Abstract
Purpose
We have assessed whether additional upright imaging increases the confidence of interpretation of stress only supine myocardial perfusion imaging (MPI) in obese patients.
Methods and results
Tc-MIBI stress MPI of 101 consecutive patients (M = 49, 62 ± 12 years) with BMI ≥30 scanned on the D-SPECT cardiac camera were assessed. Images were interpreted as diagnostic or equivocal and the need for a rest study was recorded. Stress supine MPI was interpreted first, then gated and finally upright data were added. Defects on supine but not on upright were defined as artefacts and defects seen on both as abnormal. The total perfusion deficit (TPD) was also quantified. There were 27 normal, 22 abnormal, and 52 equivocal supine scans. The median EF was 52%, unaffecting the need for rest imaging. Upright imaging reclassified 32/52 (62%) equivocal studies as normal and 6/52 (11%) as abnormal (P < 0.001). Rest scan was deemed needed in 74/101 patients on supine vs 42/101 on supine/upright (P < 0.001). Supine TPD was normal in 53 and supine/upright TPD was normal in 70 patients (P < 0.001).
Conclusion
Supine stress MPI is inadequate in obese patients. The addition of upright imaging significantly increases the ability to interpret scans as diagnostic and may reduce considerably the need for rest imaging.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Stress MPI with single photon emission computed tomography (SPECT) is well established for the diagnosis and risk stratification of patients with known or suspected coronary artery disease (CAD). Soft tissue attenuation causes artefacts that reduce the diagnostic accuracy of MPI SPECT (MPS).1,2 Several methods have been proposed to determine the presence of artefacts. Gated stress/rest MPS has been used to characterize fixed myocardial defects as infarct or attenuation artefact.3 Combined prone and supine imaging has been proposed to improve inferior wall uniformity and to reduce artefacts associated with motion during supine acquisitions.4,5 Attenuation correction (AC) solutions have been developed and when applied to stress only MPI have been shown to reduce the need for rest imaging.6-10 Stress only MPI may have advantages compared to the conventional stress and rest protocols including improvement in patients’ convenience, reducing radiation exposure and increasing clinical throughput. Excellent outcome was demonstrated in patients with low to medium probability of CAD and normal stress only MPI with AC.11 Stress only imaging with AC was shown to be useful in patients with no prior history of CAD undergoing evaluation for bariatric surgery.12 The feasibility of stress only imaging using a CZT camera with no AC has been reported.13 AC is not typically available on D-SPECT and due to the design of the camera prone imaging is not possible. Combined-supine-upright stress MPS using high-speed (HS) SPECT with solid-state cadmium-zinc-telluride (CZT) detectors (D-SPECT, Spectrum-Dynamics) has high diagnostic accuracy for the detection of CAD in comparison to invasive coronary angiography.14 We have assessed whether combined supine-upright stress only MPI with D-SPECT increases the confidence of interpretation compared to stress-only supine MPI in a group of obese patients, thus reducing the physician-perceived need for rest imaging.
Material and methods
Study population
Stress-gated MPS studies of 103 consecutive obese patients (BMI ≥ 30) referred to the Institute of Nuclear Medicine, University College London Hospitals from September 2011 to December 2011 and imaged on the D-SPECT dedicated cardiac scanner were retrospectively interpreted by two experienced Nuclear Medicine physicians who were blinded to the clinical information. Two patients undergoing dobutamine stress did not achieve target heart rate and were excluded from further analysis. The clinical characteristics of the remaining 101 patients are summarized in Table 1. There were 49 (49%) male patients, the average age was 62 ± 12 years and the median BMI was 36 (IQR 32-39). Risk factors included diabetes (39%), hypertension (68%) and hypercholesterolemia (57%), and 35% of the patients had known CAD.
Our institutional review board granted permission to use pre-acquired anonymized patient data, and requirement for individual informed consent was waived.
