Abstract
The descending branch of the lateral femoral circumflex artery (LFCA) has found recent use as a new arterial graft for coronary artery bypass grafting (CABG). Anatomical variants of the LFCA were assessed on femoral arteriograms obtained before CABG in 131 adult patients. The most common pattern, found in 78.6% of extremities, consisted of the LFCA arising from the deep femoral artery, and the arterial graft was selected from this pattern in 92.3% of patients in whom the descending branch of the LFCA was used for CABG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The lateral femoral circumflex artery (LFCA) commonly originates from the deep femoral artery (DFA), and the descending branch of the LFCA has recently been recognized as a new arterial graft for use in coronary artery bypass grafting (CABG) [5, 17]. Because of anatomical variants of the LFCA and individual differences in development of the descending branch of the LFCA, it is necessary to perform bilateral femoral arteriography before surgery for patients in whom use of the LFCA might be justified as an arterial graft [6]. In this study, we review the anatomical variants of the LFCA on angiograms obtained before CABG. Although anatomical variants of the DFA on lower limb angiograms have been reviewed by Massoud et al. [12] and Basar et al. [3], there is no other radiological literature in which anatomical variants of the LFCA have been investigated in relation to preoperative arteriographic evaluation for CABG.
Materials and methods
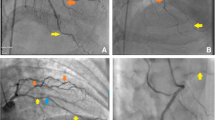
From November 1998 to December 2003, we performed preoperative digital subtraction femoral arteriography in 132 patients to assess the appropriateness of the LFCA as an arterial graft for CABG. Femoral angiography was only performed on patients from whom it was possible to acquire an arterial graft from the LFCA, such as those with multivessel disease, and was not performed for patients with suspected arteriosclerosis obliterans of the lower extremities, because the LFCA is indispensable as a contributor to the collateral circulation. Of the 132 patients upon whom femoral angiography was performed, 1 was subsequently excluded because complete occlusion of the right femoral artery (FA) became apparent. Therefore, femoral arteriograms were reviewed for 262 extremities in 131 patients, 121 males and 10 females, 32–78 years old (mean, 60.2 years old). A total of 10–15 ml of 370 mgI/ml iopamidol (Iopamiron 370, Nihon Shering, Osaka, Japan) was administered into the ipsilateral external iliac artery at a rate of 2–3 ml/s, and bilateral femoral arteriograms were then obtained separately for each side, acquiring data at three frames/s using an Advantx LCA (General Electric Medical Systems, Milwaukee, WI). The images were stored in hard copy and also on videotape. All of the femoral arteriograms were reviewed by one experienced radiologist (H.F.) in order to analyze anatomical variants of the LFCA. The angiograms were evaluated using the hard copy images, and additionally from videotape when the origin of the LFCA was obscure because of superimposition of the FA and the DFA (Fig. 1). We classified the patterns of anatomical variation of the LFCA into six types according to the origin of the LFCA, as shown in Fig. 2. The anatomical variation of the 26 LFCAs that were used as an arterial graft for CABG in 26 patients was further assessed as a sub-group.
Patterns of anatomical variation of the LFCA. Type D: the LFCA originates from the DFA, including a pattern in which the LFCA originates from the DFA and a major branch of the LFCA arises separately from the DFA; type F1: the LFCA originates from the FA above the origin of the DFA; type F2: the LFCA originates from the FA below the origin of the DFA; type F3: the LFCA originates from the FA above the origin of the DFA and a major branch of the LFCA arises from the FA below the origin of the DFA; type DF1: the descending branch of the LFCA originates from the FA above the origin of the DFA and the ascending branch of the LFCA arises from the DFA; type DF2: the LFCA originates from the DFA and a major branch of the LFCA arises from the FA below the origin of the DFA. D DFA; F FA; L LFCA; La the ascending branch of the LFCA; Ld the descending branch of the LFCA
Results
The patterns of anatomical variation of the LFCA in the 262 extremities studied were as follows: type D in 206 extremities (78.6%, Fig. 3), type F1 in 27 (10.3%, Fig. 4a), type F2 in 14 (5.3%, Fig. 5), type F3 in 4 (1.5%, Fig. 4b), type DF1 in 3 (1.1%, Fig. 6a) and type DF2 in 8 (3.1%, Fig. 6b). The patterns of anatomical variation of the 26 LFCAs that were used as an arterial graft for CABG were: type D in 24 (92.3%), type F1 in 1 (3.8%) and type F2 in 1 (3.8%). Hence, the type D LFCA was most commonly chosen as an arterial graft for CABG, although there was no significant difference between the frequency of type D LACAs in the overall population and in the sub-group of LFCAs chosen for use in CABG ( P =0.10, chi-square test).
