Abstract
Objective
The primary aim was to evaluate the number of complications following locking plate fixation of proximal humeral fractures in country X and in country Y. The secondary aim was to identify risk factors for complications.
Methods
Multicentre retrospective case series of 282 consecutive patients with proximal humeral fractures, treated with a locking plate between 2010 and 2014. Setting: two level 1 trauma centres in country X and one in country Y. Data pertaining to demographics, postoperative complications and re-operations were collected. Fractures were classified according to the AO and Hertel classifications and experienced surgeons assessed the quality of reduction and plate fixation on the postoperative X-rays. Outcomes of the two different countries were compared and logistic regression analysis was performed to analyse the relationship between risk factors and complications.
Results
During a median follow-up of 370 days, 196 complications were encountered in 127 patients (45%). The most frequent complications were: screw perforation in the glenohumeral joint (23%), persistent shoulder complaints (16%), avascular necrosis of the humeral head (10%) and secondary fracture displacement (5%). In 80 patients (28%), 132 re-operations were performed. The patients operated in country X had significantly more complications compared with the patients operated in country Y. For implant-related complications, advanced age, non-anatomic reduction of the greater tuberosity, and country of operation were risk factors.
Conclusion
The use of locking plates for proximal humeral fractures was associated with a high number of complications in both countries; the patients operated in country Y, however, had better results compared with the patients operated in country X.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Proximal humeral fractures (PHF) account for approximately 5% of all fractures. In patients older than 65 years of age, it is the third most frequent fracture following femoral neck and wrist fractures [1, 2]. Due to an ageing population with concomitant osteoporosis, the prevalence of PHF is increasing [3, 4]. About 80% of PHF’s are minimally displaced and can be treated non-operatively with excellent results [5,6,7,8]. The residual 20% consists of comminuted and displaced fractures for which surgical treatment may be an option [9].
However, there is no consensus for the optimal surgical technique [10]. One of the available implants that have gained popularity over the last years are angular stable locking plates [11]. The locking properties of these plates provide a stable fracture fixation from a biomechanical point of view and superior screw anchorage in osteoporotic bone compared to non-locking plates. Theoretically, these locking plates should facilitate early mobilization and result in less implant-related complications [12, 13].
Several studies showed promising results with regard to shoulder function and union rates when using these angular stable locking plates [14,15,16,17,18,19,20,21,22,23]. Other studies, however, described complication rates ranging between 29 and 49% and re-operation rates ranging between 13 and 29% [22, 24,25,26,27,28]. To optimize clinical outcomes it is important to identify the risk factors for these complications.
The primary objective of this study was to analyse the number of complications following locking plate fixation for proximal humeral fractures in two European countries, country X and country Y. The secondary aim was to identify risk factors for complications and to compare the results in relation to the two different countries.
Materials and methods
This article was written in accordance with the STROBE-statement [29].
Patients
This study is a retrospective case series of all consecutive adult patients with proximal humeral fractures treated with a locking plate in two level 1 trauma centres in country X and one in country Y between 2010 and 2014. All imaging and medical records were extracted from electronic patient files. All patients had preoperative plain radiographs of the proximal humerus (AP view and a lateral scapula view). An additional CT scan with multiplanar reconstructions was performed if requested by the operating surgeon.
Surgical technique, rehabilitation and follow-up
Patients were operated under general anaesthesia in beach chair position. If indicated additional regional anaesthesia was administered. All patients received a single dose of cefazoline 30 min prior to surgery as antibiotic prophylaxis. Depending on the fracture pattern and the surgeon’s preference, either an (minimally invasive) anterolateral deltoid split or a deltopectoral approach was chosen. Sutures were placed through the insertion of the subscapularis, supra- and infraspinatus tendons. Following open reduction, the humeral head and the tuberosities were temporarily reduced to the shaft with K-wires. A locking proximal humeral plate (PHILOS or LPHP, Synthes, Oberdorf, Switzerland) was positioned. The rotator cuff tendons were secured to the plate. All procedures were performed under fluoroscopic guidance.
The postoperative rehabilitation protocol consisted of early passive range of motion exercises during the first 3 weeks followed by 3 weeks of gentle functional use and active assisted exercises. After clinical and radiographic follow-up 6 weeks postoperatively, patients were allowed to start active motion exercises, supervised by a physiotherapist. According to the hospital protocol, patients were evaluated radiographically and clinically at 2 and 6 weeks, 3 and 6 months and 1 year after surgery.
