Abstract
Purpose of Review
Comprehensive discussion of alternative techniques in imaging coronary artery anomalies (CAAs) in different diagnostic scenarios.
Recent Findings
At primary screening, intramural course essentially correlates with stenosis and clinical repercussion in some types of CAAs. Potential clinical aims in imaging patients with CAAs may be primary screening, severity evaluation, preoperative planning, and postoperative follow-up. Appropriate techniques are echocardiography, magnetic resonance imaging, computed tomography angiography, and intravascular ultrasound (IVUS). Rarely, IVUS may be needed in patients with potentially serious CAAs and has unique advantages and limitations. IVUS data are essential for in-depth knowledge of mechanisms of coronary dysfunction (exercise-related dynamic stenosis of variable severity) and for indicating interventional treatment.
Summary
In adolescents or adults, intramural course of an anomalous coronary artery is the only important feature accompanied by stenosis of potential severity and is especially relevant in patients with a high-risk status (elite sport athletes, military recruits).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary artery anomalies (CAAs) are the focus of a subspecialty in modern cardiology that has rapidly evolved over the last 25 years [1, 2]. Several aspects of the clinical relevance and technical progress in the field of CAAs require an update in order to (1) discuss the ideal approach for screening and evaluating individual patients, (2) understand the general mechanisms of dysfunction, and (3) establish interventional recommendations. The nature and prognosis of CAAs varies substantially among the many types currently recognized. It is fundamentally important to clarify initially the defining features, the terminology, and the clinical indications to study the anomalies in detail and yield useful information for clinical purposes. For many years, CAAs have been identified generically (as a group labeled with a single name such as “AAOCA”(anomalous aortic origin of a coronary artery [3]), “ACAOS” (anomalous origin of a coronary artery from “opposite” sinus of Valsalva [2, 4]), or “ACA”(anomalous coronary artery [5])) as the cause of sudden cardiac death in the young; however, recently, we have come to recognize that only a few CAAs have intrinsic mechanisms of dysfunction (stenosis) and clinical or prognostic relevance. Figure 1 shows the most important types of anomalies that can cause coronary insufficiency (i.e., myocardial ischemia) in young adults involved in strenuous exertion [6]. They can affect the right or the left coronary (and, on the left side, the left anterior descending or the circumflex artery, separately), when they have an intramural course with dynamic luminal stenosis. Anomalies of the coronary arteries should be recognized by the anatomic and functional features that differentiate them from normal anatomy. Anatomically, CCAs can feature an abnormal (1) coronary ostial location/orientation with respect to the aortic wall, (2) course of the proximal or intermediate coronary segments, or (3) termination. The main cause of ischemia in patients with CAAs is generally the narrowing of the initial segment of the coronary artery as it enters or exits the aortic wall, at an intramural course by compression in between the inner and outer layers of the aortic tunica media [7••, 8•]. ACAOS can affect the right or left coronary artery (called R-ACAOS and L-ACAOS, respectively); markers of stenosis are not present in any others (intraseptal or infundibular, retroaortic, wrap-around the apex, or retrocardiac). The dynamic regimen of the compressive forces leads to variations in luminal geometry from the time of diastole (lowest degree of compression, larger cross-sectional area [CSA]) to systole (highest degree of compression, smaller CSA).
Diagram of the base of the heart shows the possible ectopic origins of the left coronary artery (or separately of the circumflex [Cx] and left anterior descending [LAD] arteries) and the right coronary artery (RCA). The connections are indicated by color lines: blue is for benign, red is for high-risk, green is for intramyocardial (infundibular). The four cardiac valve locations are indicated (M, mitral; T, tricuspid; pulmonary is anterior and aortic is posterior at the outflows) (modified with permission from Wolters Kluwer from: Angelini P, Fairchild V, eds. Coronary Artery Anomalies: A Comprehensive Approach. Baltimore, MD: Lippincott, Williams & Wilkins, 1999:27–150) [6]
The reasons for indicating any type of coronary imaging test are (1) to establish the type of CAA (to recognize specifically high-risk CAAs) and (2) to indicate, plan, conduct, or follow up on interventional corrective procedures. The intrinsic risk implicit in a given CAA type is best indicated initially by the prevalence and mortality rate of a specific type of CCA in athletes versus a control sedentary population with the same defect or with normal coronary anatomy (“relative risk”) [4, 9••]. Recently, our group published the results of the Screen to Prevent (S2P) study [4, 9••] in participants of sport exercises in an unselected population of 5,169 school students (Table 1) [9••]. In this regard, a breakthrough study was offered by the US military physicians that indicated that the highest risk of sudden cardiac death (SCD) in CCAs occurs only in carriers of L-ACAOS-IM (IM, intramural course); these findings are consistent with those from smaller clinical series from dedicated centers of coronary anomalies [7••, 8•]. The recruits’ experience showed that L-ACAOS-IM has a mortality rate about 430 times higher than that in the control population [8•, 9••]. In contrast, the risk of SCD is much lower in those with R-ACAOS-IM (not a single case in the recruits, but 14% in high-school athletes [10]). In an older population (> 35 years) with CAA, SCD related to strenuous exertion is extremely rare, whereas symptoms of chest pain or dyspnea or syncope are more prevalent [11]. This review discusses specifically the indications, limitations, and results of imaging studies performed by different techniques as used for primary screening for diagnosis of CAA type or for assessing the severity of stenosis and the indication of intervention.
