Abstract
The lateral circumflex femoral artery (LCFA) is important for surgical approaches to the hip joint; its branches are often used as grafts and pedicled flaps. Our aim was to contribute to the literature by reporting variations. The LCFA branching pattern was studied in 26 lower limbs of formalin-fixed cadavers. It was recorded whether the LCFA originated from the femoral artery (FA) or the deep femoral artery (DFA). The distances of LCFA from the mid-inguinal point (MIP) and DFA; and the diameters of LCFA and its branches were measured with metric caliper. Side differences were analyzed by Wilcoxon test. The mean shortest distance from the LCFA to the MIP was 59.45 ± 13.06 mm and to the DFA was 19.23 ± 9.63 mm. The mean diameters of LCFA and its ascending, transverse, and descending branches were 5.82 ± 1.87 mm, 3.28 ± 0.87 mm, 3.02 ± 0.92 mm, and 3.61 ± 0.98 mm, respectively. The LCFA originated from 80.8% DFA and 19.2% FA. Data were evaluated jointly (p > 0.05). In one case, an accessory transverse branch was found. Spearman analysis shows that as the distance between the LCFA and the MIP increased, the diameter of the LCFA and its branches increased. Knowledge of the LCFA branching pattern is essential for interventional options in arterial grafts, such as bypass surgery, pedicled flaps, and surgical approaches to the hip joint. Preoperative radiologic evaluation for accurate knowledge of the topography of the branching pattern and vessel size can contribute to successful management of intraoperative blood loss and avoidance of iatrogenic injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
This study aims to define the origin, branches, diameter, and variations of lateral circumflex femoral artery (LCFA). LCFA usually arises from the deep femoral artery (DFA) close to its root or directly from the femoral artery (FA) or as a common trunk with DFA and the medial circumflex femoral artery (MCFA). It courses laterally passing between the divisions of the femoral nerve, posterior to the sartorius and rectus femoris muscles and terminates by dividing into ascending (LCFAa), transverse (LCFAt) and descending (LCFAd) branches. The LCFAa and LCFAd may occasionally arise separately. The LCFA contributes blood supply to head and neck of femur, greater trochanter, vastus lateralis and knee region (Standring 2021).
Branches of the LCFA are often used as vascular grafts in surgery, such as coronary artery bypass grafting. It is also used as a pedicled flap in tissue reconstructions. Knowing the anatomy of this area can be a great help to physicians who deal with this region, in diagnosis and treatment. Our study aimed to provide data about the diameter of LCFA at the point of origin, its branching patterns, and branches to assist in medical interventions.
Materials and methods
The origin of the LCFA and its branching pattern were examined in 26 lower limbs of 13 (females three and males 10) adult formalin fixed cadavers. The age of the cadavers ranged from 38 to 88 years.
First skin was incised and reflected to remove the subcutaneous tissue, then the fascia lata in the femoral triangle was incised. The FA was exposed and traced from the inguinal ligament to the adductor canal, and its branches were revealed. Sartorius and rectus femoris muscles were incised to expose the branching LCFA. The midpoint of the shortest distance between the pubic tubercle and anterior superior iliac spine (ASIS) was used as a reference point (mid-inguinal point, MIP). Then, the following measurements were made:
-
1.
Measurement: The distance from the origin of the LCFA to the MIP
-
2.
Measurement: The distance between the origins of the LCFA and the DFA
-
3.
Measurement: The diameter of the LCFA at the origin
-
4.
Measurement: The diameter of the LCFAa at the origin
-
5.
Measurement: The diameter of the LCFAt at the origin
-
6.
