Abstract
Thawed fresh frozen plasma (FFP) if not used within 6 h, may have to be discarded due to the risk of contamination and uncertainty about its quality. The main objective of this study was to evaluate the levels of coagulation Factor II (FII), Factor VIII (FVIII), fibrinogen and bacterial growth in thawed refrozen FFP. Thirty FFP samples were collected from healthy donors. FFP were thawed in water bath at 37 °C for 20–25 min. Approximately 10 mL of plasma from each FFP unit was tested for FII, FVIII, fibrinogen and sterility. The thawed FFP units were then kept at 4 °C for 6 h before being refrozen and stored at − 20 °C. Two weeks later, the refrozen FFP were thawed again and representative samples were analysed as before. There was a significant decline in the mean FVIII level, from 155.77% to 85.6% at second thaw. The mean FII level increased significantly from 74.9% to 82%, whereas the mean fibrinogen level fell from 3.34g/L to 3.28 g/L, but the decline was not statistically significant. There was no bacterial contamination in all samples at both time points. Refrozen plasma may be considered as an alternative to the storage of thawed unused FFP provided they are kept in a controlled environment to reduce wastage. These thawed refrozen FFP can be used later in bleeding cases like other FFP as the levels of FVIII are still within the standard haematology range (0.5–2 IU/mL) and above the minimal level of 30% coagulation factors required for adequate haemostasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fresh frozen plasma (FFP) refers to the liquid portion of human blood that has been frozen at appropriate temperature to preserve the activity of labile coagulation factors [1]. It can be obtained by two methods i.e. prepared from fresh whole blood or from plasma collected by apheresis machine and frozen as soon as possible within 8 h of collection and stored at ≤ − 18 °C for 1 year or ≤ − 65 °C for 7 years [2]. Fresh frozen plasma is commonly used to treat both congenital and acquired deficiency of coagulation factors. In view of the importance of FFP transfusion in cases with bleeding tendency secondary to coagulation pathway defect or disseminated intravascular coagulopathy, the quality of these FFP products has to be monitored and regularly checked. The quality control requirement set by Malaysia National Blood Centre include volume ranging from 195 ± 20 to 283 ± 50 mL depending on the donation set and method used; factor VIII level for each unit of FFP should be > 0.7 IU/mL with clear macroscopic appearance [1].
With the regular quality control checks on FFP products, the thawed FFP that are transfused as soon as possible should have served their purpose. However, there are many occasions in which the FFP are thawed but not transfused. Some of the documented reasons are patient has expired or is not fit for transfusion or developed complications following transfusion of previous unit of FFP or bleeding has been controlled before the thawed FFP can be transfused. In some cases, multiple units of FFP are thawed for plasma exchange, but the procedure is cancelled due to technical problems with the machine or the patient is unfit for the procedure [3]. According to the current practice in our hospital at Universiti Kebangsaan Malaysia Medical Centre (UKMMC), these thawed FFP products if not used within 6 h are discarded in view of the risk of contamination and the uncertainty about the quality of these products. The UKMMC Blood Bank data from 2011 to 2013 has shown that the thawed unused FFP ranged from 126 to 167 units annually and accounted for approximately 2.0–2.5% of total FFP collection [4]. Thus many units are thawed but not transfused which is most undesirable. Therefore, we studied the refrozen FFP to determine the quality of these products to assess the feasibility of using these thawed refrozen FFP. Refrozen FFP also may be useful for massive transfusion programs or in cases that do not require therapeutic levels of Factor V and FVIII:C such as in plasma exchange procedure [3]. These FFP are also useful for rare donors or unused autologous plasma [5]. The main objective of this study was to evaluate the coagulation factor activity of Factor II, Factor VIII and fibrinogen as well as the sterility of double freeze and thawed FFP.
Materials and Methods
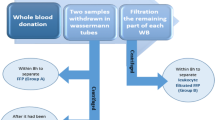
This was a quasi-experiment study on FFP done at UKMMC from May 2016 to March 2017. This research project was approved by the Research and Ethics Committee of UKM Medical Centre. Plasma was collected from healthy donors of peripheral blood stem cell during stem cell harvesting. A total of 30 allogeneic stem cells donors participated in this study who fulfilled the criteria and have consented to participate in this research. During peripheral blood stem cell collection, both the peripheral blood stem cell and 200 mL of plasma were collected using an apheresis machine (OPTIA Spectra, US). 60 mL of plasma were then transferred into Compoflex transfer bags (Fresenius Kabi, Bad Homburg, Germany) by sterile docking device (Terumo SC 201-A, Terumo Corp, Tokyo, Japan) and frozen at − 80 °C within 8 h of collection. After an overnight freeze at − 80 °C, the FFP units were subsequently transferred to − 20 °C freezer (SANYO Biomedical Freezer, Japan) until further testing in batches with 10 samples in each batch.
