). The gastric phase was simulated with pH 2.0 adjusted with 1 M HCl. Gastric juice was simulated with a pepsin solution (25 mg/mL) prepared in 0.1 M HCl added in a proportion of 0.05 mL/mL of sample and incubated with mechanical agitation (130 rpm, 37 ± 1 °C, 90 min). The intestinal phase was simulated with pH 6.0 adjusted with 1 M NaHCO3. Intestinal juice was simulated with pancreatin (2 g/L) and bile salts (12 g/L) diluted in 1 M NaHCO3. The mixture was added at a rate of 0.25 mL/mL of sample and incubated under orbital stirring (37 ± 1 °C, 90 min, 45 rpm) [16]. Enzymes and reagents were obtained from Sigma-Aldrich.
Enumeration of Viable Cell Counts and Measurements of the Physiological Status of L. fermentum 296 Cells During Exposure to Simulated Gastrointestinal Conditions
After the exposure to each simulated gastrointestinal phase, an aliquot (100 μL) of the different nutraceuticals was serially diluted (1:9 v/v, 10−1–10−5) in sterile saline solution (NaCl 8.5 g/L) and plated on MRS agar. After 48 h of anaerobic incubation (AnaeroGen) at 37 ± 1 °C, the visible colonies were enumerated, and the results were expressed as CFU/mL. The detection limit of the plate count test was 2 log CFU/mL.
In parallel, after exposure to each phase of the simulated gastrointestinal conditions, an aliquot (1 mL) of the nutraceuticals was filtered (1.0 μm pore size filter), centrifuged (4500 × g, 10 min, 4 °C) and washed two times with PBS (4500 × g, 10 min, 4 °C), and incubated (15 min) under room temperature (25 ± 1 °C) in the dark for double-staining with propidium iodide (PI, Sigma-Aldrich, 10 μg/mL) to indicate membrane integrity and carboxyfluorescein diacetate (cFDA, Sigma-Aldrich, 2.5 μg/mL) to indicate cell enzymatic/metabolic activity [21, 22]. After the staining, the cell suspensions were washed (4500 × g, 10 min, 4 °C) with an equal volume of PBS to remove excess dye [23].
For dual staining with PI and cFDA, the cell subpopulations characterized as PI-cFDA + (upper left quadrant) were considered non-permeabilized with enzymatic activity (live cells); PI + cFDA + (upper right quadrant) were considered permeabilized with enzymatic activity (damage cells); PI + cFDA- (lower right quadrant; LR) were considered permeabilized without enzymatic activity (dead cells); and PI-cFDA- (lower left quadrant) were considered artifacts or non-stained cells [24]. A flow cytometer with an argon ion laser emitting at 488 nm (BD Accuri C6, Becton Dickinson, Franklin Lakes, NJ, USA) operating with previously described analytical conditions was used to perform the analysis [23]. Data were analyzed with statistical tables indicating the numbers (log/mL), percentage of stained cells in each detector, and fluorescence intensity of each fluorescent signal. An index of injured cells, named GMean index, was calculated using the ratio of fluorescence index means of FL3 (red fluorescence, PI) and FL1 (green fluorescence, cFDA) [25]:
Determination of the Contents and Bioaccessibility of QUE and RES During Exposure to Simulated Gastrointestinal Conditions
QUE and RES were extracted in triplicate from the nutraceuticals (1 mg) for 5 min with 2 mL of methanol and centrifuged (2500 × g, 5 min, 10 °C). The supernatant was collected and filtered with a 0.22 µm PVDF (Analítica, São Paulo, SP, Brazil). A liquid chromatography system (Shimadzu, Kyoto, Japan) with two parallel pumps LC-20AD, automatic injector SIL-20AHT, system controller CBM-20A, degasser DGU-20A5, a diode-array detector (DAD) SPD-M20A, and a quadrupole mass spectrometer LCMS-2020 with electrospray ionization (ESI) was used to the analysis. An N2 generator (NM32LA, Peak Scientific, Glasgow, UK) was coupled to the LC–MS. Chromatographic separation of compounds was achieved using a Poroshell 120 EC-C18 column (2.7 μm, 100 × 3.0 mm, Agilent Technologies, St. Clara, CA, USA) coupled to a Poroshell 120 EC-C18 guard column (2.7 μm, 5 × 2.1 mm, Agilent Technologies) using previously described analytical conditions [26]. Identification of QUE and RES was done by comparison with retention time, absorption spectra, and pseudomolecular ions of standards (Sigma-Aldrich). Quantification was done using DAD data for the peak area of each standard by external calibration at 360 nm for QUE and 306 nm for RES. Data were acquired by LabSolutions software (Shimadzu Corporation, version 5.82 SP1, 2008–2015).
Determination of the Antioxidant Capacity During Exposure to Simulated Gastrointestinal Conditions
The antioxidant capacity of the nutraceuticals after exposure to each phase of the simulated gastrointestinal conditions was evaluated with DPPH (2,2-diphenyl-1-picrylhydrazyl) and ABTS (2,2′-azino-bis(3-ethylbenzothiazoline-6-sulfonic acid) assays.
DPPH solution in methanol (0.1 mL) was reacted with aliquots (0.05 mL) of the nutraceuticals and kept in the dark (30 min). DPPH scavenging activity was determined at a wavelength of 517 nm. Controls consisted of water instead of a sample. DPPH radical-scavenging activity (%) was calculated with the equation [27]:
where ABScontrol is the absorbance of the DPPH radical + water and ABSsample is the absorbance of the DPPH radical + tested sample.