Measurement: The diameter of the LCFAd at the origin
All measurements were made with a metric caliper and data are given in millimeters (mm). The topography of variant arterial branches and their relation to the surrounding tissue were documented as images and diagrams. Photographs were taken by a smartphone (iPhone 13 Pro max, Apple Inc., USA), and diagrams were prepared on a tablet computer (iPad Pro, Apple Inc., USA) with Procreate application. Differences between the right and left sides were statistically analyzed using the Wilcoxon test. A p-value of < 0.05 indicates statistically significant difference. This study was ethically approved by the Clinical Research Ethics Committee of our faculty (E-71874115–903.99–82,378) and followed the guidelines of the Declaration of Helsinki. This publication is derived from the thesis and research conducted by the author (İbiş 2022). A diagram of the LCFA is shown in the Fig. 1a, and the measurement points and distances are shown in Fig. 1b.
a A diagram of the LCFA on the left side. AA = abdominal aorta, CIA = common iliac artery, IIA = internal iliac artery, EIA = external iliac artery, FA = femoral artery, DFA = deep femoral artery, LCFA = lateral circumflex femoral artery, LCFAa = ascending branch of LCFA, LCFAt = transverse branch of LCFA, LCFAd = descending branch of LCFA, ASIS = anterior superior iliac spine, PT = pubic tubercle, IL = inguinal ligament. b A diagram of the measurement points and distances on the left side. 1 = the distance from the origin of the LCFA to the MIP, 2 = the distance between the origins of the LCFA and the DFA, 3 = the diameter of the LCFA at the origin, 4 = the diameter of the LCFAa at the origin, 5 = the diameter of the LCFAt at the origin, 6 = the diameter of the LCFAd at the origin
Results
The mean distance from the origin of the LCFA to the MIP was 59.45 ± 13.06 mm and from the LCFA to the DFA was 19.23 ± 9.63 mm.
The mean diameters of the LCFA, LCFAa, LCFAt and LCFAd were 5.82 ± 1.87 mm, 3.28 ± 0.87 mm, 3.02 ± 0.92 mm, 3.61 ± 0.98 mm, respectively. All data are shown in Table 1, the minimum, maximum and mean values are shown in Table 2.
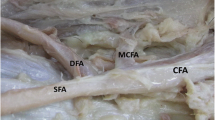
In one of the extremities (3.8%), an accessory transverse branch was found that originated from the LCFA. This branch directed laterally to pass anterior to the vastus intermedius. It gave off a muscular branch to the vastus lateralis, and then pierced this muscle wound around the femur (Fig. 2).
a A diagram of the extra transverse branch mentioned above. b Picture of the left thigh of a male cadaver. FA = femoral artery, DFA = deep femoral artery, LCFA = lateral circumflex femoral artery, LCFAa = ascending branch of LCFA, LCFAt1 = first transverse branch of LCFA, LCFAt2 = second transverse branch of LCFA, LCFAd = descending branch of LCFA, *muscular branch to the vastus lateralis
The LCFA originated from DFA in 21 (80.8%) cases and from FA in five (19.2%) cases. In 16 cases (61.5%) of LCFA originating from DFA, all branches (LCFAa, LCFAt, LCFAd) arose from the DFA as a common trunk (Fig. 3). In five cases, the LCFAd arose as a separate branch: two (7.6%) from DFA (Fig. 4) and three (11.5%) from FA (one proximal, two distal to origin of the DFA) (Fig. 5).
LCFA originating from the DFA as a single trunk (61.5%). Picture of the left thigh of a 67-year-old male. FA = femoral artery, DFA = deep femoral artery, LCFA = lateral circumflex femoral artery, LCFAa = ascending branch of the lateral circumflex femoral artery, LCFAt = transverse branch of the lateral circumflex femoral artery, LCFAd = descending branch of the lateral circumflex femoral artery
LCFA originating from the DFA and the LCFAd arising from the DFA as a separate branch (7.7%). Picture of the left thigh of a 70-year-old female. FA = femoral artery, DFA = deep femoral artery, LCFA = lateral circumflex femoral artery, LCFAa = ascending branch of the lateral circumflex femoral artery, LCFAt = transverse branch of the lateral circumflex femoral artery, LCFAd = descending branch of the lateral circumflex femoral artery
LCFA originating from the DFA and the LCFAd arising from the FA as a separate branch (11.5%). Picture of the left thigh of a 70-year-old female. FA = femoral artery, DFA = deep femoral artery, LCFA = lateral circumflex femoral artery, LCFAa = ascending branch of the lateral circumflex femoral artery, LCFAt = transverse branch of the lateral circumflex femoral artery, LCFAd = descending branch of the lateral circumflex femoral artery
Of the LCFA cases with FA origin, 4 originated from the proximal part of the FA before giving off the DFA and 1 originated from the distal part of the FA after giving off the DFA (Fig. 6). The LCFA with distal origin arose as a single trunk. In 3 cases of LCFA arising proximal to the FA, the LCFA arose as a single trunk (Fig. 7), and in 1 case, the LCFAd arose separately as a common trunk with the DFA (Fig. 8).
