Abstract
Background
ECG-gated SPECT myocardial perfusion imaging is usually acquired in supine position. However, some patients are not comfortable in this position for a variety of personal or medical reasons. Our aim was to investigate the effect of patient positioning on quantitative SPECT imaging results using normal supine database.
Methods
55 patients (mean age 58.5 ± 8.3 years) were enrolled in this prospective study. Each patient had a pair of ECG-gated stress SPECT myocardial perfusion images acquired on two gamma cameras: one in supine position and the other in upright sitting position. Left ventricular (LV) ejection fraction (EF), end-diastolic (ED), and end-systolic (ES) left ventricular volumes (V), LV mass, summed stress perfusion defect score (SSS), and total severity score (TSS) were calculated automatically relative to a supine normal reference database.
Results
There were no significant differences in LVEF using the two cameras (0.65 ± 0.08 vs. 0.66 ± 0.10; P > 0.1). However, EDV, ESV, and LV mass were significantly smaller in sitting position than in supine position (89 vs. 80 ml; 33 vs. 29 ml and 115 vs. 109 ml, respectively, all P < 0.0001). On the other hand, SSS and TSS were significantly higher in sitting position than in supine position (5.16 vs. 8.73 and 166.82 vs. 288.27, both P < 0.0001). Overall, more studies in sitting position were interpreted as abnormal than in supine position (P < 0.05).
Conclusion
Patient positioning has a significant impact on quantitative gated SPECT imaging results. Using a supine normal reference database, SSS and TSS were larger in sitting position than in supine position. Thus, for imaging in sitting position, separate normal limits are required.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
ECG-gated stress SPECT myocardial perfusion imaging is a well-established procedure for diagnosing and assessing the risk of coronary artery disease. Its excellent negative predictive value (>98%) makes radionuclide imaging an appropriate means for identifying low risk patients. Numerous studies have shown that patients with normal stress myocardial perfusion images are at low risk for future cardiovascular events.1,2 Information regarding wall motion abnormalities, left ventricular ejection fraction, and ventricular function and dimensions, in addition to conventional myocardial perfusion parameters, are all important aids in formulating a more complete clinical diagnosis.3,4,5
SPECT images are usually acquired with the patient in supine position. However, some patients are not able to lie flat on their back for an extended period of time because of a variety of medical or personal problems (e.g., orthopedic conditions, congestive heart failure, claustrophobia, etc.).
In recent years, SPECT gamma cameras have been developed, which allow for imaging with the patient in sitting or upright position.6,7,8 The upright sitting position alters the position and shape of the heart, and consequently changes soft tissue attenuation.9
Clinical stress SPECT imaging routinely incorporates commercial software for quantification of LV function and volumes and, most importantly, quantification of regional myocardial perfusion abnormalities relative to a normal reference database.12 These commercially available normal databases were created from images obtained in normal volunteers in supine position, or sometimes in prone position.
In recent years, several original articles focused on differences in imaging results using different types of gamma cameras. It has been noted that imaging in the upright position leads to fewer attenuation artifacts and that at the same time, this position was perceived by patients to be more comfortable.10,11 The aim of the present study was to evaluate the impact of patient positioning, specifically the sitting position, on quantitative ECG-gated SPECT myocardial perfusion imaging results using normal supine database.
Methods
Patients
Fifty-five patients were enrolled in this prospective study. All patients were referred for evaluation of exertional angina pectoris. The clinical characteristics of the patients are shown in Table 1. The average BMI of the study cohort was 28.7 ± 4.1. Twenty-one patients (38%) were obese (BMI > 30). This is consistent with the increasing incidence of overweight among the Hungarian population.
SPECT Imaging
All patients had vasodilator stress SPECT myocardial perfusion imaging after an overnight fast. Coffee and caffeine-containing medication, aminophylline, nitrates, or betablockers were withheld for at least 12 hour. Three min after completion of the dipyridamole infusion (0.56 mg/kg over 4 min), 400-450 MBq of technetium-99 m SestaMIBI was administered. Patients with BMI > 30 received a dose of 650 MBq.