The ABTS radical cation (ABTS• +) was generated with the reaction of 5 mL of aqueous ABTS solution (7 mM) + 88 μL of potassium persulfate solution (140 mM). The mixture was kept in the dark (14 h, 28 ± 15 °C) before use and diluted with ethanol to obtain an absorbance of 0.7 ± 0.02 units at 734 nm. Aliquots (0.05 mL) of the samples were allowed to react with 0.1 mL of the resulting blue-green ABTS radical solution, kept in the dark (6 min), and the decrease of absorbance at 734 nm was measured. The percentage inhibition was calculated with the equation [28]:
where ABScontrol is the absorbance of ABTS radical + water and ABSsample is the absorbance of ABTS radical + tested sample.
Statistical Analysis
The experiments were done in triplicate in three independent repetitions. Data were expressed as average ± standard deviation. The normal data distribution was evaluated with the Kolmogorov–Smirnov normality test. ANOVA followed by post hoc Tukey’s test was used to determine significant differences among the results. A p-value of < 0.05 was considered statistically significant. The results were submitted to a Pearson’s correlation to verify the relationship between the plate counts, counts of cells in different physiological states (live, injured, and dead), GMean index, and antioxidant capacity (ABTS and DPPH assays). Statistical analysis was done with R software (Version 2.15.3, Ross Ihaka & Robert Gentleman, University of Auckland, Auckland, New Zealand).
Results
Plate Counts of L. fermentum 296 in the Nutraceuticals During Exposure to Simulated Gastrointestinal Conditions
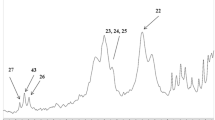
The plate counts of L. fermentum 296 in LfF, LfFQ, LfFR, and LfFQR exposed to simulated gastrointestinal conditions are shown in Fig. 1. Before exposure to simulated gastrointestinal conditions, i.e., immediately after freeze-drying (time zero), the plate counts of L. fermentum 296 in LfF, LfFQ, LfFR, and LfFQR were around 8 log CFU/mL, without significant differences between the examined nutraceuticals (p > 0.05). The exposure to oral conditions did not affect (p ≤ 0.05) L. fermentum 296 plate counts, which ranged from 8.05 ± 0.05 to 8.16 ± 0.16 log CFU/mL. However, the plate counts of L. fermentum 296 decreased (p ≤ 0.05) in the examined nutraceuticals after exposure to gastric conditions (pH 2.0), with counts ranging from 4.37 ± 0.27 to 6.48 ± 0.26 log CFU/mL. LfF had the lowest plate counts (4.37 ± 0.27 log CFU/mL) after exposure to gastric conditions (p ≤ 0.05), while LfFQR (6.26 ± 0.24 log CFU/mL) and LfFR (6.48 ± 0.26 log CFU/mL) had the highest plate counts (p ≤ 0.05). The plate counts of L. fermentum 296 did not change in LfF (3.97 ± 0.24 log CFU/mL) and LfFQ (5.25 ± 0.25 log CFU/mL) after exposure to intestinal conditions, while decreased (p ≤ 0.05) in LfFR (2.27 ± 0.25 log CFU/mL) and LfFQR (4.94 ± 0.32 log CFU/mL). As a result, LfFQ and LfFQR had the highest plate counts (p ≤ 0.05), while LfF and LfFR had the lowest plate counts (p ≤ 0.05) at the end of the simulated gastrointestinal conditions.
Plate counts (Log CFU/mL) of Limosilactobacillus fermentum 296 in the nutraceuticals exposed to simulated gastrointestinal conditions. LfF (
 ), L. fermentum 296 + fructooligosaccharides; LfFQ (
), L. fermentum 296 + fructooligosaccharides; LfFQ (
 ), L. fermentum 296 + FOS + QUE; LfFR (
), L. fermentum 296 + FOS + QUE; LfFR (
 ), L. fermentum 296 + FOS + RES; LfFQR (
), L. fermentum 296 + FOS + RES; LfFQR (
 ), L. fermentum 296 + FOS + QUE + RES. FOS, 200 mg; QUE, 160 mg; RES, 150 mg. Results are expressed as average ± standard deviation (n 3)
), L. fermentum 296 + FOS + QUE + RES. FOS, 200 mg; QUE, 160 mg; RES, 150 mg. Results are expressed as average ± standard deviation (n 3)
Physiological Status of L. fermentum 296 in the Nutraceuticals During Exposure to Simulated Gastrointestinal Conditions
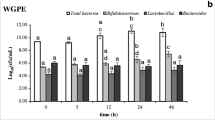
The measurements of the physiological status of L. fermentum 296 cells in LfF, LfFQ, LfFR, and LfFQR exposed to simulated gastrointestinal conditions are shown in Fig. 2 and Table 1. Before exposure to simulated gastrointestinal conditions, the examined nutraceuticals had sizes of PI-cFDA + (live) cell subpopulations ranging from 18.21 ± 0.15 to 72.21 ± 0.13%. After exposure to gastric conditions, the nutraceuticals had sizes of PI + cFDA + (injured) cell subpopulations ranging from 42.53 ± 0.61 to 57.24 ± 0.09%, while the sizes of PI + cFDA‐ (dead) cell subpopulations ranged from 15.62 ± 0.3 to 48.18 ± 0.11%. LfFQR had the highest size of live cell subpopulation (21.24 ± 0.19%) and the lowest size of dead cell subpopulation (15.62 ± 0.30%) after exposure to gastric conditions. LfF had the highest size of dead cell subpopulation after exposure to gastric conditions (48.18 ± 0.11%) and the lowest size of live cell subpopulation after exposure to intestinal conditions (2.31 ± 0.43%). LfFQR had the highest size of live cell subpopulation after exposure to intestinal conditions (28.40 ± 0.28%). LfFQ and LfFR had 15.16 ± 0.08% and 8.54 ± 0.37% of cells characterized as live, 41.24 ± 0.09% and 44.59 ± 0.41% of cells characterized as injured, and 31.52 ± 0.59% and 37.47 ± 0.23% of cells characterized as dead after exposure to intestinal conditions, respectively.