Reasons for Imaging
-
1.
Primary screening of a young population of candidates for sports participation. In light of the increased risk of SCD due to exposure to strenuous exercise, screening is well established as based on the prevalence and mortality data related to CAA [4, 8•, 10,11,12,13,14]. CAAs are congenital, and their anatomy should be stable for many years; therefore, the results of a single accurate imaging study should be adequate over a participant’s lifetime.
-
2.
Evaluation of patients known or presumed to have CAAs, based on initial testing (frequently by echocardiography or stress testing) or suggestive symptoms (chest pain, dyspnea, syncope, or aborted cardiac arrest). The typical escalation of clinical imaging (if the initial result is inconclusive) is (a) echocardiogram in the young; (b) selective coronary artery angiography, magnetic resonance imaging (MRI), or coronary computed tomography angiography (CCTA; Fig. 2) for screening adolescents or adults; and (c) intravascular ultrasound imaging (IVUS) when an operation is being discussed (Figs. 3 and 4).
-
3.
Postoperative evaluation of the results of CAA interventions. This type of evaluation enables re-qualification of athletes and is generally done by exercise nuclear stress testing and occasionally by IVUS imaging.
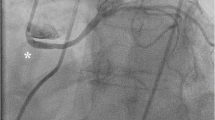
The Angelini/Cheong sign. In a right anterior oblique projection, the plane crosses the aortic root and pulmonary valves, at the level of maximal obstruction by compression of the intramural right coronary artery (in this case, the ratio of the longitudinal versus transverse diameters is about 3:1, indicating stenosis, probably severe in nature). AV, aortic valve; PV, pulmonary valve. Black arrow = compressed intramural right coronary artery
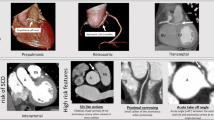
R-ACAOS-IM as seen by catheter angiography (above) and by IVUS (below). Top row: The 3 angiographic frames illustrate that the ostium appears to be enlarged in the left anterior oblique (left side, arrowhead) but severely stenotic in the right anterior oblique projection (center: arrows = proximal stenosis, asterisk = ostium); after ostial stent deployment, the ostium appears to have gained a normal size (right). Bottom row: In diastole (left panel), in systole (center panel), and at a distal reference (right panel). The stenosis was calculated as 79% in systole and 50% in diastole. The short diameter was 0.9 mm in systole and 1.9 mm in diastole, signs of severe stenosis. The outline of the cross-sectional media layer areas is shown as having a mean diameter of 4.0 mm. Dotted line = internal elastic media layer
Left panel: Histologic section of L-ACAOS-IM (section of the aortic wall and LCA origin) in a 14-year-old girl who died of SCD during moderate jogging (stain: elastica-Masson staining). At the exit from the intramural course, critical narrowing of the left main trunk is shown. The minimal luminal diameter was about 1.8 mm (critical stenosis). EPI, epicardial side; ENDO, endoluminal side of the aortic wall. Right panel: In a similar case (a 24-year-old man with acute myocardial infarction at rest), the left side shows a coronary angiographic frame, with adjoining coronary ostia from the left sinus, without evidence of stenosis, in the left anterior oblique projection. The right side shows intravascular ultrasound frames indicating the following: (A) left main trunk with proximal, mild hypoplasia; (B1) diastolic and (B2) systolic frames exiting the intramural segment of the left main trunk (the worse level of stenosis, illustrated in (B), corresponding to the left panel histology image); minimal cross diameter is 1.17 mm (B1) versus 0.83 mm (B2); and (C) distal left main trunk, showing the reference CSA (maximal systolic stenosis = 80%). LAD, left anterior descending; RCA, right coronary artery
General Acknowledgment
Most standard coronary imaging techniques are planar and tomographic, but in coronary use, they must refer to the tortuous, off-plane anatomy located over the beating heart and subjected to pulsatile hemodynamic influences. Coronary dysfunction must be evaluated as a cause of ischemia, which ultimately must be related to the severity of stenosis. A three-dimensional volume rendering of the anatomy can be reconstructed by using different postacquisition techniques (typically for CCTA), but the fine quantification of luminal stenosis can be critically affected by such techniques (typically obtained only at end-diastole). Only cross-sectional imaging perpendicular to the vessel’s direction obtained during both cardiac phases can potentially help measure the area of stenosis. In particular, the thickness of the split aortic wall at the intramural segment (in the range of 1–2 mm) is not recognized by the intrinsic spatial limitations of echocardiography, CCTA, or MRI (usually reported only in end-diastolic time); it can be imaged only by IVUS, which has about 10 times more spatial and temporal precision than other imaging techniques [7••, 8•, 15, 16].