Supine SPECT imaging was always performed first with the Cardio-C (CC) camera (Mediso Ltd, Budapest, Hungary) starting at 60-90 min after radiotracer injection to avoid the significant influence of background activity. Moreover, to decrease high hepatic concentration and to avoid liver-dominant SPECT images, a fatty meal or drink was commonly used to speed hepatobiliary clearance of the SestaMIBI. As soon as supine image acquisition was completed, the patients were moved to the CardioDesk (CD) camera (Mediso Ltd, Budapest, Hungary) for repeat imaging, now in sitting position. The mean time between the two acquisitions was 32.5 ± 5.26 min. The acquisition parameters for both cameras were the identical: low-energy high-resolution parallel-hole collimators; energy window (20%) symmetrically set over 140 keV; and 64 projections acquired over a 180° arc with 27 sec per stop. The image matrix was 64 × 64. For ECG gating, the R-R interval was divided into eight frames. No attenuation correction was applied.
Both cameras have two large field-of-view high-resolution, rectangular detectors at a fixed 90° angle (Figure 1). The only difference is the starting position of the detector heads: for the CC camera one crystal surface was positioned horizontally and the other vertically, whereas for the CD camera both crystal surfaces were in vertical position. The detector heads of both cameras rotated over a 90° arc during image acquisition. The sizes of the NaI crystals were identical (430 × 244 mm with a thickness of 9.5 mm), and each detector head housed 33 photomultipliers. Same camera installation was used, and the pixel size was also the same in both cameras (pixel size: 6 mm).
Interview XP software package (Mediso Ltd, Budapest, Hungary) was used for SPECT image reconstruction. Butterworth pre-filter (Eq. 1) was applied on each 2D projection.
(cut off to 0 (CoFZ): 70, Gain: 0, cut off frequency (CoF): 0.22, Order: 25;), OSEM iterative reconstruction were used.
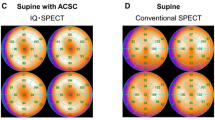
Reconstructed tomographic slices were imported into the Emory Cardiac Toolbox 3.2 (ECTb) software for quantitative analysis. During post-processing automatic contour detection was used to define the border of the myocardium (Figure 2). Image quantification was performed relative to the ECTb normal reference database. According to manufacturer’s information, this normal database was generated from 30 healthy male and 30 healthy female volunteers with low-likelihood of coronary artery disease. These volunteers had one-day stress-rest Tc-99 m Sestamibi SPECT imaging in supine position. Quantitative image data were automatically generated: left ventricular (LV) ejection fraction (EF), end-diastolic volume (EDV), end-systolic volume (ESV), LV mass (MASS). After the assignment of the center of the imaged myocardium, end-diastolic, endocardial, and epicardial borders can be estimated. Fourier analysis of the size-intensity relationship is used to compute the wall thickening throughout the cardiac cycle. During the hearth cycle, endocardial and epicardial boundary points can be determined by subtracting and adding one-half of the myocardial thickness to the myocardial center. From the calculated epicardial and endocardial volumes, left ventricular volume can also be extracted.
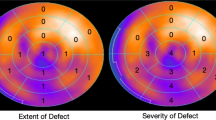
17-segment bull’s eye display of summed stress scores (SSS) and total severity score (TSS), and wall motion score were also calculated automatically. The TSS reflects both the extent and severity of myocardial perfusion abnormality and is computed on the basis of regional relative variance of radiotracer uptake compared to normal limits.
Diagnostic Image Categorization
For the present study, only stress SPECT images were used for analysis. Two experienced physicians, blinded to the patients’ medical history and clinical image interpretations, re-analyzed all the image data independently. Thus, reconstructed tomographic slices, and 17-segment bull’s eye display of regional myocardial perfusion, and wall motion were reviewed in static and dynamic cine modes, when available. Based on an integrated review of all available data on each camera, the studies were then categorized as either normal (no perfusion defect and normal, regional, and global functions (0) or abnormal.1 The interpretive 0 or 1 scores were tabulated. The numerical differences of interpretive scores (difference score) between the two cameras were recorded. For further analysis, the difference scores of the two physicians was averaged. Thus, an average difference score of 0 meant identical categorization as either normal or abnormal by both readers on images generated by the two different cameras. An averaged difference of −0.5 or 0.5 indicated that one physician concluded that the two acquisitions were different (a difference of 1 or −1), whereas the other physician concluded they were similar (difference 0). Finally, an average difference score of −1 or 1 indicated that both readers agreed that the images of the two cameras were different. Since imaging with the CC camera was always done first, a negative score sign indicates that the CC study was normal, whereas for the CD study, it was considered abnormal.