Physiological status of Limosilactobacillus fermentum 296 cells in the nutraceuticals exposed to simulated gastrointestinal conditions (B, before digestion; M, oral phase; G, gastric phase; I, intestinal phase). LfF, L. fermentum 296 + fructooligosaccharidesarides (FOS); LfFQ, L. fermentum 296 + FOS + QUE; LfFR, L. fermentum 296 + FOS + RES; LfFQR, L. fermentum 296 + FOS + QUE + RES. FOS, 200 mg; QUE, 160 mg; RES, 150 mg. Results are expressed as average ± standard deviation (n 3)
The plate counts (log CFU/mL) of L. fermentum 296 were close to the sum (log/mL) of the cell subpopulations characterized as viable and injured in all nutraceuticals before exposure to simulated gastrointestinal conditions and when exposed to oral conditions. Otherwise, the plate counts of L. fermentum 296 were lower than the sum of the cell subpopulations characterized as viable and injured in LfF, LfFQ, and LfFQR after exposure to gastric and intestinal conditions, as well as in LfFR after exposure to intestinal conditions (Table 1).
The GMean index allowed to indicate the rising of the physiological status of viable but nonculturable cells (VBNC) in L. fermentum 296 in the nutraceuticals when exposed to simulated gastrointestinal conditions (Table 1). The GMean index for L. fermentum 296 remained low (0.07–0.38 arbitrary unit) in LfF, LfFQ, LfFR, and LfFQR before exposure to simulated gastrointestinal conditions and when exposed to oral conditions. However, the GMean index increased for L. fermentum 296 cells in LfF, LfFQ, and LfFQR after exposure to gastric and intestinal conditions (0.61–1.25), and in LfFR after exposure to intestinal conditions (0.62). The comparison of the alterations in GMean index for L. fermentum 296 cells and the proportion (subpopulation size) of viable cells in a cultivable state considering the double-stained strand (PI-cFDA +) indicated that part of the viable cells became nonculturable when the GMean index reached 0.5 (arbitrary unit), which increased up to 1.25 in LfF, LfFQ, and LfFQR after exposure to gastric and intestinal conditions, as well as in LfFR after exposure to intestinal conditions.
Contents and Bioaccessibility of QUE and RES in the Nutraceuticals During Exposure to Simulated Gastrointestinal Conditions
The contents of QUE and RES in LfFQ, LfFR, and LfFQR exposed to simulated gastrointestinal conditions are shown in Table 2. QUE and RES were detected after exposure to oral, gastric, and intestinal conditions. QUE and RES contents did not change (p > 0.05) in the nutraceuticals after exposure to oral and gastric conditions. After exposure to these conditions, QUE contents ranged from 41.49 ± 3.20 to 42.95 ± 2.71 g/100 g in LfFQ; RES contents ranged from 41.93 ± 1.51 to 39.37 ± 3.75 g/100 g in LfFR, and QUE and RES contents ranged from 20.62 ± 0.15 to 20.06 ± 0.89 g/100 g and from 27.79 ± 0.74 to 27.54 ± 0.92 g/100 g in LfFQR, respectively. After exposure to intestinal conditions, QUE and RES contents decreased in the nutraceuticals, which ranged from 12.85 ± 0.86 to 29.17 ± 0.62 g/100 g and 19.83 ± 0.66 to 23.05 ± 0.33 g/100 g, respectively. LfFQ and LfFR had the highest contents of QUE (29.17 ± 0.62 g/100 g) and RES (23.05 ± 0.33 g/100 g) after exposure to intestinal conditions, respectively.
The nutraceuticals showed high bioaccessibility of QUE and RES after exposure to oral, gastric, and intestinal conditions (Table 2). LfFQ had the highest bioaccessibility (96.6 ± 0.03%) of QUE and it was observed after exposure to gastric conditions, while LfFQR had the lowest bioaccessibility (63.9 ± 0.12%). Similarly, after exposure to intestinal conditions, LfFQ had higher QUE bioaccessibility (65.6 ± 0.01%) than LfFQR (41.0 ± 0.09%). LfFQR had higher bioaccessibility of RES than LfFR after exposure to gastric (93.6 ± 0.21 vs. 91.9 ± 0.07%, respectively) and intestinal conditions (67.4 ± 0.17 vs. 53.8 ± 0.02%, respectively).
Antioxidant Capacity of the Nutraceuticals During Exposure to Simulated Gastrointestinal Conditions
The antioxidant capacity of LfF, LfFQ, LfFR, and LfFQR exposed to simulated gastrointestinal conditions was evaluated by ABTS and DPPH assays (Fig. 3). To remove the impact of the enzymes on the measured antioxidant capacity, a control experiment without enzymes was evaluated on each phase simulating the gastrointestinal conditions and the obtained values were reduced from those measured for the simulation with enzymes. LfF, LfFQ, LfFR, and LfFQR maintained their antioxidant capacity when exposed to simulated gastrointestinal conditions in either ABTS or DPPH assay, although differences between both assays were observed.
