Abstract
Introduction
This study investigated the intraocular pressure (IOP)-lowering effects and safety of tafluprost ophthalmic solution 0.0015% in actual clinical practice.
Methods
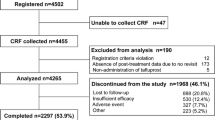
We started a mandatory prospective 2-year observational study, which collected IOP, conjunctival hyperemia score, corneal staining score, and adverse event data from glaucoma and ocular hypertension (OH) patients not previously treated with tafluprost at 2, 12, and 24 months. This report analyzes the 2-month findings.
Results
Of the 4,180 patients from 553 medical institutions in Japan, most patients had primary open-angle glaucoma (POAG, 38.1%) or normal-tension glaucoma (NTG, 44.2%). After 2 months of tafluprost administration, IOP was significantly reduced by 4.3 ± 5.2 mmHg in POAG, 2.4 ± 2.5 mmHg in NTG, 3.6 ± 5.3 mmHg in primary angle-closure glaucoma, 5.6 ± 7.1 mmHg in other types of glaucoma, and 5.3 ± 4.8 mmHg in OH. IOP was significantly reduced by 4.3 ± 4.0 mmHg in the naïve monotherapy group, 1.9 ± 3.5 mmHg in switching from prior treatment, and 3.7 ± 4.1 mmHg in the add-on therapy group. Among patients switched, the prostaglandin analog (PGA) latanoprost was the previous predominant drug (57.4%), followed by travoprost (13.8%). Significant IOP reductions were observed by 1.5 ± 3.4 mmHg in switching from latanoprost and 1.3 ± 3.7 mmHg in switching from travoprost. The conjunctival hyperemia score peaked at 1 month in the naïve monotherapy and add-on therapy groups, whereas it was significantly decreased in patients switched from another PGA. The corneal staining score showed no particular changes. Incidence of adverse drug reaction (ADR) was 7.70 % (322/4,180 patients), and all major ADRs involved the eyes or skin around the eyes.
Conclusion
Tafluprost showed significant IOP-lowering effects without any safety concerns in patients with various types of glaucoma and OH in daily clinical practice and tafluprost is highly effective in any therapeutic patterns.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glaucoma is the leading cause of acquired blindness and is characterized by visual field loss due to irreversible progressive optic nerve damage. Elevated intraocular pressure (IOP) is an important factor related to the progression of glaucoma, and the only evidence-based treatment is to delay the progression of optic nerve damage by lowering the IOP [1–4]. Although several topical ophthalmic drugs with IOP-lowering effects are now available, drugs with more potent IOP-lowering effects and better safety are always sought. Currently, prostaglandin analogs (PGAs) are the first choice of treatment because of their potent IOP-lowering effects and limited systemic adverse drug reactions (ADRs) [5].
Tafluprost (Tapros® ophthalmic solution 0.0015%, preservative, multidose, Santen Pharmaceutical Co., Ltd., Osaka, Japan) (hereinafter “tafluprost”) was developed for treatment of glaucoma and ocular hypertension (OH). Tafluprost is a PGA with two fluorine atoms at the carbon 15 position that has a high affinity for the prostanoid FP receptor [6]. A Japanese phase 3 clinical trial conducted in patients with primary open-angle glaucoma (POAG) and OH demonstrated that the IOP-lowering effect of the preservative-containing tafluprost was non-inferior to latanoprost. In addition, a phase 3 clinical trial in patients with normal-tension glaucoma (NTG) showed a significant IOP-lowering effect for tafluprost compared to placebo. Based on these results, tafluprost received marketing approval in October 2008 in Japan [7].
The target population in these previous clinical trials was limited in terms of glaucoma type, severity, concurrent diseases, and concomitant drugs. In addition, treatment was administered under stringent control. As a result, these data were insufficient with regard to generalizability in the actual clinical practice. Performing a post-marketing study using various therapeutic patterns in a wide variety of patients should make it possible to evaluate the efficacy and safety of tafluprost in routine clinical practice, thereby providing valuable information for daily clinical use. Therefore, we are currently conducting a long-term observational study with 2 years of follow-up in a large-scale population of more than 4,000 patients. After evaluating the first 2 months of data, this current report presents an analysis of the short-term results for tafluprost use in a variety of clinical settings.
Methods
Study Design
This current on-going post-marketing, multicenter, prospective, non-interventional, observational study is being conducted in accordance with the requirements of the regulatory authority in Japan, the Good Post-Marketing Study Practice (MHLW Ordinance No. 171; December 20, 2004). The study began in December 2008 and is scheduled to run through December 2014. Since the research protocol was reviewed and approved by the regulatory authority in Japan prior to beginning the study, approval by the ethics review committees at each participating medical institution is not required.
