Abstract
Malignant pleural effusion (PE) is a complication that often occurs in advanced cancer. The sensitivity of pleural fluid cytology is reported to vary from 30 to 90%; therefore, the process is less clinically practical in certain conditions. Thus, special biomarkers are needed to distinguish malignant PE and nonmalignant PE. The aim of this study is to compare the level of vascular endothelial growth factor-A (VEGF-A) in pleural fluid of patients with that in malignant and nonmalignant PE. Participants were divided into 2 groups: 19 patients with nonmalignant PE, and 34 patients with malignant PE. Both groups underwent pleural puncture procedures and were examined for VEGF-A levels. Statistical analysis was performed using the paired test or Mann–Whitney test. The ROC curve was employed to determine the VEGF-A cut-off value in malignant PE. The VEGF-A level in pleural fluid of malignant PE group was 1940.77 ± 1016.54 pg/mL, while the nonmalignant group was 178.16 ± 192.01 pg/mL (p < 0.001; 95% CI). The average VEGF-A level in malignant PE group with positive anatomic pathology results was 2036.69 ± 1008.15 pg/mL, and negative was 1855.51 ± 1045.35 pg/mL (p = 0.612; 95% CI). The cutoff value for VEGF-A level in pleural fluid for the diagnosis of malignant PE was 416.60 pg/mL with a sensitivity and specificity of 85.29% and 84.22% respectively. Examination of VEGF-A level in pleural fluid can be considered as a means of supporting the diagnosis of malignant PE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malignant pleural effusion (PE) is the most common complication found in advanced cancer. Malignant PE cases are estimated to occur in more than 150,000 people each year in the USA, and patients with complications or metastases from lung cancer account for half of the cases [1]. Epidemiological studies showed there are 22% of malignant PE and 42% of exudate PE. Epidemiological studies in Western countries found three major causes of PE, namely malignant PE, heart failure, and parapneumonic effusion [2]. Malignant PE originates from primary pleural malignancies (e.g., mesothelioma) or from pleural metastases from extrapleural malignancies. Lung cancer is the most common cause of malignant PE with an incidence of 25–52%. Metastatic adenocarcinoma is a histopathological type of tumor that most often causes malignant PE [3].
The diagnosis of malignant PE often faces problems. Current definitive method for diagnosing malignant PE is by performing cytology examination on pleural fluid. In general, the specificity of this procedure is high, but its sensitivity is reported to vary from 30 to 90%. Therefore, the process is less clinically practical in certain conditions. If the cytological examination is negative, a 7–12% diagnosis of malignant PE can be made with pleural biopsy. Medical thoracoscopy is the next diagnostic option in cases of exudative PE with a suspected cause of malignancy. However, around 10% of PE cases fail to establish the etiologic diagnosis after thoracoscopy, and more than 20% cannot be diagnosed after pleural fluid cytology and pleural biopsy [4]. The medical thoracoscopy procedure is not always available at all health facilities, and the examination costs are quite high. More than 15% of patients with exudative PE cannot be diagnosed with an etiological diagnosis after pleural cytology and biopsy. Therefore, it is necessary to find a fluid marker that can distinguish malignant and nonmalignant PE [2].
The pathophysiology of malignant PE formation includes mechanisms of pleural fluid drainage related to obstruction of blood vessels and pulmonary as well as pleural lymphatic systems. Lymphatic tissue obstruction is caused by the spread of tumors in the parietal pleural stomata and mediastinal lymph node which results in obstruction of fluid in the pleural cavity. Barriers to fluid flow from the pleural cavity are not the only cause of PE formation [2, 3]. Malignant PE does not always occur in some tumors causing lymphatic obstruction [5]. Tumor cells secrete several vasoactive mediators that contribute to the formation of malignant PE by increasing the rate of leakage of blood vessels. Increased vascular permeability results in excessive plasma leakage. The main mediators that play roles in vascular leakage are vascular endothelial growth factor (VEGF) and angiopoietin [6]. Vascular endothelial growth factor-A (VEGF-A) is one of the cytokines that play a role in the formation of malignant PE [7].