Statistical Analysis
All data are presented as mean ± standard deviation, or as median and range when appropriate. GraphPad Prism 6.0 package was used for statistical analysis.
Differences of numerical data were analyzed for statistical significance using the paired t test, Student t test, or Fisher’s exact test. For normally distributed data, the paired t test or Shapiro-Wilk test was used. For the comparison of nonparametric categorical data, the Wilcoxon Signed Rank test was used. A P value ≤0.05 was considered statistically significant.
The primary endpoints of our study were the automatically generated quantitative SPECT LV function and regional myocardial perfusion data. A secondary endpoint was the overall diagnosis by the two experienced readers: interpretive scores 0 or 1.
The differences (median and quartiles) between parameters derived from images acquired on the two cameras were displayed as Box and whisker plots.
Results
All 55 patients had good diagnostic quality static SPECT images. In two patients, ECG-synchronized gating failed because of irregular heart rate, and the gated SPECT studies were not of diagnostic quality. Thus, ECG-gated data were available in 53 patients.
Quantitative SPECT Imaging Parameters
The results of comparative quantitative statistical analysis of LV functional and regional myocardial perfusion parameters derived from images acquired with both cameras are shown in Table 2 and in Figures 3, 4 and 5.
Differences in LV functional and myocardial perfusion parameters measured in supine and sitting imaging positions in all patients. The results of statistical analysis are displayed as scatter plots. The median difference is represented by the vertical line within the figure. TOP left ventricular (LV) function parameters (n = 53): LV mass (MASS), end-systolic volume (ESV), end-diastolic volume (EDV), and LV ejection fraction (EF). The differences (median and quartile ranges) are shown. BOTTOM LEFT Summed stress scores (SSS) (n = 55). BOTTOM RIGHT Total severity scores (TSS) (n = 55). Significant differences are indicated by * (see also text)
Differences in LV function and myocardial perfusion parameters measured in supine and sitting imaging positions in patients with BMI < 30. The display is identical to that in Figure 3
Differences in LV function and myocardial perfusion parameters measured in supine and sitting imaging position in patients with BMI > 30. The display is identical to that in Figure 3
LV Function and Volumes
In the entire patient cohort population, the mean LVEF computed from gated SPECT images acquired on both cameras was not different (P = NS). However, mean EDV, ESV, and LV mass values were significantly (P < 0.0001) lower in sitting position (CD) than in supine position (CC) (Figure 3). The analysis results were similar in males and females (Table 2). Women had significantly (P < 0.01) smaller LV volumes than men.
When the patients were divided into those with BMI > 30 and BMI < 30, again LVEF was not different in the two imaging positions. Also, EDV and ESV were again significantly smaller in sitting position (CD) than in supine position (Figures 4, 5). However, although in patients with BMI < 30, LV mass was significantly less in sitting position than in supine position, in patients with BMI > 30, there was no such significant difference. (Table 2).
Regional Myocardial Perfusion
In the entire cohort of 55 patients, SSS and TSS were significantly (P < 0.0001) larger in sitting position than in supine position (Figure 3). The same was found when males and female were analyzed separately (Table 2). Patients with BMI < 30 also had higher SSS and TSS in sitting position than in supine position (Figure 4). However, although patients with BMI > 30 also had significantly higher SSS in sitting position, the TSS was not statistically different compared with supine position (Table 2; Figure 5). By the analysis of vascular territories, higher amount of RCA and LAD defects were observed with CardioDesk (Physician #1: LAD-7 vs.11 cases, RCA-5 vs. 10 cases; Physician #2: LAD-5 vs 9 cases, RCA-6 vs. 8 cases, CC and CD, respectively) (Table 5).
