Abstract
Despite primary percutaneous coronary intervention (PPCI) and the availability of optimal medications, including dual antiplatelet therapy (DAPT), most patients still experience major adverse cardiovascular events (MACEs) due to frequent recurrence of thrombotic complications and myocardial infarction (MI). MI occurs secondary to a massive loss of endothelial cells (ECs), vascular smooth muscle cells (VSMCs), and cardiomyocytes (CMs). The adult cardiovascular system gradually loses the ability to spontaneously and regularly regenerate ECs, VSMCs, and CMs. However, human cells can be induced by cytokines and growth factors to regenerate human-induced pluripotent stem cells (hiPSCs), which progress to produce cardiac trilineage cells (CTCs) such as ECs, VSMCs, and CMs, replacing lost cells and inducing myocardial repair. Nevertheless, the processes and pathways involved in hiPSC-CTC generation and their potential therapeutic effects remain unknown. Herein, we provide evidence of in vitro CTC generation, the pathways involved, in vivo transplantation, and its therapeutic effect, which may provide novel targets in regenerative medicine for the treatment of cardiovascular diseases (CVDs).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myocardial infarction (MI), which causes the irreversible death of heart muscle secondary to a prolonged lack of oxygen supply, contributes to major morbidity and mortality worldwide [1]. In spite of primary percutaneous coronary intervention (PPCI) and the existence of optimal medications, such as dual antiplatelet therapy (DAPT), most patients will experience a major adverse cardiovascular event (MACE) due to the frequent recurrence of thrombotic complications [1]. MI occurs secondary to the development and rupture of atherosclerosis (As) plaque. The formation of As plaque is closely related to the massive impairment of endothelial cell (ECs) and the proliferation of vascular smooth muscle cell (VSMCs) [1]. Studies have shown that the adult cardiovascular system gradually loses the ability to spontaneously regenerate and accelerate the replacement of ECs, VSMCs, and cardiomyocytes (CMs) [2].
EC dysfunction promotes the expression of adhesion molecules, including intercellular adhesion molecules-1 (ICAM-1) and vascular adhesion molecules-1 (VCAM-1), resulting in the recruitment of monocytes/macrophages, as well as subendothelial migration, which accelerates thickening of the intima media and As formation [3, 4]. VSMCs secrete extracellular matrix (ECM), collagen (I, II), and elastin, which increases necrotic core thickness and enhances stability of the AS plaque [5, 6]. However, continuous VSMC death reduces ECM, collagen (I, II), and elastin secretion, while increasing the susceptibility of plaque rupture. In addition, macrophage-derived foam cells in the plaque continuously secrete degrading cytokines, such as matrix metalloproteinase-2,13, which degrade the necrotic core and promote plaque rupture [7, 8].
Recent studies have reported that human cells can be induced in response to cytokines, including interleukin-1β, transforming growth factor-β (TGF-β), fibroblast growth factor (FGF), etc., to regenerate human-induced pluripotent stem cells (hiPSCs), which can progress to produce cardiac trilineage cells (CTCs), including ECs, VSMCs, and CMs [9]. Transplantation of hiPSCs-CTCs provides a favorable microenvironment for pre-existing cells to proliferate and enhances cell replacement and repair, which protect against the myocardial damage after MI [9]. The processes and pathways associated with hiPSC-CTC generation and therapeutic effect, however, still remain unexplained [10]. Herein, we provide evidence for the in vitro generation of CTCs, pathways involved, in vivo transplantation, and therapeutic effect in MI. Understanding these processes may provide a novel therapeutic strategy for the treatment of MI and other forms of cardiovascular disease (CVD).
HiPSCs Stimulants and Pathways
HiPSCs-ECs
TGF-β and bone morphogenetic protein (BMP) are multifunctional polypeptide cytokines belonging to the transforming growth factor superfamily that regulate the ESC and hiPSC transformation process during cardiac repair in adults [11]. Activated TGF-β and BMP bind to TGF-βRI/II and BMPR, respectively, transducing intercellular signaling to the smad2,3 dimer complex, which binds to smad4 and forms a trimer that translocates into the nucleus to stimulate transcription factors, including snail and twist1 (Table 1) [11]. Stimulation of snail or twist maintains iPSC and ESC stemness genes, promoting sustainability of stem cell morphology [12]. During the generation of CTCs from hiPSCs, suppression of TGF-β, snail, or twist enhances the expression of EC, VSMC, and CM markers [11, 12]. For instance, administration of SB431542, a TGF-β inhibitor, suppresses ESC genes and increases EC generation, adhesion molecule expression, and cell-to-cell adhesion, leading to tube formation [12, 13].
Furthermore, ESCs treated with IL-1β and IL-8 significantly increase EC markers, adhesion molecule expression, and EC generation [14]. In addition, fibroblast growth factor (FGF) and vascular endothelial growth factor (VEGF)-A, hormones from the growth factor family, induce cell proliferation, differentiation, angiogenesis, and cardiac repair [15]. Activation of FGF-2 and VEGF-A binds to FGFR and VEGF-AR, respectively, which further stimulates Akt and PI3K-dependent phosphorylation of IκB-NFκB complex inducing cell differentiation [16]. Activation of Akt was found to increase the survival of amniotic fluid-derived mesenchymal stem cells (AFMSCs) which increased cardioprotective effective and expression of CMs markers after intramyocardial transplantation [17]. FGF2, VEGF, and BMP4 were shown to synergistically induce generation of ECs from hiPSCs and ESCs via upregulating the Akt/PI3K pathway, which elevates vasculogenesis in mice [18].