Data analysis
Two experienced trauma surgeons, with a specific focus on upper extremity trauma and experience in surgical treatment of proximal humeral fractures, evaluated and classified all pre and postoperative radiographs. The fractures were classified using the AO and Hertel fracture classification systems [30, 31].
All local complications mentioned in the operative report (for example, damage to blood vessels, nerves or other structures) were included in this study as intraoperative complications. Operating time was defined as the time between the first incision and the final stitch and was registered by the surgeon or staff of the operating room.
Postoperative complications were divided in two groups: implant related and non-implant-related complications. Implant-related complications included: implant failure such as plate or screw breakage, subacromial impingement of either plate or bone fragments, or screw perforation into the glenohumeral joint. Non-implant-related complications included: secondary fracture displacement, non-union (diagnosed when the X-ray did not show union of the fracture after 1 year, defined as bridging bone on a minimum of three cortices in anteroposterior and lateral radiographic views), malunion (diagnosed when the head fragment or tuberosities were healed with an angular deformity greater than 45° in all planes or with more than 1 cm displacement of at least one of the fragments), frozen shoulder, avascular necrosis of the humeral head, nerve injuries (radial/axillary), persistent shoulder complaints 6 months postoperatively (requiring daily use of pain medication) and superficial or deep incisional surgical site infections (SSI). Superficial surgical site infection SSI was defined as an infection of the surgical site involving skin and subcutaneous tissue, occurring within 30 days after surgery. At least one microbiological culture had to be positive for bacterial growth. Deep SSI additionally involved deep soft tissues and could occur up to 1 year after surgery. Avascular necrosis was diagnosed using radiographs or additional imaging (CT or MRI scans) and nerve impairment (radial/axillary) had to be confirmed with an EMG. A frozen shoulder was diagnosed in case of a severe impairment of the range of motion with less than 45° abduction and anterior flexion. Re-operation was defined as any surgical procedure at the same surgical site performed after the index operation, including implant removal.
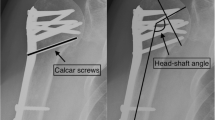
Seven criteria were defined to assess the quality of reduction and fixation: the presence of medial support (yes/no), the use of correctly placed calcar screws (yes/no), the amount of screws in the humeral head, the presence of screw perforation in the glenohumeral joint (yes/no), the plate height in respect to the greater tuberosity (correct/incorrect), anatomic reduction of the greater tuberosity (yes/no) and the neck-shaft angle after reduction (neutral/varus/valgus). A correctly placed calcar screw was defined as an oblique locking screw running through the medial curvature of the surgical neck and into the subchondral bone of the inferiomedial humeral head on the AP view, and at a central position in the humeral head on the lateral view. The plate height was considered correct if the plate was placed between 5 and 10 mm distal to the tip of the greater tuberosity. The postoperative neck-shaft angle was measured, using a digital goniometer, on the first postoperative X-ray 1 day after surgery. It was considered neutral when ranging between 125° and 140°, varus if <125° and valgus if >140°.
Statistical analysis
Data were analysed using the PASW Statistics version 20.0 (IBM Corporation, Armonk, NY). Normality of continuous data was tested with the Kolmogorov–Smirnov test and by inspecting the frequency distributions. The homogeneity of variances was tested using the Levene’s test.
Descriptive analysis was performed to compare baseline characteristics between patients with and without complications. For continuous data: mean ± SD (parametric data) or medians and percentiles (non-parametric data) were calculated. Categorical data were compared using the Chi-square test.
A logistic regression analysis was performed to determine the relation between various patients related and implant related covariates and complications. The analysed risk factors were: age, gender, comorbidities, smoking, type of trauma (high/low energy), fracture type and impaction, injury-to-surgery interval, plate type, surgical approach, operating time and the criteria for quality of reduction as described above. Furthermore, outcomes and risk factors were analysed in relation to country. A p value of <0.05 was considered the threshold of statistical significance.
Results
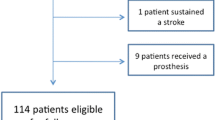
A total of 335 patients with 338 proximal humeral fractures were treated with a locking plate between 2010 and 2014. Fifty-three patients were excluded; consequently 282 patients with 285 fractures were included in the analyses. An overview of patient numbers at each follow-up stage of the study is shown in Fig. 1. The median follow-up time was 370 days (IQR 259–471).