The FFP samples were thawed in water bath at 37 °C for 15–20 min until fully thawed. Each bag was gently mixed before the sample was drawn for testing. Approximately 10 mL of plasma sample was taken from each FFP unit under aseptic technique and labeled as first thawed samples. From this sample, 3 mL was used for coagulation parameters (Factor II, Factor VIII and fibrinogen) while 7 mL was used for sterility testing. After the first thawed samples were collected for testing, the thawed FFP units were kept into a 4 °C blood fridge for 6 h and then refrozen again at − 20 °C and stored in a − 20 °C freezer. Two weeks later, the refrozen FFP units were thawed for the second time and labeled as second thaw. Respective samples were taken and investigated as in the first thawed sample. As the main aim was to test on the refrozen and re-thawed plasma, for our convenience, 2 weeks was selected because if thawing and refreezing have any effect on the coagulation factor activity and sterility, it would be obvious within these 2 weeks’ time period.
Factor II and Factor VIII were analyzed by measuring the clotting time using STA-Deficient II and STA-Deficient VIII reagent (STA Compact, Paris). Fibrinogen level was measured quantitatively by clotting method of Clauss using STA Fib2 reagent. The coagulation parameters are interpreted in percentage for Factor II and Factor VIII and in g/L for fibrinogen.
For sterility assessment, plasma samples were cultured in BD BACTEC™ Plus Aerobic/F vials (Becton, Dickinson and Company, USA) and were incubated at 35 °C in the BD BACTEC™ FX blood culture system. The incubated vials were continuously monitored for up to 5 days. Culture vials which were not flagged as positive by the system at the end of the 5-day incubation period were regarded as negative for bacterial growth and therefore sterile; and for positive cases, a Gram staining would be done on that sample to identify the possible microorganism(s).
Data were collected and analysed. Descriptive analysis of the data was presented in numbers and percentages. Numerical variable was articulated as mean and standard deviation. Paired t test was used to compare the mean between the first and second thawed samples. A P value of less than 0.05 was considered as significant.
Results
The results of coagulation factor II, factor VIII and fibrinogen at first and second thaw are shown in Table 1. Figure 1 is the Box and Whisker Plot graph showing the comparison between FII, FVIII and fibrinogen levels in first thawed (A) and second thawed (B) FFP. Here, the lower quartile, median and upper quartile appears as a box, while the minimum and maximum data points are shown as whiskers at the two ends.
The mean values of Factor II at first and second thaw were 74.9% versus 82.03% which was increased significantly by 7.13%. For fibrinogen, there was no significant difference between first thaw and second thaw (P > 0.05). The fibrinogen level fell from 3.34 g/L at first thaw to 3.28 g/L (mean difference = 0.06).
Regarding Factor VIII, there was significant reduction in Factor VIII mean levels between first thaw and second thaw (P < 0.05). The level of Factor VIII fell from 155.77% to 85.6% (mean difference = 70.17%). However, the mean values at second thaw were still above the lower limit of National Blood Centre release criteria for FFP products i.e. .70%. The FVIII levels ranged from 98.58% to 212.96% at first thaw and 54.8% to 116.4% at second thaw. All the 30 units of FFP have Factor VIII of at least 70% at first thaw. Unfortunately, 8 out of 30 (26.6%) of these units did not fulfilled the release criteria of at least 70% of Factor VIII at second thaw. For sterility assessment, all plasma samples were negative at both time points (at first thaw and second thaw).
Discussion
FFP is commonly used to treat both congenital and acquired deficiency of coagulation factors. There are two main indications for FFP transfusion which are used as prophylaxis or therapeutic [6]. One-third of all FFP requested by physician are given as prophylaxis before surgery or invasive procedure in patient with prolonged coagulation profile [7]. In this study, we evaluated Factor II, Factor VIII and fibrinogen levels and sterility check on twice freezing and thawed FFP under controlled environment.
