Abstract
Background
Significance of electrocardiographic (ECG) changes during vasodilator stress myocardial perfusion imaging (MPI) is controversial. We examined the diagnostic and prognostic significance of ECG changes during vasodilator single photon emission computerized tomography (SPECT) MPI.
Methods
We studied consecutive patients who underwent vasodilator SPECT MPI from 1995 to 2009. Patients with baseline ECG abnormalities, previous history of coronary artery bypass graft surgery or myocardial infarction (MI) were excluded. Significant coronary artery disease (CAD) was defined as >70% stenosis of any vessel or ≥50% stenosis of left main. Mean follow-up was 2.4 ± 1.5 years for cardiac events (cardiac death and non-fatal MI).
Results
Of patients in the diagnostic cohort, ST depression was associated with increased incidence of CAD with abnormal (P = .020 and P <.001) but not in those with normal perfusion (P = .342). Of 3,566 patients with follow-up in the prognostic cohort, including 130 (5.0%) with ST depression and normal perfusion, the presence of ST depression ≥1 mm did not affect the outcomes in any summed stress score category.
Conclusions
ST depression ≥1 mm during vasodilator SPECT MPI is associated with CAD in patients with abnormal perfusion, but provides no additional risk stratification beyond concomitant perfusion imaging, including those with normal studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vasodilator single photon emission computerized tomography (SPECT) myocardial perfusion imaging (MPI) is a frequently used noninvasive strategy for evaluation of suspected or known coronary artery disease (CAD) and has a high accuracy for the detection of CAD. During MPI combined with exercise stress testing, the electrocardiographic (ECG) data alone does not provide any additional diagnostic or prognostic value.1-6 However, data regarding the significance of such ECG changes during vasodilator stress MPI are both limited and controversial.
The occurrence of ST-segment depression during vasodilator stress test is infrequent with an incidence of 3%-27%. While previous studies have demonstrated an association between vasodilator stress ST-segment depression and CAD, the diagnostic significance of ST-segment depression in the presence of normal stress MPI is uncertain.7-11 Patients with ischemic ECG changes in conjunction with a normal MPI usually do not undergo cardiac catheterization; hence, the difficulty in establishing the diagnostic value of a positive ECG response. The prognostic significance of ST-segment depression during vasodilator stress is also controversial. Two studies have suggested a worse outcome12,13 in those with ST-segment depression and normal perfusion, while two other studies demonstrated no difference in outcomes.14,15 Therefore, the purpose of this study was to evaluate the diagnostic and prognostic significance of ST-segment depression during vasodilator stress, particularly when integrated with perfusion data.
Methods
Patient Selection
From the Nuclear Cardiology Laboratory clinical database at Hartford Hospital, 5,665 consecutive patients who underwent vasodilator stress Tc-99m sestamibi ECG-gated SPECT MPI between June 1995 and April 2009 were identified. Patients with baseline ECG abnormalities including left bundle branch block (LBBB), paced rhythm, and Wolff Parkinson White pattern as well as those with a previous history of coronary artery bypass graft (CABG) surgery or myocardial infarction (MI) were excluded. This study was approved by and conducted within guidelines of the Institutional Review Board at Hartford Hospital.
Dipyridamole and Adenosine Stress MPI Protocol
Patients were instructed to fast overnight or ≥8 hours prior to stress MPI and to withhold beta-blockers, caffeine-containing food and drugs as well as oral dipyridamole for 24-48 hours prior to testing. Vital signs and 12-lead ECG were monitored before, during, and after termination of stress testing. Dipyridamole and adenosine stress was performed utilizing standard protocols, techniques, and guidelines.16 Aminophylline (50-100 mg) was administered to all patients at least one minute after the injection of the radiopharmaceutical agent.
ECG Analysis
Stress ECGs were reviewed and analyzed by two independent investigators without knowledge of SPECT and catheterization results to determine the presence and magnitude of ST-segment depression. The presence of horizontal or down-sloping ST-segment depression of 1 mm or more measured 80 ms after the J-point in 2 contiguous leads was considered an ischemic response.