Patient’s demographics
Patients’ demographics are presented in Table 1. AO and Hertel fracture classifications are shown in Figs. 2 and 3. The majority of fractures had a valgus impaction 175 (62%); only 12 (4%) had a neutral angle. The median time to surgery was 3 days (IQR 1–8). No intraoperative complications were reported. In the 5-year period of this study two types of implants were used: Proximal Humerus Internal Locking System (PHILOS) (97%) and Locking Proximal Humerus Plate (LPHP) (3%). Subgroup-analysis showed no significant differences in complications or re-operations between the two groups with p = 0.51 and p = 0.16, respectively. The median postoperative head-shaft angle was 135° (IQR 128–140).
Complications
One hundred and fifty-five of two hundred and eighty-two patients (55%) recovered uneventfully. The 127 remaining patients (45%) encountered 196 complications. Of these 196 complications 80 were implant-related complications in 75 different patients. Of these 196 complications 116 were non-implant-related complications in 91 patients. Forty-six patients had more than one complication. See Table 2.
One hundred and thirty-two re-operations were performed in 80 of 282 patients (28%). In total, 48 implants were removed and 12 implants were revised. Thirteen patients (5%) had a secondary arthroplasty (hemi or reversed). Data on types of re-operations can be found in Table 3. Nine patients had a deep SSI; in this group 35% of revision surgeries (n = 46) were performed. There was no difference in mean operating time between the deep SSI and superficial SSI group (p = 0.096).
Analysis of risk factors
As shown in Table 4, logistic regression analyses using four variables showed that non-anatomic reduction of the greater tuberosity is an independent risk factors for complications. No significant association between age, plate height or AO fracture type and complications was found. Logistic regression analysis using the same four variables showed that in addition to non-anatomic reduction of the greater tuberosity, advanced age is also a significant risk factor for implant-related complications specifically, see Table 5.
Results in relation to country
In total 174 of the 282 patients (61%) were operated in a hospital in country Y and 108 in two hospitals in country X (39%). Fracture types according to country can be found in Table 6. A larger portion of patients in country Y had a B1 type fracture compared to the patients in country X. Mean operating time was similar in both groups (p = 0.084). The mean time interval between injury and surgery, however, was significantly longer in country X, 5.42 vs 0.62 days (p = 0.000). Another difference between the countries was that significantly more patients were operated with a deltopectoral approach in country Y (48 vs 21%, p = 0.000). Furthermore, there was a trend towards superior reduction of the greater tuberosity in country Y (p = 0.097).
Patients who were operated in country X had significantly more complications (p = 0.015), specifically implant-related complications (p = 0.000). The re-operation rates were similar in both countries, 28% in country Y versus 30% in country X.
Logistic regression analysis using five variables showed that being operated in country X is an additional independent risk factor for implant-related complications to advanced age and non-anatomic reduction of the greater tubercle (Table 7).
Discussion
This study examined a cohort of 282 patients treated with a locking plate for proximal humeral fractures. One hundred ninety-six (45%) complications were encountered in 127 patients and 132 re-operations (28%) were performed in 80 patients.
In the literature complication rates for this procedure vary between 12 and 49% [22, 23, 25,26,27,28, 32]. The most frequent complication found in this study was screw perforation, which was high compared with previous studies. All but two of the screw perforations were secondary screw perforations, i.e., not visible on the first postoperative radiograph. An adequate technique of screw length measurement and shorter screw selection as described by Brunner et al. [33] does seem to reduce the number of primary screw protrusions. Unfortunately, it does not reduce the rate of secondary protrusions. In this study all postoperative X-rays were analysed for screw perforations. Owsley et al. performed a comparable study where radiographic signs of complications were analysed and they found a similar screw perforation rate of 23% [24]. Possibly, a part of patients who developed screw perforation on X-ray did not have accompanying shoulder complaints that required surgery and were, therefore, missed in other studies.
This study showed that the use of locking plates is associated with a high rate of re-operations. Revision surgery was performed in 28% of patients. Hardeman et al. found a similar re-operation rate of 28% in a retrospective study that included 122 PHF’s that were fixated using a locking plate [34]. Brunner et al. found a complication rate of 35% in a prospective case series of 158 patients with a proximal humeral fracture treated with a PHILOS-plate [33]. These rates are, however, much higher than the 14% found in the systematic reviews by Thanassas et al. and Sproul et al. [26, 27]. It is difficult to accurately compare these studies because of differences in inclusion criteria, age distribution, fracture types, follow-up time, and implants used.
Anatomic reduction of the greater tuberosity and a younger patient age were associated with lower complication rates. Previous studies that assessed these factors in relation to functional outcome found a similar positive effect [18, 26, 35].