Patients and Registration
The study inclusion criteria required that patients with glaucoma and OH had not been previously treated with tafluprost. A central registration system was used to eliminate patient selection bias. When patients met the study inclusion criteria, participating physicians registered patients by facsimile within 2 weeks after prescribing tafluprost. Since the Japanese regulatory authority does not require informed consent for post-marketing observational studies, this study did not obtain informed consent from the patients.
Observation and Test Items
The observation period was defined as 2 years after starting treatment with tafluprost. The data were divided into three periods (up to 2 months, up to 12 months, and up to 24 months after starting treatment). The compiled information includes patient demographics, tafluprost treatment regimen, previous and concomitant drugs, IOP, objective findings (conjunctival hyperemia, corneal fluorescein staining), and adverse events.
Therapeutic patterns with tafluprost were classified based on previous and concomitant drug information. The groups were defined as follows: naïve monotherapy, no previous treatment or concomitant drugs; switch from prior treatment, switched to tafluprost after treatment with at least one previously used drug; add-on therapy, addition of tafluprost while continuing previous drugs; and others, which consisted of therapy other than as described above.
For data collection, a 4-point scale was used to determine the conjunctival hyperemia and corneal staining scores. The scoring grades used were: 0, none; 1, mild; 2, moderate; and 3, severe. For adverse events, the physicians evaluated a causal relationship with tafluprost. Adverse events whose causal relationship to tafluprost could not be ruled out were defined as adverse drug reactions (ADRs).
Statistical Analysis
Tabulation and analysis were performed using SAS (Version 9.2, SAS Institute, Cary, NC, USA). Data are expressed as mean ± SD. The starting point of treatment with tafluprost was used as the baseline (0 month). When comparing the IOP between 0 and 2 months, 1-month data served as 2-month data when 2-month data were missed. The level of statistical significance was 5% (two-sided). The IOP was compared by a paired t test, and the objective finding scores were compared by Wilcoxon’s signed-rank sum test, with the P value then calculated. The incidence of ADRs among the subgroups was compared using Fisher’s exact test.
Results
Patient Demographic Analysis
As of April 2013, data for 4,180 patients from 553 medical institutions have been analyzed. Table 1 summarizes the patient demographics.
In this patient group, 46.4% were males and 53.6% were females, with a mean age of 66.8 ± 12.7 years. Patient diagnoses included 38.1% with POAG (IOP >21 mmHg without treatment), 44.2 % with NTG (IOP ≤21 mmHg without treatment), 3.9% with primary angle-closure glaucoma (PACG), 7.0% with OH (IOP >21 mmHg without treatment, and absence of optic nerve damage or visual field loss), and 6.8% with other types of glaucoma, which included 2.8% with pseudo exfoliation glaucoma, 0.8% with uveitis secondary glaucoma, and 0.8% with neovascular glaucoma.
Therapeutic Patterns
The therapeutic patterns used for the patients included naïve monotherapy in more than half (52.9%), switch from prior treatment in 34.4%, and add-on therapy in 6.0% (Table 2). Among the patients switched from prior treatment (n = 1,438), 3.0% were switched from multiple drugs to tafluprost. The drugs previously used were latanoprost in 57.4%, followed by travoprost in 13.8%, isopropyl unoprostone in 9.5%, timolol in 8.6%, and carteolol in 6.1% (Table 3). For the add-on therapy patients (n = 250), 16.0% used multiple baseline drugs. The baseline drugs were timolol in 40.4%, followed by carteolol in 26.8%, brinzolamide in 15.6%, and dorzolamide in 10.4% (Table 4).
IOP-Lowering Effects
The mean IOP in all analyzed patients was 18.6 ± 5.7 mmHg at baseline and 15.0 ± 4.3 mmHg at 2 months, which showed a significant reduction of 3.6 ± 4.5 mmHg (P < 0.001). IOP was significantly reduced in all types of glaucoma by 4.3 ± 5.2 mmHg in POAG, 2.4 ± 2.5 mmHg in NTG, 3.6 ± 5.3 mmHg in PACG, 5.6 ± 7.1 mmHg in other types of glaucoma, and 5.3 ± 4.8 mmHg in OH (Fig. 1). The IOP was also significantly reduced in any types of the secondary glaucoma by 6.0 ± 7.0 mmHg in pseudo exfoliation glaucoma, 7.7 ± 8.0 mmHg in uveitis secondary glaucoma, and 3.2 ± 5.2 mmHg in neovascular glaucoma (Fig. 2).