Moreover, the activation of insulin-like growth factor (IGF)I/IGFIR axis binds to αvβ3 integrin to form IGFI-IGFIR-αvβ3 complex that activated Akt/PI3K pathway and increased ECs production from hiPSCs [19]. HiPSCs treated with IGFI exhibited elevated hiPSC-EC generation and replication via activation of Akt/PI3K, which facilitated vascularization and directly improved cardiac performance after MI in swine [10, 20]. Activation of IL-1β, IL-8, and TNF-α has also been found to significantly increase EC generation from iPSCs in an Akt-dependent manner [14, 21], leading to microvascular network formation in type 1 diabetes mellitus (T1D) patients [22, 23].
Wnt-1, a highly evolutionarily conserved proto-oncogene involved in sinoatrial node (pacemaker) formation during embryonic development, stimulates nuclear translocation of β-catenin, which binds to the T cell factor/lymphoid enhancer factor (TCF/LEF) transcription factor to induce stem cell differentiation [24]. In inactivated cells, β-catenin is degraded through its phosphorylation by polyposis coli (APC), Axin, and kinase glycogen synthase kinase-3β (GSK-3β), abolishing β-catenin nuclear translocation, TCF/LEF activation, and stem cell differentiation [25]. While activated Wnt-1 has been found to bind frizzled (FZD) and low-density lipoprotein receptor-related protein-5/6 (LRP-5/6), which enhances APC, Axin, and GSK-3β recruitment to the cell membrane and promotes β-catenin stability, nuclear translocation and TCF/LEF activation lead to stem cell differentiation [24, 26]. Studies have demonstrated that Wnt-1/β-catenin stimulation in hiPSCs promotes EC markers and adhesion molecule expression, which enhance hiPSCs-ECs generation and replication [27,28,29].
HiPS-VSMCs
Activation of the TGF-β/smad2/3/4 pathway upregulates VSMC markers, including calponin and transgelin (SM22-α), and VSMC generation [30]. Furthermore, hiPSCs-ECs generated by Wnt-1/β-catenin exhibit multipotent capabilities, leading to VSMC generation [29], cardiac-specific gene expression, and CM generation in bone marrow mesenchymal cells (BM-MSCs) [31]. In addition, activated angiotensin II (Ang II), a hormone that acts as a vasoconstrictor, interacts with the Ang II type 1 (AT1) receptor to promote stem cell differentiation through two pathways [32]. First, Ang II promotes cell differentiation via the Akt/PI3K/NFκB pathway or by accelerating phosphorylation of JAK and STAT3, which triggers the expression of transcription factors, including NF-κB, and increases generation of VSMCs [32, 33]. In addition, Notch signaling also significantly upregulates VSMC generation [34, 35], which promotes arteriogenesis in adult mouse heart [36]. Moreover, triggering Notch signaling in iPSCs facilitates CM generation and improves MI outcomes in mice [37,38,39].
HiPS-CMs
Recent reports have indicated that AFMSCs treated with TGF-β increase expression of CMs markers which are proceeded to CMs generation [40]. Furthermore, activin-A, a member of the TGF-β superfamily, binds to type II activin-A receptors (ActRII-A), which in turn stimulate type IB activin-A receptor (ALK4), and triggers smad signaling to induce CM generation [41, 42]. Combined activation of activin-A, BMP4, and FGF-2 induces both EC and CM generation in hair follicle-associated pluripotent stem cells (HAPSCs) [43, 44]. Furthermore, IFN-γ activation in iPSCs-MSCs upregulates expression of cTnT and promotes CM generation [45].
Wnt-1/β-catenin activation in response to administration of CHIR99021, a GSK3β inhibitor, promoted CM generation and self-renewal by maintaining continual expression of Oct-4 and Sox2 in ESCs [46, 47]. Wnt-1/β-catenin also increased cardiac-specific gene expression and CM generation in BM-MSCs [31]. Notch signal transduction patterns that regulate embryonic endocardium compartmentalization were shown to be relevant in a hiPSC generation technique and in adult cardiac repair [48]. Furthermore, impaired Notch signaling led to neonatal congenital cardiomyopathy [49, 50]. Stimulation of Delta-1 (Dll1), a Notch activator, leads to Notch cleavage by γ-secretase to produce the notch intercellular domain (NICD), which translocates into the nucleus, binds to recombination signal binding protein for immunoglobulin kappa J region (RBPJK/CSL/Su(H)), and recruits coactivator mastermind-like (MAML) to form a protein complex [51]. The NICD-RBPJK-MAML complex directly activates target genes, including basic-helix-loop-helix (bHLH) peptides, leading to cellular transformation [50,51,52]. In addition, Notch signaling facilitates CM marker expression and CM generation in iPSCs [37,38,39], as well as promoting cardiogenesis [53] (Fig. 1).
Schematic representation of signaling pathways involved in iPSC transformation into MCs and trilineage cells: adhesion of Dll1 to Notch leads to its cleavage and dissociation from the cell membrane. γ-Secretase induces further cleavage of Notch to NICD. NICD binds to RBPJK/MAML to form the NICD-RBPJK/MAML complex, which translocate to the nucleus to instigate expression of snail, Klf4, α/β-MHC, bHLH, and Nkx2.5. In addition, TGF-β, BMP4, and activin-A adhere to TGF-βRI/TGF-βRII, BMP4, ActRII-A, respectively, leading to stimulation of smad2,3 to form a complex with smad 4. The smad2,3,4 complex translocates into the nucleus, activating snail, twist, GATA4, Sox2, α/β-MHC, etc. Additionally, Wnt binds to FZD/LPR5/6, leading to abrogation of β-catenin degradation by APC, Axin, and GSK3β, which enhances the stability and nuclear translocation of β-catenin to stimulate expression of TCF/LEF, GATA4, and Oct4. Furthermore, Ang II, FGF-2,10, IGF-I, IL-1β, IL-8, VEGF-A, and TNF-α adhere to AT-1, FGF-2,10R, IL-1βR, IL-8R, VEGF-AR, and TNF-αR, respectively, to transmit signaling to Akt, PI3K, and MAPK. The stimulation of MAPK leads to phosphorylation of IκB-NFκB, which degrades IκB and allows NFκB nucleoplasmic translocation to activate FoxO3a, GATA4, Sox2, Oct4, and Nkx2.5. Moreover, Ang II/AT-1 activation phosphorylates JAK, which further phosphorylates STAT3. P-STAT3 translocates to the nucleus to stimulate transcription factors including FoxO3a, GATA4, Sox2, Oct4, and Nkx2.5. Activation of these transcriptional factors by the abovementioned stimulants promotes iPSC transformation to generate MCs and cardiac trilineage cells
In summary, activation of the appropriate cytokines and pathways actually promotes CTC generation from iPSCs. Although the use of hiPSCs for the treatment of MI and other forms of CVD was previously a myth, transplantation of hiPSCs in animal myocardium has demonstrated a novel and promising therapeutic strategy for the amelioration of MI, suggesting that hiPSC-CTC generation and transplantation may represent a potential therapeutic strategy for the treatment of CVDs, though the exact effects remain to be clarified (Table 1).