LCFA originating from the FA as a single trunk, after giving off the DFA (3.8%). Picture of the left thigh of a 75-year-old male. FA = femoral artery, DFA = deep femoral artery, LCFA = lateral circumflex femoral artery, LCFAa = ascending branch of the lateral circumflex femoral artery, LCFAt = transverse branch of the lateral circumflex femoral artery, LCFAd = descending branch of the lateral circumflex femoral artery
LCFA originating from the FA as a single trunk, before giving off the DFA (11.5%). Picture of the left thigh of a 75-year-old male. FA = femoral artery, DFA = deep femoral artery, LCFA = lateral circumflex femoral artery, LCFAa = ascending branch of the lateral circumflex femoral artery, LCFAt = transverse branch of the lateral circumflex femoral artery, LCFAd = descending branch of the lateral circumflex femoral artery
LCFA originating proximal to the FA and LCFAd arising distally as a common trunk with the DFA (3.8%). Picture of the left thigh of a 67-year-old man. FA = femoral artery, DFA = deep femoral artery, LCFA = lateral circumflex femoral artery, LCFAa = ascending branch of the lateral circumflex femoral artery, LCFAt = transverse branch of the lateral circumflex femoral artery, LCFAd = descending branch of the lateral circumflex femoral artery
Cases in which LCFA originated from DFA are shown in Figs. 3, 4, 5; cases in which LCFA originated from FA are shown in Figs. 6, 7, 8.
The significance of the difference between the data of the right and left subinguinal region was analyzed with the Wilcoxon test; the results are shown in Table 3. Due to the limited number of female cadavers, the gender difference was not examined. Therefore, all data were evaluated as one pool.
Discussion
Embryology of the femoral artery
The arteries to the developing lower limbs are mainly derived from the fifth lumbar intersegmental artery. This artery initially supplies the limb bud by joining an axial or axis artery that develops along the central axis of the limb bud. In the lower limb, the axis artery (which arises as a distal continuation of the internal iliac artery) largely degenerates, and the definitive supply is provided almost entirely by the external iliac artery, which arises as a new branch of the fifth lumbar intersegmental artery, as mentioned above. The axis artery persists as three remnants: the small sciatic (ischiadic) artery, which supplies the sciatic nerve in the posterior thigh; a segment of the popliteal artery; and a segment of the fibular (peroneal) artery in the leg. The axial artery is the major artery of the early leg bud. Later in development it regresses through remodeling. The proximal part later (sciatic) receives a more specialized function, forming the sciatic nerve’s accompanying artery. The external iliac/femoral artery penetrates the lower limb after the axial artery, it temporarily joins the axial/sciatic artery in the region of the future popliteal artery. This connection is severed, and the dorsal thigh is supplied primarily by the deep femoral artery, which branches from the femoral artery. In the early embryonic period, variations in the capillary channels in the anastomotic networks formed between the femoral artery and the sciatic artery can be seen due to blood flow differences caused by unknown causes. The LCFA variation seen in the present case may have occurred in this way, but the mechanism of the variations has not yet been proven (Schoenwolf et al. 2015; Qazi et al. 2022).
Origins of the lateral circumflex femoral artery
LCFA frequently originates from the DFA and less frequently from the FA. We found that the LCFA originated from the DFA in 80.8% of cases, and from the FA in 19.2%. Among these, there were six cases where LCFAd arose as a separate branch (Fig. 4, Fig. 5, Fig. 8), and in five of them LCFAa and LCFAt originated from DFA as a common trunk, and based on these findings we accepted and reported that the origin of the LCFA is DFA. In one of these six cases, LCFAd had a common trunk with DFA and origin of LCFA is FA (Fig. 8). Results of the present study are similar to the results of the other researchers’ (Table 4). Our results were in agreement with Williams et al. (1934). We did not find a duplication or absence of LCFA as in Ma et al. (2021), Vuksanović-Božarić et al. (2018); however, in one of our cases we found an accessory LCFAt branch that we could not classify, and like which could not be found in literature searches (Fig. 2).
