Abstract
Open reduction and internal fixation (ORIF) with locking plates or primary arthroplasty remains a controversial issue in the management of complex proximal humerus fractures. Aim of this study was to evaluate the surgeon- and patient-based outcome of patients older than 65 years who underwent ORIF using locking plate fixation of a 3- or 4-part fracture of the proximal humerus. Twenty-seven patients older than 65 years were treated with locking plate fixation (PHILOS, Fa. Synthes, Umkirch, Germany). At an average follow-up of 44 months, the clinical and the subjective outcome were evaluated, and complications were analyzed. The mean age- and gender-related Constant score was 70% (30–100%) compared with 92% (47–108%) of the contralateral non-injured shoulder. The mean DASH score was 29 points (0–71). Five patients (18.5%) showed clinical signs of an impingement, which was related to malpositioning of the plate in 3 cases. Screw cutout was seen in 22.2% (6 patients). Avascular necrosis of the head or the tubercula was found in 8 patients (29.6%). The revision rate was 29.6%. However, the patients considered the functional status of their shoulder as “good” or “satisfactory.” The functional and patient-orientated results of the locking plate fixation of complex displaced proximal humerus fractures in the elderly are comparable to those of primary arthroplasty and minimally invasive treatment. Proper surgical technique (screw length, plate position) is mandatory for reducing the revision rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The treatment of complex displaced fractures of the proximal humerus remains controversial. These fractures are clinically challenging for trauma and orthopedic surgeons, particularly in elderly patients with osteoporotic bones. Similar to an increasing incidence of fractures of the proximal femur with age [1], the number of humeral head fractures has been rising steadily. The use of preshaped locking plates for the proximal humerus has represented technological progress and has widened the indications for reconstruction rather than primary arthroplasty. Nevertheless, high complication rates after locking plate fixation have been reported in the literature, even in younger patients. Systematic reviews have revealed a failure rate of up to 49% [2, 3] with up to 14% of the cases requiring revision [3–5]. Recent studies by Hertel et al. and Kralinger et al. have established factors that negatively influence outcomes after fractures of the proximal humerus [6, 7]. Low bone density, increasing age, disruption of the medial hinge, and displacement between the head fragment and the shaft positively correlate with the failure rate after open reduction and internal fixation (ORIF) of humeral head fractures.
However, an ORIF of complex fractures of the proximal humerus seems to result in better functional outcomes compared to primary arthroplasty, even in the elderly [4, 8].
In any case, the number of studies examining the middle- and long-term outcomes of elderly patients treated operatively with the use of locking plates is still insufficient, and there is little evidence to favor ORIF over arthroplasty in comminuted proximal humerus fractures [4, 9]. Furthermore, the subjective outcomes of the patients who sustain such fractures are not thoroughly documented.
The goal of the present study was to evaluate both the functional and radiological outcomes and patient satisfaction after locking plate fixation of 3- and 4-part proximal humerus fractures in patients aged 65 years and older. In addition, the complications associated with this group of patients were analyzed.
Patients and methods
Between January 2004 and December 2008, a total of 430 patients were treated either conservatively or operatively for fractures of the proximal humerus. Forty-eight patients older than 65 years with 3- or 4-part fractures were treated by locking plate fixation using the PHILOS plate (Fa. Synthes, Umkirch, Germany). Twenty-four patients with similar fractures have been treated with arthroplasty, intramedullary nailing systems, or conservatively. However, this group was very heterogeneous and could, therefore, not serve as a control group. Table 1 outlines the inclusion and exclusion criteria of the study.
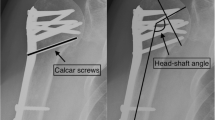
The fractures were classified according to Neer [10] on the basis of the preoperative X-rays (or CT scans when available) and compared with the intraoperative findings. The fractures with a head-shaft angle >140° were classified as valgus-impaction fractures, and those with an angle <130° were classified as varus-impaction fractures.