HiPSC-CTC Transplantation and MI Repair
Endothelial Cells
ECs line the inner layer of the cardiovascular system and maintain homeostasis by preventing clotting and thrombosis. Impairment of EC function promotes the development of AS [4] and MI [54]. Recent studies have demonstrated ECs generated from stem cells improve cardiovascular function [14]. For instance, human urine-derived stem cells (hUSCs) subjected to vascular endothelial growth factor-A (VEGF-A) responded by increasing expression of EC markers, including Ve-cad and CD31, molecules that support cell-to-cell adhesion and tubule network formation [55,56,57]. One study confirmed that hiPSCs-ECs maintain barrier integrity, permeability, and homeostasis more effectively compared to primary ECs [58]. In addition, hiPSCs-ECs adequately regulate thrombosis and prevent MI [58, 59]. Previously, intramyocardial transplantation of hiPSC-ECs (1 × 106) was shown to significantly reduce MI size and improve survival rate within 14 days in adult mice [27]. Furthermore, combined intramyocardial transplantation of hiPSC-ECs, hiPSC-VSMCs, and hiPSC-CMs provided a favorable microenvironment for pre-existing CTC proliferation, which promoted MI repair within 4 weeks in swine [10]. Moreover, intramyocardial transplantation of induced expandable cardiovascular progenitor cells (ieCPCs) upregulated vessel-like structure formation and significantly reduced scar size in the heart after 2 weeks of therapy in MI mice [9]. In addition, to generation of ECs from hiPSCs, ESCs and intramuscular injection of hiPSCs-ECs elevated vasculogenesis and LVEF, while reducing MI size 10 weeks after cell transplantation in mice [18]. Transplantation of hiPSCs-ECs further increased the expression of cardiac-specific markers cTnT, Nkx2.5, etc. [10, 27], suggesting that hiPSCs-ECs may enhance the replication of CMs to facilitate rapid recovery after MI. These data suggest that EC generation and administration may represent a strategy to instigate proliferation of pre-existing VSMCs and CMs to reduce cardiac abnormalities, particularly in response to MI.
Vascular Smooth Muscle Cells
VSMCs are a component of the arterial medial layer that maintain vessel integrity by controlling diameter due to their contraction and relaxation potential in response to vasoactive stimuli [60]. Excessive proliferation and migration of VSMCs accelerate AS plaque development and stability, while ectopic loss of VSMCs enhances AS plaque rupture, thrombus release, arterial occlusion, and MI, suggesting that maintaining appropriate VSMC proliferation can stabilize or prevent AS [61, 62] and MI [63]. Similar to EC generation, VSMCs can be generated from other cells [64]. A neural crest cell line exposed to TGF-β and activin-A induced calponin, SM-γ-actin, SM myosin heavy chain (SMMHC), and VSMCs markers, proceeding to VSMC generation [64]. Interestingly, while combined treatment of BMP-2,7 and activin-A exhibited antagonistic effect by failing to promote neural crest cell differentiation to VSMCs, combined treatment of BMP4 and activin-A promoted higher levels of VSMCs [64,65,66], suggesting that BMP-2,7 and activin-A coactivation may terminate VSMC generation while BMP4 and activin-A coactivation increases VSMC production. Another study affirmed that neonatal skin fibroblasts exposed to TGF-β increased generation of VSMCs, which exhibited appropriate contraction and successfully formed tissue rings [67]. Intramyocardial transplantation of mesp1-cardiac progenitor cells (mesp1-CPCs) accelerated VSMC proliferation and neovasculogenesis, restored blood flow to infarcted areas, and reduced MI after 3 months of therapy in mice [68]. These findings indicate that hiPSCs may promote vascular repair by inducing VSMC proliferation and replacement. Therefore, administration of hiPSCs-VSMCs into the infarct area of the heart in ischemic infarct patients may represent a therapeutic strategy for the treatment of MI.
Cardiomyocytes
CMs are cardiac muscle cells responsible for generating contractile force to enhance blood distribution and control of rhythmic beating of the heart. CMs fail to replicate or regenerate in the adult human heart, leading to reduced cardiac output [69]. However, CMs can be generated from hiPSCs and transplanted into the heart to induce cardiac repair [70]. Exposure of iPSCs to FGF-10 accelerated the expression of cardiac-specific transcription factors, such as Nkx2.5, and promoted the generation of CMs [71, 72]. Exposure of epicardia cells to FGF-2 and TGF-β separately promoted CM production, while costimulation with FGF-2 and TGF-β strongly terminated CM generation [73, 74], suggesting an antagonistic effect between TGF-β and FGF-2 during cell differentiation. Furthermore, hypoxia inducible factor 1α (HIF-1α) upregulated CM generation by increasing Notch signaling in interstitial pluripotent stem cells (IPSCs) and ESCs [75]. However, HIF-2α activation increased β-catenin protein expression, cardiac protein expression, and CM generation [76], indicating that HIF-1α stimulates CM generation through Notch signaling but that HIF-2α induces CM generation via Wnt/β-catenin signaling.