Mean distance of the origin of the lateral circumflex femoral artery from mid-inguinal point
The mean distance from the origin of the LCFA to the MIP was 59.45 ± 13.06 mm in our study. Considering the data presented by other researchers, Ma et al. (2021) divided the different types of LCFA into 7 groups and calculated and reported the mean of each of them. The shortest mean distance was reported as 17.26 ± 13.26 mm and the longest as 92.92 ± 4.40 mm. Tomaszewski et al., (2017) reported the measurements of the LCFA from DFA and FA separately as 51.06 mm and 38.79 mm, respectively. Totlis et al. (2020) measured the distance from the anterior superior iliac spine and reported the mean as 110 mm. Data on the distance from the origin of the LCFA to the MIP are presented in Table 5. The shortest distance in our study was 36.9 mm, which is close to the value reported by Tomaszewski et al. (2017). Prior to any medical intervention it should be taken into consideration that the distance of LCFA from MIP can vary greatly.
Mean distance of the origin of the lateral circumflex femoral artery from the origin of the deep femoral artery
Based on the data that LCFA most frequently originates from DFA, we measured the distance between the origins of DFA and LCFA. The mean distance was 19.23 ± 9.63 mm, regardless of whether the LCFA originated from the DFA or FA. Considering the data presented by other researchers, Prakash et al. (2010) reported the measurements of the LCFA from DFA and FA separately as 25 mm and 21 mm, respectively. Data on the distance of the origin of the LCFA from the origin of the DFA are shown in Table 6. Comparing the data presented by other researchers, the mean values are similar to our study. Prakash et al. (2010) and Tomaszewski et al. (2017) reported that in the cases that LCFA arose from FA were often of a proximal origin. Some of other researchers reported a common trunk of LCFA and DFA (Adachi 1928; Üzel et al. 2008; Tomaszewski et al. 2017). The shortest distance in our study was 0.1 mm and the longest was 37 mm which similar to Samarawickrama et al. (2009).
Mean diameter of the lateral circumflex femoral artery at the origin
The mean diameter of the LCFA at the origin was 5.82 ± 1.87 mm in our study. Data on the diameter of the LCFA at the origin are shown in Table 7. Considering the data presented by other researchers, the mean values are similar to ours. However, when we analyzed the data in the present study, it was observed that as the distance between the origin of the LCFA and the MIP increased, the diameter of the LCFA increased; and as the diameter of the LCFA increased, the diameters of the LCFAa, LCFAt and LCFAd increased. According to the nonparametric correlation we used if p < 0.05 and rs > 0.4 in Spearman analysis, this indicates a moderate correlation. The Spearman analysis for these increases in our study showed a significant correlation between these data (Fig. 9). Accordingly, the values in bold in Table 8 show the data with a significant correlation.
Mean diameter of the ascending branch of lateral circumflex femoral artery at the origin
The mean diameter at the origin of the LCFAa was 3.28 ± 0.87 mm in our study. Other researchers reported it as 2.6 mm (Choi et al. 2007), 3.1 mm (Xu et al. 1989), 2.7 mm (Kalandar and Morris 2019), 3.15 mm (Zhao et al. 2018). Totlis et al. (2020) reported it 2.9 mm and emphasized the possibility of damage and regional necrosis during hip arthroplasty. According to Liu et al. (2016) and Li et al. (2020) the use of LCFAa was reported to be a safe and effective method for locally vascularized bone grafts in the proximal femur.
Mean diameter of the transverse branch of lateral circumflex femoral artery at the origin
The mean diameter at the origin of the LCFAt was 3.02 ± 0.92 mm in our study. Other researchers reported it as 2.7 mm (Totlis et al. 2020), 2.4 mm (Choi et al. 2007). Rodaix et al. (2021) reported that the flap obtained by preserving the LCFAt instead of the classical vastus lateralis flap used in proximal femur resections, reduced morbidity. In the present study, we found an accessory transverse branch that originated from the LCFA and pierced the vastus lateralis. It also gave off a muscular branch to the vastus lateralis, and this branch ran between the descending and transverse branches of the LCFA and pierced the vastus lateralis (Fig. 2). In their study, Wong et al. (2009) referred to this muscular branch as the oblique branch type 2 and mentioned the advantages of using this branch in the anterolateral femoral flap.