Stress imaging protocol
Patients were instructed to discontinue beta-blockers and calcium antagonists 48 hour before testing and nitrates and caffeine-containing products 24 hour before testing. For pharmacological stress with adenosine (n = 98) an infusion of 140 μg/kg/min was given for 6 minutes with radiopharmaceutical injection between the 3rd and 4th minute, augmented where possible with low-level dynamic exercise. For pharmacological stress with dobutamine (n = 3) a continuous intravenous infusion was administered using 3 minutes stages at incremental doses of 10, 20, 30, and 40 μg/kg/min with radiopharmaceutical injection when ≥85% of maximum predicted heart rate was reached or at 40 μg/kg/min. 99mTc-sestamibi stress doses were 208-930 MBq (502 ± 214 MBq, depending on BMI) and the rest doses were 650-1150 MBq (866 ± 120 MBq), as part of 1-day stress/rest protocol (n = 53 [52%]) or 2-day protocol (BMI > 35).
HS-SPECT and image acquisition
Supine and upright images were acquired on the D-SPECT (Spectrum-Dynamics, Caesarea, Israel) HS-SPECT camera. The system comprises nine rotating pixilated detector columns of 5-mm-thick CZT crystals (2.46 × 2.46 mm), each fitted with a large aperture tungsten collimator, all within a stationary small 90° geometry gantry,15-17 scanning preferentially the heart. Six-minute stress gated (8 frames/cycle) supine acquisition (120 projections per detector, 3 seconds per projection) was performed approximately 45 minutes after the injection and was followed by a six minute upright acquisition. Transaxial images were generated using a custom designed Broadview reconstruction algorithm (Spectrum-Dynamics, Caesarea, Israel) based on the maximum likelihood expectation maximization method.16 No AC or scatter correction was applied. Images were re-oriented into short-axis, horizontal and vertical long-axis slices using QPS software (Cedars-Sinai Medical Center, LA, CA).
Visual assessment
The stress studies were interpreted in consensus in three stages: first, based on stress supine MPI alone, then after gated data were added, finally after the upright data were added as diagnostic (normal or abnormal) or equivocal. At this stage the rest studies were not provided for assessment. Concordant defects on supine and upright images were defined as abnormal and defects seen on supine but not on upright were defined as artefacts. In each study, the confidence of interpretation was noted as well as whether a rest study was considered necessary (in abnormal studies to determine fixed or reversible defects and in equivocal studies to determine whether the scan is normal or abnormal). All studies were then re-read blindly. At this stage both the stress and the rest components were provided, and the results were compared with the previous reading. Defects in the anterior and septal walls were allocated to the left anterior descending (LAD) artery, in the inferior wall to the right coronary artery (RCA) and in the lateral wall to the left circumflex (LCx) artery.
Quantitative assessment
Upright and supine images were quantified separately using their respective reference limits by automatic computer analysis.14,18 Automatically generated myocardial contours were evaluated by an experienced nuclear medicine technologist, blinded to the clinical data. In 5% of cases contours were adjusted to correspond to the myocardium. Stress perfusion defects were assessed by the total perfusion defect (TPD), expressed as percentage of the myocardium, which combines defect severity and extent,17,18 separately for supine (S-TPD), upright (U-TPD) and combined supine/upright (C-TPD). A mean absolute deviation >3.0 was used for limiting the TPD assessment from the supine images to pixels that have been quantified as abnormal on the upright images.14 C-TPD reflects the myocardium which is abnormal on both supine and upright scans in the same location, representing true perfusion defects. S-TPD > 5% and C-TPD > 3% were defined abnormal.14,18,19
Invasive coronary angiography
Nineteen patients underwent coronary angiography (ICA) within 90 days of MPI with no intervening coronary event, interventional procedure or change in symptoms. The presence of significant CAD was defined as a visually determined diameter stenosis of ≥70% in the left main, LAD, LCx, or RCA and their main branch vessels. Vessels supplied by patent bypass grafts were considered patent.
Statistical analysis
Continuous parametric variables are presented as mean ± SD and compared using student t test. Continuous non-parametric variables are presented as median (interquartile range, IQR) and compared using Mann-Whitney U test. Proportions were compared using χ2 analysis. A P value <0.05 was considered significant.