Moreover, ESCs treated with IGF-I activated CM markers, including α-MHC, α-actinin, and troponin I, which were stabilized and propagated to CMs upon activation of insulin-like growth factor binding protein-4 (IGFBP4) [77, 78] and improved cardiac performance and attenuated MI upon hiPSC intramyocardial transplantation in swine [10, 20]. In addition, intramyocardial transplantation of iPSCs-MSCs (2 × 108) promoted neovascularization, cTnT expression, and pre-existing CM replication, resulting in improved LVEF within 8 weeks after therapy in MI pigs [45, 79].
Recent reports indicate that intramyocardial transplantation of hiPSCs-CMs (0.5 × 106) prevents MI and improves LVEF with 2–4 weeks of therapy in mice [70]. Additionally, transcutaneous echo-guided injection of hiPSCs-CMs (1.4 × 106) enhanced pre-existing CM proliferation and dead CM replacement, which improved LVEF in MI mice after 7 weeks of treatment (Fig. 2) [9, 10, 48, 80]. Collectively, these data prove that triggering various genes in different pluripotent stem cells upon transplantation may generate CMs that can be used for MI treatment in vivo (Table 2).
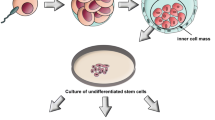
Diagrammatic illustration of MC and cardiac trilineage cell generation: exposure of iPSCs to stimulants, including TGF-β, Notch, Wnt-1, IGF-1, BMP4, etc., enhances generation of cardiac trilineage cells. When iPSCs are programmed to undergo EC generation, Ve-cad and CD31 markers are expressed. Successful generation of ECs is shown by subsequent expression of adhesion molecules, such as ICAM-1 and VCAM-1, which promote vasculogenesis and vascular repair. In addition, iPSC differentiation into VSMCs results in expression of markers, such as SM22α and SM-γ-actin. VSMCs increase coronary angiogenesis and vascular repair. Additionally, iPSCs transform into CMs by expressing cardiac markers, such as α/β-MHC, TnC, TnI, and TnT, which increase cardiac cell proliferation, cardiac repair, and cardiogenesis
Pros and Cons
CTC generation and transplantation have revealed both advantages and disadvantages. Electrophysiological and contractile functions of the cardiovascular system are highly important to maintain optimal functionality. HiPSCs-CTCs have been found to induce appropriate electrophysiological and contractile roles in cardiovascular system. For instance, Ca2+ plays a crucial role in VSMC and CM contractility. Reduced Ca2+ sensitivity promotes vascular abnormalities and arrythmia. Interestingly, HiPSCs-CTCs showed increased and appropriate biophysical properties of the ionic currents INa, ICaL, IK1, which include the genes SCN5A, CACNA1C, CACNA1D, KCNQ, and KCNH2, as well as upregulated Na+, Ca2+, and K+ sensibility [81], preventing MI after iPSC-CM transplantation in mice [82].
Moreover, hiPSCs-CTCs express higher level of plasmalogen phosphatidylethanolamines that promote lipid metabolism [83]. In addition, hiPSCs-CTCs have shown increased levels of GLUT1, GLUT3, GLUT4 and insulin secretion, which elevate glucose uptake and metabolism, while reducing reactive oxygen species (ROS) production and accumulation, inflammation, and vascular abnormalities [84,85,86]. Recently, studies have shown that hiPSCs-CTCs exhibit significant roles in homeostasis, resulting in appropriate adhesion molecule expression and decreasing inflammatory responses that lead to improved MI and extended lifespan in animals [87].
Furthermore, hiPSCs-CTCs exhibit optimal responses to drugs. HiPSCs-CTCs rapidly reduce oxidative stress after administration of cardioprotectant 312 (CP-312), an antioxidant response marker [88, 89]. Researchers have successfully generated cardiomyocytes from patients with congenital long QT syndromes (LQT2), and transplanted LQT2 hiPSCs-CMs responded appropriately to clinically relevant pharmacological treatment [90].
Nonetheless, therapy using iPSCs has raised significant concerns due to their capability to promote immunodeficiency, tumor occurrence, or teratomas. HiPSCs-CTCs may be recognized as foreign cells, which may trigger an immune response, indicating that immunosuppression will be necessary during therapy [91]. It has been reported that inefficient differentiation or purification techniques of iPSCs may lead to the development of cancer after transplantation. Previously, generation of iPSCs was based on genetic modifications. However, this method has been shown to be inappropriate and less clinically relevant. More recently, fluorescently activated cell sorting (FACS)-based techniques, including mitochondrial specific fluorescent dyes or hiPSC-CTC marker selection, nongenetic iPSC production, and isolation techniques, which do not stimulate tumorigenesis after transplantation, are applied [92,93,94]. Data indicate that in spite of the beneficial roles of hiPSC-CTC therapy, there are still disadvantages to overcome, such as immunosuppression and tendency toward tumor development, that need to be addressed (Table 3).
Conclusions
Studies have revealed a loss of CTCs in human MI. Therefore, the replacement of lost cardiovascular cells to prevent MI has become important from a therapeutic perspective. Researchers have reported that hiPSCs can be reprogrammed to generate CTCs through complex processes and pathways. Recent studies have shown that transplanted hiPSC-derived CTCs improved MI outcome in both mouse and swine models [9, 10], although the actual pathways involved in hiPSC differentiation remain unclear. The present study explains the pathways associated with the generation of CTCs through activation stimulants, such as TGF-β and BMP-4/smad signaling, which activate snail and twist transcription factors. Other cytokines, such as IL1β, FGF, VEGF-A, Ang II, etc., stimulate CTC production via Akt, PI3K, and transcription factors, such as NFκB, snail, Oct4, Nkx2.5, α/β-MHC, etc. Moreover, hiPSCs provide an adequate microenvironment that promotes the replication of pre-existing cells to allow replacement of dead cells, preventing MI. It is clear that hiPSC transplantation promotes rapid cardiac repair more so than contemporary surgical and pharmacological therapy, suggesting that adaptation and encouraging of hiPSC therapy may minimize CVD-related mortality worldwide. Nonetheless, more testing guides for hiPSCs therapy in human must be encouraged in randomized clinical trials, including sequential, multiple assessment, randomized control trials, and cohort studies. Moreover, providing a tracking system for transplanted cells to assess proliferation rate to avoid overproliferation and tumor development may prove useful. In addition, regular monitoring of patients receiving hiPSC immunity to prevent complete immunodeficiency may enable termination of opportunistic infections and other complications.