Surgical technique
The patients were placed in a modified beach-chair position. A deltopectoral approach was used to gain access to the glenohumeral joint. After visualization of the fracture, the tuberosity fragments were manipulated using sutures through the rotator cuff. The reduction in the head fragment was accomplished using an elevator and was temporarily fixed by K-wires. The locking plate was applied, and fixation was performed under an image intensifier to verify the anatomic reduction, plate position, and screw length. In case of massive metaphyseal defects, either a cancellous bone graft or a synthetic bone substitute (e.g., Actifuse™ABX, Fa. Apatec, distributed by Baxter Germany GmbH, Unterschleissheim, Germany) was brought into the defect to facilitate fracture healing and to support the reduction. The tuberosities were fixed to the plate using the sutures initially brought into the rotator cuff to maintain the stability of the reconstruction (Fig. 1). All of the patients were postoperatively immobilized in a sling, and physiotherapy was begun within the first week after the surgery.
Follow-up
At an average of 44 months (range: 18–75 months), the patients underwent a detailed follow-up examination. The age- and gender-related Constant–Murley score (CMS) [11, 12] was used to evaluate the functional outcome of the affected shoulder in comparison with the uninjured contralateral joint. The functional results were assessed depending on the initial fracture pattern (3- vs. 4-part fracture and varus vs. valgus impaction). The DASH score [13] was used to evaluate any limitations in the activities of daily living. In addition, the subjective outcomes were assessed using a 10-item questionnaire that was developed to facilitate better outcome assessment in this specific group of patients.
Complications and revisions were recorded and analyzed separately according to the implant-related and general complications.
Written consent to use their data for the present study was obtained from all of the patients before the follow-up examination.
Statistical analysis
We used SPSS 17.0 for Windows (SPSS Inc., Chicago, IL, USA) for the data analysis. The Mann–Whitney U test was used to examine the differences in the outcomes by the initial fractures pattern (3- vs. 4-part fracture and varus vs. valgus impaction). The level of significance was set at 0.05.
Results
Of the 48 patients, only 27 (56%) were available for follow-up. Nine patients had died in the intervening period, and 4 suffered from severe comorbidities that made an examination impossible. Five patients were unavailable, and 3 patients refused to take part in the study.
The mean age of the remaining 27 patients at the time of their trauma was 71 years (range: 65–85 years). Seven patients were men, and 20 patients were women. The right shoulder was affected in 17 cases, and 10 patients sustained a fracture of the left proximal humerus. In 23 patients, the injury was caused by a fall on the shoulder in question. According to the Neer classification, we found nine 3-part and eighteen 4-part fractures (from the intraoperative findings). Five patients showed a posteromedial (varus) impaction on the initial X-rays, and 14 patients had valgus-impaction fractures. The other patients had no significant deviations with respect to varus or valgus impaction.
The interval between the trauma and surgery was 3.5 days (range: 0–21 days). Seven patients had additional cancellous bone grafts or allografts for reconstructing metaphyseal defects that occurred in valgus-impaction fractures.
Functional results
The overall CMS of the affected shoulder was 56 points (range: 24–77 points) compared to 74 points (range, 45–89 points) on the uninjured side. Accordingly, the age- and gender-related CMSs were 70 and 92%, respectively. The range of motion was limited to 111° of forward flexion and 103° of abduction on the fracture side (155° and 145°, respectively, on the unaffected shoulder). Table 2 shows the detailed CMS results. The range of motion and strength was considerably restricted, while the pain and daily activity results were more comparable to those of the unaffected arm.
The patients who sustained 4-part fractures had higher CMSs than those with 3-part fractures (75 vs. 60%), although this difference was not statistically significant (p = 0.105). The patients with varus-impaction fractures had slightly better functional outcomes than those patients with valgus-impaction fractures (71 vs. 65%), although this difference, again, was not significant (p = 0.517).
The mean DASH score was 29.17 points (range: 0–71.4 points). There were no significant differences between the patients with 3- or 4-part fractures or between those with valgus- or varus-impaction fractures.
The patient-based outcomes were superior compared to the objectively evaluated outcome of the CMS. Approximately 50% of the patients stated that there was no significant decrease in their postoperative quality of life compared to their preoperative condition. Furthermore, over 50% rated their activity levels as comparable to those of other people of their age. Table 3 shows the results of the questionnaire that evaluated the patient-based outcomes.
