Abstract
Coronary artery anomalies range in prevalence from 0.2 to 2.3 % of the population. They range from benign incidental findings to an important cause of sudden cardiac death (SCD). In fact, coronary anomalies are the second leading cause of SCD in athletes and are responsible for ∼30 % of SCD in the young. Clinically, anomalous coronary arteries arising from the opposite sinus and anomalous left coronary artery arising from the pulmonary artery are the most important as they are associated with the highest risk of mortality. Several high-risk features and their pathophysiology are reviewed. Multiple imaging modalities have been utilized to study coronary artery anomalies; however, coronary computed tomography angiography (CTA) is uniquely suited to characterize coronary artery anomalies as it allows for clear elucidation of origin, course, and termination in relationship to other relevant anatomy with high spatial resolution. This paper will provide an overview of the wide spectrum of coronary artery anomalies and variants, review the most relevant coronary CTA imaging features for each, and differentiate benign from malignant varieties.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Collectively, anomalous coronary arteries and variants are estimated to have a prevalence of 0.2–2.3 % [1•, 2, 3••, 4]. However, the true prevalence of these conditions is unknown since detection is subject to referral bias and the work-up is usually prompted by suspicion for coronary artery disease or a coronary anomaly. Importantly, coronary anomalies are the second most common cause of mortality in competitive athletes (after hypertrophic cardiomyopathy) and are associated with ∼30 % of sudden cardiac death (SCD) in young adults [5, 6]. Historically, conventional coronary angiography (CCA) has been considered the gold standard for detecting coronary artery anomalies. However, CCA is an invasive procedure and it only detects about half of coronary artery anomalies [7, 8]. Other modalities such as cardiac MRI (CMR) elucidate the proximal coronary artery but lack the spatial resolution needed to define the entire course. Conversely, coronary computed tomography angiography (CTA) is well suited to characterize the coronary origin, course, and termination with superb spatial and temporal resolution. Additionally, it has the advantage of defining the anomalous coronary arteries relative to other important anatomic structures, such as the great vessels. There is increasing recognition of the utility of coronary CTA for this purpose. Recommendations for the use of coronary CTA in the evaluation of anomalous coronary arteries have been incorporated into ACC/AHA Guidelines and Appropriate Use Criteria [9, 10].
Variants vs Anomalies
The distinction between a coronary anomaly and a variant is defined by population prevalence. By definition, coronary artery anomalies are present in <1 % of the population and normal variants are found in >1 % of the population [11]. However, several studies have demonstrated a higher prevalence of certain coronary “anomalies” [4, 12, 13] (Table 1). Fortunately, many anomalies are benign and serve simply as incidental findings without prognostic relevance. The current discussion will focus on the most clinically relevant coronary anomalies. Clearly, individuals who interpret coronary CTA studies need to be familiar with the entire spectrum of coronary anomalies in order to differentiate those that are benign from those that are malignant.
Prevalence of Coronary Anomalies in Congenital Heart Disease
This review focuses on isolated coronary artery anomalies, not in the setting of concomitant congenital heart disease. However, coronary anomalies are found much more commonly in the setting of congenital heart disease with a prevalence as high as 36 % in single ventricle patients and 15 % overall in a diverse group of congenital heart disease subtypes [14].
Anomalies of Origin and Course
The majority of coronary anomalies fall within this group. This group is further divided into three subcategories: absent left main coronary artery, anomalous coronary ostium outside of the aortic sinuses, and anomalous origin of a coronary artery from the opposite sinus (ACAOS).
Absent Left Main Coronary Artery
Absent left main coronary artery is characterized by separate ostia for the left anterior descending artery and the left circumflex. It is associated with a higher proportion of left dominant coronary circulation and myocardial bridging. The prevalence of this benign anomaly is estimated at 0.4 % in one series [15].
Anomalous Coronary Ostium Outside of the Aortic Sinuses
The spectrum of coronary ostial anomalies and variants outside of the aortic sinuses is broad, ranging from clinically benign conditions to those that result in early mortality, often within the first year of life if corrective surgery is not pursued early. Some variants, such as superior takeoff of the right coronary artery, are common (8.7 %) and are unlikely to be of clinical significance [1•]. Other anomalies such as coronary origins from the left ventricular outflow tract, ascending aorta (Fig. 1), and brachiocephalic or subclavian arteries are found less commonly, and their clinical significance is uncertain.