Results
Visual assessment
On stress only supine images there were 27 normal, 22 abnormal, and 52 equivocal studies. The median EF was 52% (IQR 52-68%) and did not change the need for rest imaging. Wall motion abnormalities were present in 17 patients, corresponding to the perfusion defects in abnormal scans, and did not change the need for rest imaging. In the 52 equivocal studies there were no regional wall motion abnormalities and the EF were all in the normal range (47%-80%). A rest scan was considered needed in all equivocal and abnormal scans, 74/101 (73%) patients.
After adding the upright scan, there were 59 normal, 28 abnormal, and 14 equivocal studies (Fig. 1). There was no change in interpretation of studies with a definitive diagnosis on supine; however, only 14/52 (27%) equivocal supine scans remained equivocal, whereas 32/52 (62%) studies were reclassified as normal and 6/52 (11%) as abnormal (P < 0.001) (Fig. 2) and the perceived need for a rest scan was reduced to 42/101 (42% for supine/upright vs 73% supine only, P < 0.001) (Fig. 3).
Twenty-six of 40 (65%) supine defects in the LAD territory and 17/48 (35%) supine defects in the RCA territory (P < 0.001) resolved on upright imaging.
Results in male and female patients
The results in male and female patients are summarized in Table 2. On supine imaging there were an identical number of male and female patients with equivocal scans (26 each). After adding the upright scan, 18/26 (69%) equivocal scans in male patients and 20/26 (77%) equivocal scans in female patients were reclassified as normal (15/18, 17/20) or abnormal (3/18, 3/20) (Table 2). The perceived need for rest scanning was reduced in males from 44 to 29 patients and in females from 30 to 13 patients.
In the 52 equivocal supine scans, LAD territory findings were more common in females (78%) and RCA territory findings were more common in males (80%) (P < 0.001).
Results in patients with and without previously known CAD
The results by presence or absence of CAD are summarized in Table 3. Obese patients with known CAD were more likely to have abnormal scans by combined supine and upright stress MPI (58% vs 10%). Considerable reduction in equivocal scans with additional upright imaging was noted in patients with known CAD (47% vs 8%) as well as patients without previously known CAD (55% vs 16%, P < 0.001 in both groups). Additional rest scan was deemed unnecessary in 25/67 (37%) patients with normal scans and with previously unknown CAD on supine MPI and in 49/67 (73%) when upright imaging was added (P < 0.001). In patients with known CAD rest imaging was considered unnecessary in 2/36 (5%) patients on supine MPI and in 12/36 (33%) when upright imaging was added (P < 0.001).
Comparison with blinded stress-rest reading
There were 67 normal stress-rest scans compared to 27 (40%) normal stress only supine and 58 (87%) normal on stress supine-upright. All normal supine only stress studies remained normal after reviewing the rest study.
Of 34 abnormal stress-rest scans 22 (65%) were abnormal on supine and 28 (82%) were abnormal on supine/upright.
Quantitative analysis
The median S-TPD was 4 (IQR 2.25-9), median U-TPD was 5 (IQR 3-10) and median C-TPD was 1 (IQR 0-5). By S-TPD there were 53 normal and 48 abnormal studies and by C-TPD there were 70 normal and 31 abnormal scans (P < 0.001). Twelve/14 equivocal scans by visual analysis were normal and 2/14 were abnormal by C-TPD. In addition there were 8 discrepant cases: four patients with normal MPI by visual analysis (supine equivocal, supine/upright normal) were abnormal on quantitative analysis. ICA was available in 5/8 patients and showed patent grafts in one patient. The remaining 4/8 patients had abnormal studies by visual analysis (both supine and upright) but normal C-TPD values. ICA showed in one patient LAD obstruction and no obstruction in 4, but aberrant RCA in one.
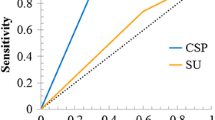
Correlation with ICA
Of 19 patients with ICA seven had 1-vessel disease, one had 3-vessel disease and 11 patients had no obstructive CAD. The sensitivity and specificity of supine stress were 93% and 70%, 93% and 93% for combined supine and upright stress and 93% and 90% when rest was added. Eight patients with no obstructive CAD had normal stress MPI by combined supine-upright visual assessment and 7/8 patients had normal C-TPD. There were 4 cases of “falsely abnormal” supine-upright stress studies in patients with previous infarcts and no coronary obstruction, two of these were also abnormal by C-TPD. One equivocal supine stress only study (LCx territory) was normal on stress only supine-upright, but was abnormal after the rest scan (Table 4) (“false negative supine/upright”) and had abnormal C-TPD. ICA revealed LCx stenosis. In addition, one patient with aberrant origin of RCA had a falsely abnormal visual assessment and a falsely abnormal C-TPD.