Radiopharmaceutical Injection and Image Acquisition
Radiopharmaceutical dosing, image acquisition and processing were performed within guidelines of the American Society of Nuclear Cardiology.17 A one-day rest and stress imaging protocol was utilized in most of the patients (n = 2,583, 72.4%), while the remaining underwent a two-day protocol (n = 714, 20.0%). Some patients with normal perfusion and function on stress imaging did not undergo rest imaging (n = 269, 7.5%). Attenuation correction data were not used.
Gated SPECT Image Interpretation
Images were interpreted during daily clinical reading sessions by a consensus of 2 or more experienced readers using a 17-segment model and scoring system.18 In visual assessment of left ventricular (LV) perfusion, each segment was scored on a scale of 0 to 4 (0 = normal to 4 = absent photon activity). A summed stress score (SSS) and a summed rest score (SRS) were calculated by adding the segment scores at stress and rest, respectively. In classification of the presence and severity of perfusion defects, a SSS 0 to 3 was considered normal, 4-8 mildly abnormal, and >8 moderately to severely abnormal.19-21 A summed difference score (SDS) was derived for each image by subtracting the SRS from the SSS. LV cavity size at stress and rest was assessed visually and scored on a scale of 0 to 3 (0 = normal, 1 = mild, 2 = moderate, 3 = severe dilation). If LV cavity size was dilated at stress, it was further classified as fixed (score at stress equal to the score at rest) or transient ischemic dilation ([TID] score at stress greater than the score at rest22). Left ventricular ejection fraction (LVEF) was calculated using an automated quantitative method and confirmed visually.23
Coronary Angiography
Cardiac catheterization results were visual estimates by the performing interventional cardiologist and available in the clinical database. Significant CAD was defined as >70% diameter stenosis in any of the three major coronary arteries or ≥50% stenosis of the left main coronary artery.
Follow-up
Patient follow-up data was obtained through mailed questionnaires followed by a scripted telephone interview for patients that did not respond. An investigator blinded to the clinical, stress testing, and SPECT data confirmed events by reviewing hospital records, the Social Security Death Index, and death certificates. The primary endpoints of the prognostic analysis were hard events including cardiac death (CD) and non-fatal MI (NFMI). Patients who underwent early revascularization (percutaneous coronary intervention or CABG, 60 days after SPECT MPI) were excluded from the analysis. Follow-up was censored at 5 years or first event.
Statistical Analysis
Statistical analyses were performed with the SPSS software version 15.0 (SPSS Inc., Chicago, IL, USA, 2006). Clinical and baseline characteristics were expressed as mean ± standard deviation or as percentages. Inter-group comparisons were performed using a two-tailed t test for continuous variables and the χ2 or Fisher exact test for categorical variables. Annualized cardiac event rates were calculated as the number of occurrences divided by the total exposure years. Multivariate analysis was performed using binary logistic regression and Cox regression forward stepwise method for diagnostic and prognostic populations, respectively. Estimation of cumulative cardiac event-free survival was completed using the Kaplan-Meier method. Statistical significance was conferred at P < .05 for all analyses.
Results
Study Population
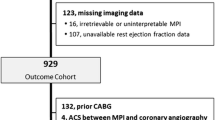
From the Hartford Hospital database, 5,665 patients who underwent the vasodilator stress SPECT MPI from 1995 to 2009 were considered for inclusion into the study. Of the 928 patients who underwent vasodilator Tc-99m sestamibi SPECT imaging and cardiac catheterization within 90 days from 1995 through 2009, 622 patients were included in the diagnostic cohort after excluding patients with baseline ECG abnormalities and previous history of MI or CABG. Of those, 555 (89%) patients underwent dipyridamole stress MPI, the remaining 67 (11%) underwent adenosine stress MPI. The prognostic cohort consisted of 3,566 patients of which 91% had available follow-up.