Changes in IOP were also analyzed according to the therapeutic pattern (Figs. 3, 4). The IOP was significantly reduced in all groups by 4.3 ± 4.0 mmHg in naïve monotherapy, 1.9 ± 3.5 mmHg in switch from prior treatment, and 3.7 ± 4.1 mmHg in add-on therapy. In patients switched from prior treatment, the IOP was significantly reduced in any types of drug used in prior treatment by 1.5 ± 3.4 mmHg in latanoprost, 1.3 ± 3.7 mmHg in travoprost, 2.4 ± 3.0 mmHg in isopropyl unoprostone, 3.0 ± 2.5 mmHg in timolol, and 3.5 ± 3.3 mmHg in carteolol.
Among patients switched from another PGA, when ≥10% reduction in the IOP was defined as “improved,” and a fluctuation in the IOP within 10% was defined as “unchanged,” while an increase in the IOP ≥10% was defined as “worsened,” 44.7% of patients were “improved,” 41.4% were “unchanged,” and 13.9% were “worsened” (Fig. 5).
Objective Finding Scores
The mean conjunctival hyperemia scores in all patients analyzed were: baseline, 0.10 ± 0.34; 1 month, 0.17 ± 0.43; and 2 months, 0.14 ± 0.38. These scores were significantly higher at 1 month and later as compared to baseline. When analyzed according to the therapeutic pattern, there was a significant increase in the scores in the naïve monotherapy and add-on therapy groups at 1 month. These scores subsequently decreased or tended to decrease by 2 months. In the group of patients switched from another PGA, the baseline score was higher than that observed in the naïve monotherapy and add-on therapy groups. This score significantly decreased after these patients were switched to tafluprost (Fig. 6).
The mean corneal staining scores in all patients analyzed were: baseline, 0.08 ± 0.30; 1 month, 0.08 ± 0.28; and 2 months, 0.07 ± 0.27. When analyzed according to therapeutic pattern, there were no significant changes up to 2 months in the naïve monotherapy or add-on therapy groups. In patients switched from another PGA, the score significantly decreased after switching to tafluprost (Fig. 7).
Adverse Drug Reactions
Among all 4,180 patients, 395 cases of ADRs were found in 322 patients (7.70%) (Table 5). The major ADRs were conjunctival hyperemia, blepharal pigmentation, corneal epithelium disorder, vellus hair changes of the eyelid, iris hyperpigmentation, conjunctivitis, and eye itching. The incidence of ADRs was also analyzed whether previously treated with a PGA or not. The incidence of ADRs in patients switched from another PGA (4.36%) was significantly lower compared to that in patients not previously treated with a PGA (8.77%). Furthermore, when these patients were analyzed according to the type of ADR, the incidence of conjunctival hyperemia, blepharal pigmentation, and vellus hair changes of the eyelid was found to be significantly lower.
Discussion
The majority of patients treated with tafluprost had NTG or POAG, with both types accounting for more than 80% of the cases. The Tajimi Glaucoma Epidemiological Study conducted in Japan found that ≥70% of glaucoma patients had NTG [8, 9]. Almost half of the glaucoma patients in our study had NTG, and this study also showed that NTG is common among Japanese glaucoma patients who require treatment. Besides NTG, POAG, and OH, our study also included patients with PACG, pseudo exfoliation glaucoma, uveitis secondary glaucoma, and neovascular glaucoma, which have not been thoroughly investigated in previous clinical trials. Since tafluprost significantly reduced the IOP in each type of glaucoma, this suggests that it is effective for use in treating a wide variety of glaucoma types in actual clinical practice.
Tafluprost also significantly reduced IOP for each therapeutic pattern. In particular, the largest IOP reduction was 4.3 mmHg (from a baseline of 18.7 mmHg) in the naïve monotherapy group. In a phase 3 clinical trial, a reduction of 4.0 mmHg from a baseline IOP value of 17.7 mmHg was reported for the naïve monotherapy NTG patients after 4 weeks [7]. Although the naïve monotherapy group in the present study also included glaucoma types besides NTG, the IOP-lowering effect with naïve monotherapy in daily clinical use was confirmed to be equivalent to that reported in clinical trials.
With regard to naïve monotherapy safety, although increases were initially seen for the conjunctival hyperemia score, these tended to decrease after 2 months. On the other hand, no significant changes were observed for the corneal staining score. Thus, overall there were no concerns regarding any adverse influence of tafluprost or the preservative on the ocular surface.