Complications and revisions
Complications were observed in 16 patients (59%). In 9 cases, the complications appeared not to be implant related (hematoma, superficial wound infection, avascular necrosis, and pseudoarthrosis). Specific complications were found in 12 patients (44%). These complications are illustrated in Table 4. Note that both nonspecific and specific complications may have occurred in the same patient. The revision rate was 29.6% (Table 5).
Discussion
Despite an increasing incidence of proximal humerus fractures among an aging population, there is still no consensus concerning the treatment of these fractures in elderly patients. Conservative treatment of these displaced fractures is associated with poorer results, but is still widely performed [14, 15]. However, to date, no surgical treatment option has been proven to be superior.
Functional results
Our patients achieved age- and gender-related CMSs of 70% for the affected shoulder and 92% for the contralateral side. These results are comparable to those reported in the literature. In a systematic review consisting of 12 studies with a total of 514 patients, Sproul et al. [3] found a mean CMS of 74 points and a mean DASH score of 27 points. These findings have been confirmed by other reviews [5]. Regarding the patients’ ages at trauma, Kettler et al. [16] did not find any significant differences in outcomes between those patients older than 65 years and those younger than 65 years who sustained a displaced proximal humerus fracture.
The influence of the initial fracture pattern does not seem to be well defined. While Solberg et al. [9] have found better results in patients with valgus-impaction fractures treated operatively with locking plate fixation (a CMS of 71 points in the valgus group vs. 63 points in the varus group), and Foruria et al. [17] have observed the opposite results with better functional outcomes in the patients with varus-impaction fractures that were treated conservatively. Furthermore, the complication rate was higher in the valgus-impaction group. In our opinion, the inferior results of our patients with initial valgus displacement were due to large metaphyseal defects in these fractures, which complicated the anatomic reduction and fixation of the fracture. The typical mechanism that causes these fracture patterns seems to explain the occurrence of these defects. A fall on the outstretched arm leads to impaction of the head fragment into the glenoid. A metaphyseal void remains after the reduction, making retention of the anatomic reduction difficult. Furthermore, impaction leads to the fracture of the tuberosities, according to the eggshell model described by Hertel [18]. In addition, dislocation of the head fragment may lead to a disruption of the medial hinge, which compromises the blood supply and makes reduction even more difficult. Therefore, the medial hinge has been described as a “key structure” in proximal humerus fractures [7, 19].
Hertel et al. [7] have shown that a fracture of the anatomic neck, a short metaphyseal head extension (<8 mm), and a ruptured medial hinge result in a positive predictive value for a head ischemia of 97%.
A comparison with the other treatment options available for fractures of the proximal humerus indicates that there is no “gold standard.” In a systematic review, Misra et al. [15] found that patients treated conservatively for a displaced 3- or 4-part fracture had more pain than did patients treated operatively. They did not observe any differences in the functional results between ORIF and primary arthroplasty. Furthermore, reverse arthroplasty, which is increasingly used (particularly in the elderly), fails to yield significant advantages. Cazeneuve and Cristofari [20] followed 36 patients for 6.6 years and found a CMS of 56 points. Radiographic evidence for loosening of the glenoid component was seen in 63% of the cases. Bufquin et al. [21] have found an age- and gender-related CMS of 66% in patients who had reverse arthroplasty for a 3- or 4-part humeral head fracture. According to these results and our own experience, reverse arthroplasty remains an option for elderly patients with complex fractures and degenerative lesions of the rotator cuff. The application of reverse arthroplasty in younger patients (<70 years) is still restricted. However, the newer generation of reverse prostheses may improve the results.
Minimally invasive treatment seems to be a reliable option that is associated with satisfying results. Bogner et al. [22] have reported on a series of 50 patients over 70 years of age who were treated by percutaneous reduction and internal fixation using the Humerusblock device. The mean CMS of the patients with 3-part fractures was 61.2 points (range: 35–87 points), which was 84.9% of the score for the uninjured arm. The patients with a 4-part fracture achieved a CMS of 49.5 points (range: 18–87 points) or 68.5% of the score for the uninjured arm. However, the required surgical technique is demanding.
Complications
ORIF of proximal humerus fractures using locking plates is associated with considerable complication rates, even in younger patients. In a multicenter analysis that included 157 patients aged between 14 and 97 who had ORIF using the PHILOS plate, Brunner et al. [2] found implant-related complications (e.g., screw perforation) in 9% and non-implant-related complications (e.g., avascular necrosis) in 35% of the cases after a 1-year follow-up. Likewise, Young et al. [23] have observed a complication rate of 35.9% within 2 years.