Mean diameter of the descending branch of lateral circumflex femoral artery at the origin
The mean diameter at the origin of the LCFAd was 3.61 ± 0.98 mm in our study. Other researchers reported it as 2.9 mm (Choi et al. 2007), 3.4 mm (Luo et al. 2021), 2.9 mm (Loskot et al. 2016), 1.2 mm (Meric et al. 2014). In the study by Loskot et al. (2016), LCFAd’s lumen narrower than 2 mm was found in 9% of cases and was reported to be unsuitable for coronary artery bypass grafting. These studies agree that the LCFAd can be used as a coronary artery bypass graft. In addition, Gholami et al. (2021) examined the blood supply areas of the branches of the LCFA used as an anterolateral thigh perforator flap and reported that the most commonly used artery and the artery supplying blood to the tissue in the largest area was the LCFAd with a frequency of 66.7%.
Clinical significance of variations of lateral circumflex femoral artery
The branches of the LCFA are used in clinical applications; as an anterolateral pedicled tissue flap (Yang et al., 2023), in the reconstruction of knee defects (Dorfman and Pu 2013), as a tissue flap in scar contracture deformity of the hand and foot (Xiao et al. 2022), as a musculo-periosteal iliac tissue flap in femoral head necrosis, and to provide blood supply in vascularized iliac transplantation (Li et al. 2021), skull base reconstruction (Camporro et al. 2011), breast tissue reconstruction after mastectomy (Tuinder et al. 2014), oral and maxillofacial defect reconstruction (Gong et al. 2015), facial and neck region reconstruction (Park and Miles 2011), tissue reconstruction after oncologic resections (Brunetti et al. 2021). It can also be used in aorto-popliteal bypass surgery (Sugawara et al. 1998), coronary artery bypass surgery (Fukuda et al. 2005; Loskot et al. 2016), extracranial and intracranial bypass surgery (Ravina et al. 2018), as hepatic artery graft in liver transplantation (Hong et al. 2021), and as collateral artery in blood supply deficiency (Halvorson et al. 2008). In cases where an artery is going to be used as graft tissue, the adequacy of the blood supply of the region and the morphological structure of the artery should be examined and as reported by Tokumato et al. (2015) because of the links among peripheral vessels between the LCFAt and a LCFAd on the iliotibial tract it should be kept in mind. In case of insufficiency in other arterial structures due to various reasons, it should be taken into consideration that removal of an arterial branch that plays an active role in the blood supply of the region may cause necrosis in the thigh and leg or that the vessel may not be present in the planned location during the intervention. Therefore, it is recommended to use radiologic diagnostic methods such as angiography to investigate the branching characteristics and variations of the artery before the interventions (Hage and Woerdeman 2004; Liu et al. 2016). In our study, we aimed to show the branching characteristics and diameters of the LCFA in our cadavers and provide data to the literature in this region.
Conclusion
The mean distance from the origin of the DFA to the MIP was 42.88 ± 16.39 mm, from the origin of the LCFA to the MIP was 59.45 ± 13.06 mm, from the origin of the LCFA to the DFA was 19.23 ± 9.63 mm, the mean diameter of the LCFA at the origin was 5.82 ± 1.87 mm, LCFAa at the origin was 3.28 ± 0.87 mm, LCFAt at the origin was 3.02 ± 0.92 mm and LCFAd at the origin was 3.61 ± 0.98 mm.
We found that the LCFA frequently originates from the DFA (80.8%) and sometimes from the FA (19.2%); its branches can arise as separate branches from both arteries. We also found in one extremity, that DFA and LCFAd arising from a common stem. In another one extremity, we found an accessory transverse branch of LCFA.