Clinical, Stress, and SPECT Characteristics
Demographics and baseline characteristics in patients undergoing cardiac catheterization (622 patients) are shown in Table 1. Of the diagnostic cohort, 447 (72%) had an abnormal vasodilator stress MPI while 357 (57%) had evidence of significant CAD by cardiac catheterization (Figure 1). Compared to patients without significant CAD, those with CAD were older and more likely to be male, have diabetes mellitus (DM), and hypertension (HTN). In addition, patients with significant CAD had higher SSS, TID, abnormal LVEF and were significantly (P = .001) more likely to have ST-segment depression ≥1 mm (Table 1). Furthermore, the presence of ST-segment depression was associated with a higher SDS (5.7 ± 4.7 vs 4.0 ± 4.4, P < .001) and TID (19% vs 9%, P = .001) with a trend toward a higher SSS (8.6 ± 6.7 vs 7.5 + 6.1, P = .057).
Diagnostic Implications of Vasodilator Stress ECG Changes
Of the 622 patients, 152 (24%) had ≥1 mm ST-segment depression during pharmacologic stress. As shown in Table 1, ST-segment depression ≥1 mm was associated with CAD compared to those with no ECG changes. The impact of ischemic ECG changes for identification of CAD in relation to each SSS category also was examined. As shown in Figure 1, for patients with a SSS 4-8 and SSS >8, those with ST-segment depression ≥1 mm had a higher incidence of significant CAD than those with ST-segment depression <1 mm (P = .020 and P < .001, respectively). However, there was no difference in the incidence of significant CAD when ST-segment depression ≥1 mm was present with a normal perfusion study [SSS 0-3 (P = .342)]. The incidence of CAD (30%-40%) in those with normal perfusion (SSS 0-3) is relatively high because of referral bias. Of those with normal perfusion and ST-segment depression, 7 (10.1%) had an abnormal LVEF and 2 (2.9%) had evidence of TID.
Predictors of Significant CAD
All the clinical, perfusion, and ECG variables shown in Table 1 were included in the multivariate analysis except for TID and LVEF. These variables were excluded because of incomplete data. Clinical characteristics such as age, male gender, DM, and HTN were identified as independent predictors for significant CAD (Table 2). The SSS >8 as well as ST-segment depression ≥1 mm were also identified as independent predictors of significant CAD. Furthermore, other variables such as history of PCI, hypercholesterolemia, and smoking were not predictors of CAD.
Prognostic Significance of ECG Changes
In the prognostic cohort, the mean follow-up was 2.4 ± 1.5 years for 3,566 patients. ST-segment depression occurred in 248 (7%) patients including 130 (5.0%) with normal studies. The demographics and baseline characteristics of patients with and without cardiac events are shown in Table 3. Patients with a cardiac event were older, more likely to be males, have DM and HTN when compared to patients with no cardiac events. Furthermore, those with cardiac events were more likely to have ECG changes, higher SSS, and LVEF <50%.
The annualized cardiac events (CD or NFMI) in relation to the SSS and ST-segment depression were examined. Two hundred fifty eight cardiac events (NFMI—97, CD—161) occurred in the 5 year follow-up. Twenty six events (NFMI—10, CD—16) occurred in the positive ECG group and 232 events (NFMI—87, CD—145) in those with no ECG changes. The relationship between cardiac events and ECG changes during vasodilator SPECT MPI was examined (Figure 2). The presence of ST-segment depression ≥1 mm did not affect outcomes in any SSS category. The incidence of cardiac events in patients in any SSS category was not significantly different between those with or without ST-segment depression.
The cardiac event rates in patients with and without ECG changes were examined over time. The Kaplan-Meier curves for cumulative event-free survival from CD and NFMI in the four groups are illustrated in Figure 3. The four groups were identified as follows: Group 1: (−)ECG and (−)SSS; Group 2: (+)ECG and (−)SSS; Group 3: (−)ECG and (+)SSS; Group 4: (+)ECG and (+)SSS. There was no significant difference observed in patients with and without ECG changes in SSS 0-3 [(−)SSS] (P = .216). Higher event rates were observed in those with abnormal MPI (SSS > 4) [(+)SSS] but the presence of ECG changes did not affect their outcomes (P = .452).