Primary Screening in Potentially High-Risk Population
An accurate initial assessment of CAAs in sports participants is of interest to individual/families, the school system, the state government, the insurance companies, and the public health system, specifically for those candidates who participate in strenuous exercise (sports, military personnel, professional athletes) or who have suspicious symptoms or abnormal stress testing. In large populations and in those with a low pretest likelihood of disease, the ideal imaging technique should be precise, simple, economical, and non-invasive for the primary aim of establishing the diagnosis of CAA type.
In children, the choice is usually echocardiography, which may not be adequate in those with larger bodies (> 40 kg) and when performed in less expert environments (on-the-field screening acquired by technicians). In smaller children, sedation or even general anesthesia may be necessary to secure an accurate diagnosis. The use of Doppler interrogation improves the precision of echocardiographic diagnosis (high velocity is the probable marker of stenosis). Specifically, diastolic flow velocity is higher than in systole, whereas systolic compression is more severe in systole. The few, large-scale screening echocardiographic studies in adolescents indicate a much lower prevalence of CAAs (close to 0–4% of the expected) than that obtained with screening MRI (s-MRI) (about 0.45%, absolute prevalence) [4, 9••, 17, 18•].
In adolescents or adults, s-MRI is the ideal testing tool. This test can yield a consistently specific diagnosis of high-risk CAA type, and it can be performed quickly and reliably without side effects or discomfort [9••]. Moreover, the test does not require potentially dangerous radiation (ionizing) or the administration of intravenous medicines and contrast, and the data can be acquired in 10–15 min [9••]. Specialized reading of the data can be obtained easily, possibly even by remote analysis at specialized centers. The basic interpretation technique for CAAs involves clarifying the location of the aortic valve commissures (and sinuses), the coronary ostia, and the proximal course of the ectopic coronary artery. Only the intramural aortic course is associated with some degree of stenosis, but the exact quantification of stenosis cannot be achieved by s-MRI (and by CCTA). In a screening context, CCTA imaging requires intravenous access and the use of ionizing radiation, contrast medium, beta-blockers, and occasional sedation. CCTA is more precise than s-MRI in confirming the anomalous origin, the proximal course, and the approximate severity of stenosis by using a cross-sectional image at the level of the aorto/pulmonary septum (anterior commissure of the aortic valve) that consists of the Angelini/Cheong sign (Fig. 2), which comprises the cross-sectional ratio between the long and short axes of the anomalous intramural artery; a ratio greater than 2:1 suggests significance [16].
Follow-up IVUS may be needed when high-risk factors are present (as in elite athlete certification, in the presence of symptoms or positive stress test). Based on the S2P study, none of the potentially high-risk CAAs (ACAOS-IM by s-MRI) was identified on the basis of symptoms or EKG findings.
Selective catheter angiography can be technically laborious and difficult in the presence of tangential and ectopic coronary origin. Special catheters have been recently developed that make the cannulation and backup support easier (for IVUS catheterization, stent PCI, besides angiography) [2]. In ACAOS, catheter angiography is primarily used for definitive imaging of the distal vessel (dominance coronary tree pattern and atherosclerotic burden). Ostial stenosis is generally poorly evaluated by catheter angiography [7••, 8•].