When the data obtained in this study were compared with other researchers’, the mean values were found to be similar. In addition, Spearman’s analysis showed that as the distance between the origin of the LCFA and the MIP increased, the diameter of the LCFA and accordingly the diameter of its branches increased, which is accepted significant. In accordance with the literature, we found cases with typical morphology, but we have also met cases with more complex and different morphologies of LCFA. The LCFA variability plays an important role for flaps, and arterial grafts, therefore this variability should be kept in mind during surgical approaches in this region. Anatomical knowledge is crucial for clinicians to avoid iatrogenic injuries when performing procedures in the femoral region, and thus radiographic assessment prior to surgery is recommended.
Data availability
The data that support the findings of this study are openly available in figshare at https://doi.org/10.6084/m9.figshare.26395999.
References
Adachi B (1928) Das Arteriensystem der Japaner, vol II. Verlag der Kaiserlich, Kyoto
Başar R et al (2002) Distinct intergender difference in the femoral artery ramification patterns found in the Turkish population: angiographic study. Anat Sci Int/japanese Assoc Anat 77(4):250–253. https://doi.org/10.1046/j.0022-7722.2002.00015.x
Brunetti B et al (2021) Versatility of the lateral circumflex femoral artery sparing perforator-based anterolateral thigh flaps in loco-regional thigh reconstruction after skin cancer, melanoma, and sarcoma resection. Microsurgery. https://doi.org/10.1002/MICR.30836
Camporro D et al (2011) Use of lateral circumflex femoral artery system free flaps in skull base reconstruction. J Craniofacial Surg 22(3):888–893. https://doi.org/10.1097/SCS.0b013e3182139cae
Choi SW et al (2007) An anatomic assessment on perforators of the lateral circumflex femoral artery for anterolateral thigh flap. J Craniofacial Surg 18(4):866–871. https://doi.org/10.1097/scs.0b013e3180a03304
Dixit D et al (2011) A study of variations in the origin of profunda femoris artery and its circumflex. Int J Biol Med Res 2(4):1084–1089
Dorfman DW, Pu LLQ (2013) Using the descending branch of the lateral circumflex femoral artery and vein as recipient vessel for free tissue transfer to the difficult areas of the lower extremity. Ann Plast Surg 70(4):397–400. https://doi.org/10.1097/SAP.0b013e3182853d49
Fukuda H et al (2005) Anatomical variants of the lateral femoral circumflex artery: an angiographic study. Surgical and Radiologic Anatomy : SRA 27(3):260–264. https://doi.org/10.1007/S00276-004-0312-5
Gholami M et al (2021) Anatomical variations of anterolateral thigh flap: a fresh cadaver dissection study. World J Plastic Surg 10(3):18–24. https://doi.org/10.52547/wjps.10.3.18
Gong ZJ et al (2015) Chimeric flaps pedicled with the lateral circumflex femoral artery for individualised reconstruction of through-and-through oral and maxillofacial defects. Br J Oral Maxillofac Surg 53(2):148–152. https://doi.org/10.1016/j.bjoms.2014.10.017
Hage JJ, Woerdeman LAE (2004) Lower limb necrosis after use of the anterolateral thigh free flap: is preoperative angiography indicated? Ann Plast Surg 52(3):315–318. https://doi.org/10.1097/01.sap.0000100422.66597.13
Halvorson EG, Taylor HOB, Orgill DP (2008) Patency of the descending branch of the lateral circumflex femoral artery in patients with vascular disease. Plast Reconstr Surg 121(1):121–129. https://doi.org/10.1097/01.prs.0000293862.68476.97
Hong QE et al (2021) Use of the descending branch of the lateral circumflex femoral artery as an arterial graft in living donor liver transplant. Transpl Proc 53(7):2335–2338. https://doi.org/10.1016/j.transproceed.2021.07.015
İbiş, EC 2022, ‘Yetişkin kadavralarında arteria circumflexa femoris lateralis’in morfolojisi’, Tıpta Uzmanlık Tezi, İstanbul Üniversitesi-Cerrahpaşa, Cerrahpaşa Tıp Fakültesi, İstanbul, Türkiye. Available at: https://tez.yok.gov.tr/UlusalTezMerkezi/tezSorguSonucYeni.jsp