Antioxidant capacity of the nutraceuticals exposed to simulated gastrointestinal conditions (B, before digestion; M, oral phase; G, gastric phase; I, intestinal phase). LFf, L. fermentum 296 + FOS; LfFQ, L. fermentum 296 + FOS + QUE; LfFR, L. fermentum 296 + FOS + RES; LfFQR, L. fermentum 296 + FOS + QUE + RES. FOS, 200 mg; QUE, 160 mg; RES, 150 mg. Results are expressed as average ± standard deviation (n 3). a–d: different lowercase letters denote differences among the different nutraceuticals at each gastrointestinal phase, based on Tukey’s test (p ≤ 0.05)
After exposure to gastric conditions, the lowest and highest antioxidant capacity evaluated by ABTS assay was observed in LfF (13.59 ± 0.58%) and LfFQR (79.26 ± 1.05%), respectively. In the ABTS assay, the antioxidant capacity of all examined nutraceuticals increased (p < 0.05) after exposure to intestinal conditions compared to gastric conditions, where the highest and lowest antioxidant capacity were found in LfFQR (88.18 ± 1.16%) and LfF (50.21 ± 1.12%), respectively. In the DPPH assay, the antioxidant capacity of the nutraceutical formulations increased and decreased after exposure to gastric and intestinal conditions, respectively. LfFQR (75.54 ± 0.65%) and LfF (25.00 ± 0.70%) had the highest and lowest antioxidant capacity after exposure to gastric conditions, respectively (p < 0.05).
Pearson’s correlation results showed that L. fermentum 296 plate counts correlated positively with the live cell counts measured by flow cytometry (p < 0.001; R = 0.76) and antioxidant capacity measured by DPPH assay (p < 0.001; R = 0.56), while L. fermentum 296 plate counts correlated negatively with GMean index (p < 0.001; R = − 0.72) (Fig. 4).
Pearson’s correlation coefficients indicate the associations between the plate counts, physiological states, and Gmean index of Limosilactobacillus fermentum 296, and the antioxidant capacity in the nutraceuticals exposed to simulated gastrointestinal conditions. The white cell represents no significant correlation
Discussion
Viability is a key factor in probiotics to confer the claimed health benefits on the host [29]. Before exposure to simulated gastrointestinal conditions, L. fermentum 296 had plate counts of around 8 log CFU/mL in LfF, LfFQ, LfFR, and LfFQR. There is no standard recommendation regarding the plate counts (viable bacterial cell concentration) of a probiotic to be consumed to reach a health benefit. However, it is generally accepted that a probiotic must have a concentration of at least 6 log CFU/g or mL of the delivery product [30]. During the exposure to simulated gastrointestinal conditions, the plate counts of L. fermentum 296 in LfF, LfFQ, LfFR, and LfFQR decreased, especially after exposure to gastric conditions. The acidic environment and presence of pepsin in the stomach may account for damage to the cell membrane, DNA, and cell proteins, leading to bacterial viability loss [31,32,33]. The nutraceuticals with QUE and RES in their composition, i.e., LfFQ, LfFR, and LfFQR, had higher plate counts of L. fermentum 296 after exposure to gastric conditions, indicating that QUE and RES exert protective effects on L. fermentum 296 cells when challenged with an acidic environment. The capacity of QUE and RES to increase probiotic lactobacilli survival when exposed to pH 2 or 3 was previously reported, suggesting that polyphenols could act as buffers to protect probiotics against low pH values [7].
Although the plate counts of L. fermentum 296 continued to decrease when exposed to intestinal conditions, LfFQ, LfFR, and LfFQR had minor reductions compared to the nutraceutical without QUE and RES (LfF). Considering that the target of probiotics is the intestine, the capability of LfFQ, LfFR, and LfFQR in helping to keep the viability of L. fermentum 296 up to reaching the intestinal phase is an important result because the release of viable probiotics is necessary for gastrointestinal tract colonization [7, 34].
The examined nutraceuticals had a small portion of injured L. fermentum 296 cells before exposure to simulated gastrointestinal conditions, which may be due to the freeze-drying process used in their production. However, the more remarkable changes in the physiological status of L. fermentum 296 cells in the nutraceuticals occurred after exposure to gastric conditions. The increase in the subpopulation of injured and dead cells after exposure to gastric conditions could be expected due to acid stress (pH around 2.0) and presence of pepsin that can injure or even inactivate probiotic cells (Melchior et al. [32]). However, LfFQR had the lowest subpopulation of L. fermentum 296 dead cells, followed by LfFQ and LfFR. The subpopulations of injured and dead cells increased at the end of the simulated gastrointestinal conditions, although the nutraceuticals with QUE and/or RES had the lowest subpopulations of dead cells. The protective effects of QUE and RES on L. fermentum 296 cells could be linked to their antioxidant capacity [35], which is reinforced by the positive correlation between the plate counts and antioxidant capacity (DPPH assay) in LfFQ, LfFR, and LfFQR during exposure to simulated gastrointestinal conditions.
The cFDA and PI dual staining was a sensitive and effective method to assess the physiological status of L. fermentum 296 cells in the nutraceuticals exposed to simulated gastrointestinal conditions. Some studies have shown the relationship between the bacterial cell viability (live cell phenotype) indicated by staining and plate culture capacity [34, 36]. In this study, when the values of the plate counts and the sum of the live and injured cells were close, the injured cells could be as cultivable as the viable cells. However, when the values of the plate counts were smaller than the sum of the viable and injured cells, it could indicate that part of the injured cells became nonculturable. VBNC cells could enter this state because exposure to digestive stressing conditions can disturb physiological functions and cause sublethal cell damage [37].
Stressed probiotic bacteria that enter in VBNC state are metabolically active but do not grow in culture media, being undetectable by plate counting [25, 34]. These cells can be detected by combining plate counts and physiological function measurements with flow cytometry [38, 39]. This study showed that in the gastrointestinal conditions causing the greatest stress (gastric and intestinal phases), part of L. fermentum 296 cells could be entered the VBNC state, where an arbitrary GMean index unit was defined to classify it (above 0.5). The existence of VBNC cells in some probiotic lactobacilli is suggested as a common incidence [25, 40]. However, probiotic lactobacilli VBNC cells could recover from sublethal damage, restore broad functioning, and replicate in more favorable environments, such as when implanted in the gut [41]. The plate counts and live cell counts of L. fermentum 296 in the nutraceuticals exposed to simulated gastrointestinal conditions correlated positively, while the plate counts correlated negatively with GMean index, confirming that the higher the GMean index the lower the population of cells cultivable in agar.