References
Zwi-Dantsis, L., et al. (2013). Derivation and cardiomyocyte differentiation of induced pluripotent stem cells from heart failure patients. European Heart Journal, 34(21), 1575–1586.
D'Amico, R. W., et al. (2018). Pulmonary vascular platform models the effects of flow and pressure on endothelial dysfunction in BMPR2 associated pulmonary arterial hypertension. International Journal of Molecular Sciences, 19(9), 2561.
Tang, N., et al. (2016). Monocyte exosomes induce adhesion molecules and cytokines via activation of NF-kappaB in endothelial cells. The FASEB Journal, 30(9), 3097–3106.
Chen, L., et al. (2019). CTRP3 alleviates ox-LDL-induced inflammatory response and endothelial dysfunction in mouse aortic endothelial cells by activating the PI3K/Akt/eNOS pathway. Inflammation, 1–10.
Cai, H., et al. (2019). Hypochlorous acid-modified extracellular matrix contributes to the behavioral switching of human coronary artery smooth muscle cells. Free Radical Biology & Medicine, 134, 516–526.
Lacolley, P., et al. (2017). Vascular smooth muscle cells and arterial stiffening: relevance in development, aging, and disease. Physiological Reviews, 97(4), 1555–1617.
Jin, H., et al. (2018). Local delivery of miR-21 stabilizes fibrous caps in vulnerable atherosclerotic lesions. Molecular Therapy, 26(4), 1040–1055.
Luo, Y., et al. (2017). Macrophagic CD146 promotes foam cell formation and retention during atherosclerosis. Cell Research, 27(3), 352–372.
Zhang, Y., et al. (2016). Expandable cardiovascular progenitor cells reprogrammed from fibroblasts. Cell Stem Cell, 18(3), 368–381.
Ye, L., et al. (2014). Cardiac repair in a porcine model of acute myocardial infarction with human induced pluripotent stem cell-derived cardiovascular cells. Cell Stem Cell, 15(6), 750–761.
Zhou, J., et al. (2010). High-efficiency induction of neural conversion in human ESCs and human induced pluripotent stem cells with a single chemical inhibitor of transforming growth factor beta superfamily receptors. Stem Cells, 28(10), 1741–1750.
Bai, H., et al. (2013). The balance of positive and negative effects of TGF-beta signaling regulates the development of hematopoietic and endothelial progenitors in human pluripotent stem cells. Stem Cells and Development, 22(20), 2765–2776.
Wang, J., et al. (2013). Transforming growth factor beta-regulated microRNA-29a promotes angiogenesis through targeting the phosphatase and tensin homolog in endothelium. The Journal of Biological Chemistry, 288(15), 10418–10426.
Adams, W. J., et al. (2013). Functional vascular endothelium derived from human induced pluripotent stem cells. Stem Cell Reports, 1(2), 105–113.
Bulysheva, A. A., et al. (2016). Vascular endothelial growth factor-A gene electrotransfer promotes angiogenesis in a porcine model of cardiac ischemia. Gene Therapy, 23(8–9), 649–656.
Lv, Y. X., et al. (2018). VEGF-A and VEGF-B coordinate the arteriogenesis to repair the infarcted heart with vagus nerve stimulation. Cellular Physiology and Biochemistry, 48(2), 433–449.
Wang, Y., et al. (2016). The transplantation of Akt-overexpressing amniotic fluid-derived mesenchymal stem cells protects the heart against ischemia-reperfusion injury in rabbits. Molecular Medicine Reports, 14(1), 234–242.
Harding, A., et al. (2017). Highly efficient differentiation of endothelial cells from pluripotent stem cells requires the MAPK and the PI3K pathways. Stem Cells, 35(4), 909–919.
Zhang, Z., et al. (2015). Activated phosphatidylinositol 3-kinase/Akt inhibits the transition of endothelial progenitor cells to mesenchymal cells by regulating the forkhead box subgroup O-3a signaling. Cellular Physiology and Biochemistry, 35(4), 1643–1653.
Wang, Y., et al. (2014). Suicide gene-mediated sequencing ablation revealed the potential therapeutic mechanism of induced pluripotent stem cell-derived cardiovascular cell patch post-myocardial infarction. Antioxidants & Redox Signaling, 21(16), 2177–2191.
Rosa, S., et al. (2019). Functional characterization of iPSC-derived arterial- and venous-like endothelial cells. Scientific Reports, 9(1), 3826.
Songstad, A. E., et al. (2017). Connective tissue growth factor promotes efficient generation of human induced pluripotent stem cell-derived choroidal endothelium. Stem Cells Translational Medicine, 6(6), 1533–1546.
Chan, X. Y., et al. (2015). Three-dimensional vascular network assembly from diabetic patient-derived induced pluripotent stem cells. Arteriosclerosis, Thrombosis, and Vascular Biology, 35(12), 2677–2685.
Hurlstone, A. F., et al. (2003). The Wnt/beta-catenin pathway regulates cardiac valve formation. Nature, 425(6958), 633–637.
Cai, X., et al. (2013). Tbx20 acts upstream of Wnt signaling to regulate endocardial cushion formation and valve remodeling during mouse cardiogenesis. Development, 140(15), 3176–3187.