A 71-year-old male underwent non-invasive coronary evaluation for chest pain. a An oblique axial maximum intensity projection image demonstrates the superior origin of the right coronary artery (arrow) from the ascending aorta at the level of the right pulmonary artery. b A three-dimensional volume-rendered image demonstrates the superior takeoff of the right coronary artery above the right sinus of Valsalva (arrow) with normal origin of the left coronary artery. Ao aorta, RPA right pulmonary artery
Patients with anomalous origin of the left coronary artery from the pulmonary artery (ALCAPA) typically present in the first few months of life with angina-like episodes and/or cardiomyopathy [16]. This condition occurs in 1 in 300,000 live births and, if untreated, is associated with a 1-year mortality ranging from 35 to 90 % as a result of progressive heart failure or life-threatening arrhythmia [16, 17]. ALCAPA pathophysiology results in myocardial ischemia as a result of coronary steal. The right coronary with a normal course is perfused at aortic diastolic pressure which then flows down a pressure gradient through collaterals to the left coronary artery and ultimately to the pulmonary artery whose maximum pressure is the pulmonary artery systolic pressure (typically less than half the aortic diastolic pressure). Rare individuals with ALCAPA can develop very robust collaterals and thus present later in childhood or adulthood with angina or SCD [16, 18]. ALCAPA can be repaired with direct coronary re-implantation or intrapulmonary or extrapulmonary baffling of the left coronary artery. Direct coronary re-implantation appears to have the least post-operative complications but is not always feasible when the length of the coronary artery is insufficient [19]. Intrapulmonary baffling commonly leads to suprapulmonary stenosis (16 of 21 patients) or baffle leaks (11 of 21 patients) [19].
Anomalous origin of the right coronary artery from the pulmonary artery (ARCAPA) (Fig. 2) is found less commonly than ALCAPA with an estimated prevalence of only 0.002 % in the general population. It can manifest with a presentation similar to ALCAPA with heart failure or sudden cardiac death in infancy. However, patients with ARCAPA typically present later (average age at diagnosis 22.8 years) with signs of ischemia or during an evaluation for a murmur [20] (Fig. 2).
A 52-year-old male presents with dyspnea on exertion. An evaluation led to a coronary CTA. a The maximum intensity projection image demonstrates the anomalous right coronary artery arising directly from the pulmonary artery (ARCAPA) (arrow). b The three-dimensional volume-rendered image demonstrates a markedly dilated and tortuous left anterior descending artery (arrow) that supplies extensive collaterals to the anomalous right coronary artery (arrowhead) arising from the pulmonary artery. PA pulmonary artery, Ao aorta
ACAOS
ACAOS comprises a large group of coronary anomalies that is of utmost clinical importance. This condition has received a great deal of attention as an important cause of SCD in competitive athletes and young adults. For most clinicians, it represents the entity that is evoked during a discussion of anomalous coronary arteries. The prevalence estimates of ACAOS by echocardiography, coronary CTA, CMR, CCA, and autopsy range widely from 0.15 [21] to 2.1 % [2, 22]. The prevalence of coronary anomalies and specifically ACAOS has been reported extensively (Table 1) [1•, 2, 3••, 13, 22, 23••, 24–30]. Since patients undergoing diagnostic tests that identify ACAOS typically have symptoms prompting the referral, the true population prevalence of ACAOS is expected to be lower than reported prevalence estimates. Indeed, the few large studies that have prospectively evaluated asymptomatic patients found the incidence of ACAOS to be much lower at 0–0.17 % [31–33]. Younger cohorts with ACAOS are commonly asymptomatic. However, as these patients age, chest pain, myocardial infarction, and arrhythmia become more common [3••]. Significant interest has been focused on identifying the anatomical and pathophysiological features that predict these adverse outcomes.
Extensive classification systems have been developed [12] but ACAOS is typically grouped into four main categories (Fig. 3): left main coronary artery from the right sinus of Valsalva, left anterior descending artery from the right sinus of Valsalva (Fig. 4), left circumflex from the right sinus of Valsalva or, more commonly, right coronary artery (Fig. 5) [34•], and right coronary artery from the left sinus of Valsalva (Table 2). The proximal course of the anomalous coronary is further categorized into interarterial (between the aortic root and pulmonary artery) (Fig. 6), anterior (prepulmonic) (Fig. 7), intraseptal (subpulmonic) (Fig. 8), and posterior (retroaortic) (Fig. 9) subtypes. A single coronary that supplies the left anterior descending, left circumflex, and right coronary arteries is extremely rare (Fig. 10). It shares some overlapping features with ACAOS, including a similar risk for ischemia and sudden cardiac death depending on its origin and course.