Discussion
We explored whether the addition of upright stress imaging to the conventional supine stress imaging in obese patients imaged with D-SPECT increases the proportion of patients in whom stress only imaging might be performed. Our results show that the additional upright acquisition resulted in a significant improvement in reader’s confidence, with a 73% reduction in the number of equivocal studies and a 43% reduction in the number for whom additional rest imaging was considered necessary. Furthermore, in a subgroup of patients undergoing ICA, there was excellent agreement between the interpretations of the combined supine-upright stress scans and ICA findings.
Comparison with other studies
Stress only MPI has been previously recommended in selected groups of patients, but its use is limited by attenuation artefacts.20 ECG-gated Tc-99m sestamibi MPI enables to characterize fixed myocardial perfusion defects as infarct or artefact, showing improved specificity over perfusion SPECT alone for the detection of CAD, reducing borderline normal and abnormal readings in patients with a low likelihood of CAD, and helping defining studies as abnormal in patients with known CAD.3,21 In our population none of the equivocal studies showed wall motion abnormalities, therefore gated SPECT did not affect the interpretations, likely due to the design of the study, as only stress images were available for review.
AC has been shown to reduce attenuation artefacts and to improve the specificity of MPI.6-9 In 90 stress only MPI 37% were interpreted as definitely normal or abnormal while 77% needed additional rest imaging, which reduced to 43% with AC (9). In 1,383 stress only MPI in symptomatic patients 58% were abnormal, 83% of them were re-classified as normal after AC.10 In 257/383 obese patients undergoing evaluation for bariatric surgery stress only MPI resulted in a high percentage of normal studies with no need for further rest imaging.12
Attenuation correction is not typically available on D-SPECT. On conventional gamma cameras combined supine and prone MPI has been shown to be more accurate than supine MPI alone.4,5 Due to the design of D-SPECT prone imaging is not possible. However, the principle of changing position to differentiate attenuation artefacts from real perfusion defects can be obtained on this specific camera by supine/upright imaging.22 Recently automated quantification of combined supine-upright MPI on HS-SPECT has been developed, using combined reference limits for supine-upright imaging, showing high diagnostic accuracy for detecting clinically significant CAD.14 Using combined supine-upright MPS and visual analysis on HS-SPECT, we observed in obese patients similar findings to Heller et al. with conventional SPECT and AC.9 In our data 49% of stress supine studies were interpreted as definitely normal or abnormal and 73% needed further rest imaging, but with supine-upright 86% of studies were interpreted as definitely normal or abnormal and rest imaging was needed in 42%. In this study, a lower percent of patients had definitely normal supine MPI compared to Mathur et al. with no AC10 (27% vs 58%, respectively), possibly due to the different selection criteria of the studies, i.e., obese patients in our series and clinically indicated stress only MPI in Mathur’s series. The addition of upright MPI has increased the percent of studies with definite interpretation in our series, as did AC in Mathur’s series (59% vs 83%, respectively).