Overall Interpretive Score
The two readers were in complete agreement with each other in 40 (72%) of 55 paired patient studies (Table 3). The distribution of disagreements in 15 paired SPECT studies is also shown in Table 3. Disagreements appeared to occur more often on SPECT images of women than on those of men. Based on all available imaging information, physician #1 interpreted 14 (25%) of 55 SPECT images acquired in supine position as abnormal, whereas he interpreted 22 (40%) of the SPECT images acquired in sitting position as abnormal. Similarly, physician #2 interpreted 13 (24%) of the images acquired in supine position as abnormal and 19 of the images acquired in sitting position (35%) as abnormal. Thus, overall more SPECT studies acquired in sitting position were interpreted as abnormal than those acquired in supine position (P < 0.05) (Table 4).
Discussion
This study demonstrates that patient positioning has a significant and quantifiable impact on semi-quantitative and quantitative parameters derived from ECG-gated SPECT imaging. In the upright sitting position, regional myocardial perfusion abnormalities (SSS and TSS) were significantly larger than in the conventional supine position. On the other hand, EDV, ESV, and LV mass were significantly smaller in upright sitting position, whereas LVEF was not affected. Our analysis further showed that not only were there quantitative differences, but also significant differences in overall image interpretation by experienced readers.
It has long been recognized that myocardial perfusion images may be different when acquired in supine, prone or left-lateral position.8,9,10,11 The different image appearance is attributed to soft tissue attenuation. In some laboratories, this understanding is even used for identifying soft tissue attenuation artifacts by reviewing images acquired in both positions.13,14 Such artefactual different appearance may be altered using attenuation correction devices.11
Several investigators also reported differences in LV dimensions in different positions.15,16,17,18,19,21 The smaller volumes of EDV and ESV in the sitting position can be readily explained by decreased LV preload. Since LVEF represents a ratio of volumes, and EDV and ESV are equally affected by a change in position, it should be no surprise that LVEF was unchanged (Table 5).
Over the recent decades, important innovations have been introduced in SPECT gamma camera design, detector geometry, reconstructive software, and also by introducing imaging in different body positions. Traditionally, cardiac SPECT imaging was performed with the patient in supine position. This position may be uncomfortable for patients with orthopedic shoulder or back problems, congestive heart failure, obesity, debilitating illness, or simply claustrophobia. This may be especially problematic when imaging time is prolonged. Most patients, when given the choice, prefer imaging in sitting position rather than in supine position.10
Thus far, published reports on differences of myocardial perfusion images acquired in supine or sitting position were based on subjective segmental scoring, although some reports describe differences in the quantitatively determined scores.10,11 Our analysis was based on computer-generated semi-quantitative SSS and TSS.
In many laboratories, quantitative software is routinely used to improve reproducibility of interpretation, which is suboptimal when limited to subjective visual analysis.22,23 Presently available commercial quantitative software packages incorporate normal reference databases derived from volunteers imaged in supine position. To the best of our knowledge, no commercial software offers normal databases for imaging in sitting position. Our quantitative analysis was done using a supine normal reference database.
The observation of significant quantitative differences in SSS and TSS in sitting position does not necessarily imply that imaging in sitting position is more accurate. Since the differences were independent of anatomic location, gender, and BMI, our findings cannot readily be explained by altered soft tissue attenuation in sitting position alone.
Limitations of Study
An important limitation of our study is that no attenuation correction was applied in either the supine or sitting position. Certain inferior diaphragmatic attenuation artifacts may be less in the sitting position, whereas anterior breast artifacts may be more pronounced while sitting. Accordingly it is unclear why in our analysis, myocardial perfusion abnormalities were consistently larger in the sitting position, regardless of anatomic location, gender, and BMI. These issues may only be resolved by the use of position-specific normal reference databases and attenuation correction.
In our imaging protocol, each patient had supine imaging first, followed by imaging in sitting position. It is conceivable that, although unlikely, with the increasing time interval after stress, the effects of ischemia on radiotracer uptake and regional wall motion may have been different.24,25,26 All our patients underwent pharmacological stress, which generates flow heterogeneity, but rarely true myocardial ischemia. Nevertheless, it would have been preferable using a random sequence of imaging. The lack of rest acquisition analysis is an important limitation of our study; however, the expansion of our study population with rest acquisition would add a new parameter resulting in a slight heterogeneity in the statistical analysis and leading to further possibilities for discrepancies.