Normal coronary artery origin and course contrasted with several varieties of ACAOS. a Normal coronary artery origin and course. b Anomalous origin of the LCX from the RCA with a posterior (retroaortic) course; this is more commonly encountered than ACAOS of the LCX from the right sinus of Valsalva. c ACAOS of the LM with an anterior (prepulmonic) course. d ACAOS of the LM with a posterior (retroaortic) course. e ACAOS of the LM with a subpulmonic (intramyocardial) course. f ACAOS of the LM with an interarterial course. g ACAOS of the RCA with an interarterial course. LCX left circumflex coronary artery, RCA right coronary artery, LAD left anterior descending artery
A three-dimensional volume-rendered image demonstrates anomalous right coronary artery arising from the left anterior descending artery (arrow) as it courses anterior (prepulmonic) to the pulmonary artery. This coronary anomaly is considered benign and is not associated with a significant risk for sudden cardiac death or ischemia. Ao aorta, PA pulmonary artery
A 54-year-old male with multiple medical problems presented with intermittent, non-exertional chest pain and underwent coronary CTA. a A multiplanar reformatted thin maximum intensity projection image demonstrates the anomalous origin of the left circumflex (arrow) from the proximal right coronary artery with evidence of calcified atherosclerotic plaque. b, c The three-dimensional volume-rendered images demonstrate the posterior course (arrow) of the anomalous circumflex between the aorta and the left atrium. This anomaly does not carry an increased risk for sudden cardiac death but is associated with a high prevalence of atherosclerosis [34•]. Ao aorta, LA left atrium
A 55-year-old female presented with exertional syncope. The evaluation culminated in a coronary CTA that demonstrated an anomalous left main coronary artery arising from the right sinus of Valsalva and coursing between the aorta and pulmonary artery. a The three-dimensional volume-rendered image demonstrates the malignant interarterial course of the anomalous left main (arrow) coronary artery between the aorta and pulmonary artery (subtracted to visualize the left main). b The maximum intensity projection image demonstrates the acute angulation, slit-like ostium, and the anomalous course of the left main coronary artery (arrow) between the aorta and pulmonary artery. The interarterial form of ACAOS is associated with an intramural course that leads to coronary intussusception with exertion, luminal compression, critical reduction of flow, and an increased risk for sudden cardiac death. Ao aorta, PA pulmonary artery
Anomalous left main coronary artery arising from the right sinus of Valsalva and coursing anterior to the pulmonary artery discovered incidentally on coronary CTA during evaluation for atypical chest pain in a 47-year-old woman. a The maximum intensity projection image demonstrates the left main coronary artery arising from the right sinus of Valsalva with a course anterior to the pulmonary artery (prepulmonic) (arrowhead). b, c The three-dimensional volume-rendered images demonstrate the benign course anterior to the pulmonary artery (arrows) without acute angulation or a slit-like coronary ostium. This ACAOS is considered benign. LV left ventricle, RV right ventricle, Ao aorta, PA pulmonary artery
A 57-year-old male presented with atypical chest pain and subsequently underwent coronary CTA. The CT demonstrated an anomalous left main coronary artery originating from the right sinus of Valsalva with an intraseptal (subpulmonic) course. a The maximum intensity projection image demonstrates the anomalous left main coronary artery arising from the right sinus and coursing within the interventricular septum (arrow). b The oblique coronal image demonstrates the intraseptal course of the anomalous coronary artery (arrow) as it passes below the pulmonary artery. This ACAOS is considered benign. Ao aorta, LV left ventricle
A 35-year-old man was referred for coronary CTA after a non-gated chest CT suggested ACAOS. a The maximum intensity projection image demonstrates the left main coronary artery arising from the right sinus of Valsalva with a posterior (retroaortic) course (arrow). Calcified atherosclerotic plaques in the left main coronary artery are present. b The three-dimensional volume-rendered image demonstrates the relationship of the anomalous left main coronary artery (arrow) to the right coronary artery (chevron). This ACAOS is considered benign. Ao aorta, PA pulmonary artery
A 67-year-old male presented with chest pain and was found to have a pulmonary embolism. Incidental note was made of a coronary anomaly that was further evaluated with coronary CTA. a A maximum intensity projection image demonstrates the single coronary ostium from the right coronary cusp, branching into the right coronary artery (arrowhead), left circumflex (with a posterior course) (chevron), and left anterior descending artery (with an anterior course) (arrow). b A three-dimensional volume-rendered image demonstrates the normal RCA course (arrowhead) and the anomalous origin of the LAD from the RCA (arrow). c Another three-dimensional volume-rendered image demonstrates the single coronary ostium with all three branch arteries in view with an anterior course of the left anterior descending artery (arrow), a posterior course of the left circumflex (arrowhead), and a normal RCA course (chevron). Ao aorta
High-Risk Anatomic Features of ACAOS
ACAOS is a heterogeneous group of coronary anomalies with variable clinical expression. In fact, most ACAOS are not associated with a high risk of myocardial ischemia/SCD. The malignant variety is almost exclusively limited to ACAOS with an interarterial course (Figs. 6 and 11). High-risk anatomical features of ACAOS with an interarterial course associated with myocardial ischemia and SCD include acute angle of origin, a slit-like coronary ostium, and an intramural course. Anomalous left coronary arteries have a higher risk of SCD compared to anomalous right coronary arteries [6, 35, 36]. Not surprisingly when the anomalous coronary artery is dominant, higher rates of SCD have been observed [37]. Although anomalous right coronary arteries (Fig. 11) are associated with a lower rate of SCD, they may be more prone to ischemia as evidenced by a higher proportion of patients presenting with chest pain compared to anomalous left coronary arteries [23••].