In our study, it was found that on the contrary Factor II levels had significantly increased from 74.9% at first thaw to 82.03% at second thaw. The main concern of this study is whether there is reduction of factors activities in these products. As the activity was not reduced, it is assumed that the quality of the FFP products was not deteriorated. The differences of the result may be due to the minor variation of two different samples prepared at two different time period as well as the variation caused by the equipment used. For fibrinogen, although the levels have reduced, there was no significant difference between first thaw and second thaw. These findings have similarities with previous studies where the authors showed that these factors remain stable and adequate for transfusion in twice-thawed-and-refrozen FFP [5, 6].
For Factor VIII, we found that there was a significant reduction in the mean levels between first thaw and second thaw. However, the mean values were still within normal limits of release criteria. Our findings were supported by one previous study which was the only data available about FVIII:C level upon repeated freezing and thawing where the authors showed that there was a statistically significant deterioration in FVIII:C level (23% dropped) after re-thawing and refrigerated storage for 2–4 h, but did not approach unsatisfactory level for haemostasis. Hence, they suggest that such plasmas would be therapeutic to patients receiving refrozen FFP. It is evidenced that most factors except Factor VIII remain stable if separation and freezing are done within 24 h of collection [8]. According to American Association of Blood Banks (AABB), once thawed, FFP must be stored at 1–6 °C for no longer than 24 h before transfusion. After 24 h, plasma can be stored for additional 4 days at 1–6 °C, but has to be labelled as Thawed Plasma [9].
In this present study, in the first thaw all the 30 units have FVIII ranged from 98.58% to 212.96% which is above the quality control requirement of at least 70% (0.70 IU/mL). While in the second thaw, FVIII level ranged from 54.8% to 116.4% where 73.4% of the units fulfilled the released criteria; which is very near to the quality control requirement of at least 75% of the units sampled should have FVIII more than 0.70 IU/mL. Moreover, if we look into the standard haematology range (0.5–2 IU/mL) [10], all these units were within the standard haematology range.
A study by Agus et al. (2012) on FFP units prepared after 24 h of storage at 4 °C revealed that 50% units contained more than 0.70 IU/mL of FVIII while 90% units contained more than 0.5 IU/mL of FVIII. They showed that although a good percentages of units contain standard levels of FVIII (0.70 IU/mL), but the percentage increases much higher considering the standard haematology range of 0.5–2 IU/mL. They viewed that the loss of coagulation factors observed is unlikely to be clinically significant and these FFP units still contained a reasonable level of FVIII (0.50 IU/mL) for treatment of disseminated intravascular coagulation and massive transfusion and would be an acceptable product for most patients requiring fresh-frozen plasma [10].
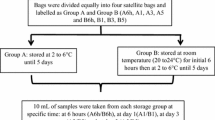
Another study at Malaysia National Blood Centre on two groups of thawed FFP where Group A was stored at 2–6 °C for 5 days and Group B was stored at 20–24 °C for initial 6 h followed by 2–6 °C for 5 days was done. They showed that all coagulation factors mean activities in both storage groups decreased over 5 days of storage but most of the activities were still above 30%. The mean FVIII activity at day 5 of storage was 36.9% and 39.8% in Group A and Group B respectively. The other coagulation factors mean activities were > 50% on day 5 of storage in both groups. They concluded that the coagulation factors activities were still sufficient to treat bleeding patients as the activities were more than 30%, as 30% is the minimal level of coagulation factors required for adequate haemostasis [11].
In our present study, 73% of the double thawed FFP units fulfilled the standard quality control requirements, and all the units were within the standard haematology range (0.5–2 IU/mL) and above the minimal level of coagulation factors required for adequate haemostasis. Thus, we expect the coagulation factor levels in the FFP units are sufficient for adequate haemostasis in bleeding cases. Therefore, the thawed plasma may be refrozen if it is kept at controlled environment at 4 °C for 6 h and to be used later in bleeding cases like other FFP. These thawed plasma are recommended to be used like other FFP units that is immediately after thawing.
One local unpublished data on thawed plasma during prolonged storage at 4 °C has shown that level for factor II at 6 h of thaw increased from 73.43% to 73.73% (increased by 0.4%), Factor VIII decreased from 177 to 144% and fibrinogen level was static compared to the level immediately after thaw. These factor levels continued to drop further to 71% and 69.8% for Factor II and 81% and 71% for Factor VIII at day 3 and day 5 when stored in a 4 °C fridge. Our result found that, when we refreeze thawed plasma at 6 h, and re-thaw 2 weeks later, the level of Factor II and Factor VIII are similar to those stored at 4 °C for 3 days.