The contents of QUE and RES in the nutraceutical did not change up to exposure to gastric conditions, while were lower when exposed to intestinal conditions compared to oral and gastric conditions. The contents of QUE and RES in phenolic-rich matrices can decrease when exposed to gastrointestinal conditions, being changes in pH as the main factor causing the irreversible breakdown of QUE and RES [35]. In addition, the hydrogen bonds of QUE and RES can be cleaved by hydrolytic enzymes, such as amylase, pepsin, and pancreatic enzymes. Most dietary polyphenols, including phenolic acid and flavonoids, are stable under acidic conditions in the stomach [35] but are sensitive to mildly alkaline conditions in the small intestine [35, 42].
Bioaccessibility is the efficiency of digestion and absorption (or digestibility and absorptivity) of a given food constituent and is usually expressed as a percentage of the actual amount released and absorbed concerning its total content [43]. LfFQ, LfFR, and LfFQR showed bioaccessibility of QUE and RES during exposure to simulated gastrointestinal conditions. The highest percentage of bioaccessibility was found after exposure to oral and gastric conditions, while it slightly decreased after exposure to intestinal conditions.
Oral conditions typically do not affect the bioaccessibility of phenolic compounds due to the short time of exposure to salivary amylase [44, 45]. The greater bioaccessibility of phenolic compounds after exposure to gastric conditions compared to intestinal conditions has been also linked to their greater stability in acidic pH. Phenolic compounds may change in neutral to alkaline pH found in the intestine, which could explain their lower bioaccessibility after exposure to intestinal conditions [26, 46], agreeing with the results of QUE and RES contents and their bioaccessibility in LfFQ, LfFR, and LfFQR. The bioaccessibility of QUE was lower when combined with RES in LfFQR, which could be linked to the low solubility of QUE in the intestinal fluid. Additionally, the combination with RES could reduce the QUE solubility and restrict its release in the buffer solution [36, 47].
LfFQ, LfFR, and LfFQR maintained the antioxidant capacity during exposure to simulated gastrointestinal conditions when measured by ABTS and DPPH assays. However, the assays showed different patterns since in the DPPH assay, the nutraceuticals had a higher antioxidant capacity when exposed to gastric conditions, while in the ABTS assay, the nutraceuticals had a lower antioxidant capacity when exposed to gastric conditions. ABTS and DPPH assays have different mechanisms to measure antioxidant capacity. The transition from acidic to alkaline media typically increases the release of phenolic compounds and flavonoids, contributing to an increased antioxidant capacity due to the deprotonation of the hydroxyl groups forming the aromatic rings [48,49,50]. Another influential factor in the antioxidant capacity of phenolic compounds is their interaction with other compounds released during the gastrointestinal passage, such as the sugars present in FOS used as a cryoprotectant to prepare the examined nutraceuticals, which can increase the antioxidant capacity in the intestinal environment [51]. The maintenance of the antioxidant capacity of the nutraceuticals during the gastrointestinal passage is important since they can exert a local antioxidant effect and regulate gastrointestinal inflammation due to their ability to protect the body against oxidative stress [52], besides reaching the colon with high contents of bioactive components to exert the reported beneficial impacts on the intestinal microbiota [14]. Although the protocol used in this study has shown high accuracy and consistent results indicating the maintenance of the bioactive components and potential functionalities of the examined nutraceuticals through the gastrointestinal tract, one possible limitation of this study could be the characteristics of the material resulting from their exposure to each phase of the simulated gastrointestinal conditions that could differently compared to in vivo models because of the difficulties to simulate complex physicochemical and physiological events occurring in the human digestive tract. Thereby, further in vivo investigations could confirm the expected beneficial effects caused by the consumption of the examined nutraceuticals on parameters linked to intestinal health and systemic outcomes.
Conclusion
The results showed that the nutraceuticals with QUE and/or RES exerted protective effects on L. fermentum 296 during exposure to simulated gastrointestinal conditions, helping to keep high counts of viable and physiologically functioning potentially probiotic cells. When exposed to gastric and intestinal conditions, part of L. fermentum 296 cells in the nutraceuticals could be entered the VBNC state but maintained their vitality, where an arbitrary GMean index (above 0.5) was defined to classify it. Furthermore, the nutraceuticals kept high contents and bioaccessibility of QUE and RES, as well as antioxidant capacity during exposure to simulated gastrointestinal conditions, which could be linked to the protective effects on L. fermentum 296. This study showed for the first time that nutraceuticals combining potentially probiotic L. fermentum 296, QUE, and/or RES could cross along the gastrointestinal tract with high concentrations of functioning cells, bioavailable phenolic compounds, and antioxidant capacity to exert the local and systemic beneficial impacts on the consumers’ health, being an innovative strategy for co-ingestion of these bioactive components and formulation of novel added-value nutraceuticals.