A 71-year-old female presented with exertional chest pain and underwent coronary CTA which demonstrated ACAOS of the right coronary artery. a An oblique sagittal maximum intensity projection image demonstrates the acute angle of takeoff and a slit-like orifice of the anomalous right coronary artery (arrowhead) as it courses between the aorta and the pulmonary artery. b The oblique coronal multiplanar reformat demonstrates lateral luminal compression of the anomalous right coronary artery (arrow), suggestive of an intramural course. c The luminal shape and diameter are restored distally (arrow) as it exits the intramural portion. This ACAOS with an interarterial course is considered malignant and is associated with increased risk of sudden cardiac death. Ao aorta, PA pulmonary artery
Mechanism of Sudden Cardiac Death in ACAOS
The physiological underpinning(s) for myocardial ischemia/SCD in ACAOS has been a matter of debate. Table 3 lists a number of proposed mechanisms for reduced coronary flow in the setting of ACAOS [37, 38]. As previously mentioned, an interarterial coronary course is the subtype of ACAOS that is associated with the worst prognosis [12, 37, 39–41]. In particular, a left main coronary artery with an interarterial course is associated with the highest risk of sudden cardiac death. However, since the true prevalence is unknown, so is the actual risk of sudden death among affected individuals. The association between an interarterial course and SCD led many to hypothesize that the great arteries critically compress the anomalous coronary, leading to ischemia and fatal arrhythmia [42]. However, since coronary diastolic pressure is greater than pulmonary artery diastolic pressure (in the absence of pulmonary hypertension), mechanical compression of the coronary artery is unlikely. Using intravascular ultrasound (IVUS), Angelini et al. [43] demonstrated that an interarterial course is associated with a proximal segment of the coronary anomaly that runs within the aortic wall (intramural course). During pharmacologic stress, proximal intussusception of the anomalous artery at the aortic root wall occurs, leading to significant coronary stenosis. The degree of coronary hypoplasia and lateral compression of the coronary lumen, both found within the intramural segment, predicts ischemia as well. A large degree of interindividual variation exists with regard to the extent of coronary hypoplasia, lateral compression, and ultimately stenosis length. This variation likely, in large part, explains the heterogeneity in clinical presentation of ACAOS. Other investigators have investigated anomalous right coronary artery from the left cusp with fractional flow reserve (FFR) during dobutamine stress [44••]. Of 33 patients, 3 demonstrated an abnormal FFR (≤0.80) and all affected patients had an interarterial course and a slit-like coronary ostium. Their findings with FFR were corroborated by the degree of stenosis assessed by IVUS. Interestingly, 9 patients had a positive non-invasive stress test, but none of them had a significant stenosis by IVUS or FFR.
Anomalies of Intrinsic Coronary Artery Anatomy
Left Main Coronary Atresia
Left main coronary atresia is a rare condition associated with absence of a left coronary ostium/left main trunk (Fig. 12) [45]. The blood supply to the left anterior descending coronary artery and left circumflex originates through collaterals from the right coronary artery. Left main coronary atresia is almost universally symptomatic with only one patient reported in the literature that remained asymptomatic throughout life. Prognosis is poor without coronary artery bypass grafting [46].
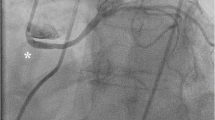
A 66-year-old male presented with new-onset exertional chest pain. His exercise stress test was positive for ischemia and he was referred for coronary CTA. a A three-dimensional volume-rendered image of the coronary tree demonstrates an atretic left main coronary artery. Collateral vessels arising from the right coronary artery supply the left coronary artery system. b A three-dimensional whole heart volume-rendered image demonstrates collateral vessels (arrows) from the conus branch supplying segments of the left anterior descending artery (arrows). Image reprinted with permission [45]. RCA right coronary artery, LCX left circumflex coronary artery, LAD left anterior descending artery. c The invasive coronary angiogram confirms the atretic left main coronary artery. A selective injection of the conus branch demonstrates collaterals to the mid- and distal LAD with retrograde filling of the proximal vessel and LCX
Myocardial Bridging
Myocardial bridges are coronary anatomic variants in which a segment of the epicardial coronary artery takes an intramyocardial course. Myocardial bridges most commonly occur in the mid-segment of the left anterior descending artery (Fig. 13) [47]. Most patients are asymptomatic; a small subgroup develops ischemia. The cause of ischemia is uncertain as the majority of coronary blood flow occurs during diastole and compression of the myocardial bridge occurs during systole. Interestingly, the tunneled segment of the coronary artery exhibits less atherosclerosis compared to anatomically normal coronary arteries [48]. However, the coronary segment proximal to the myocardial bridge demonstrates a higher rate of plaque development [49•], implicating sheer forces as the likely culprit. However, the mechanism for proximal atherosclerosis is still incompletely understood.
A 67-year-old female presented with atypical, non-exertional chest pain and underwent coronary CTA. a An oblique sagittal image demonstrates a left anterior descending artery bridge as it courses deeply into the myocardium (arrowhead). b A cross-sectional thin multiplanar reformat of the left anterior descending artery bridge demonstrates its depth (arrow) within the myocardium. LV left ventricle, RV right ventricle
The prevalence of myocardial bridges is difficult to define precisely for many of the same reasons alluded to earlier regarding selection bias. However, until recently, myocardial bridges were diagnosed by either autopsy or CCA. CCA demonstrates only modest sensitivity in diagnosing myocardial bridges as compared to autopsy series [50, 51]. Coronary CTA has produced similar prevalence estimates relative to autopsy series, ranging from approximately 14 to 30 % [52–55], secondary to its ability to visualize not only the coronary lumen but the overlying myocardium as well.