Conclusion
The results of our study show that body position of a patient during SPECT image acquisition has an important and quantifiable impact on cardiac functional and regional myocardial perfusion parameters. In 13% of the patients studied, experienced readers came to different diagnostic conclusions when reviewing all available SPECT image data acquired in sitting position than in supine position. These results emphasize that specific normal databases must be developed and used for the specific position in which a patient is imaged.
New Knowledge Gained
Patient positioning during SPECT image acquisition has an important and quantifiable impact on LV functional and regional myocardial perfusion parameters. Specific normal databases must be used for specific patient positions.
Abbreviations
- MPI:
-
Myocardial perfusion imaging
- SPECT:
-
Single photon emission computed tomography
- SSS:
-
Summed stress score
- TSS:
-
Total severity score
- LVEF:
-
Left ventricular ejection fraction
- EDV:
-
End-diastolic volume
- ESV:
-
End-systolic volume
- ECTb:
-
Emory cardiac tool box
- BMI:
-
Body mass index
References
Iskander S, Iskandrian AE. Risk assessment using single-photon emission computed tomographic technetium-99 m sestamibi imaging. J Am Coll Cardiol 1998;32:57-62.
Hachamovitch R, Hayes S, Friedman JD, Cohen I, Shaw LJ, Germano G, et al. Determinants of risk and its temporal variation in patients with normal stress myocardial perfusion scans: What is the warranty period of a normal scan? J Am Coll Cardiol 2003;41:1329-40.
Sharir T, Germano G, Kavanagh PB, Lai S, Cohen I, Lewin HC, et al. Incremental prognostic value of post-stress left ventricular ejection fraction and volume by gated myocardial perfusion single photon emission computed tomography. Circulation 1999;100:1035-42.
Shaw LJ, Iskandrian AE. Prognostic value of gated myocardial perfusion SPECT. J Nucl Cardiol 2004;11(2):171-85.
Iskandrian AE, Heo J, Mehta D, Tauxe EL, Yester M, Hall MB, et al. Gated SPECT perfusion imaging for the simultaneous assessment of myocardial perfusion and ventricular function in the BARI 2D trial: An initial report from the nuclear core laboratory. J Nucl Cardiol 2006;13(1):83-90.
Songy B, Lussato D, Guernou M, Queneau M, Geronazzo R. Comparison of myocardial perfusion imaging using thallium-201 between a new cadmium-zinc-telluride cardiac camera and a conventional SPECT camera. Clin Nucl Med 2011;36(9):776-80.
Garcia EV, Faber TL, Esteves FP. Cardiac dedicated ultrafast SPECT cameras: New designs and clinical implications. J Nucl Med 2011;52(2):210-7.
Ben-Haim S, Almukhailed O, Neill J, Slomka P, Allie R, Shiti D, Berman DS, Bomanji J. Clinical value of supine and upright myocardial perfusion imaging in obese patients using the D-SPECT camera. J Nucl Cardiol 2014;21(3):478-85.
Chawla D, Rahaby M, Amin AP, Vashistha R, Alyousef T, Martinez HX, Doukky R. Soft tissue attenuation patterns in stress myocardial perfusion SPECT images: A comparison between supine and upright acquisition systems. J Nucl Cardiol 2011;18(2):281-90.
Tonge CM, Armstrong IS, Arumugam P, James JM, Al-Bahrani GI, Lawson RS, et al. Changes in the appearance of attenuation artefacts due to change in posture in myocardial perfusion imaging. Nucl Med Commun 2008;29(5):441-7.
Tout D, Tonge C, Austin P, Adams J, Arumugam P. A comparison between upright and supine myocardial perfusion imaging with attenuation correction. Nucl Med Commun 2014;35(8):832-8.
Danias PG, Ahlberg AW, Travin MI, Mahr NC, Abreu JE, Marini D, et al. Visual assessment of left ventricular perfusion and function with electrocardiography-gated SPECT has high intraobserver and interobserver reproducibility among experienced nuclear cardiologists and cardiology trainees. J Nucl Cardiol 2002;9(3):263-70.