Umbhauer, M., et al. (2000). The C-terminal cytoplasmic Lys-thr-X-X-X-Trp motif in frizzled receptors mediates Wnt/beta-catenin signalling. The EMBO Journal, 19(18), 4944–4954.
Maltabe, V. A., et al. (2016). Isolation of an ES-derived cardiovascular multipotent cell population based on VE-cadherin promoter activity. Stem Cells International, 2016, 8305624.
Marchetti, S., et al. (2002). Endothelial cells genetically selected from differentiating mouse embryonic stem cells incorporate at sites of neovascularization in vivo. Journal of Cell Science, (115(Pt 10), 2075–2085.
Lian, X., et al. (2014). Efficient differentiation of human pluripotent stem cells to endothelial progenitors via small-molecule activation of WNT signaling. Stem Cell Reports, 3(5), 804–816.
Collado, M. S., et al. (2017). Exposure of induced pluripotent stem cell-derived vascular endothelial and smooth muscle cells in coculture to hemodynamics induces primary vascular cell-like phenotypes. Stem Cells Translational Medicine, 6(8), 1673–1683.
Shen, X., et al. (2017). Differentiation of mesenchymal stem cells into cardiomyocytes is regulated by miRNA-1-2 via WNT signaling pathway. Journal of Biomedical Science, 24(1), 29.
Ishizuka, T., et al. (2012). Effect of angiotensin II on proliferation and differentiation of mouse induced pluripotent stem cells into mesodermal progenitor cells. Biochemical and Biophysical Research Communications, 420(1), 148–155.
Zheng, X., et al. (2013). Angiotensin II promotes differentiation of mouse embryonic stem cells to smooth muscle cells through PI3-kinase signaling pathway and NF-kappaB. Differentiation, 85(1–2), 41–54.
Jiao, J., et al. (2018). Induced pluripotent stem cells with NOTCH1 gene mutation show impaired differentiation into smooth muscle and endothelial cells: implications for bicuspid aortic valve-related aortopathy. The Journal of Thoracic and Cardiovascular Surgery, 156(2), 515–522 e1.
Jiao, J., et al. (2016). Differentiation defect in neural crest-derived smooth muscle cells in patients with aortopathy associated with bicuspid aortic valves. EBioMedicine, 10, 282–290.
Chang, L., et al. (2012). Differentiation of vascular smooth muscle cells from local precursors during embryonic and adult arteriogenesis requires Notch signaling. Proceedings of the National Academy of Sciences of the United States of America, 109(18), 6993–6998.
Liu, Y., et al. (2014). Timely inhibition of Notch signaling by DAPT promotes cardiac differentiation of murine pluripotent stem cells. PLoS One, 9(10), e109588.
Yang, C., et al. (2017). Induced pluripotent stem cell modelling of HLHS underlines the contribution of dysfunctional NOTCH signalling to impaired cardiogenesis. Human Molecular Genetics, 26(16), 3031–3045.
Gong, H., et al. (2014). Knockdown of nucleosome assembly protein 1-like 1 induces mesoderm formation and cardiomyogenesis via notch signaling in murine-induced pluripotent stem cells. Stem Cells, 32(7), 1759–1773.
Jiang, S., & Zhang, S. (2017). Differentiation of cardiomyocytes from amniotic fluid-derived mesenchymal stem cells by combined induction with transforming growth factor beta1 and 5azacytidine. Molecular Medicine Reports, 16(5), 5887–5893.
Ishizuka, T., et al. (2014). Involvement of beta-adrenoceptors in the differentiation of human induced pluripotent stem cells into mesodermal progenitor cells. European Journal of Pharmacology, 740, 28–34.
Ikuno, T., et al. (2017). Correction: efficient and robust differentiation of endothelial cells from human induced pluripotent stem cells via lineage control with VEGF and cyclic AMP. PLoS One, 12(4), e0176238.
Yamazaki, A., et al. (2016). Isoproterenol directs hair follicle-associated pluripotent (HAP) stem cells to differentiate in vitro to cardiac muscle cells which can be induced to form beating heart-muscle tissue sheets. Cell Cycle, 15(5), 760–765.
Shirai, K., et al. (2017). Hypoxia enhances differentiation of hair follicle-associated-pluripotent (HAP) stem cells to cardiac-muscle cells. Journal of Cellular Biochemistry, 118(3), 554–558.
Liao, S., et al. (2019). Potent immunomodulation and angiogenic effects of mesenchymal stem cells versus cardiomyocytes derived from pluripotent stem cells for treatment of heart failure. Stem Cell Research & Therapy, 10(1), 78.
Kim, J. A., et al. (2015). Regulation of mesenchymal stromal cells through fine tuning of canonical Wnt signaling. Stem Cell Research, 14(3), 356–368.
von Gise, A., et al. (2011). WT1 regulates epicardial epithelial to mesenchymal transition through beta-catenin and retinoic acid signaling pathways. Developmental Biology, 356(2), 421–431.
Mahapatra, S., Martin, D., & Gallicano, G. I. (2018). Re-defining stem cell-cardiomyocyte interactions: focusing on the paracrine effector approach. Journal of Stem cells and Regenerative Medicine, 14(1), 10–26.
Luxan, G., et al. (2016). Endocardial notch signaling in cardiac development and disease. Circulation Research, 118(1), e1–e18.
Wu, K. H., et al. (2018). MicroRNA-34a modulates the Notch signaling pathway in mice with congenital heart disease and its role in heart development. Journal of Molecular and Cellular Cardiology, 114, 300–308.
High, F. A., et al. (2007). An essential role for Notch in neural crest during cardiovascular development and smooth muscle differentiation. The Journal of Clinical Investigation, 117(2), 353–363.
Godby, R. C., et al. (2014). Cross talk between Notch signaling and biomechanics in human aortic valve disease pathogenesis. Journal of Cardiovascular Development and Disease, 1(3), 237–256.