Another independent risk factor that has not been evaluated so far is the difference between two modern western European countries with an advanced health care system. All patients were operated in a Level 1 Trauma Centre, in country Y; the operation was in most cases performed by a senior consultant as the first surgeon. In the hospitals in country X, surgical residents perform this procedure often as the first surgeon under supervision of a senior consultant.
With respect to differences between both countries, it has to be acknowledged that in country Y more patients with a B1 fracture were operated. There was a significant difference in the injury-to-surgery interval and surgical approach between the two countries. On average, the patients in country Y were operated within 1 day after trauma, which most likely will facilitate the reduction and fixation. A deltopectoral approach was chosen in nearly 50% of the patients in country Y, compared to 20% in country X.
We acknowledge limitations of this study, starting with the retrospective design with its known and unknown sources of bias. Moreover, there were no data on functional and patient related outcome as there were no DASH or Constant scores available for this group of patients.
In the past decade many authors have studied the outcomes of plate osteosynthesis of the proximal humerus in terms of shoulder function, complications and re-operations [14,15,16,17, 19,20,21,22, 24, 25, 28, 36]. Although results were promising in the early, smaller cohorts, it seems that authors are getting more cautious about recommending locking plate fixation for proximal humeral fractures [18, 24, 27]. In most studies, including the present, there is a group of patients that recovers fast with excellent functional results. On the other hand, there is a relatively large group of patients that encounters postoperative complications for which revision surgery is required.
There are generally two possible explanations for this high failure rate: an inadequate implant or an inadequate surgical technique. Arguments for the first explanation are, that even though the implants as well as the surgical techniques have evolved over the last years; recent case series persistently show high rates of complications and unplanned re-operations [18, 24, 27, 28, 32, 37]. The technical aspects of the implant placement might be too demanding for inexperienced surgeons. Additionally, there are high rates of late complications such as secondary screw protrusion, which cannot be prevented during the initial operation.
Recent literature, however, shows a trend towards the second explanation (inadequate surgical technique). The main argument for that statement is that the majority of local factors that lead to complications are present at the end of the initial surgery. In addition, significant positive effects of surgical factors like adequate reduction of the tuberosities on the outcome supports this point of view.
An interesting result, which has not been addressed before is the significant difference in outcome between two western European countries. Despite the limitations of our study some conclusions can still be made. It seems that, despite the possible drawbacks of the implant there is a significant difference in the number of complications between both countries. Minimally invasive plate osteosynthesis of the proximal humerus is a complex procedure with a long learning curve. The senior author from country Y was one of the co-founders of this technique and is likely to have more experience. This learning curve should be taken into account when choosing the treatment strategy, especially for complex fractures. When the surgeon is still in training, an open approach for complex fractures might lead to fewer complications compared with a minimal invasive technique. Moreover, the high number of complications makes it questionable if this operation should be a teaching procedure for residents. Results of the present study, therefore, also support that adjustments to the surgical technique and performing surgeons might lead to less postoperative complications for this procedure.
Conclusion
Complication- and re-operation rates for the locking humerus plate are high.
If locking plate osteosynthesis is applied, efforts must be made to obtain anatomic reduction of the greater tuberosity. The experience of the surgeon with minimal invasive plate osteosynthesis of the proximal humerus should be taken into account as well as the patients’ age especially when treating complex fractures. Future, adequately designed and powered trials are needed to analyse possible differences between countries and performing surgeons as the performing surgeon seems to be more important for complication rates than the implant itself.