Coronary Aneurysms
Coronary aneurysms are defined as dilated coronary segments that are 1.5 times the diameter of the reference segment. The prevalence of coronary aneurysms was reported to be 1.4 % in a population referred for coronary angiography. This same cohort demonstrated a high prevalence (83 %) of obstructive coronary artery disease [56]. Indeed, atherosclerosis is the most common etiology for coronary aneurysms in the USA. Worldwide, Kawasaki disease remains the most common cause of coronary aneurysms. Approximately 25 % of patients with untreated acute Kawasaki disease develop coronary artery aneurysms (Fig. 14), with giant aneurysms at risk of developing mural thrombi and/or rupture [57]. Coronary CTA can be extremely useful at defining these aneurysms and associated complications. Other causes of coronary artery aneurysms include congenital, iatrogenic, traumatic, mycotic, embolic, and connective tissue diseases.
A 37-year-old male with Kawasaki disease underwent coronary CTA. a A maximum intensity projection image demonstrates multiple sequential aneurysms, most notably in the proximal right coronary artery without atherosclerosis (arrowhead). b A three-dimensional volume-rendered image demonstrates the proximal RCA aneurysms with discrete stenoses between aneurysmal segments (arrows). Ao aorta, LV left ventricle, RV right ventricle
Anomalies of Termination
Coronary Artery Fistulas
Coronary artery fistulas are abnormal communications between a coronary artery and the pulmonary artery (Fig. 15) or coronary sinus (coronary arteriovenous fistula) (Fig. 16), or between a coronary artery and any cardiac chamber (coronary cameral fistula). Similar to ALCAPA, coronary drainage into a lower-pressure structure can lead to a steal phenomenon and ischemia. Small- to moderate-sized fistulas are generally asymptomatic and associated with a good prognosis. About half of affected adults develop dyspnea (high-output heart failure) and/or chest pain. Children are rarely symptomatic. Treatment is reserved for fistulas that either cause symptoms or are associated with large aneurysms. Management strategies for hemodynamically significant coronary artery fistulas include transcatheter approaches, surgical ligation, and/or medical therapy [58].
A 65-year-old female presented with dyspnea with subsequent evaluation by coronary CTA. a An axial maximum intensity projection image demonstrates the left anterior descending artery (arrow) supplying feeder vessels (arrowheads) to the pulmonary artery. b A three-dimensional volume-rendered image illustrates the feeder vessels (arrowhead) to the pulmonary artery from the left anterior descending artery (arrow) and the right coronary artery (chevron). PA pulmonary artery, Ao aorta
A 68-year-old male presented with dyspnea and an abnormal transthoracic echocardiogram. He was subsequently referred for a coronary CTA. a An axial maximum intensity projection image at the level of the aortic root demonstrates a massively dilated proximal left circumflex (arrow). b A more caudal slice demonstrates an aneurysm secondary to a left circumflex to coronary sinus fistula. c, d Three-dimensional volume-rendered images demonstrate the dilated left circumflex (arrowhead) and fistulous connection (arrow) to the coronary sinus. CS coronary sinus, Ao aorta, LV left ventricle, RV right ventricle
Conclusion
Coronary anomalies are an important contributor to SCD, particularly in athletes and young adults, and thus represent an important clinical entity. While most coronary anomalies are benign, it is important to be aware of potentially malignant varieties, as identification is likely to inform patient management. ACAOS with an interarterial course is the most common of the malignant coronary anomalies. Historically, CCA has been considered the gold standard for evaluation of coronary anomalies. However, defining the origin and course of the anomalous coronary remains challenging with this technique. With refinements in technology, coronary CTA has emerged as an accurate and robust non-invasive method to define the full spectrum of coronary artery anomalies. Given the three-dimensional nature of this technique, the origin, course, and termination of anomalous coronary arteries are easily delineated relative to other important anatomic structures, such as the great vessels. Given its utility for the evaluation of patients with anomalous coronary arteries, recommendations for coronary CTA have been incorporated into appropriate use criteria and national guidelines.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Namgung J, Kim JA. The prevalence of coronary anomalies in a single center of Korea: origination, course, and termination anomalies of aberrant coronary arteries detected by ECG-gated cardiac MDCT. BMC Cardiovasc Disord. 2014;14:48. doi:10.1186/1471-2261-14-48. It describes a very large cohort of CCTA patients from a single institution, helping understand the prevalence of anomalous coronary arteries.
von Ziegler F, Pilla M, McMullan L, Panse P, Leber AW, Wilke N, et al. Visualization of anomalous origin and course of coronary arteries in 748 consecutive symptomatic patients by 64-slice computed tomography angiography. BMC Cardiovasc Disord. 2009;9:54. doi:10.1186/1471-2261-9-54.
Opolski MP, Pregowski J, Kruk M, Witkowski A, Kwiecinska S, Lubienska E, et al. Prevalence and characteristics of coronary anomalies originating from the opposite sinus of Valsalva in 8,522 patients referred for coronary computed tomography angiography. Am J Cardiol. 2013;111(9):1361–7. doi:10.1016/j.amjcard.2013.01.280. It also describes a very large cohort of CCTA patients from a single institution, helping understand the prevalence of anomalous coronary arteries.