Screw perforation into the glenohumeral joint is a frequently seen specific complication. In a systematic review that included 12 studies, Sproul et al. [3] found screw perforations in 8% of the cases. In elderly patients, screw fixation is compromised by osteopenia of the head and the metaphyseal bone. Krappinger et al. [6] have found that low bone mineral density has a significant influence on the failure rate after ORIF of humeral head fractures. In our patients, we found a perforation of 1 or more screws in 22% (n = 6) of the cases. Screw perforation was associated with a loss of the reduction, which occurred in 44% of the cases. In 2 cases, the screw perforation was already seen on the postoperative X-rays. Such technical errors may be preventable if careful dynamic fluoroscopy is performed intraoperatively to ensure that the screws do not perforate the medial cortex. Our findings regarding loss of the reduction and screw perforation are consistent with those of Dietrich et al. [4] who found loss of the reduction in 46% and a screw perforation in 24% of the cases that they examined.
Loss of the reduction occurs because of comminution of the medial cortical support. Therefore, some authors have recommended accepting a slight varus impaction to allow contact of the head and shaft fragments, which results in inferomedial support [5]. Furthermore, Zhang et al. [24] have found that the use of medial support screws placed in the inferomedial region of the head may improve mechanical stability and reduce the risk of secondary loss of the reduction. In addition, Osterhoff et al. [25] have investigated using an intramedullary fibula bone graft for medial support in a biomechanical fracture model and have found higher stiffness of the bone–implant construct and lower fragment migration. However, further clinical studies are needed to verify the benefits of those techniques.
Impingement (classified as primary or secondary) was another frequently observed (18.5%) complication. Primary impingement occurred in 3 cases and was caused by cranial malpositioning of the plate. A proper surgical technique is mandatory for avoiding this specific complication. The PHILOS plate provides an aiming device with a proximal hole, which allows controlling the correct position of the plate using a K-wire (Fig. 2). In our study, plate removal, due to impingement, was necessary in the 3 cases mentioned above. Thus, impingement was both the most frequent complication and the most frequent reason for surgical revision.
In 8 cases (29.6%), we observed a partial (n = 2) or complete (n = 6) avascular necrosis of the head and the tuberosities (Fig. 3). This rate was higher than those previously reported in the literature. Solberg et al. [9] found avascular necrosis in 17% of 24 patients older than 55 years at the time of trauma who underwent locking plate fixation for a 3- or 4-part humeral head fracture.
It is remarkable, however, that objectively evaluated complications do not necessarily result in surgical revision. The revision rate was 29.6% in our study, even though the complication rate was considerably higher (59%). Limitation of shoulder function is of secondary importance to elderly patients, as long as the activities of daily living can be accomplished and the patient is free of pain. This consideration is reflected in our patient-based subjective outcomes. Approximately 70% of our patients rated the general condition of their shoulders as “very good,” “good,” or “satisfactory,” while the CMS according to Boehm found “satisfying” or “fair” results [26].
The retrospective design of our study decreased its validity. Furthermore, there was no comparison group because we pursued a strategy of reconstruction instead of primary arthroplasty over several years. We attribute the limited number of cases in our study (only 27 patients were available for follow-up) to the complex conditions concerning our collection of elderly patients. The number of these patients inevitably deceased over time, due to mortality, and numerous comorbidities, particularly neurodegenerative and cardiovascular changes, which hindered assessment of their functional statuses. Thus, the follow-up rate was only 56.2%. This result is consistent with the follow-up rates reported in similar studies. In a study by Dietrich et al. [4], approximately 30% of the patients over 70 years of age were lost to follow up 1 year after surgical treatment for proximal humerus fractures.
Nonetheless, the present study investigates a homogeneous group of patients who were older than 65 years and who sustained complex 3- or 4-part fractures of the proximal humerus. All of the patients underwent locking plate fixation with a standard surgical procedure and rehabilitation program. The follow-up period of 44 months was longer than that of most comparable studies. Less complex fractures and younger patients are frequently included to increase the number of patients, which leads to more heterogeneous groups and less specific results [27–29]. With respect to locking plate fixation, only the study by Solberg et al. [9], which was mentioned above, reported functional results for elderly patients in particular. However, the mean age at trauma in that study was “only” 67 years (±6.7).