Secondary Evaluation of CAAs
Our group and others involved in this subspecialty believe that secondary evaluation of the severity of stenosis in some (but only a few) coronary anomalies should be conducted (generally by IVUS, at specialized centers), if echocardiography, MRI or CCTA, or stress testing results suggest an intramural diagnosis and hemodynamic significance. Functional studies, including nuclear stress testing of fractional flow reserve, do not contribute to a definitive severity characterization in ACAOS [5, 19].
IVUS is a catheter-based procedure (Figs. 3 and 4) in which high-precision cross-sectional imaging of the coronary lumen is obtained by passing an ultrasound probe over a coronary catheter guidewire in a patient who has been transiently anticoagulated (typically with heparin). Obtaining this in vivo highly precise imaging is important because coronary stenosis in ACAOS-IM occurs in phasic fashion (present at baseline, with systolic worsening). In athletes, the concern is focused paradoxically on highly trained individuals (able to compete at very high heart rates and cardiac outputs) who participate in strenuous exercise and who are usually asymptomatic (by self-bias selection, in light of the fact that only asymptomatic athletes do sports). In cases with borderline severity, measuring the severity of coronary narrowing during simulated exertion may be useful. Currently, this study is indicated when the baseline resting stenosis is mild (< 50% in L-ACAOS-IM and < 55% in R-ACAOS-IM) and the clinical need to assess stenosis is important (the need to establish an indication for intervention or disqualification from competitive sports) [7••, 8•]. The severity of intramural CSA stenosis is calculated in reference to the distal extramural reference vessel (Figs. 3 and 4). IVUS can also confirm with certainty that the stenosis in R- or L-ACAOS-IM is always “intramurally, inside the aortic tunica media”; the frequently purported mechanism of stenosis by inter-arterial coronary compression between aorta and pulmonary artery is never seen. Much of the discussion about inter-arterial course nomenclature has marred this field in cardiology and should be abandoned, based on the overwhelming evidence offered by IVUS. The only case of CAAs with an initially inter-arterial course, but without an intramural course, has an intraseptal (or infundibular) course, and it should not be considered inter-arterial (generally a benign variant) [7••].
In R-ACAOS-IM, the stenosis is always ostial, whereas in L-ACAOS-IM, the site of maximal narrowing can vary and can be seen at the ostium or at the mid-section or distal to the intramural section (Fig. 4). IVUS can establish the length of the intramural segment and the level of the intramural course with respect to the upper edge of the anterior commissure (important for surgical considerations).
Conclusions
The Texas Heart Institute’s Center for Coronary Artery Anomalies has recently recommended creating specialized Centers of Excellence in this new field of cardiology. Such centers should be focused on increasing the knowledge base required to better understand coronary anatomy and physiology in CAAs and to enable improvements and validation of treatment guidelines for this rare and diverse pathology. The introduction of IVUS (and occasionally optical coherence tomography) has been fundamental in acquiring initial experience of critical value. Stent angioplasty in adults with ACAOS-IM has been safely developed on the basis of IVUS data and is currently a promising therapeutic option, especially for patients with R-ACAOS-IM [4].
Summarizing the full range of diagnostic imaging in ACAOS, we make the following recommendations (which still require statistical validation in prospective multicenter studies for their preventive effects especially relating to the incidence of SCD during exertion). First, high-risk candidates (elite athletes and military recruits) should undergo screening imaging. s-MRI is the most useful because it is simple, can be quickly performed, and provides definitive value in establishing the primary diagnosis of potentially high-risk ACAOS-IM, which is the most serious type of CAA. Additionally, s-MRI enables the recognition of low-risk CAAs (which do not usually require further testing) with an unmatched low rate of false-positive and false-negative results [9••]. Echocardiography may be a feasible but not required technique in children because there is no strong evidence of a clinical need for screening preadolescent children. Second, CTA with intravenous contrast may occasionally be useful for patients that are claustrophobic, if the MRI images are not diagnostic, or as a secondary confirmation of the same diagnoses that can be established with MRI that does not use ionizing radiation and contrast agents. Third, in cases of ACAOS-IM in which a definitive evaluation of the severity of stenosis is clinically indicated, IVUS (performed at expert centers) can yield a precise quantification. Finally, IVUS data are particularly valuable in establishing indications for intervention and execution of stent angioplasty.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Angelini P. Normal and anomalous coronary arteries: definitions and classification. Am Heart J. 1989;117:418–34.
Angelini P. Novel imaging of coronary artery anomalies to assess their prevalence, the causes of clinical symptoms, and the risk of sudden cardiac death. Circ Cardiovasc Imaging. 2014;7:747–54.