Several studies have shown comparable prognostic value of stress only MPI with AC while reducing radiation exposure in comparison with the conventional stress-rest protocol.11,12,21,23,24 In 729 patients referred to the emergency room for the assessment of chest pain a normal stress only scan was associated with 0.6% cardiac event rate.13 In 16,854 patients with a normal stress MPI scan, followed for 4.76 years, there were no significant differences in mortality in patients with normal stress only vs patients with normal stress-rest MPI.23 Duvall et al.24 have assessed 1,673 patients with normal stress only MPI and 3,237 patients with a normal rest-stress MPI. At 40 months follow up total deaths and cardiac deaths were 2.7% and 0.4% in the stress-only group vs 3.7% and 0.5% in the rest-stress group. In obese patients undergoing preoperative assessment with MPI with AC prior to bariatric surgery 253/383 (67%) underwent stress-only imaging and had normal studies. 1-year survival was 99% in patients with normal as in patients with abnormal MPI.12
Limitations
The study is limited by its retrospective nature and includes a heterogeneous group of patients; however, consecutive obese patients were enrolled, representing clinical referrals. This is a single center study; the readers were experienced with HS-SPECT. Therefore there may be variability in visual assessment if performed in other centers. In addition, visual assessment of the studies was sequential, beginning with stress supine MPI. Therefore, there may have been a bias in the readings. However, this is the routine clinical setting in our department, supine MPI is the standard and upright imaging is used to clarify equivocal findings. The readers stated whether they would have deemed a rest study as needed; however, this was in a setting of already collected data, and whether the rest studies would actually have not been obtained in the clinical setting could not be assessed. There was no gold standard in most patients, however, comparison to blinded stress-rest interpretation revealed overall good agreement. In addition, the results of ICA in a subgroup of 19 patients showed excellent agreement with the stress only combined supine-upright interpretations in 18/19 patients. Finally, radiation dose reduction has been achieved in obese patients using a low dose protocol on a CZT camera,25 but was not part of this study. However, our results suggest that stress only supine/upright MPI has the potential to reduce radiation exposure in obese patients by increasing reporting confidence.
New Knowledge Gained
This study shows for the first time the added clinical value of additional upright MPI in obese patients undergoing supine MPI on the D-SPECT camera. In the absence of attenuation correction and since prone imaging is not possible with this specific camera the additional upright scan may improve the accuracy of D-SPECT MPI.
Conclusion
In obese patients undergoing stress MPI on D-SPECT stress only supine imaging is inadequate. The addition of upright to the supine stress imaging increases reader’s confidence and reduces significantly the perceived need for further rest imaging. If proven in larger prospective patient series, the actual ability of the approach to reduce the need for resting scans in obese patients can be validated, potentially reducing considerably radiation exposure, while also increasing patient throughput.
References
Kim C, Kwok YS, Heagerty P, Redberg R. Pharmacologic stress testing for coronary disease diagnosis: a meta-analysis. Am Heart J 2001;142:934-44.
Singh B, Bateman TM, Case JA, Heller G. Attenuation artefact, attenuation correction and the future of myocardial perfusion SPECT. J Nucl Cardiol 2007;14:153-64.
DePuey EG, Rozanski A. Using gated technetium-99m-sestamibi SPECT to characterize fixed myocardial defects as infarct or artefact. J Nucl Med 1995;36:952-5.
Kiat H, Van Train KF, Friedman JD, et al. Quantitative stress-redistribution thallium-201 SPECT using prone imaging: methodologic development and validation. J Nucl Med 1992;33:1509-15.
Hayes SW, De Lorenzo A, Hachamovitch R, et al. Prognostic implications of combined prone and supine acquisitions in patients with equivocal or abnormal supine myocardial perfusion SPECT. J Nucl Med 2003;44:1633-40.
Ficaro EP, Fessler JA, Shreve PD, et al. Simultaneous transmission/emission myocardial perfusion tomography. Diagnostic accuracy of attenuation-corrected 99mTc-sestamibi single-photon emission tomography. Circulation 1996;93:463-73.
Vidal R, Buvat I, Darcourt J, et al. Impact of attenuation correction by simultaneous emission/transmission tomography on visual assessment of 201Tl myocardial perfusion images. J Nucl Med 1999;40:1301-9.
Hendel RC, Corbett JR, Cullom SJ, et al. The value and practice of attenuation correction for myocardial perfusion SPECT imaging: a joint position statement from the American Society of Nuclear Cardiology and Society of Nuclear Medicine. J Nucl Cardiol 2002;9:135-43.
Heller GV, Bateman TM, Johnson LL, et al. Clinical value of attenuation correction in stress-only Tc-99m sestamibi SPECT imaging. J Nucl Cardiol 2004;11:273-81.
Mathur S, Heller GV, Bateman TM, et al. Clinical value of stress-only Tc-99m SPECT imaging: importance of attenuation correction. J Nucl Cardiol 2013;20:27-37.