Conclusion
Despite a high complication rate, the functional and patient-orientated results of the locking plate fixation of complex displaced proximal humerus fractures in the elderly are satisfying and comparable to those of primary arthroplasty and minimally invasive treatments. Proper surgical technique (screw length, plate position) is mandatory for reducing the revision rate. Surgeons should be aware that objectively evaluated complications do not necessarily require surgical revision if shoulder function is satisfactory and the patient has only mild discomfort. If anatomic reduction and fixation cannot be obtained even with augmentation of the metaphyseal defects and support of the medial hinge, alternative options, such as primary (reverse) arthroplasty, should be considered.
References
Frerichmann U, Raschke MJ, Stockle U, Wohrmann S, Lohmann R (2007) Proximal femoral fractures in the elderly. Data from health insurance providers on more than 23 million insured persons–part 2. Unfallchirurg 110(7):610–616. doi:10.1007/s00113-007-1258-y
Brunner F, Sommer C, Bahrs C, Heuwinkel R, Hafner C, Rillmann P, Kohut G, Ekelund A, Muller M, Audige L, Babst R (2009) Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate: a prospective multicenter analysis. J Orthop Trauma 23(3):163–172. doi:10.1097/BOT.0b013e3181920e5b
Sproul RC, Iyengar JJ, Devcic Z, Feeley BT (2010) A systematic review of locking plate fixation of proximal humerus fractures. Injury. doi:10.1016/j.injury.2010.11.058
Dietrich M, Meier C, Lattmann T, Zingg U, Gruninger P, Platz A (2008) Complex fracture of the proximal humerus in the elderly. Locking plate osteosynthesis vs hemiarthroplasty. Chirurg 79(3):231–240. doi:10.1007/s00104-007-1436-z
Thanasas C, Kontakis G, Angoules A, Limb D, Giannoudis P (2009) Treatment of proximal humerus fractures with locking plates: a systematic review. J Shoulder Elbow Surg 18(6):837–844. doi:10.1016/j.jse.2009.06.004
Krappinger D, Bizzotto N, Riedmann S, Kammerlander C, Hengg C, Kralinger FS (2011) Predicting failure after surgical fixation of proximal humerus fractures. Injury. doi:10.1016/j.injury.2011.01.017
Hertel R, Hempfing A, Stiehler M, Leunig M (2004) Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg 13(4):427–433. doi:10.1016/S1058274604000795
Bastian JD, Hertel R (2009) Osteosynthesis and hemiarthroplasty of fractures of the proximal humerus: outcomes in a consecutive case series. J Shoulder Elbow Surg 18(2):216–219. doi:10.1016/j.jse.2008.09.015
Solberg BD, Moon CN, Franco DP, Paiement GD (2009) Locked plating of 3- and 4-part proximal humerus fractures in older patients: the effect of initial fracture pattern on outcome. J Orthop Trauma 23(2):113–119. doi:10.1097/BOT.0b013e31819344bf
Neer CS 2nd (1970) Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am 52(6):1077–1089
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Thomas M, Dieball O, Busse M (2003) Normal values of the shoulder strength in dependency on age and gender–comparison with the constant, UCLA, ASES scores and SF36 health survey. Z Orthop Ihre Grenzgeb 141(2):160–170. doi:10.1055/s-2003-38662
Offenbacher M, Ewert T, Sangha O, Stucki G (2003) Validation of a German version of the ‘disabilities of arm, shoulder and hand’ questionnaire (DASH-G). Z Rheumatol 62(2):168–177. doi:10.1007/s00393-003-0461-7
Lill H, Josten C (2001) Conservative or operative treatment of humeral head fractures in the elderly? Chirurg 72(11):1224–1234
Misra A, Kapur R, Maffulli N (2001) Complex proximal humeral fractures in adults–a systematic review of management. Injury 32(5):363–372. doi:S0020-1383(00)00242-4