Furthermore, there was also a significant IOP-lowering effect when patients were switched from another PGA (mainly latanoprost and travoprost), with a mean IOP reduction of about 1.5 mmHg. Clinically, 1 mmHg of IOP reduction is considered to be significant, because the results from the Early Manifest Glaucoma Trial (ClinicalTrials.gov #NCT00000132) revealed an estimated 10% decrease in risk of progression with each millimeter of mercury of IOP reduction [1]. Analysis of the treatment response in each of the patients who was switched from another PGA showed that 44.7% had a ≥10% reduction in their IOP, whereas 13.9% had a ≥10% increase in the IOP. Previous studies have reported that some patients exhibit low responses to the various PGA treatments [10–13]. In a non-clinical study, when ocular normotensive cynomolgus monkeys who were latanoprost low-responders were switched to tafluprost, the IOP decreased by 2.4 mmHg from the 16.5 mmHg baseline value at the time of switching [14]. This finding suggests that in actual clinical practice, switching a patient from a PGA to a different PGA may be beneficial. However, when switching topical ophthalmic drugs, the safety of both the active ingredient and any additives must be considered. In our current study, we found that there were decreases in both the conjunctival hyperemia and corneal staining scores in patients switched to tafluprost from another PGA. Furthermore, after switching the patients to tafluprost, very few had any new onset or worsening of typical ADRs normally seen with PGAs, including conjunctival hyperemia, blepharal pigmentation, or vellus hair changes of the eyelid. Therefore, this demonstrates that there are no particular safety concerns when switching to tafluprost.
When using tafluprost as add-on therapy, precautions are necessary with regard to not only the active ingredient, but also for any associated additive. Although the patients in the tafluprost add-on therapy group initially exhibited an increase in their conjunctival hyperemia scores, these scores peaked at 1 month and then decreased. On the other hand, the corneal staining score was not affected by the tafluprost add-on therapy. Therefore, while precautions are necessary with respect to ADRs that may occur due to the active ingredient when using tafluprost add-on therapy, safety is not a particular concern just because of an increase in the number of topical ophthalmic drugs.
Incidence of ADR in this study was 7.70% which was lower than that in previous interventional clinical studies [7, 15, 16]. It is considered to be caused by the difference in the extent of clinical monitoring for adverse events between an interventional clinical study and a daily clinical practice.
Since this study analyzed a large-scale population of 4,180 patients, we were able to evaluate both the safety and efficacy of tafluprost under a variety of actual use conditions due to the sufficiently large sample size. However, there were several limitations in this study. Unlike with an interventional study, there was no control group, and specified testing and drug compliance cannot be controlled in an observational study. Standard deviation of IOP reduction in this study was considered to be larger than the previous interventional studies such as phase 3 clinical trial of tafluprost [7]. This is because, unlike with an interventional study, patients with a variety of background were enrolled in this study. It has been reported that tafluprost showed almost equivalent IOP reduction to latanoprost [7, 16] or travoprost [12, 17], whereas there were statistically significant IOP reductions in patients who were switched from another PGA in this study. One of the reasons is considered to be a tentative improved compliance after the start of using tafluprost in this open-label observational study. Despite these limitations, data that reflect the actual use of a treatment can be obtained in observational studies. Thus, our current findings can serve as a reference for assessing the actual use of tafluprost in clinical practice. Furthermore, even though our current study only analyzed short-term data up to 2 months, our results suggest that tafluprost is an effective drug for the treatment of glaucoma in a variety of clinical settings. Since glaucoma usually requires chronic treatment, both long-term efficacy and safety data will need to be collected and analyzed. This 2-year observational study is still ongoing. The long-term findings are forthcoming and will be presented once the data are analyzed at the end of the study period.
Conclusion
Evaluation of the short-term results obtained during the 2 months after starting tafluprost treatment demonstrates that tafluprost is highly effective when used with various therapeutic patterns for the treatment of a wide variety of glaucoma types and OH without particular concerns about the safety of this drug in actual clinical practice.
References
Heijl A, Leske MC, Bengtsson B, et al. Reduction of intraocular pressure and glaucoma progression: results from the early manifest glaucoma trial. Arch Ophthalmol. 2002;120:1268–79.
The AGIS investigators. The advanced glaucoma intervention study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130:429–40.
Collaborative Normal-Tension Glaucoma Study Group. Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Am J Ophthalmol. 1998;126:487–97.
Leske MC, Heijl A, Hussein M, et al. Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma treatment trial. Arch Ophthalmol. 2003;121:48–56.
Marquis RE, Whitson JT. Management of glaucoma: focus on pharmacological therapy. Drugs Aging. 2005;22:1–21.
Takagi Y, Nakajima T, Shimazaki A, et al. Pharmacological characteristics of AFP-168 (tafluprost), a new prostanoid FP receptor agonist, as an ocular hypotensive drug. Exp Eye Res. 2004;78:767–76.