Data Availability
The datasets generated during and or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, Morelli L, Canani RB, Flint HJ, Salminen S, Calder PC, Sanders ME (2014) The International scientific association for probiotics and prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol 11:506–514. https://doi.org/10.1038/nrgastro.2014.66
Huang R, Wang K, Hu J (2016) Effect of probiotics on depression: a systematic review and meta-analysis of randomized controlled trials. Nutrients. https://doi.org/10.3390/nu8080483
Roobab U, Batool Z, Manzoor MF, Shabbir MA, Khan MR, Aadil RM (2020) Sources, formulations, advanced delivery and health benefits of probiotics. Curr Opin Food Sci 32:17–28. https://doi.org/10.1016/j.cofs.2020.01.003
Rodrigues FJ, Cedran MF, Bicas JL, Sato HH (2020) Encapsulated probiotic cells: Relevant techniques, natural sources as encapsulating materials and food applications – a narrative review. Food Res Int 137:109682. https://doi.org/10.1016/j.foodres.2020.109682
Chen S, Cao Y, Ferguson LR, Shu Q, Garg S (2012) Flow cytometric assessment of the protectants for enhanced in vitro survival of probiotic lactic acid bacteria through simulated human gastro-intestinal stresses. Appl Microbiol Biotechnol 95:345–356. https://doi.org/10.1007/s00253-012-4030-3
dos Santos AS, de Albuquerque TMR, de Brito Alves JL, de Souza EL (2019) Effects of quercetin and resveratrol on in vitro properties related to the functionality of potentially probiotic Lactobacillus strains. Front Microbiol 10:1–13. https://doi.org/10.3389/fmicb.2019.02229
Repossi G, Das UN, Eynard AR (2020) Molecular basis of the beneficial actions of resveratrol. Arch Med Res 51:105–114. https://doi.org/10.1016/j.arcmed.2020.01.010
Bostancıeri N, Elbe H, Eşrefoğlu M, Vardı N (2022) Cardioprotective potential of melatonin, quercetin and resveratrol in an experimental model of diabetes. Biotech Histochem 97:152–157. https://doi.org/10.1080/10520295.2021.1918766
Mrkus L, Batinić J, Bjeliš N, Jakas A (2019) Synthesis and biological evaluation of quercetin and resveratrol peptidyl derivatives as potential anticancer and antioxidant agents. Amino Acids 51:319–329. https://doi.org/10.1007/s00726-018-2668-6
Yang Z, McClements DJ, Peng X, Xu Z, Meng M, Chen L, Jin Z (2023) Fabrication of zein–carboxymethyl cellulose nanoparticles for co-delivery of quercetin and resveratrol. J Food Eng 341:111322. https://doi.org/10.1016/j.jfoodeng.2022.111322
Santini A, Cammarata SM, Capone G, Ianaro A, Tenore GC, Pani L, Novellino E (2018) Nutraceuticals: opening the debate for a regulatory framework. Br J Clin Pharmacol 84:659–672. https://doi.org/10.1111/bcp.13496
Sampaio KB, do Nascimento YM, Tavares JF, Cavalcanti MT, de Brito Alves JL, Garcia EF, Souza EL (2021) Development and in vitro evaluation of novel nutraceutical formulations composed of Limosilactobacillus fermentum, quercetin and/or resveratrol. Food Chem 342:128264. https://doi.org/10.1016/j.foodchem.2020.128264
Nascimento DS, Sampaio KB, do Nascimento YM, de Souza TA, de Souza FS, Júnior JVC, Tavares JF, da Silva MS, de Souza EL (2022) Evaluating the stability of a novel nutraceutical formulation combining probiotic Limosilactobacillus fermentum 296, quercetin, and resveratrol under different storage conditions. Probiotics Antimicrob Proteins. https://doi.org/10.1007/s12602-022-10011-z
Sampaio KB, de Brito Alves JL, do Nascimento YM, Tavares JF, da Silva MS, dos D SN, Lima MS, Rodrigues NPA, Garcia EF, de Souza EL (2022) Nutraceutical formulations combining Limosilactobacillus fermentum, quercetin, and or resveratrol with beneficial impacts on the abundance of intestinal bacterial populations, metabolite production, and antioxidant capacity during colonic fermentation. Food Res Int 161:111800. https://doi.org/10.1016/j.foodres.2022.111800
Garcia EF, Luciano WA, Xavier DE, Costa WCA, Oliveira KS, Franco OL, de Morais Júnior MA, Lucena BTL, Picão RC, Magnani M, Saarela M, de Souza EL (2016) Identification of lactic acid bacteria in fruit pulp processing byproducts and potential probiotic properties of selected Lactobacillus strains. Front Microbiol 7:1–11. https://doi.org/10.3389/fmicb.2016.01371
de Albuquerque TMR, Garcia EF, de Oliveira AA, Magnani M, Saarela M, de Souza EL (2018) In vitro characterization of Lactobacillus strains isolated from fruit processing by-products as potential probiotics. Probiotics Antimicrob Proteins 10:704–716. https://doi.org/10.1007/s12602-017-9318-2
Cavalcante RGS, de Albuquerque TMR, de Luna Freire MO, Ferreira GAH, Carneiro dos Santos LA, Magnani M, Cruz JC, Braga VA, de Souza EL, de Brito Alves JL (2019) The probiotic Lactobacillus fermentum 296 attenuates cardiometabolic disorders in high fat diet-treated rats. Nutr Metab Cardiovasc Dis 29:1408–1417. https://doi.org/10.1016/j.numecd.2019.08.003
Ferreira GAF, Magnani M, Cabral L, Brandão LR, Noronha MF, Cruz JC, de Souza EL, de Brito-Alves JL (2022) Potentially probiotic Limosilactobacillus fermentum fruit-derived strains alleviate cardiometabolic disorders and gut microbiota impairment in male rats fed a high-fat diet. Probiotics Antimicrob Proteins 14:349–359. https://doi.org/10.1007/s12602-021-09889-y