Kettler M, Biberthaler P, Braunstein V, Zeiler C, Kroetz M, Mutschler W (2006) Treatment of proximal humeral fractures with the PHILOS angular stable plate. Presentation of 225 cases of dislocated fractures. Unfallchirurg 109(12):1032–1040. doi:10.1007/s00113-006-1165-7
Foruria AM, de Gracia MM, Larson DR, Munuera L, Sanchez-Sotelo J (2011) The pattern of the fracture and displacement of the fragments predict the outcome in proximal humeral fractures. J Bone Joint Surg Br 93(3):378–386. doi:10.1302/0301-620X.93B3.25083
Hertel R (2005) Fractures of the proximal humerus in osteoporotic bone. Osteoporos Int 16(suppl 2):S65–S72. doi:10.1007/s00198-004-1714-2
Kralinger F, Unger S, Wambacher M, Smekal V, Schmoelz W (2009) The medial periosteal hinge, a key structure in fractures of the proximal humerus: a biomechanical cadaver study of its mechanical properties. J Bone Joint Surg Br 91(7):973–976. doi:10.1302/0301-620X.91B7.21857
Cazeneuve JF, Cristofari DJ (2010) The reverse shoulder prosthesis in the treatment of fractures of the proximal humerus in the elderly. J Bone Joint Surg Br 92(4):535–539. doi:10.1302/0301-620X.92B4.22450
Bufquin T, Hersan A, Hubert L, Massin P (2007) Reverse shoulder arthroplasty for the treatment of three- and four-part fractures of the proximal humerus in the elderly: a prospective review of 43 cases with a short-term follow-up. J Bone Joint Surg Br 89(4):516–520. doi:10.1302/0301-620X.89B4.18435
Bogner R, Hubner C, Matis N, Auffarth A, Lederer S, Resch H (2008) Minimally-invasive treatment of three- and four-part fractures of the proximal humerus in elderly patients. J Bone Joint Surg Br 90(12):1602–1607. doi:10.1302/0301-620X.90B12.20269
Young SW, Segal BS, Turner PC, Poon PC (2010) Comparison of functional outcomes of reverse shoulder arthroplasty versus hemiarthroplasty in the primary treatment of acute proximal humerus fracture. ANZ J Surg 80(11):789–793. doi:10.1111/j.1445-2197.2010.05342.x
Zhang L, Zheng J, Wang W, Lin G, Huang Y, Edem Prince GA, Yang G (2011) The clinical benefit of medial support screws in locking plating of proximal humerus fractures: a prospective randomized study. Int Orthop. doi:10.1007/s00264-011-1227-5
Osterhoff G, Baumgartner D, Favre P, Wanner GA, Gerber H, Simmen HP, Werner CM (2011) Medial support by fibula bone graft in angular stable plate fixation of proximal humeral fractures: an in vitro study with synthetic bone. J Shoulder Elbow Surg 20(5):740–746. doi:10.1016/j.jse.2010.10.040
Boehm D (2002) Scores. In: Gohlke F, Hedtmann A (eds) Schulter: Das Standardwerk für Klinik und Praxis. Thieme, Stuttgart-New York, pp 98–104
Bjorkenheim JM, Pajarinen J, Savolainen V (2004) Internal fixation of proximal humeral fractures with a locking compression plate: a retrospective evaluation of 72 patients followed for a minimum of 1 year. Acta Orthop Scand 75(6):741–745
Handschin AE, Cardell M, Contaldo C, Trentz O, Wanner GA (2008) Functional results of angular-stable plate fixation in displaced proximal humeral fractures. Injury 39(3):306–313. doi:10.1016/j.injury.2007.10.011
Parmaksizoglu AS, Sokucu S, Ozkaya U, Kabukcuoglu Y, Gul M (2010) Locking plate fixation of three- and four-part proximal humeral fractures. Acta Orthop Traumatol Turc 44(2):97–104. doi:10.3944/AOTT.2010.2275
Conflict of interest
No fund was received in support of this study. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schliemann, B., Siemoneit, J., Theisen, C. et al. Complex fractures of the proximal humerus in the elderly—outcome and complications after locking plate fixation. Musculoskelet Surg 96 (Suppl 1), 3–11 (2012). https://doi.org/10.1007/s12306-012-0181-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-012-0181-8