Yamanaka O, Hobbs RE. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Catheter Cardiovasc Diagn. 1990;21(1):28–40.
Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980–2006. Circulation. 2009;119(8):1085–92. doi:10.1161/CIRCULATIONAHA.108.804617.
Eckart RE, Scoville SL, Campbell CL, Shry EA, Stajduhar KC, Potter RN, et al. Sudden death in young adults: a 25-year review of autopsies in military recruits. Ann Intern Med. 2004;141(11):829–34.
Shi H, Aschoff AJ, Brambs HJ, Hoffmann MH. Multislice CT imaging of anomalous coronary arteries. Eur Radiol. 2004;14(12):2172–81. doi:10.1007/s00330-004-2490-2.
Schmitt R, Froehner S, Brunn J, Wagner M, Brunner H, Cherevatyy O, et al. Congenital anomalies of the coronary arteries: imaging with contrast-enhanced, multidetector computed tomography. Eur Radiol. 2005;15(6):1110–21. doi:10.1007/s00330-005-2707-z.
Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, et al. ACC/AHA 2008 Guidelines for the Management of Adults with Congenital Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines on the management of adults with congenital heart disease). Circulation. 2008;118(23):e714–833. doi:10.1161/CIRCULATIONAHA.108.190690.
Taylor AJ, Cerqueira M, Hodgson JM, Mark D, Min J, O’Gara P, et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Cardiovasc Comput Tomogr. 2010;4(6):407 e1–33. doi:10.1016/j.jcct.2010.11.001.
Angelini P. Normal and anomalous coronary arteries: definitions and classification. Am Heart J. 1989;117(2):418–34.
Angelini P, Velasco JA, Flamm S. Coronary anomalies: incidence, pathophysiology, and clinical relevance. Circulation. 2002;105(20):2449–54.
Nasis A, Machado C, Cameron JD, Troupis JM, Meredith IT, Seneviratne SK. Anatomic characteristics and outcome of adults with coronary arteries arising from an anomalous location detected with coronary computed tomography angiography. Int J Cardiovasc Imaging. 2015;31(1):181–91. doi:10.1007/s10554-014-0535-4.
Yu FF, Lu B, Gao Y, Hou ZH, Schoepf UJ, Spearman JV, et al. Congenital anomalies of coronary arteries in complex congenital heart disease: diagnosis and analysis with dual-source CT. J Cardiovasc Comput Tomogr. 2013;7(6):383–90. doi:10.1016/j.jcct.2013.11.004.
Topaz O, DiSciascio G, Cowley MJ, Soffer A, Lanter P, Goudreau E, et al. Absent left main coronary artery: angiographic findings in 83 patients with separate ostia of the left anterior descending and circumflex arteries at the left aortic sinus. Am Heart J. 1991;122(2):447–52.
Wesselhoeft H, Fawcett JS, Johnson AL. Anomalous origin of the left coronary artery from the pulmonary trunk. Its clinical spectrum, pathology, and pathophysiology, based on a review of 140 cases with seven further cases. Circulation. 1968;38(2):403–25.
Dodge-Khatami A, Mavroudis C, Backer CL. Anomalous origin of the left coronary artery from the pulmonary artery: collective review of surgical therapy. Ann Thorac Surg. 2002;74(3):946–55.
Donataccio MP, Li W, Ramasamy M, Senior R. Anomalous origin of left coronary artery from the pulmonary artery (ALCAPA): a rare presentation in late adulthood. Int J Cardiol. 2014;182C:179–80. doi:10.1016/j.ijcard.2014.12.127.
Schwartz ML, Jonas RA, Colan SD. Anomalous origin of left coronary artery from pulmonary artery: recovery of left ventricular function after dual coronary repair. J Am Coll Cardiol. 1997;30(2):547–53.
Williams IA, Gersony WM, Hellenbrand WE. Anomalous right coronary artery arising from the pulmonary artery: a report of 7 cases and a review of the literature. Am Heart J. 2006;152(5):1004 e9–17. doi:10.1016/j.ahj.2006.07.023.
Correia E, Ferreira P, Rodrigues B, Santos L, Faria R, Nunes L, et al. Prevalence of anomalous origin of coronary arteries: a retrospective study in a Portuguese population. Rev Port Cardiol. 2010;29(2):221–9.
Villines TC, Devine PJ, Cheezum MK, Gibbs B, Feuerstein IM, Welch TS. Incidence of anomalous coronary artery origins in 577 consecutive adults undergoing cardiac CT angiography. Int J Cardiol. 2010;145(3):525–6. doi:10.1016/j.ijcard.2010.04.059.