References
Baron JA, Karagas M, Barrett J, Kniffin W, Malenka D, Mayor M, Keller RB (1996) Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology (Cambridge, Mass) 7(6):612–618
Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: a review. Injury 37(8):691–697. doi:10.1016/j.injury.2006.04.130
Kannus P, Palvanen M, Niemi S, Parkkari J, Jarvinen M, Vuori I (1996) Increasing number and incidence of osteoporotic fractures of the proximal humerus in elderly people. BMJ (clinical research ed) 313(7064):1051–1052
Kannus P, Palvanen M, Niemi S, Parkkari J, Jarvinen M, Vuori I (2000) Osteoporotic fractures of the proximal humerus in elderly Finnish persons: sharp increase in 1970–1998 and alarming projections for the new millennium. Acta Orthop Scand 71(5):465–470. doi:10.1080/000164700317381144
Neer CS 2nd (1970) Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Jt Surg Am 52(6):1077–1089
Zyto K (1998) Non-operative treatment of comminuted fractures of the proximal humerus in elderly patients. Injury 29(5):349–352
Gaebler C, McQueen MM, Court-Brown CM (2003) Minimally displaced proximal humeral fractures: epidemiology and outcome in 507 cases. Acta Orthop Scand 74(5):580–585. doi:10.1080/00016470310017992
Hanson B, Neidenbach P, de Boer P, Stengel D (2009) Functional outcomes after nonoperative management of fractures of the proximal humerus. J Shoulder Elbow Surg 18(4):612–621. doi:10.1016/j.jse.2009.03.024
Roux A, Decroocq L, El Batti S, Bonnevialle N, Moineau G, Trojani C, Boileau P, de Peretti F (2012) Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol Surg Res 98(6):715–719. doi:10.1016/j.otsr.2012.05.013
Handoll HH, Ollivere BJ, Rollins KE (2012) Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev 12:000434. doi:10.1002/14651858.CD000434.pub3
Ring D (2007) Current concepts in plate and screw fixation of osteoporotic proximal humerus fractures. Injury 38(Suppl 3):S59–S68. doi:10.1016/j.injury.2007.08.013
Chudik SC, Weinhold P, Dahners LE (2003) Fixed-angle plate fixation in simulated fractures of the proximal humerus: a biomechanical study of a new device. J Shoulder Elbow Surg 12(6):578–588. doi:10.1016/s1058274603002179
Siffri PC, Peindl RD, Coley ER, Norton J, Connor PM, Kellam JF (2006) Biomechanical analysis of blade plate versus locking plate fixation for a proximal humerus fracture: comparison using cadaveric and synthetic humeri. J Orthop Trauma 20(8):547–554. doi:10.1097/01.bot.0000244997.52751.58
Agudelo J, Schurmann M, Stahel P, Helwig P, Morgan SJ, Zechel W, Bahrs C, Parekh A, Ziran B, Williams A, Smith W (2007) Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. J Orthop Trauma 21(10):676–681. doi:10.1097/BOT.0b013e31815bb09d
Gardner MJ, Weil Y, Barker JU, Kelly BT, Helfet DL, Lorich DG (2007) The importance of medial support in locked plating of proximal humerus fractures. J Orthop Trauma 21(3):185–191. doi:10.1097/BOT.0b013e3180333094
Handschin AE, Cardell M, Contaldo C, Trentz O, Wanner GA (2008) Functional results of angular-stable plate fixation in displaced proximal humeral fractures. Injury 39(3):306–313. doi:10.1016/j.injury.2007.10.011
Aggarwal S, Bali K, Dhillon MS, Kumar V, Mootha AK (2010) Displaced proximal humeral fractures: an Indian experience with locking plates. J Orthop Surg Res 5:60. doi:10.1186/1749-799x-5-60
Clavert P, Adam P, Bevort A, Bonnomet F, Kempf JF (2010) Pitfalls and complications with locking plate for proximal humerus fracture. J Shoulder Elbow Surg 19(4):489–494. doi:10.1016/j.jse.2009.09.005
Duralde XA, Leddy LR (2010) The results of ORIF of displaced unstable proximal humeral fractures using a locking plate. J Shoulder Elbow Surg 19(4):480–488. doi:10.1016/j.jse.2009.08.008
Ricchetti ET, Warrender WJ, Abboud JA (2010) Use of locking plates in the treatment of proximal humerus fractures. J Shoulder Elbow Surg 19(2 Suppl):66–75. doi:10.1016/j.jse.2010.01.001
Roderer G, Erhardt J, Graf M, Kinzl L, Gebhard F (2010) Clinical results for minimally invasive locked plating of proximal humerus fractures. J Orthop Trauma 24(7):400–406. doi:10.1097/BOT.0b013e3181ccafb3
Faraj D, Kooistra BW, Vd Stappen WA, Werre AJ (2011) Results of 131 consecutive operated patients with a displaced proximal humerus fracture: an analysis with more than two years follow-up. Eur J Orthop Surg Traumatol 21(1):7–12. doi:10.1007/s00590-010-0655-z
Sun JC, Li YL, Ning GZ, Wu Q, Feng SQ (2013) Treatment of three- and four-part proximal humeral fractures with locking proximal humerus plate. Eur J Orthop Surg Traumatol 23(6):699–704. doi:10.1007/s00590-012-1040-x