Nishina H, Slomka PJ, Abidov A, Yoda S, Akincioglu C, Kang X, et al. Combined supine and prone quantitative myocardial perfusion SPECT: Method development and clinical validation in patients with no known coronary artery disease. J Nucl Med 2006;47(1):51-8.
Nakazato Ryo, Tamarappoo Balaji K, Kang Xingping, Wolak Arik, Kite Faith, Hayes Sean W, et al. Quantitative upright-supine high-speed SPECT myocardial perfusion imaging for detection of coronary artery disease: Correlation with invasive coronary angiography. J Nucl Med 2010;51(11):1724-31.
Heo J, Htay T, Mehta D, Sun L, Lacy J, Iskandrian AE. Assessment of left ventricular function during upright treadmill exercise with tantalum 178 and multiwire gamma camera. J Nucl Cardiol 2005;12(5):560-6.
Ather S, Iqbal F, Gulotta J, Aljaroudi W, Heo J, Iskandrian AE, Hage FG. Comparison of three commercially available softwares for measuring left ventricular perfusion and function by gated SPECT myocardial perfusion imaging. J Nucl Cardiol 2014;21(4):673-81.
Rowland T, Unnithan V, Barker P, Guerra M, Roche D, Lindley M. Orthostatic effects on echocardiographic measures of ventricular function. Echocardiography 2012;29(5):523-7.
Schaefer WM, Lipke CS, Kühl HP, Koch KC, Kaiser HJ, Reinartz P, et al. Prone versus supine patient positioning during gated 99mTc-sestamibi SPECT: Effect on left ventricular volumes, ejection fraction, and heart rate. J Nucl Med 2004;45(12):2016-20.
Thadani U, West RO, Mathew TM, Parker JO. Hemodynamics at rest and during supine and sitting bicycle exercise in patients with coronary artery disease. Am J Cardiol 1977;39:776.
Thadani U, Parker JO. Hemodynamics at rest and during supine and sitting bicycle exercise in normal subjects. Am J Cardiol 1978;41:52.
Manyari DE, Kostuk WJ. Left and right ventricular function at rest and during bicycle exercise in the supine and sitting positions in normal subjects and patients with coronary artery disease. Assessment by radionuclide ventriculography. Am J Cardiol 1983;51(1):36-42.
Mahmarian JJ, Moye LA, Verani MS, Bloom MF, Pratt CM. High reproducibility of myocardial perfusion defects in patients undergoing serial exercise thallium-201 tomography. Am J Cardiol 1995;75:1116-9.
Berman DS, Kang X, Gransar H, Gerlach J, Friedman JD, Hayes SW, et al. Quantitative assessment of myocardial perfusion abnormality on SPECT myocardial perfusion imaging is more reproducible than expert visual analysis. J Nucl Cardiol 2009;16(1):45-53.
Paul AK, Hasegawa S, Yoshioka J, Tsujimura E, Yamaguchi H, Tokita N, et al. Characteristics of regional myocardial stunning after exercise in gated myocardial SPECT. J Nucl Cardiol 2002;9:388-94.
Ward RP, Gundeck EL, Lang RM, Spencer KT, Williams KA. Overestimation of postischemic myocardial stunning on gated SPECT imaging: Correlation with echocardiography. J Nucl Cardiol 2006;13(4):514-20.
Demir H, Kahraman G, Isgoren S, Tan YZ, Kilic T, Berk F. Evaluation of post-stress left ventricular dysfunction and its relationship with perfusion abnormalities using gated SPECT in patients with cardiac syndrome. Nucl Med Commun 2008;29(3):208-14.
Acknowledgments
This article was finalized under the auspices of the “Mentorship at Distance” committee of the Journal of Nuclear Cardiology. The authors gratefully acknowledge the editorial suggestions by Frans J. Th. Wackers, MD, PhD.
Disclosure
The authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kracskó, B., Barna, S., Sántha, O. et al. Effect of patient positioning on the evaluation of myocardial perfusion SPECT. J. Nucl. Cardiol. 25, 1645–1654 (2018). https://doi.org/10.1007/s12350-017-0865-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-017-0865-4