Krupinski M, Urbanczyk-Zawadzka M, Laskowicz B, Irzyk M, Banys R, Klimeczek P, et al. Anomalous origin of the coronary artery from the wrong coronary sinus evaluated with computed tomography: “high-risk” anatomy and its clinical relevance. Eur Radiol. 2014;24(10):2353–9. doi:10.1007/s00330-014-3238-2. It evaluates a large cohort of 7,115 CCTA patients and found that the highest rates of chest pain and cardiac events occurred in anomalous right coronary arteries, not left. They also noted that anomalous right coronaries were more likely to have an interarterial course in this cohort which are unique findings.
Szymczyk K, Polguj M, Szymczyk E, Majos A, Grzelak P, Stefanczyk L. Prevalence of congenital coronary artery anomalies and variants in 726 consecutive patients based on 64-slice coronary computed tomography angiography. Folia Morphol (Warsz). 2014;73(1):51–7. doi:10.5603/FM.2014.0007.
Park JH, Kwon NH, Kim JH, Ko YJ, Ryu SH, Ahn SJ, et al. Prevalence of congenital coronary artery anomalies of Korean men detected by coronary computed tomography. Korean Circ J. 2013;43(1):7–12. doi:10.4070/kcj.2013.43.1.7.
Zhang LJ, Yang GF, Huang W, Zhou CS, Chen P, Lu GM. Incidence of anomalous origin of coronary artery in 1879 Chinese adults on dual-source CT angiography. Neth Heart J Mon J Neth Soc Cardiol Neth Heart Found. 2010;18(10):466–70.
Cheng Z, Wang X, Duan Y, Wu L, Wu D, Liang C, et al. Detection of coronary artery anomalies by dual-source CT coronary angiography. Clin Radiol. 2010;65(10):815–22. doi:10.1016/j.crad.2010.06.003.
Kosar P, Ergun E, Ozturk C, Kosar U. Anatomic variations and anomalies of the coronary arteries: 64-slice CT angiographic appearance. Diagn Interv Radiol. 2009;15(4):275–83. doi:10.4261/1305-3825.DIR.2550-09.1.
Duran C, Kantarci M, Durur Subasi I, Gulbaran M, Sevimli S, Bayram E, et al. Remarkable anatomic anomalies of coronary arteries and their clinical importance: a multidetector computed tomography angiographic study. J Comput Assist Tomogr. 2006;30(6):939–48. doi:10.1097/01.rct.0000230004.38521.8e.
Sato Y, Inoue F, Matsumoto N, Tani S, Takayama T, Yoda S, et al. Detection of anomalous origins of the coronary artery by means of multislice computed tomography. Circ J Off J Jpn Circ Soc. 2005;69(3):320–4.
Davis JA, Cecchin F, Jones TK, Portman MA. Major coronary artery anomalies in a pediatric population: incidence and clinical importance. J Am Coll Cardiol. 2001;37(2):593–7.
Pelliccia A, Spataro A, Maron BJ. Prospective echocardiographic screening for coronary artery anomalies in 1,360 elite competitive athletes. Am J Cardiol. 1993;72(12):978–9.
Zeppilli P, dello Russo A, Santini C, Palmieri V, Natale L, Giordano A, et al. In vivo detection of coronary artery anomalies in asymptomatic athletes by echocardiographic screening. Chest. 1998;114(1):89–93.
Mohsen GA, Mohsin KG, Forsberg M, Miller E, Taniuchi M, Klein AJ. Anomalous left circumflex artery from the right coronary cusp: a benign variant? J Invasive Cardiol. 2013;25(6):284–7. In a small cohort of anomalous left circumflex artery patients, they demonstrate a very high rate of atherosclerosis in anomalous LCx.
Basso C, Maron BJ, Corrado D, Thiene G. Clinical profile of congenital coronary artery anomalies with origin from the wrong aortic sinus leading to sudden death in young competitive athletes. J Am Coll Cardiol. 2000;35(6):1493–501.
Taylor AJ, Rogan KM, Virmani R. Sudden cardiac death associated with isolated congenital coronary artery anomalies. J Am Coll Cardiol. 1992;20(3):640–7.
Kragel AH, Roberts WC. Anomalous origin of either the right or left main coronary artery from the aorta with subsequent coursing between aorta and pulmonary trunk: analysis of 32 necropsy cases. Am J Cardiol. 1988;62(10 Pt 1):771–7.
Virmani R, Chun PK, Rogan K, Riddick L. Anomalous origin of four coronary ostia from the right sinus of Valsalva. Am J Cardiol. 1989;63(11):760–1.
Roberts WC, Kragel AH. Anomalous origin of either the right or left main coronary artery from the aorta without coursing of the anomalistically arising artery between aorta and pulmonary trunk. Am J Cardiol. 1988;62(17):1263–7.
Frescura C, Basso C, Thiene G, Corrado D, Pennelli T, Angelini A, et al. Anomalous origin of coronary arteries and risk of sudden death: a study based on an autopsy population of congenital heart disease. Hum Pathol. 1998;29(7):689–95.
Cheitlin MD, De Castro CM, McAllister HA. Sudden death as a complication of anomalous left coronary origin from the anterior sinus of Valsalva, a not-so-minor congenital anomaly. Circulation. 1974;50(4):780–7.