Hrstka, S. C., et al. (2017). NOTCH1-dependent nitric oxide signaling deficiency in hypoplastic left heart syndrome revealed through patient-specific phenotypes detected in bioengineered cardiogenesis. Stem Cells, 35(4), 1106–1119.
Bischoff, J., et al. (2016). CD45 expression in mitral valve endothelial cells after myocardial infarction. Circulation Research, 119(11), 1215–1225.
Skelton, R. J., et al. (2014). SIRPA, VCAM1 and CD34 identify discrete lineages during early human cardiovascular development. Stem Cell Research, 13(1), 172–179.
Clayton, Z. E., et al. (2018). Induced pluripotent stem cell-derived endothelial cells promote angiogenesis and accelerate wound closure in a murine excisional wound healing model. Bioscience Reports, 38(4).
Liu, G., et al. (2018). Human urine-derived stem cell differentiation to endothelial cells with barrier function and nitric oxide production. Stem Cells Translational Medicine.
Nakayama, K. H., et al. (2015). Bilayered vascular graft derived from human induced pluripotent stem cells with biomimetic structure and function. Regenerative Medicine, 10(6), 745–755.
Halaidych, O. V., et al. (2018). Inflammatory responses and barrier function of endothelial cells derived from human induced pluripotent stem cells. Stem Cell Reports, 10(5), 1642–1656.
Ding, X., et al. (2017). Upregulation of SRF is associated with hypoxic pulmonary hypertension by promoting viability of smooth muscle cells via increasing expression of Bcl-2. Journal of Cellular Biochemistry, 118(9), 2731–2738.
Liu, S., et al. (2019). MiR-378a-5p regulates proliferation and migration in vascular smooth muscle cell by targeting CDK1. Frontiers in Genetics, 10, 22.
Bai, Y., et al. (2019). Modulation of the proliferation/apoptosis balance of vascular smooth muscle cells in atherosclerosis by lncRNA-MEG3 via regulation of miR-26a/Smad1 Axis. International Heart Journal, 60(2), 444–450.
Jamaiyar, A., et al. (2017). Alignment of inducible vascular progenitor cells on a micro-bundle scaffold improves cardiac repair following myocardial infarction. Basic Research in Cardiology, 112(4), 41.
Chen, S., & Lechleider, R. J. (2004). Transforming growth factor-beta-induced differentiation of smooth muscle from a neural crest stem cell line. Circulation Research, 94(9), 1195–1202.
Chan, M. C., et al. (2010). Molecular basis for antagonism between PDGF and the TGFbeta family of signalling pathways by control of miR-24 expression. The EMBO Journal, 29(3), 559–573.
Patsch, C., et al. (2015). Generation of vascular endothelial and smooth muscle cells from human pluripotent stem cells. Nature Cell Biology, 17(8), 994–1003.
Dash, B. C., et al. (2016). Tissue-engineered vascular rings from human iPSC-derived smooth muscle cells. Stem Cell Reports, 7(1), 19–28.
Liu, Y., et al. (2016). Mesp1 marked cardiac progenitor cells repair infarcted mouse hearts. Scientific Reports, 6, 31457.
Remedios, L. J. Y. H. S. H. C. G.d. (2003). Cardiomyocyte apoptosis is associated with increased wall stress in chronic failing left ventricle. European Heart Journal, 24(8), 742–751.
Tachibana, A., et al. (2017). Paracrine effects of the pluripotent stem cell-derived cardiac myocytes salvage the injured myocardium. Circulation Research, 121(6), e22–e36.
Martinez-Fernandez, A., et al. (2010). c-MYC independent nuclear reprogramming favors cardiogenic potential of induced pluripotent stem cells. Journal of Cardiovascular Translational Research, 3(1), 13–23.
Chan, S. S., et al. (2010). Fibroblast growth factor-10 promotes cardiomyocyte differentiation from embryonic and induced pluripotent stem cells. PLoS One, 5(12), e14414.
Morabito, C. J., et al. (2001). Positive and negative regulation of epicardial-mesenchymal transformation during avian heart development. Developmental Biology, 234(1), 204–215.
Karimzadeh, F., & Opas, M. (2017). Calreticulin is required for TGF-beta-induced epithelial-to-mesenchymal transition during cardiogenesis in mouse embryonic stem cells. Stem Cell Reports, 8(5), 1299–1311.
Wang, K., et al. (2018). Hypoxia-stressed cardiomyocytes promote early cardiac differentiation of cardiac stem cells through HIF-1alpha/Jagged1/Notch1 signaling. Acta Pharmaceutica Sinica B, 8(5), 795–804.
Sun, X., et al. (2015). HIF2alpha induces cardiomyogenesis via Wnt/beta-catenin signaling in mouse embryonic stem cells. Journal of Translational Medicine, 13, 88.
Xue, Y., et al. (2014). Insulin-like growth factor binding protein 4 enhances cardiomyocytes induction in murine-induced pluripotent stem cells. Journal of Cellular Biochemistry, 115(9), 1495–1504.
Minato, A., et al. (2012). Cardiac differentiation of embryonic stem cells by substrate immobilization of insulin-like growth factor binding protein 4 with elastin-like polypeptides. Biomaterials, 33(2), 515–523.
Sebastiao, M. J., et al. (2019). Human cardiac progenitor cell activation and regeneration mechanisms: exploring a novel myocardial ischemia/reperfusion in vitro model. Stem Cell Research & Therapy, 10(1), 77.
El Harane, N., et al. (2018). Acellular therapeutic approach for heart failure: in vitro production of extracellular vesicles from human cardiovascular progenitors. European Heart Journal, 39(20), 1835–1847.
Blazeski, A., et al. (2012). Cardiomyocytes derived from human induced pluripotent stem cells as models for normal and diseased cardiac electrophysiology and contractility. Progress in Biophysics and Molecular Biology, 110(2–3), 166–177.