Owsley KC, Gorczyca JT (2008) Fracture displacement and screw cutout after open reduction and locked plate fixation of proximal humeral fractures (corrected). J Bone Jt Surg Am 90(2):233–240. doi:10.2106/JBJS.F.01351
Sudkamp N, Bayer J, Hepp P, Voigt C, Oestern H, Kaab M, Luo C, Plecko M, Wendt K, Kostler W, Konrad G (2009) Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. J Bone Jt Surg Am 91(6):1320–1328. doi:10.2106/JBJS.H.00006
Thanasas C, Kontakis G, Angoules A, Limb D, Giannoudis P (2009) Treatment of proximal humerus fractures with locking plates: a systematic review. J Shoulder Elbow Surg 18(6):837–844. doi:10.1016/j.jse.2009.06.004
Sproul RC, Iyengar JJ, Devcic Z, Feeley BT (2011) A systematic review of locking plate fixation of proximal humerus fractures. Injury 42(4):408–413. doi:10.1016/j.injury.2010.11.058
Spross C, Platz A, Rufibach K, Lattmann T, Forberger J, Dietrich M (2012) The PHILOS plate for proximal humeral fractures—risk factors for complications at one year. J Trauma Acute Care Surg 72(3):783–792. doi:10.1097/TA.0b013e31822c1b5b
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP (2008) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61(4):344–349. doi:10.1016/j.jclinepi.2007.11.008
Hertel R, Hempfing A, Stiehler M, Leunig M (2004) Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg 13(4):427–433. doi:10.1016/s1058274604000795
Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audige L (2007) Fracture and dislocation classification compendium—2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma 21(10 Suppl):S1–133
Hirschmann MT, Quarz V, Audige L, Ludin D, Messmer P, Regazzoni P, Gross T (2007) Internal fixation of unstable proximal humerus fractures with an anatomically preshaped interlocking plate: a clinical and radiologic evaluation. J Trauma 63(6):1314–1323. doi:10.1097/01.ta.0000240457.64628.38
Brunner F, Sommer C, Bahrs C, Heuwinkel R, Hafner C, Rillmann P, Kohut G, Ekelund A, Muller M, Audige L, Babst R (2009) Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate: a prospective multicenter analysis. J Orthop Trauma 23(3):163–172. doi:10.1097/BOT.0b013e3181920e5b
Hardeman F, Bollars P, Donnelly M, Bellemans J, Nijs S (2012) Predictive factors for functional outcome and failure in angular stable osteosynthesis of the proximal humerus. Injury 43(2):153–158. doi:10.1016/j.injury.2011.04.003
Kettler M, Biberthaler P, Braunstein V, Zeiler C, Kroetz M, Mutschler W (2006) Treatment of proximal humeral fractures with the PHILOS angular stable plate. Presentation of 225 cases of dislocated fractures. Unfallchirurg 109(12):1032–1040. doi:10.1007/s00113-006-1165-7
Yang H, Li Z, Zhou F, Wang D, Zhong B (2011) A prospective clinical study of proximal humerus fractures treated with a locking proximal humerus plate. J Orthop Trauma 25(1):11–17. doi:10.1097/BOT.0b013e3181d2d04c
Bahrs C, Kuhle L, Blumenstock G, Stockle U, Rolauffs B, Freude T (2015) Which parameters affect medium- to long-term results after angular stable plate fixation for proximal humeral fractures? J Shoulder Elbow Surg 24(5):727–732. doi:10.1016/j.jse.2014.08.009
Acknowledgements
We like to thank Dr.med. Matthias von Allmen for his contribution to this manuscript. With his essential statistical knowledge and his critical analysis that he contributed to the quality of the presented results.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
We herewith declare that for all authors the following apply concerning the compliance to ethical standards.
Conflict of interest
FJP Beeres, NDL Hallensleben, SJ Rhemrev, JC Goslings, F Oehme, SAG Meylaerts, R Babst and NWL Schep declare that they have no conflict of interest.
Funding
There was no funding source.
Ethical approval
For this retrospective cohort study no ethical approval was needed from any of the Local Ethical Commissions in either the Netherlands or Switzerland.
Informed consent
No informed consent was obtained nor needed for this blinded retrospective cohort study.
Additional information
F. J. P. Beeres and N. D. L. Hallensleben shared first authorship.
Rights and permissions
About this article
Cite this article
Beeres, F.J.P., Hallensleben, N.D.L., Rhemrev, S.J. et al. Plate fixation of the proximal humerus: an international multicentre comparative study of postoperative complications. Arch Orthop Trauma Surg 137, 1685–1692 (2017). https://doi.org/10.1007/s00402-017-2790-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2790-z