Discussion
In the field of plastic and reconstructive surgery, the LFCA has often been used to supply composite tissue as an anterolateral thigh flap [8, 9, 14], and in the field of cardiovascular surgery the LFCA has been recognized as a new arterial conduit for CABG [5], since Tatsumi et al. [17] first reported a case in which the descending branch of the LFCA was used as an arterial free graft for CABG. Since there are anatomical variants and individual differences in properties such as length and diameter of the branches of the LFCA, arteriographic evaluation of the LFCA is necessary before use [6]. At our institution, the descending branch of the LFCA has been used as an arterial graft for CABG since 1997, and since that time bilateral femoral arteriography has been performed before surgery for patients in whom the use of the LFCA might be justified. Based on the preoperative femoral arteriograms, we have analyzed anatomical variations of the LFCA by reviewing arteriograms from procedures performed since November 1998, when our latest angiographic instrument, which allows retrospective review using videotape, was installed.
The origin of the LFCA was frequently obscure in the hard copy images because the DFA and FA were superimposed anteroposteriorally [10, 12, 13]. In such cases, a frame with lower contrast was developed from videotape to identify the precise origin of the LFCA (Fig. 1). Massoud et al. [12] have reviewed digital subtraction aortograms performed for demonstration of lower limb arteries in order to assess anatomical variants of the DFA. In the current study, we performed bilateral femoral arteriography separately on each side and additionally analyzed the variations using videotape, which permitted a more accurate anatomical evaluation.
As there was a tendency that the internal mammary artery [11], the radial artery [1] and the right gastroepiploic artery [16] were more frequently selected as an arterial graft than the LFCA in our institution, only 26 LFCAs were used for CABG in 26 of the 131 patients (19.8%). The type D LFCA occurred much more commonly (78.6%) than any of the other patterns, and LFCAs of type D were most commonly chosen as an arterial graft for CABG (92.3%), although there was no significant difference between the frequency of type D LFCAs in the overall group and that in the sub-group chosen for use in CABG ( P =0.10). One possible explanation for this finding is that LFCA variants other than type D are prone to develop an immature descending branch. It might be possible when an LFCA originates from two regions, such as a type F3, type DF1 or type DF2, that each branch tends to be underdeveloped. Indeed, no LFCA of type F3, type DF1 or type DF2 was applied as an arterial graft. On the other hand, since the appropriateness of an LFCA for use as an arterial graft for CABG is evaluated individually, and other factors also play a role in the decision, even a well-developed descending branch of a LFCA is not always used for arterial grafting. Hence, the usage frequency does not necessarily represent the degree of development of the descending branch of the LFCA. We did not perform quantitative or qualitative analysis of the degree of development of the descending branch of each LFCA.
Previous articles have classified anatomical variation of the DFA based on patterns of the LFCA and the medial femoral circumflex artery (MFCA) [2, 3, 10, 12, 13, 15, 18]. Although the MFCA is a significant artery in surgery of the proximal femur or hip [7], preoperative angiographic evaluations of the MFCA are not commonly used. In addition, identification of the origin of the MFCA on the angiogram is often difficult, since the MFCA is a smaller branch than the LFCA. Hence, we focused on the LFCA, since in addition this has recently been used as an arterial graft for CABG [5, 17], and preoperative anatomical assessment through arteriographic evaluation of the LFCA is now clinically indispensable in such procedures [6].
The type F3 LFCA has not been reported in the previous English literature illustrating schemata of anatomical patterns [3, 10, 12, 13, 18]. Type F3 LFCAs might previously have been categorized as type F1, because of failure to demonstrate that the branch of the LFCA originates from the FA below the origin of the DFA when using older angiography techniques with lower resolution [3, 12]. There might have been no discrimination between the FA above and below the origin of the DFA in previous reports [2, 18]. For example, the schemata described by Williams et al. [18] showing the LFCA, the descending branch of the LFCA and the DFA derived from the FA in order, defined as type 1b and type 1c, might have included the type F3 classification. In the Japanese literature, Emura et al. [4] reported a case with an illustration of a variant pattern in accordance with a type F3 LFCA. In Adachi [2], a German anatomical textbook that was based on Japanese data, there are no illustrated schemata of anatomical patterns of the FA. Patterns in which the DFA and the MFCA make a common trunk and the LFCA originates directly from the FA, and in which the DFA, MFCA and LFCA all originate separately from the FA, might have included the type F3 LFCA.