Kaplan-Meier curve of cardiac event-free survival in relation to ECG changes and SPECT MPI. (−)ECG(−)SSS vs (+)ECG(−)SSS, P = .216; (+)ECG(−)SSS vs (−)ECG(+)SSS, P = .007; (−)ECG(−)SSS vs (−)ECG(+)SSS, P < .001; (+)ECG(−)SSS vs (+)ECG(+)SSS, P = .004; (−)ECG(−)SSS vs (+)ECG(+)SSS, P < .001; (−)ECG(+)SSS vs (+)ECG(+)SSS, P = .452. ECG, electrocardiogram; SSS, summed stress score
Predictors of Cardiac Death and Non-Fatal MI
Variables shown in Table 3, except for LVEF and TID (because of missing data) were included in the multivariate analysis. Cox regression identified clinical characteristics of age, male gender, DM, and HTN as well as perfusion variables, SSS 4-8 and SSS >8, as independent predictors for cardiac events (Table 4). However, ST-segment depression ≥1 mm was not identified as an independent predictor of cardiac events (P = .419).
Discussion
Previous studies regarding the diagnostic and prognostic significance of vasodilator-induced ECG changes during SPECT MPI are limited and controversial, but with potentially important clinical implications. We found in 622 patients with vasodilator stress MPI and cardiac catheterization, the presence of ECG changes with abnormal SPECT studies enhanced the detection of CAD, but did not affect those with normal studies. In follow-up of over 3,500 patients, the presence of ST-segment depression did not affect outcomes regardless of whether the SPECT study was normal or abnormal. We conclude that the presence of ECG changes with vasodilator stress is of minimal diagnostic or prognostic significance.
Diagnostic Significance of ECG Changes
Previous studies examining the diagnostic significance of ECG changes during vasodilator stress MPI are limited and based on small data sets. Laarman and colleagues examined 37 patients undergoing dipyridamole Tl-201 imaging and cardiac catheterization and demonstrated the presence of significant CAD in patients with ischemic ST depression.8 However, in an analysis of 41 patients with documented angiographic CAD who also underwent dipyridamole Tl-201 imaging, Chambers and Brown did not find ECG changes to be an independent predictor of CAD.9 In a larger cohort of 339 patients, Iskandrian et al demonstrated that ST-segment depression ≥1 mm during vasodilator stress was associated with extensive CAD, including left main disease and three-vessel CAD, and was an independent predictor of extensive CAD.24 In all these studies, the presence of ST-segment depression was highly associated with an abnormal perfusion scan, hence, the association with CAD. However, data regarding the diagnostic significance of ST-segment depression in those with normal MPI is unknown. Conclusions derived from these prior studies are based on a limited number of patients with ECG changes and angiographic data.
Our study represents the largest population of patients with vasodilator-induced ECG changes and corresponding angiographic data. We found the greatest diagnostic value of ischemic ST-segment depression was with the integration of perfusion data, specifically, SSS ≥4. The likelihood of significant CAD was increased in those with abnormal MPI and ST-segment depression ≥1 mm. However, our study did not demonstrate diagnostic value in 37 patients with ischemic ECG changes and normal MPI. There have been no studies to demonstrate the diagnostic significance of ST-segment depression in the setting of normal MPI using coronary angiography. The lack of data has to do with the concept of referral bias. A majority of patients with normal MPI, despite ischemic ECG changes, are not referred for cardiac catheterization.25 Recently, Sharma et al demonstrated the presence of severe CAD by angiography requiring revascularization in patients with diabetes who had adenosine-induced ECG changes and normal imaging.15 Hence, Sharma and colleagues suggested that diabetic patients with ischemic ECG changes should be considered for angiography despite a normal MPI.15 However, based on our data, the incidence of CAD is identical between those with and without ST-segment depression in this setting of normal MPI. Therefore, pursuit of coronary angiography based solely on the presence of ST-segment depression in those with normal MPI is of limited value.