Poynter JA, Williams WG, McIntyre S, Brothers JA, Jacobs ML, the Congenital Heart Surgeons Society AAOCA Working Group, et al. Anomalous aortic origin of a coronary artery: a report from the Congenital Heart Surgeons Society Registry. World J Pediatr Congenit Heart Surg. 2014;5:22–30.
Angelini P, Cheong BY, Lenge De Rosen VV, et al. Magnetic resonance imaging-based screening study in a general population of adolescents. J Am Coll Cardiol. 2018;71:579–80.
Grani C, Benz DC, Schmied C, et al. Hybrid CCTA/SPECT myocardial perfusion imaging findings in patients with anomalous origin of coronary arteries from the opposite sinus and suspected concomitant coronary artery disease. J Nucl Cardiol. 2017;24:226–34.
Angelini P, Villanson S, Chan AVJ, et al. Normal and anomalous coronary artery in humans. In: Angelini P, Fairchild V, editors. Coronary artery anomalies: a comprehensive approach. Baltimore: Lippincott, Williams & Wilkins; 1999. p. 27–150.
•• Angelini P, Uribe C. Anatomic spectrum of left coronary artery anomalies and associated mechanisms of coronary insufficiency. Catheter Cardiovasc Interv. 2018;92:313–21 Findings from this report explain the wide spectrum of presentation of high-risk cases of left coronary anomalies, based on intravascular ultrasound imaging.
• Angelini P, Uribe C, Monge J, et al. Origin of the right coronary artery from the opposite sinus of Valsalva in adults: characterization by intravascular ultrasonography at baseline and after stent angioplasty. Catheter Cardiovasc Interv. 2015;86:199–208 This report explains the fundamental mechanism of ischemia in any coronary anomaly with an intramural course, as shown by intravascular ultrasound.
•• Angelini P, Cheong BY, Lenge De Rosen VV, et al. High-risk cardiovascular conditions in sports-related sudden death: prevalence in 5,169 schoolchildren screened via cardiac magnetic resonance. Tex Heart Inst J. 2018;45:205–13 This report describes the unprecedented findings of a large general population screening study, based on an accurate imaging technique (screening MRI).
Eckart RE, Scoville SL, Campbell CL, Shry EA, Stajduhar KC, Potter RN, et al. Sudden death in young adults: a 25-year review of autopsies in military recruits. Ann Intern Med. 2004;141:829–34.
Smallman DP, Webber BJ, Mazuchowski EL, Scher AI, Jones SO, Cantrell JA. Sudden cardiac death associated with physical exertion in the US military, 2005-2010. Br J Sports Med. 2016;50:118–23.
Harmon KG, Asif IM, Klossner D, Drezner JA. Incidence of sudden cardiac death in National Collegiate Athletic Association athletes. Circulation. 2011;123:1594–600.
Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006. Circulation. 2009;119:1085–92.
Toresdahl BG, Rao AL, Harmon KG, Drezner JA. Incidence of sudden cardiac arrest in high school student athletes on school campus. Heart Rhythm. 2014;11:1190–4.
Angelini P, Flamm SD. Newer concepts for imaging anomalous aortic origin of the coronary arteries in adults. Catheter Cardiovasc Interv. 2007;69:942–54.
Cheong BY, Angelini P. Magnetic resonance imaging of the coronary arteries. In: Willerson JT, Holmes DR, editors. Coron Artery Dis. London: Springer-Verlag; 2007. p. 283–338.
Angelini P. Is echocardiography adequate to identify the severity of anomalous coronary arteries? JACC Cardiovasc Imaging. 2016;9:898–9.
• Malhotra A, Dhutia H, Finocchiaro G, Gati S, Beasley I, Clift P, et al. Outcomes of cardiac screening in adolescent soccer players. N Engl J Med. 2018;379:524–34 This large echocardiography screening study follows a large group of soccer players for a significant period of time and documents the limitations of such a screening program.
Lee SE, Yu CW, Park K, Park KW, Suh JW, Cho YS, et al. Physiological and clinical relevance of anomalous right coronary artery originating from left sinus of Valsalva in adults. Heart. 2016;102:114–9.
Acknowledgments
Dr. Carlo Uribe has provided expert assistance with the imaging used in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Paolo Angelini declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Echocardiography
Rights and permissions
About this article
Cite this article
Angelini, P. Imaging Approaches for Coronary Artery Anomalies: Purpose and Techniques. Curr Cardiol Rep 21, 101 (2019). https://doi.org/10.1007/s11886-019-1188-7
Published:
DOI: https://doi.org/10.1007/s11886-019-1188-7