Kalandar A, Morris SF (2019) Three-dimensional vascular anatomical study of the tensor fasciae latae muscle and perforators. J Reconstr Microsurg 35(6):389–394. https://doi.org/10.1055/S-0038-1677010/ID/JR180116-18/BIB
Łabętowicz P et al (2019) A morphological study of the medial and lateral femoral circumflex arteries: a proposed new classification. Folia Morphologica (poland) 78(4):738–745. https://doi.org/10.5603/FM.a2019.0033
Li Z et al (2020) Repair of massive bone defects of the proximal femur using iliac bone flaps of the ascending branch of the lateral circumflex femoral artery: a retrospective report. Ann Plastic Surg 84(5S Suppl 3):S235–S240. https://doi.org/10.1097/SAP.0000000000002361
Li BR et al (2021) Clinical application of the musculoperiosteal iliac flap for osteonecrosis of the femoral head. Ann Plast Surg 87(6):e129–e136. https://doi.org/10.1097/SAP.0000000000003007
Lippert H, Pabst R (1985) Arterial variations in man classification and frequency, 1st edn. J. F. Bergmann Verlag München, München
Liu YP et al (2016) Hemodynamic changes in osteonecrosis treatment of the femoral head with iliac bone flaps pedicled with the lateral femoral circumflex artery ascending branch: a 10-year report. Technol Health Care 24(6):S493–S498. https://doi.org/10.3233/THC-161173
Loskot P et al (2016) The descending branch of the lateral circumflex femoral artery as an alternative conduit for coronary artery bypass grafting: experience from an anatomical, radiological and histological study. Clin Anat 29(6):779–788. https://doi.org/10.1002/ca.22737
Luo XJ et al (2021) Application of the descending branch of the lateral circumflex femoral artery in coronary artery bypass grafting. J Thorac Cardiovasc Surg 161(4):1266–1271. https://doi.org/10.1016/J.JTCVS.2019.09.172
Ma M et al (2021) An analysis of the variations and clinical applications of the lateral circumflex femoral artery. Folia Morphologica (poland) 80(3):557–566. https://doi.org/10.5603/FM.a2020.0094
Meric G, et al (2014) ‘Descending branch of the lateral circumflex femoral artery as a recipient vessel for vascularized fibular grafts: clinical case series’. https://doi.org/10.1002/micr.22299
Park CW, Miles BA (2011) The expanding role of the anterolateral thigh free flap in head and neck reconstruction. Curr Opin Otolaryngol Head Neck Surg 19(4):263–268. https://doi.org/10.1097/MOO.0b013e328347f845
Patel S et al (2022) A novel clinically based classification system for the profunda femoris artery and the circumflex femoral arteries. Ann Vasc Surg. https://doi.org/10.1016/J.AVSG.2022.03.001
Prakash et al (2010) Variations in the origins of the profunda femoris, medial and lateral femoral circumflex arteries: a cadaver study in the Indian population. Rom J Morphol Embryol 51(1):167–170
Qazi E et al (2022) Arteries of the lower limb—embryology, variations, and clinical significance. Can Assoc Radiol J 73(1):259–270. https://doi.org/10.1177/08465371211003860/ASSET/IMAGES/10.1177_08465371211003860-IMG1.PNG
Ravina K et al (2018) Occipital artery to posterior cerebral artery bypass using descending branch of the lateral circumflex femoral artery graft for treatment of fusiform, unruptured posterior cerebral artery aneurysm: 3-dimensional operative video. Operative Neurosurg 15(5):E50–E51. https://doi.org/10.1093/ons/opy057
Rodaix C et al (2021) The proximal vastus lateralis flap: an anatomical and radiological study. Morphologie: Bulletin De L’association Des Anatomistes 106(353):75–79. https://doi.org/10.1016/j.morpho.2021.02.011
Samarawickrama M et al (2009) Branching pattern of the femoral artery at the femoral triangle: a cadaver study. Galle Medical Journal 14(1):31. https://doi.org/10.4038/gmj.v14i1.1169
Schoenwolf GC et al (2015) Larsen’s humanembryology, 5th edn. Elsevier, Cham
Siddharth P et al (1985) Variational anatomy of the deep femoral artery. Anat Rec 212(2):206–209. https://doi.org/10.1002/ar.1092120216
Standring S (2021) Gray’s anatomy e-book: the anatomical basis of clinical practice. Elsevier Health Sciences