Prognostic Significance of Vasodilator Stress ECG Changes
Previous studies have evaluated the prognostic significance of ECG changes in the setting of normal MPI with conflicting results.12-15 Abbott and colleagues13 concluded that ST-segment depression during adenosine infusion appeared to be a relatively specific marker for significant CAD and were predictive of future cardiac events, regardless of perfusion results. Klodas et al12 demonstrated similar results, and concluded that the electrocardiogram appeared to identify some high-risk patients who escaped detection by SPECT MPI. However, Hage et al14 demonstrated no difference in outcomes in patients with ischemic ECG changes and normal MPI as compared to those with no ECG changes. In this study, patients with known CAD were excluded from the analysis in contrast to the previous two studies which included those with known or suspected CAD. One of the potential explanations for such results in the two earlier studies is the concept of balanced ischemia in patients with normal MPI and significant three-vessel CAD. In animal studies, vasodilators in the setting of severe coronary stenoses have been shown to create changes in the endocardial-epicardial flow ratio which could result in ischemic ECG changes in those with normal perfusion.26 Recently, Sharma and colleagues demonstrated a very low incidence of hard events (CD or MI) in patients with normal MPI and adenosine-induced ischemic ECG changes.15 Similar to the patient population in the study by Hage, Sharma et al also excluded patients with known CAD. Finally, Chow et al studied the prognostic value of dipyridamole-induced ST-segment depression in patients with normal positron emission tomography (PET) perfusion imaging.27 They concluded that ECG changes in the setting of a normal PET MPI provides no additional prognostic value.27
In our prognostic analysis, ST-segment depression in the setting of normal MPI did not affect the incidence of CD or MI. Furthermore, correlation with angiographic data in patients with and without ST-segment depression in the setting of normal MPI revealed an equal incidence of CAD in both groups, respectively. Based on our findings, the hypothesis of balanced ischemia as a reason for discordant ECG response and perfusion imaging is not supported. Finally, ischemic ECG changes provided no additional risk stratification in those with abnormal SPECT MPI despite the higher incidence of CAD in those with ST-segment depression.
Ischemic ECG changes also occur during exercise SPECT MPI including patients with normal imaging. Previous studies have evaluated the diagnostic and prognostic significance of ST-segment depression during exercise SPECT MPI.28-33 During exercise SPECT MPI, ST-segment depression was associated with the presence of CAD.28-30 However, patients with normal exercise MPI, including those with ECG changes during exercise, have a low annual risk of MI and CD.6,31-33 These results corroborate our findings with vasodilator stress MPI.
Limitations
Although the data was collected prospectively, this was a retrospective analysis of patients referred for cardiac catheterization based on clinical indications. Anti-anginal medications prior to the SPECT study were not taken into consideration which can also underestimate the extent and severity of CAD.34 Another limitation of this study that needs to be taken into context is the presence of a referral bias. All these patients in the diagnostic cohort were referred for a cardiac catheterization at the discretion of the cardiologist. The incidence of ST-segment depression during vasodilator stress was low and is a limitation in our study along with all the previous studies.
Conclusion
In patients undergoing vasodilator stress MPI, ST-segment depression ≥1 mm has diagnostic value when incorporated with abnormal MPI but not in those with normal MPI. Furthermore, ischemic ECG changes during vasodilator stress MPI offer no additional risk stratification over concomitant perfusion results, including patients with normal imaging.
References
Wackers FJ, Russo DJ, Russo D, Clements JP. Prognostic significance of normal quantitative planar thallium-201 stress scintigraphy in patients with chest pain. J Am Coll Cardiol. 1985;6:27-30.
Krishnan R, Lu J, Daw MW, Botvinick EH. Does myocardial perfusion scintigraphy demonstrate clinical usefulness in patients with markedly positive exercise tests? An assessment of the method in a high risk subset. Am Heart J. 1994;127:804-16.
Raiker K, Sinusas AJ, Wackers FJ, Zaret BL. One-year prognosis of patients with normal planar or SPECT technetium 99m-labeled sestamibi exercise imaging. J Nucl Cardiol. 1994;1:449-56.