Dower JI, Geleijnse JM, Gijsbers L, Schalkwijk C, Kromhout D, Hollman PC (2015) Supplementation of the pure flavonoids epicatechin and quercetin affects some biomarkers of endothelial dysfunction and inflammation in (pre)hypertensive adults: a randomized double-blind, placebo-controlled, crossover trial. J Nutr 145:1459–1463. https://doi.org/10.3945/jn.115.211888
European Food Safety Authority (EFSA) (2016) Safety of synthetic trans-resveratrol as a novel food pursuant to Regulation (EC) No 258/97. EFSA J 14:1–30. https://doi.org/10.2903/j.efsa.2016.4368
Gandhi A, Shah NP (2015) Effect of salt on cell viability and membrane integrity of Lactobacillus acidophilus, Lactobacillus casei and Bifidobacterium longum as observed by flow cytometry. Food Microbiol 49:197–202. https://doi.org/10.1016/j.fm.2015.02.003
Sträuber H, Müller S (2010) Viability states of bacteria-specific mechanisms of selected probes. Cytometry A 77:623–634. https://doi.org/10.1002/cyto.a.20920
de Sousa Guedes JP, de Souza EL (2018) Investigation of damage to Escherichia coli, Listeria monocytogenes and Salmonella Enteritidis exposed to Mentha arvensis L. and M. piperita L. essential oils in pineapple and mango juice by flow cytometry. Food Microbiol 76:564–571. https://doi.org/10.1016/j.fm.2017.09.020
Paparella A, Taccogna L, Aguzzi I, Chaves-López C, Serio A, Marsilio F, Suzzi G (2008) Flow cytometric assessment of the antimicrobial activity of essential oils against Listeria monocytogenes. Food Cont 19:1174–1182. https://doi.org/10.1016/j.foodcont.2008.01.002
El Arbi A, Ghorbal S, Delacroix-Buchet A, Bouix M (2011) Assessment of the dynamics of the physiological states of Lactococcus lactis ssp. cremoris SK11 during growth by flow cytometry. J Appl Microbiol 111:1205–1211. https://doi.org/10.1111/j.1365-2672.2011.05114.x
Inada KOP, Silva TBR, Lobo LA, Domingues RMCP, Perrone D, Monteiro M (2020) Bioaccessibility of phenolic compounds of jaboticaba (Plinia jaboticaba) peel and seed after simulated gastrointestinal digestion and gut microbiota fermentation. J. Funct. Foods 67:103851. https://doi.org/10.1016/j.jff.2020.103851
Brand-Williams W, Cuvelier ME, Berset CLWT (1995) Use of a free radical method to evaluate antioxidant activity. LWT-Food Sci Technol 28:25–30. https://doi.org/10.1016/S0023-6438(95)80008-5
Re R, Pellegrini N, Proteggente A, Pannala A, Yang M, Rice-Evans C (1999) Antioxidant activity applying an improved ABTS radical cation decolorization assay. Free Rad Biol Med 26:1231–1237. https://doi.org/10.1016/S0891-5849(98)00315-3
Zendeboodi F, Khorshidian N, Mortazavian AM, da Cruz AG (2020) Probiotic: conceptualization from a new approach. Curr Opin Food Sci 32:103–123. https://doi.org/10.1016/j.cofs.2020.03.009
Food and Agriculture Organization - World Health Organization (FAO/WHO) (2006) Probiotics in food: health and nutritional properties and guidelines for evaluation. FAO. Internet: https://www.fao.org/3/a0512e/a0512e.pdf. Accessed 13 Sept 2022. https://doi.org/10.1201/9781420009613.ch16
Amund OD (2016) Exploring the relationship between exposure to technological and gastrointestinal stress and probiotic functional properties of lactobacilli and bifidobacteria. Can J Microbiol 62:715–725. https://doi.org/10.1139/cjm-2016-0186
Melchior S, Marino M, D’Este F, Innocente N, Nicoli MC, Calligaris S (2021) Effect of the formulation and structure of monoglyceride-based gels on the viability of probiotic: Lactobacillus rhamnosus upon in vitro digestion. Food Funct 12:351–361. https://doi.org/10.1039/d0fo01788d
Ramos PE, Abrunhosa L, Pinheiro A, Cerqueira MA, Motta C, Castanheira I, Chandra-Hioe MV, Arcot J, Teixeira JA, Vicente AA (2016) Probiotic-loaded microcapsule system for human in situ folate production: encapsulation and system validation. Food Res Int 90:25–32. https://doi.org/10.1016/j.foodres.2016.10.036
Rodrigues NPA, Garcia EF, Sampaio KB, do Nascimento HMA, de Sousa Guedes JP, de Souza EL (2022) Dynamics of physiological responses of potentially probiotic fruit-derived Limosilactobacillus fermentum in apple and orange juices during refrigeration storage and exposure to simulated gastrointestinal conditions. Arch Microbiol 204:1–11. https://doi.org/10.1007/s00203-021-02672-1
Lee SY, Lee SJ, Yim DG, Hur SJ (2020) Changes in the content and bioavailability of onion quercetin and grape resveratrol during in vitro human digestion. Foods. https://doi.org/10.3390/foods9060694
Chen X, McClements DJ, Zhu Y, Chen Y, Zou L, Liu W, Cheng C, Fu D, Liu C (2018) Enhancement of the solubility, stability and bioaccessibility of quercetin using protein-based excipient emulsions. Food Res Int 114:30–37. https://doi.org/10.1016/j.foodres.2018.07.062
Robben C, Fister S, Witte AK, Schoder D, Rossmanith P, Mester P (2018) Induction of the viable but non-culturable state in bacterial pathogens by household cleaners and inorganic salts. Sci Reports 8:1–9. https://doi.org/10.1038/s41598-018-33595-5