Grollman Jr JH, Mao SS, Weinstein SR. Arteriographic demonstration of both kinking at the origin and compression between the great vessels of an anomalous right coronary artery arising in common with a left coronary artery from above the left sinus of Valsalva. Catheter Cardiovasc Diagn. 1992;25(1):46–51.
Angelini P, Velasco JA, Ott D, Khoshnevis GR. Anomalous coronary artery arising from the opposite sinus: descriptive features and pathophysiologic mechanisms, as documented by intravascular ultrasonography. J Invasive Cardiol. 2003;15(9):507–14.
Lee SH, Koo BK, Yu CH, Kim JH, Park KW, Kang HJ, et al. Physiologic assessment of anomalous origin of right coronary artery from left coronary cusp using dobutamine stress fractional flow reserver. J Am Coll Cardiol. 2012;59(13s1):E832-E. In a superb investigation, the authors demonstrate, through the tools of FFR and IVUS, that anomalous right coronary arteries with an interarterial course and slit like ostia demonstrate ischemia (FFR <0.80) and have significant stenosis on IVUS. They also reinforce that stress testing is unreliable to predict ischemia in ACAOS.
Pursnani A, Jacobs JE, Saremi F, Levisman J, Makaryus AN, Capunay C, et al. Coronary CTA assessment of coronary anomalies. J Cardiovasc Comput Tomogr. 2012;6(1):48–59. doi:10.1016/j.jcct.2011.06.009.
Musiani A, Cernigliaro C, Sansa M, Maselli D, De Gasperis C. Left main coronary artery atresia: literature review and therapeutical considerations. Eur J Cardiothorac Surg Off J Eur Assoc Cardiothorac Surg. 1997;11(3):505–14.
Reyman H. Disertatio de vasis cordis propriis. Med Diss Univ Göttingen. 1737;7th Sept:1–32.
Verhagen SN, Rutten A, Meijs MF, Isgum I, Cramer MJ, van der Graaf Y, et al. Relationship between myocardial bridges and reduced coronary atherosclerosis in patients with angina pectoris. Int J Cardiol. 2013;167(3):883–8. doi:10.1016/j.ijcard.2012.01.091.
Nakaura T, Nagayoshi Y, Awai K, Utsunomiya D, Kawano H, Ogawa H, et al. Myocardial bridging is associated with coronary atherosclerosis in the segment proximal to the site of bridging. J Cardiol. 2014;63(2):134–9. doi:10.1016/j.jjcc.2013.07.005. Atherosclerosis is more likely to occur in the coronary artery segment prior to a myocardial bridge.
Mohlenkamp S, Hort W, Ge J, Erbel R. Update on myocardial bridging. Circulation. 2002;106(20):2616–22.
Tovar EA, Borsari A, Landa DW, Weinstein PB, Gazzaniga AB. Ventriculotomy repair during revascularization of intracavitary anterior descending coronary arteries. Ann Thorac Surg. 1997;64(4):1194–6.
Ma ES, Ma GL, Yu HW, Wu W, Li K. Assessment of myocardial bridge and mural coronary artery using ECG-gated 256-slice CT angiography: a retrospective study. Sci World J. 2013;2013:947876. doi:10.1155/2013/947876.
Konen E, Goitein O, Sternik L, Eshet Y, Shemesh J, Di Segni E. The prevalence and anatomical patterns of intramuscular coronary arteries: a coronary computed tomography angiographic study. J Am Coll Cardiol. 2007;49(5):587–93. doi:10.1016/j.jacc.2006.09.039.
Vanker EA, Ajayi NO, Lazarus L, Satyapal KS. The intramyocardial left anterior descending artery: prevalence and surgical considerations in coronary artery bypass grafting. S Afr J Surg. 2014;52(1):18–21.
Sahni D, Jit I. Incidence of myocardial bridges in northwest Indians. Indian Heart J. 1991;43(6):431–6.
Hartnell GG, Parnell BM, Pridie RB. Coronary artery ectasia. Its prevalence and clinical significance in 4993 patients. Br Heart J. 1985;54(4):392–5.
Kato H, Sugimura T, Akagi T, Sato N, Hashino K, Maeno Y, et al. Long-term consequences of Kawasaki disease. A 10- to 21-year follow-up study of 594 patients. Circulation. 1996;94(6):1379–85.
Said SA, Lam J, van der Werf T. Solitary coronary artery fistulas: a congenital anomaly in children and adults. A contemporary review. Congenit Heart Dis. 2006;1(3):63–76. doi:10.1111/j.1747-0803.2006.00012.x.
Compliance with Ethics Guidelines
Conflict of Interest
J McLarry declares no conflicts of interest.
M Ferencik has received research grants from the American Heart Association (13FTF16450001).
MD Shapiro declares no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Cardiac Computed Tomography
Rights and permissions
About this article
Cite this article
McLarry, J., Ferencik, M. & Shapiro, M.D. Coronary Artery Anomalies: a Pictorial Review. Curr Cardiovasc Imaging Rep 8, 23 (2015). https://doi.org/10.1007/s12410-015-9339-8
Published:
DOI: https://doi.org/10.1007/s12410-015-9339-8