In this present study, sterility assessment was negative for bacterial growth at both time points (at first thaw and second thaw). However, the result of this sterility testing could be biased due to the small sample size in this study. Our decision to omit the usage of anaerobic culture vials was based on the usual practice of storing thawed plasma in aerobic conditions which do not favour the growth of obligate anaerobic bacteria such as Propionibacterium sp. There was no previous study done on sterility of repeated freezing and thawing of FFP to support our findings.
The limitation of this study is the relatively small sample size of 30 and the fact that the study was conducted on plasma collected by apheresis method. Although apheresis plasma is one of the methods of collection, the methodology used for apheresis collection is different as it is collected during a stem cell harvesting procedure.
Conclusion
This study results showed that the refrozen and thawed FFP units contained a reasonable level of FVIII and other coagulation factor (Factor II and fibrinogen). We would like to propose that thawed plasma may be refrozen if it is kept in a controlled environment at 4 °C for not more than 6 h and can be used later in bleeding cases like other FFP as the levels of FVIII are still within the standard haematology range (0.5–2 IU/mL) and above the minimal level of 30% coagulation factors required for adequate haemostasis.
References
National Blood Centre (2016) Transfusion Practice Guidelines for Clinical and Laboratory Personnel, 4th edn. Ministry of Health Malaysia
Hughes VC, Wright PA (2005) Donor screening and component preparation. In: Harmening DM (ed) Modern blood banking and transfusion practices, 5th edn. FA Davis Company, New York, pp 207–241
Dzik WH, Riibner MA, Linehan SK (1989) Refreezing previously thawed fresh frozen plasma. Stability of coagulation factors V and VIII: C. Transfusion 29:600–604
Blood Bank data (2014) FFP usage record. UKM Medical Centre
Ben-Tal O, Zwang E, Eichel R, Badalbev T, Hareuveni M (2003) Vitamin K-dependent coagulation factors and fibrinogen levels in FFP remain stable upon repeated freezing and thawing. Transfusion 43(7):873–877
Philip J, Sarkar RS, Pathak A (2013) The effect of repeated freezing and thawing on levels of vitamin K-dependent coagulation factors and fibrinogen in fresh frozen plasma. Asian J Transfus Sci 7(1):11–15
Dzik W, Rao A (2004) Why do physicians request fresh frozen plasma? Transfusion 44(9):1393–1394
O’Neill EM, Rowley J, Hansson-Wicher M, McCarter S, Ragno G, Valeri CR (1999) Effect of 24-hour whole blood storage on plasma clotting factors. Transfus Med 39(5):488–491
Dumont LJ, Papari M, Aronson CA, Dumont DF (2014) Whole-blood collection and component processing. In: Fung MK, Grossman BJ, Hillyer CD, Westhoff CM (eds) Technical manual, AABB, 18th edn. Bethesda, pp 135–166
Agus N, Yilmaz N, Colak A, Liv F (2012) Levels of factor VIII and factor IX in fresh-frozen plasma produced from whole blood stored at 4 °C overnight in Turkey. Blood Transfus 10:191–193
Noordin SS, Karim FA, Wan Mohammad WMZ, Hussein AR (2018) Coagulation factor activities changes over 5 days in thawed fresh frozen plasma stored at different initial storage temperatures. Indian J Hematol Blood Transfus 34(3):510–516
Shamsudin S, Yousuf R, Tang YL, Ding CH, Leong CF (2017) Evaluation of coagulation factor activity and sterility of thawed fresh frozen plasma during storage up to 5 days at 4 °C. MJPath (paper submitted under review)
Acknowledgements
We would like to thank UKM Medical Centre for providing a research Grant (Code: FF-2016-075). We would also like to thank the staff, UKMMC for their technical help in this study.
Funding
This study was funded by UKM Medical Centre (Research Grant Code: FF-2016 075).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors of this article declared that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee (Secretariat for Medical Research and Innovation, National Medical Research Registry) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.”
Informed Consent
Informed consent was obtained from all individual participants included in the study. A Preliminary Study on Coagulation Parameters and Sterility of Thawed Refrozen Fresh Frozen Plasma.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Draman, R., Yousuf, R., Abdul Aziz, S. et al. A Preliminary Study on Coagulation Parameters and Sterility of Thawed Refrozen Fresh Frozen Plasma. Indian J Hematol Blood Transfus 36, 112–116 (2020). https://doi.org/10.1007/s12288-019-01171-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12288-019-01171-0