Sugawara Y et al (1998) Utilization of the lateral circumflex femoral artery as a midway outflow for aorto-popliteal grafting: report of a case. Surg Today 28(9):967–970. https://doi.org/10.1007/s005950050264
Tokumato H et al (2015) An anatomical and histological study of the vascularized iliotibial tract graft. Microsurgery. https://doi.org/10.1002/micr
Tomaszewski KA et al (2017) The variable origin of the lateral circumfloex femoral artery: a meta-analysis and proposal for a new classification system. Folia Morphologica (poland) 76(2):157–167. https://doi.org/10.5603/FM.a2016.0056
Totlis T et al (2020) Surgical anatomy of the lateral circumflex femoral artery branches: contribution to the blood loss control during hip arthroplasty. Ann Anat 232:151566. https://doi.org/10.1016/j.aanat.2020.151566
Tuinder S et al (2014) Septocutaneous tensor fasciae latae perforator flap for breast reconstruction: radiological considerations and clinical cases. J Plast Reconstr Aesthet Surg 67(9):1248–1256. https://doi.org/10.1016/J.BJPS.2014.05.008
Turan B et al (2022) Morphological investigation of deep femoral artery variations using multidetector computed tomography angiography. Acta Chir Belg. https://doi.org/10.1080/00015458.2022.2092962
Üzel M, Tanyeli E, Yildirim M (2008) An anatomical study of the origins of the lateral circumflex femoral artery in the Turkish population. Folia Morphol 67(4):226–230
Vazquez T et al (2007) Patterns of the circumflex femoral arteries revisited. Clin Anat 20(2):180–185. https://doi.org/10.1002/ca.20336
Vuksanović-Božarić A et al (2018) Clinical significance of understanding lateral and medial circumflex femoral artery origin variability. Anat Sci Int 93(4):449–455. https://doi.org/10.1007/s12565-018-0434-1
Williams GD, Martin CH, McIntire LR (1934) Origin of the deep and circumflex femoral group of arteries. Anat Rec 60(2):189–196. https://doi.org/10.1002/AR.1090600206
Wong CH et al (2009) Alternative vascular pedicle of the anterolateral thigh flap: the oblique branch of the lateral circumflex femoral artery. Plast Reconstr Surg 123(2):571–577. https://doi.org/10.1097/PRS.0b013e318195658f
Xiao S et al (2022) Application of thin free lateral femoral circumflex artery perforator flap in repair of scar contracture deformity in hand and foot. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi = Zhongguo Xiufu Chongjian Waike Zazhi = Chine J Reparative Reconstr Surg 36(2):220–223. https://doi.org/10.7507/1002-1892.202109065
Xu DC, Kong JM, Zhong SZ (1989) The ascending branch of the lateral circumflex femoral artery. Surg Radiol Anat 11(4):263–264. https://doi.org/10.1007/bf02098692
Yang L et al (2023) Morphological study of branches of lateral femoral circumflex artery based on digital subtraction angiography. J Plastic, Reconstr Aesthet Surg : JPRAS. https://doi.org/10.1016/J.BJPS.2022.08.075
Zhao D et al (2018) Pedicled iliac crest bone flap transfer for the treatment of upper femoral shaft fracture nonunion: an anatomic study and clinical applications. Microsurgery 38(8):882–888. https://doi.org/10.1002/MICR.30278
Acknowledgements
The authors would like to express their sincere gratitude to those who have donated their bodies to science so that anatomical research can be conducted. The results of such research have the potential to improve patient care and increase human knowledge. Therefore, these donors and their families deserve our highest gratitude.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
ECI: Manuscript writing—review & editing, Project administration, Data collection and management, Dissection and photographic documentation, Data analysis. ET: Project development, Data management, Manuscript writing—review & editing. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. All authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
İbiş, E.C., Tanyeli, M.E. Morphology of the lateral circumflex femoral artery in adult cadavers. Anat Sci Int (2024). https://doi.org/10.1007/s12565-024-00791-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12565-024-00791-5