Barbosa IM, Almeida ÉTC, Gomes ACA, de Souza EL (2020) Evidence on the induction of viable but non-culturable state in Listeria monocytogenes by Origanum vulgare L. and Rosmarinus officinalis L. essential oils in a meat-based broth. Innov Food Sci Emerg Technol 62:102351. https://doi.org/10.1016/j.ifset.2020.102351
Pane M, Allesina S, Amoruso A, Nicola S, Deidda F, Mogna L (2018) Flow cytometry evolution of microbiological methods for probiotics enumeration. J Clin Gastroenterol 52:S41–S45. https://doi.org/10.1097/MCG.0000000000001057
Lahtinen SJ, Ouwehand AC, Reinikainen JP, Korpela JM, Sandholm J, Salminen SJ (2006) Intrinsic properties of so-called dormant probiotic bacteria, determined by flow cytometric viability assays. Appl Environ Microbiol 72:5132–5134. https://doi.org/10.1128/AEM.02897-05
Davis C (2014) Enumeration of probiotic strains: review of culture-dependent and alternative techniques to quantify viable bacteria. J Microbiol Methods 103:9–17. https://doi.org/10.1016/j.mimet.2014.04.012
Zupančič Š, Lavrič Z, Kristl J (2015) Stability and solubility of trans-resveratrol are strongly influenced by pH and temperature. Eur J Pharm Biopharm 93:196–204. https://doi.org/10.1016/j.ejpb.2015.04.002
Shahidi F, Peng H (2018) Bioaccessibility and bioavailability of phenolic compounds. J Food Bioact 4:11–68. https://doi.org/10.31665/jfb.2018.4162
José Jara-Palacios M, Gonçalves S, Hernanz D, Heredia FJ, Romano A (2018) Effects of in vitro gastrointestinal digestion on phenolic compounds and antioxidant activity of different white winemaking byproducts extracts. Food Res Int 109:433–439. https://doi.org/10.1016/j.foodres.2018.04.060
Verotta L, Panzella L, Antenucci S, Calvenzani V, Tomay F, Petroni K, Caneva E, Napolitano A (2018) Fermented pomegranate wastes as sustainable source of ellagic acid: antioxidant properties, anti-inflammatory action, and controlled release under simulated digestion conditions. Food Chem 246:129–136. https://doi.org/10.1016/j.foodchem.2017.10.131
Faria A, Fernandes I, Norberto S, Mateus N, Calhau C (2014) Interplay between anthocyanins and gut microbiota. J Agric Food Chem 62:6898–6902. https://doi.org/10.1021/jf501808a
Carbonell-Capella JM, Buniowska M, Barba FJ, Esteve MJ, Frígola A (2014) Analytical methods for determining bioavailability and bioaccessibility of bioactive compounds from fruits and vegetables: a review. Compr Rev Food Sci Food Saf 13:155–171. https://doi.org/10.1111/1541-4337.12049
Farias DP, de Araújo FF, Neri-Numa IA, Dias-Audibert FL, Delafiori J, Catharino RR, Pastore GM (2021) Effect of in vitro digestion on the bioaccessibility and bioactivity of phenolic compounds in fractions of Eugenia pyriformis fruit. Food Res Int 150:110767. https://doi.org/10.1016/j.foodres.2021.110767
Dutra RLT, Dantas AM, Marques DA, Batista JDF, Meireles BRLA, de Magalhães Cordeiro ÂMT, Magnani M, Borges GSC (2017) Bioaccessibility and antioxidant activity of phenolic compounds in frozen pulps of Brazilian exotic fruits exposed to simulated gastrointestinal conditions. Food Res Int 100:650–657. https://doi.org/10.1016/j.foodres.2017.07.047
Dantas AM, Mafaldo IM, Oliveira PML, Lima MS, Magnani M, Borges GSC (2019) Bioaccessibility of phenolic compounds in native and exotic frozen pulps explored in Brazil using a digestion model coupled with a simulated intestinal barrier. Food Chem 274:202–214. https://doi.org/10.1016/j.foodchem.2018.08.099
Sollano-Mendieta XC, Meza-Márquez OG, Osorio-Revilla G, Téllez-Medina DI (2021) Effect of in vitro digestion on the antioxidant compounds and antioxidant capacity of 12 plum (Spondias purpurea L.) ecotypes. Foods 10:1995. https://doi.org/10.3390/foods10091995
Caponio GR, Lippolis T, Tutino V, Gigante I, De Nunzio V, Milella RA, Gasparro M, Notarnicola M (2022) Nutraceuticals: focus on anti-inflammatory, anti-cancer, antioxidant properties in gastrointestinal tract. Antioxidants 11:1274. https://doi.org/10.3390/antiox11071274
Funding
This study was funded by CNPq (Brazil) (Grant 404353/2021–5) and CAPES (Brazil) (Finance code 001).
Author information
Authors and Affiliations
Contributions
Conceptualization: KBS, EFG, JLBA, ELS. Data curation: KBS, ELS. Formal analysis: KBS, YMN, JFT, NPAR, ELS. Funding acquisition: ELS, MSS, MSL; investigation: KBS, YMN, DSN, MCM, JFT, NPAR, ELS; methodology: KBS, EFG, YMN, JFT, MCM, DSN, MSL, NPAR, ELS; project administration: ELS. Supervision: ELS, EFG. Validation: KBS, ELS. Visualization, writing—original draft: KBS, ELS, EFG, MCM, JLBA. Writing—review and editing: KBS, ELS.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sampaio, K.B., de Brito Alves, J.L., do Nascimento, Y.M. et al. Effects of Simulated Gastrointestinal Conditions on Combined Potentially Probiotic Limosilactobacillus fermentum 296, Quercetin, and/or Resveratrol as Bioactive Components of Novel Nutraceuticals. Probiotics & Antimicro. Prot. 16, 308–319 (2024). https://doi.org/10.1007/s12602-023-10046-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12602-023-10046-w