VEGF-A has two main functions, namely increasing vascular permeability, and serving as the most important angiogenic factor in various physiological and pathological conditions including infection. Bacterial infection causes an acute inflammatory response associated with neutrophil influx, increased vascular permeability, and edema. A study of neutrophil stimulation in vitro showed that bacterial infection also induces VEGF-A secretion [8]. In addition to acute bacterial infections, an increase in VEGF level is detected in granulomatous diseases, such as tuberculosis. Alveolar macrophage stimulation in the tuberculosis infection process secretes various cytokines including VEGF. In tuberculosis patients, there is an increase in serum VEGF levels compared with those of inactive tuberculosis patients [9].
Biomarkers of the nature of VEGF are involved in normal physiological processes and in many diseases, including inflammatory conditions and are essential for angiogenesis that is a prerequisite for growth or healing. Pleural fluid contains VEGF receptors, and many cells like macrophages mesothelial cells, infiltrating inflammatory cells, cancer cells, adjacent airway epithelial cells, type II alveolar cells, alveolar macrophages, infiltrating neutrophils, and eosinophils of the lung—all of which may contribute to VEGF accumulation in pleural fluid [10, 11].
In the study, Matsuyama et al. [9] measured subsets of VEGF in duplicate serum samples and characterized the soluble isoforms VEGF 165 and VEGF 121. Their assays were reported to be sensitive to the presence of just 9 pg/mL and were not affected by the presence of other cytokines like platelet-derived growth factor (PDGF) and other homologous markers. They found high titers in active pulmonary tuberculosis and related the falling titers over a period of 6 months, with an improvement of PT. They also studied the Presence of VEGF in macrophages of the lung specimens by histochemistry. Biomarkers thus can sometimes help in monitoring the clinical course as is well known with others such as CRP, ProCal, etc. In a controlled blinded prospective study, Shu et al. [4] estimated VEGF in both serum and pleural fluid simultaneously and evaluated them against the standard of clinical evaluation by pleural cytology and pleural biopsy. They found that after “using receiver operating characteristic analysis” the cutoff values of VEGF levels in PE and serum to be 959.25 pg/mL and 212.36 pg/mL respectively for diagnosis of malignant PE (sensitivity 47%, 69% and specificities of 98% and 86% respectively). In other words as a diagnostic test, it is inadequate and at best can be an expensive test to aid a diagnosis awaiting confirmation by other means.
This study measured VEGF-A level in pleural fluid of patients with malignant PE related to lung cancer, and patients with nonmalignant PE related to the infection process, as well as assessing the difference between the two. The aim of this study is to determine the potential of VEGF-A level in pleural fluid as a biomarker in the diagnosis of malignant PE and provide a pathophysiological picture of malignant PE related to lung cancer and nonmalignant PE related to infection.
Methods
Participants in this study were patients with PE in Dr. Soetomo General A Hospital, Surabaya, Indonesia. The inclusion criteria were patients aged > 16 years old with malignant PE diagnosis (lung cancer) and patients diagnosed with nonmalignant PE (pneumonia and/or lung tuberculosis). Patients with malignant PE receiving chemotherapy and empyema patients were excluded from this study. The participants filled the consent form before the study. The diagnosis of lung cancer used standard diagnosis in Dr. Soetomo General Academic Hospital, Surabaya, Indonesia [12, 13].
A cross-sectional method was employed with a consecutive sampling technique. The study was conducted in Dr. Soetomo General Academic Hospital from August to December 2018. A total of 53 participants were divided into two groups: malignant PE group consisting of 34 patients and non-malignant PE group consisting of 19 patients (Fig. 1). All participants were examined for VEGF-A level in pleural fluid, followed by a comparative analysis between the two groups. This study was reviewed by the ethical committee and has received approval (0609/KEPK/Ix/2018) before its conduct.
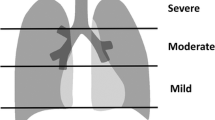
The examination of VEGF-A level was conducted following the thoracentesis procedure. The pleural fluid was obtained by firstly determining the position of the lung where PE took place. Then, a needle was inserted to a point in the midaxillary line in the 6th, 7th, or 8th intercostal [14]. In the case of minimum PE, the thoracentesis procedure was assisted with ultrasonography guidance [15]. Pleural fluid was obtained with a volume of 20 cc, placed in a tube and centrifuged for 10 min. The supernatant was extracted and stored in a fridge at 18–25 °C. The VEGF-A serum was measured using a Sandwich Enzyme-Linked Immunosorbent Assay (ELISA; system R&D, USA), and was read at 450 nm in a 680XR microplate reader (Biorad, USA) [16].