Aihara M. Clinical appraisal of tafluprost in the reduction of elevated intraocular pressure (IOP) in open-angle glaucoma and ocular hypertension. Clin Ophthalmol. 2010;4:163–70.
Iwase A, Suzuki Y, Araie M, et al. The prevalence of primary open-angle glaucoma in Japanese: the Tajimi Study. Ophthalmology. 2004;111:1641–8.
Yamamoto T, Iwase A, Araie M, et al. The Tajimi Study report 2: prevalence of primary angle closure and secondary glaucoma in a Japanese population. Ophthalmology. 2005;112:1661–9.
Ikeda Y, Mori K, Ishibashi T, Naruse S, Nakajima N, Kinoshita S. Latanoprost nonresponders with open-angle glaucoma in the Japanese population. Jpn J Ophthalmol. 2006;50:153–7.
Camras CB, Hedman K, US Latanoprost Study Group. Rate of response to latanoprost or timolol in patients with ocular hypertension or glaucoma. J Glaucoma. 2003;12:466–9.
Mizoguchi T, Ozaki M, Unoki K, Dake Y, Eto T, Arai M. A randomized crossover study comparing tafluprost 0.005% with travoprost 0.004% in patients with normal-tension glaucoma. Clin Ophthalmol. 2012;6:1579–84.
Kawaguchi I, Higashide T, Ohkubo S, Kawaguchi C, Sugiyama K. Comparison of efficacy of four prostaglandin analogues by bilateral treatment in healthy subjects. Jpn J Ophthalmol. 2012;56:346–53.
Kurashima H, Asai Y, Aihara M, Ishida N, Nakamura M, Araie M. Ocular hypotensive effect of tafluprost in latanoprost low-responder cynomolgus monkeys. J Glaucoma. 2012;21:123–8.
Nakano T, Yoshikawa K, Kimura T, Suzumura H, Nanno M, Noro T. Efficacy and safety of tafluprost in normal-tension glaucoma with intraocular pressure of 16 mmHg or less. Jpn J Ophthalmol. 2011;55:605–13.
Uusitalo H, Pillunat LE, Ropo A. Efficacy and safety of tafluprost 0.0015% versus latanoprost 0.005% eye drops in open-angle glaucoma and ocular hypertension: 24-month results of a randomized, double-masked Phase III study. Acta Ophthalmol. 2010;88:12–9.
Schnober D, Hofmann G, Maier H, Scherzer ML, Ogundele AB, Jasek MC. Diurnal IOP-lowering efficacy and safety of travoprost 0.004% compared with tafluprost 0.0015% in patients with primary open-angle glaucoma or ocular hypertension. Clin Ophthalmol. 2010;8:1459–63.
Acknowledgments
All named authors meet the ICMJE criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published. We wish to express our gratitude to the physicians at the medical institutions who cooperated in the study. Sponsorship and article processing charges for this study were funded by Santen Pharmaceutical Co., Ltd., Osaka, Japan. English language editing and manuscript preparation for submission for this study were provided by James Eudeikis, Forte Science Communications (Tokyo, Japan) and Hiromi Okubo, Springer Japan (Tokyo, Japan). This support was funded by Santen Pharmaceutical Co. Ltd. (Osaka, Japan).
Conflict of interest
Yasuaki Kuwayama is affiliated with Fukushima Eye Clinic, and has received consulting fees from Bausch & Lomb Japan, Kowa Pharmaceutical, Pfizer Japan, Santen Pharmaceutical and Senju Pharmaceutical, and honoraria from Alcon Japan, MSD and Otsuka Pharmaceutical. Akio Nomura is an employee of Santen Pharmaceutical Co., Ltd.
Compliance with ethics guidelines
This current on-going post-marketing, multicenter, prospective, non-interventional, observational study is being conducted in accordance with the requirements of the regulatory authority in Japan, the Good Post-Marketing Study Practice (MHLW Ordinance No. 171; December 20, 2004). The study began in December 2008 and is scheduled to run through December 2014. Since the research protocol was reviewed and approved by the regulatory authority in Japan prior to beginning the study, approval by the ethics review committees at each participating medical institution is not required. The Japanese regulatory authority does not require informed consent for post-marketing observational studies; this study did not obtain informed consent from the patients.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kuwayama, Y., Nomura, A. Prospective Observational Post-Marketing Study of Tafluprost for Glaucoma and Ocular Hypertension: Short-Term Efficacy and Safety. Adv Ther 31, 461–471 (2014). https://doi.org/10.1007/s12325-014-0109-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-014-0109-9