Gibson PB, Demus D, Noto R, et al. Lowe vent rate for stress-only perfusion imaging in patients evaluated for chest pain. J Am Coll Cardiol 2002;39:999-1004.
Gemignani AS, Muhlebach SG, Abbott BG, Roye GD, Harrington DT, Arrighi JA. Stress-only or stress/rest myocardial perfusion imaging in patients undergoing evaluation for bariatric surgery. J Nucl Cardiol 2011;18:886-92.
Duvall WL, Baber U, Levine EJ, Croft LB, Henzlova MJ. A model for the prediction of a successful stress-first Tc-99m SPECT MPI. J Nucl Cardiol 2012;19:1124-34.
Nakazato R, Tamarappoo BK, Kang X, et al. Quantitative upright-supine high-speed SPECT myocardial perfusion imaging for detection of coronary artery disease: correlation with invasive coronary angiography. J Nucl Med 2010;51:1724-31.
Sharir T, Ben-Haim S, Merzon K, et al. High-speed myocardial perfusion imaging: initial clinical comparison with conventional dual detector anger camera imaging. JACC Cardiovasc Imaging 2008;1:156-63.
Gambhir SS, Berman DS, Ziffer J, et al. A novel high-sensitivity rapid-acquisition single-photon cardiac imaging camera. J Nucl Med 2009;50:635-43.
Slomka PJ, Patton JA, Berman DS, Germano G. Advances in technical aspects of myocardial perfusion SPECT imaging. J Nucl Cardiol 2009;16:255-76.
Slomka PJ, Nishina H, Berman DS, et al. Automated quantification of myocardial perfusion SPECT using simplified normal limits. J Nucl Cardiol 2005;12:66-77.
Xu Y, Fish M, Gerlach J, et al. Combined quantitative analysis of attenuation corrected and non-corrected myocardial perfusion SPECT: method development and clinical validation. J Nucl Cardiol 2010;17:591-9.
Bhavanni SP, Heller GV. Stress-only myocardial perfusion imaging … it IS time for a change! J Nucl Cardiol 2011;18:836-9.
Taillefer R, DePuey EG, Udelson JE, Beller GA, Latour Y, Reeves F. Comparative diagnostic accuracy of Tl-201 and Tc-99m sestamibi SPECT imaging (perfusion and ECG-gated SPECT) in detecting coronary artery disease in women. J Am Coll Cardiol 1997;29:69-77.
Berman DS, Kang X, Tamarappoo B, et al. Stress thallium 201/rest technetium 99m sequential dual isotope high-speed myocardial perfusion imaging. JACC Cardiovasc Imaging 2009;2:273-82.
Chang SM, Nabi F, Xu Y, Raza U, Mahmarian JJ. Normal stress-only versus standard stress/rest myocardial perfusion imaging: similar patient mortality with reduced radiation exposure. J Am Coll Cardiol 2009;55:221-30.
Duvall WL, Wijetunga MN, Klein TM, et al. The prognosis of a normal stress-only Tc-99m myocardial perfusion imaging study. J Nucl Cardiol 2010;17:370-7.
Gimelli A, Bottai M, Giorgetti A, Genovesi D, Filidei E, MArzullo P. Evaluation os ischaemia in obese patients: feasibility and accuracy of a low-dose protocol with a cadmium-zinc telluride camera. Eur J Nucl Med Mol Imaging 2012;39:1254-61.
Acknowledgement
This study was undertaken at UCLH/UCL who received a proportion of funding from the Department of Health’s NIHR Biomedical Research Centres funding scheme. Dr. Simona Ben-Haim is consultant for Spectrum-Dynamics. Dalia Shiti is employed by Spectrum-Dynamics. Dr. Daniel Berman owns shares at Spectrum-Dynamics and is a member of the Medical Advisory Board and consultant for Spectrum-Dynamics.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ben-Haim, S., Almukhailed, O., Neill, J. et al. Clinical value of supine and upright myocardial perfusion imaging in obese patients using the D-SPECT camera. J. Nucl. Cardiol. 21, 478–485 (2014). https://doi.org/10.1007/s12350-014-9853-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-014-9853-0