Hachamovitch R, Berman DS, Kiat H, Cohen I, Lewin H, Amanullah A, et al. Incremental prognostic value of adenosine stress myocardial perfusion SPECT and impact on subsequent management in patients with or suspected of having myocardial ischemia. Am J Cardiol. 1997;80:426-33.
Hachamovitch R, Berman DS, Shaw LJ, Kiat H, Cohen I, Cabico JA, et al. Incremental prognostic value of myocardial perfusion SPECT for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation. 1998;97:535-43.
Gibbons RJ, Hodge DO, Berman DS, Akinboboye OO, Heo J, Hachamovitch R, et al. Long-term outcome of patients with intermediate-risk exercise electrocardiograms who do not have myocardial perfusion defects on radionuclide imaging. Circulation. 1999;100:2140-5.
Verani MS, Mahmarian JJ, Hixson JB, Boyce TM, Staudacher RA. Diagnosis of coronary artery disease with adenosine and thallium-201 scintigraphy in patients unable to exercise. Circulation. 1990;82:80-7.
Laarman G, Verzijllbergen JF, Ascoop CA. Ischemic ST changes after dipyridamole infusion. Int J Cardiol. 1987;14:384.
Chambers CE, Brown KA. Dipyridamole-induced ST segment depressing during thallium-201 imaging in patients with coronary artery disease: Angiographic and hemodynamic determinants. J Am Coll Cardiol. 1988;12:7-41.
Nguyen T, Heo J, Ogilby JD, Iskandrian AS. SPECT with thallium-201 during adenosine-induced coronary hyperemia: Correlation with coronary arteriography, exercise thallium and two-dimensional echocardiography. J Am Coll Cardiol. 1990;16:1375-83.
Iskandrian AS, Heo J, Nguyen T, Beer SG, Cave V, Ogilby JD, et al. Assessment of coronary artery disease using SPECT with thallium-201 during adenosine induced coronary hyperemia. Am J Cardiol. 1991;67:1190-4.
Klodas E, Miller TD, Christian TF, Hodge DO, Gibbons RJ. Prognostic significance of ischemic electrocardiographic changes during vasodilator stress testing in patients with normal SPECT images. J Nucl Cardiol. 2003;10:4-8.
Abbott BG, Afshar M, Berger AK, Wackers FJ. Prognostic significance of ischemic electrocardiographic changes during adenosine infusion in patients with normal myocardial perfusion imaging. J Nucl Cardiol. 2003;10:9-16.
Hage F, Dubovsky E, Jaekyeong H, Iskandrian A. Outcome of patients with adenosine-induced ST-segment depression but with normal perfusion on tomographic imaging. Am J Cardiol. 2006;98:1009-11.
Sharma J, Roncari C, Giedd KN, Fox JT, Kanei Y. Patients with adenosine-induced ST-segment depressions and normal myocardial perfusion imaging: Cardiac outcomes at 24 months. J Nucl Cardiol. 2010;17:874-80.
Henzlova MJ, Cerqueira MD, Mahmarian JJ, Yao SS. Quality Assurance Committee of the American Society of Nuclear Cardiology. Stress protocols and tracers. J Nucl Cardiol. 2006;13:e80-90.
American Society of Nuclear Cardiology. Imaging guidelines for nuclear cardiology procedures, part 2. J Nucl Cardiol. 1999;6:G47-84.
Cerqueria MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105:539-42.
Sharir T, Germano G, Kavanaugh PB, Lai S, Cohen I, Lewin HC, et al. Incremental prognostic value of post-stress left ventricular ejection fraction and volume by gated myocardial perfusion single photon emission computed tomography. Circulation. 1999;100:1035-42.
Petix NR, Sestini S, Marcucci G, Coppola A, Arena A, Nassi F, et al. Can the reversible regional wall motion abnormalities on stress gated Tc-99m sestamibi SPECT predict a future cardiac event? J Nucl Cardiol. 2005;12:20-31.
Petix NR, Sestini S, Coppola A, Marcucci G, Nassi F, Taiti A, et al. Prognostic value of combined perfusion and function by stress technetium-99m sestamibi gated SPECT myocardial perfusion imaging in patients with suspected or known coronary artery disease. Am J Cardiol. 2005;95:1351-7.