Wang, H., et al. (2016). Generation of electrophysiologically functional cardiomyocytes from mouse induced pluripotent stem cells. Stem Cell Research, 16(2), 522–530.
Nakamura, Y., et al. (2017). Changes of plasmalogen phospholipid levels during differentiation of induced pluripotent stem cells 409B2 to endothelial phenotype cells. Scientific Reports, 7(1), 9377.
Al-Ahmad, A. J. (2017). Comparative study of expression and activity of glucose transporters between stem cell-derived brain microvascular endothelial cells and hCMEC/D3 cells. American Journal of Physiology. Cell Physiology, 313(4), C421–C429.
Shaer, A., et al. (2015). Differentiation of human-induced pluripotent stem cells into insulin-producing clusters. Experimental and Clinical Transplantation, 13(1), 68–75.
Nose, N., et al. (2018). Metabolic substrate shift in human induced pluripotent stem cells during cardiac differentiation: functional assessment using in vitro radionuclide uptake assay. International Journal of Cardiology, 269, 229–234.
Ju, Z., et al. (2017). Exosomes from iPSCs delivering siRNA attenuate intracellular adhesion molecule-1 expression and neutrophils adhesion in pulmonary microvascular endothelial cells. Inflammation, 40(2), 486–496.
Kirby, R. J., et al. (2018). Discovery of novel small-molecule inducers of heme oxygenase-1 that protect human iPSC-derived cardiomyocytes from oxidative stress. The Journal of Pharmacology and Experimental Therapeutics, 364(1), 87–96.
Yue, X., Acun, A., & Zorlutuna, P. (2017). Transcriptome profiling of 3D co-cultured cardiomyocytes and endothelial cells under oxidative stress using a photocrosslinkable hydrogel system. Acta Biomaterialia, 58, 337–348.
Matsa, E., et al. (2011). Drug evaluation in cardiomyocytes derived from human induced pluripotent stem cells carrying a long QT syndrome type 2 mutation. European Heart Journal, 32(8), 952–962.
Kooreman, N. G., et al. (2017). Alloimmune responses of humanized mice to human pluripotent stem cell therapeutics. Cell Reports, 20(8), 1978–1990.
Hattori, F., et al. (2010). Nongenetic method for purifying stem cell-derived cardiomyocytes. Nature Methods, 7(1), 61–66.
Dubois, N. C., et al. (2011). SIRPA is a specific cell-surface marker for isolating cardiomyocytes derived from human pluripotent stem cells. Nature Biotechnology, 29(11), 1011–1018.
Tohyama, S., et al. (2013). Distinct metabolic flow enables large-scale purification of mouse and human pluripotent stem cell-derived cardiomyocytes. Cell Stem Cell, 12(1), 127–137.
Jiang, Y., et al. (2018). TGF-beta1-induced SMAD2/3/4 activation promotes RELM-beta transcription to modulate the endothelium-mesenchymal transition in human endothelial cells. The International Journal of Biochemistry & Cell Biology, 105, 52–60.
Miscianinov, V., et al. (2018). MicroRNA-148b targets the TGF-beta pathway to regulate angiogenesis and endothelial-to-mesenchymal transition during skin wound healing. Molecular Therapy, 26(8), 1996–2007.
Wang, J., et al. (2017). The mechanism of TGF-beta/miR-155/c-Ski regulates endothelial-mesenchymal transition in human coronary artery endothelial cells. Bioscience Reports, 37(4).
Bezenah, J. R., Kong, Y. P., & Putnam, A. J. (2018). Evaluating the potential of endothelial cells derived from human induced pluripotent stem cells to form microvascular networks in 3D cultures. Scientific Reports, 8(1), 2671.
Maleszewska, M., et al. (2013). IL-1beta and TGFbeta2 synergistically induce endothelial to mesenchymal transition in an NFkappaB-dependent manner. Immunobiology, 218(4), 443–454.
Maleszewska, M., et al. (2015). Enhancer of zeste homolog-2 (EZH2) methyltransferase regulates transgelin/smooth muscle-22alpha expression in endothelial cells in response to interleukin-1beta and transforming growth factor-beta2. Cellular Signalling, 27(8), 1589–1596.
Tang, R. N., et al. (2013). Effects of angiotensin II receptor blocker on myocardial endothelial-to-mesenchymal transition in diabetic rats. International Journal of Cardiology, 162(2), 92–99.
Giordano, S., et al. (2017). Induced pluripotent stem cell-derived endothelial cells overexpressing Interleukin-8 receptors a/B and/or C-C chemokine receptors 2/5 inhibit vascular injury response. Stem Cells Translational Medicine, 6(4), 1168–1177.
Chang, A. C., et al. (2014). A Notch-dependent transcriptional hierarchy promotes mesenchymal transdifferentiation in the cardiac cushion. Developmental Dynamics, 243(7), 894–905.
Chang, A. C., et al. (2011). Notch initiates the endothelial-to-mesenchymal transition in the atrioventricular canal through autocrine activation of soluble guanylyl cyclase. Developmental Cell, 21(2), 288–300.
Funding
This research was supported by the National Natural Sciences Foundation of China (81470569), The Innovation Foundation for Postgraduate of Hunan Province (CX2017B550, CX2016B490), Natural Science Foundation of Hunan Province, China (2018JJ2341), Science Foundation of The Heath and Family Planning Commission in Hunan Province of China (B2019122), and the National College Students Innovation and Entrepreneurship Fund (201710555015, 201710555010).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interests
All authors declare that they have no conflicts of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Associate Editor Joost Sluijter oversaw the review of this article
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jackson, A.O., Tang, H. & Yin, K. HiPS-Cardiac Trilineage Cell Generation and Transplantation: a Novel Therapy for Myocardial Infarction. J. of Cardiovasc. Trans. Res. 13, 110–119 (2020). https://doi.org/10.1007/s12265-019-09891-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-019-09891-4