All patients in the present study were Japanese, and most were male, because they were recruited from ischaemic heart disease patients who were eligible for CABG. The frequency of patterns other than type D that are defined as having an LFCA of direct origin from the FA was 21.4%, a similar result to that obtained (21.8%) by Adachi [2], also based on Japanese data (no data regarding gender were given by Adachi). Williams et al. [18] mentioned that the frequency of LFCAs of direct origin from the FA was 23.1% for white males, 23.1% for white females, 24.1% for black males and 23.3% for black females, indicating insignificant sex or race differences. Basar et al. [3] have reported conflicting results, suggesting that in Turkey the frequency of LFCAs of direct origin from the FA was significantly higher in women (46.2%) than in men (19.7%). No significant left- or right-sided predominance has been reported regarding the direct origin of the LFCA [15, 18].
Conclusion
We have presented anatomical data regarding the LFCA. The most common pattern consisted of an LFCA arising from the DFA, and there was a tendency for selection of LFCAs with such a pattern as arterial grafts for use in CABG.
References
Acar C, Jebara VA, Portoghese M, Beyssen B, Pagny JY, Grare P, Chachques JC, Fabiani JN, Deloche A, Guermonprez JL (1992) Revival of the radial artery for coronary bypass grafting. Ann Thorac Surg 54:652–659
Adachi B (1928) Drei Hauptäste der A. femoralis. In: Das Arteriensystem der Japaner, Band II. Kaiserlich-Japanischen Universtät zu Kyoto, Kyoto, pp 147–153
Basar R, Sargon MF, Cumhur M, Bayramoglu A, Demiryurek D (2002) Distinct intergender difference in the femoral artery ramification patterns found in the Turkish population: angiographic study. Anat Sci Int 77:250–253
Emura S, Shoumura S, Ishizaki N, Yamahira T, Ito M, Chen HY, Isono H (1989) The anatomical study on the branches of the femoral artery (II): comparison with the findings of Adachi’s classification (in Japanese). Kaibogaku Zasshi 64:196–205
Fabbrocini M, Fattouch K, Camporini G, Demicheli G, Bertucci C, Cioffi P, Mercogliano D (2003) The descending branch of lateral femoral circumflex artery in arterial CABG: early and midterm results. Ann Thorac Surg 75:1836–1841
Faidutti B, Kalangos A (1999) Coronary artery bypass grafting with the descending branch of the lateral femoral circumflex artery used as an arterial conduit: Is arteriographic evaluation necessary before use? J Thorac Cardiovasc Surg 117:1229–1230
Gautier E, Ganz K, Krugel N, Gill T, Ganz R (2000) Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br 82:679–683
Koshima I, Fukuda H, Yamamoto H, Moriguchi T, Soeda S, Ohta S (1993) Free anterolateral thigh flaps for reconstruction of head and neck defects. Plast Reconstr Surg 92:421–428
Koshima I, Yamamoto H, Hosoda M, Moriguchi T, Orita Y, Nagayama H (1993) Free combined composite flap using the lateral circumflex femoral system for repair of massive defects of the head and neck regions: an introduction to the chimeric flap principle. Plast Reconstr Surg 92:411–420
Lippert H, Pabst R (1985) The profunda femoris artery. In: Arterial variations in man: classification and frequency. Bergman, Munich, p 61
Loop FD, Lytle BW, Cosgrove DM, Stewart RW, Goormastic M, Williams GW, Golding LA, Gill CC, Taylor PC, Sheldon WC (1986) Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med 314:1–6
Massoud TF, Fletcher EW (1997) Anatomical variants of the profunda femoris artery: an angiographic study. Surg Radiol Anat 19:99–103
Siddharth P, Smith NL, Mason RA, GironF (1985) Variational anatomy of the deep femoral artery. Anat Rec 212:206–209
Song YG, Chen GZ, Song YL (1984) The free thigh flap: a new free flap concept based on septocutaneous artery. Br J Plast Surg 37:149–159
Suder E, Nizankowski C (1985) Variations in the origin of the deep femoral arteries in human fetuses. Folia Morphol 44:262–269
Suma H, Wanibuchi Y, Terada Y, Fukuda S, Takayama T, Furuta S (1993) The right gastroepiploic artery graft. Clinical and angiographic midterm results in 200 patients. J Thorac Cardiovasc Surg 105:615–622
Tatsumi TO, Tanaka Y, Kondoh K, Minohara S, Sawada Y, Tsuchida T, Tajima S, Sasaki S (1996) Descending branch of lateral femoral circumflex artery as a free graft for myocardial revascularization: a case report. J Thorac Cardiovasc Surg 112:546–547
Williams GD, Martin CH, McIntire LR (1934) Origin of the deep and circumflex group of arteries. Anat Rec 60:189–196
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fukuda, H., Ashida, M., Ishii, R. et al. Anatomical variants of the lateral femoral circumflex artery: an angiographic study. Surg Radiol Anat 27, 260–264 (2005). https://doi.org/10.1007/s00276-004-0312-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-004-0312-5