Stratmann HG, Younis LT, Wittry MD, Amato M, Miller DD. Dipyridamole technetium-99m sestamibi myocardial tomography in patients evaluated for elective vascular surgery: Prognostic value of perioperative and late cardiac events. Am Heart J. 1996;131:923-9.
Germano G, Kiat H, Kavanagh PB, Moriel M, Mazzanti M, Su HT, et al. Automatic quantification of ejection fraction from gated myocardial perfusion SPECT. J Nucl Med. 1995;36:2138-47.
Iskandrian AS, Heo J, Lemlek J, Ogilby JD, Untereker WJ, Iskandrian B, et al. Identification of high risk patients with left main and three vessel coronary artery disease by adenosine SPECT thallium imaging. Am Heart J. 1993;125:1130-5.
O’Keefe JH Jr, Bateman TM, Ligon RW, Case J, Cullom J, Barnhart C, et al. Outcome of medical versus invasive treatment strategies for non-high-risk ischemic heart disease. J Nucl Cardiol. 1998;5:28-33.
He ZX, Cwajg E, Hwang W, Hartley CJ, Funk E, Michael LH, et al. Myocardial blood flow and myocardial uptake of 201-Tl and 99m-Tc-sestamibi during coronary vasodilation induced by CGS-21680, a selective adenosine A2A receptor agonist. Circulation. 2000;102:438-44.
Chow BJW, Wong JW, Yoshinaga K, Ruddy TD, Williams K, deKemp RA, et al. Prognostic significance of dipyridamole-induced ST depression in patients with normal 82Rb PET myocardial perfusion imaging. J Nucl Med. 2005;46:1095-101.
Aksut SV, Mallavarapu C, Russell J, Heo J, Iskandrian AS. Implications of increased lung thallium uptake during exercise single photon emission computed tomography imaging. Am Heart J. 1995;l30:367-73.
Moralidis E, Spyridonidis T, Arsos G, Anagnostopoulos C. Identification of advanced coronary with exercise myocardial perfusion imaging: the clinical value of a novel approach for assessing lung thallium-201 uptake. Eur J Nucl Med Mol Imaging. 2007;34:573-83.
Chae SC, Heo J, Iskandrian AS, Wasserleben V, Cave V. Identification of extensive coronary artery disease in women by exercise single-photon emission computed tomographic (SPECT) thallium imaging. J Am Coll Cardiol. 1993;21:1305-11.
Boyne TS, Koplan BA, Parsons WJ, Smith WH, Watson DD, Beller GA. Predicting adverse outcome with exercise SPECT technetium-99m sestamibi imaging in patients with suspected or known coronary artery disease. Am J Cardiol. 1997;79:270-4.
Acampa W, Petretta M, Florimonte L, Mattera A, Cuocolo A. Prognostic value of exercise cardiac tomography performed late after percutaneous coronary intervention in symptomatic and symptom-free patients. Am J Cardiol. 2003;91:259-63.
Schalet BD, Kegel JG, Heo J, Segal BL, Iskandrian AS. Prognostic implications of normal exercise SPECT Thallium images in patients with strongly positive exercise electrocardiograms. Am J Cardiol. 1993;72:1201-3.
Sharir T, Rabinowitz B, Livschitz S, Moalem I, Baron J, Kaplinsky E, et al. Underestimation of extent and severity of coronary artery disease by dipyridamole stress thallium-201 single photon emission computed tomographic myocardial perfusion imaging in patients taking antianginal drugs. J Am Coll Cardiol. 1998;31:1540-6.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by a grant from the Department of Research Administration, Hartford Hospital, Hartford, CT, USA.
Rights and permissions
About this article
Cite this article
Azemi, T., Rai, M., Parwani, P. et al. Electrocardiographic changes during vasodilator SPECT myocardial perfusion imaging: Does it affect diagnosis or prognosis?. J. Nucl. Cardiol. 19, 84–91 (2012). https://doi.org/10.1007/s12350-011-9457-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-011-9457-x