The results were presented in the form of mean ± standard deviation (SD). Statistical analysis was performed using the paired t test or Mann–Whitney test (CI 95%; p < 0.05). Kolmogorov–Smirnov test was employed to examine data distribution. Receiver operating characteristics (ROC) was employed to determine the cutoff value of VEGF-A in malignant PE patients. The ROC was obtained by measuring sensitivity and specificity values of malignant PE. IBM SPSS Statistics software version 23.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis.
Results
Characteristics of the Participants
Participants were divided into two groups: malignant PE (34 patients; 54.15%) and nonmalignant PE (19 patients; 35.85%). Most participants were female patients, consisting of 52.64% in nonmalignant group and 55.88% in malignant group. The average age of the participants was 53.58 ± 13.53 years old, ranging from 16 to 81 years old. Most participants in nonmalignant group attended senior high school (36.84%), followed by elementary school (26.31%). On the other hand, most participants in malignant group were elementary school graduates (38.23%), followed by senior high school graduates (32.35%). In terms of occupation, housewives consisted of 26.31% in nonmalignant group and 44.12% in malignant group. In terms of smoking status, most participants were non-smokers(32 patients,60.38%; Table 1).
For the diagnosis of participants, out of 34 malignant PE patients, 29 patients were diagnosed with adenocarcinoma (85.29%), 1 patient with adenosquamous carcinoma (2.94%), 3 patients with squamous cell carcinoma (8.82%), and 1 patient with small-cell carcinoma (2.94%). In the nonmalignant group, there were 17 patients with tuberculous PE (89.47%), 1 patient with pneumonia (5.26%), and 1 patient with pneumonia + tuberculosis (5.26%).
Results of Pleural Fluid Analysis
The average number of cells in the nonmalignant group (2433.11 ± 2463.30/μl) was higher than the malignant group (1876.82 ± 1808.00/μl). On the other hand, the average number of mononuclear (MN) in the nonmalignant group (69.84 ± 32.09%) was lower than the malignant group (75.17 ± 28.65%). The average protein content in the two groups showed nearly similar values. Statistics comparisons of the cell, MN, and protein amount were not significant. A significant comparison between nonmalignant and malignant groups was found for glucose content (p = 0.024) and lactic acid dehydrogenase/LDH (p = 0.025; Table 2).
The pathology examination of pleural fluid in terms of cytology in malignant group showed 13 positive patients (38.23%) and 21 negative patients (61.77%). On the other hand, pathology anthology examination on cell block found 18 negative participants (52.94%) and 16 positive participants (47.06%).
VEGF-A Level in Pleural Fluid
The average VEGF-A level in pleural fluid of malignant and non-malignant groups were 1940.77 ± 1016.54 pg/mL and 178.16 ± 192.01 pg/mL respectively (p < 0.001; Fig. 2). In the malignant group with positive anatomic pathology values, the VEGF-A level was 2036.69 ± 1008.15 pg/mL, while the VEGF-A level in negative anatomic pathologies was 1855.51 ± 1045.35 pg/mL (p = 0.612).
Cut-off, Sensitivity, and Specificity Values of VEGF-A in Pleural Fluid of Patients with Malignant Pleural Effusion
The cut-off value lay in the area under 0.963, where the intersection point between sensitivity and specificity was at point 22 with a VEGF-A value of 416.60 pg/mL (Fig. 3). The VEGF-A sensitivity and specificity values in this study were 85.29% and 84.22% respectively. Positive predictive value (PPV) of VEGF-A in this study was the number of samples in malignant PE group with VEGF-A levels ≥ cutoff values among all samples with VEGF-A levels ≥ cutoff values. Meanwhile, the negative predictive value (NPV) of VEGF-A in this study was the number of samples in nonmalignant PE group with VEGF-A levels < cutoff values among all samples with VEGF-A levels < cutoff values. The values of PPV and NPV VEGF-A in this study were 93.55% and 76.19% respectively.
Discussion
This study found that adenocarcinoma was the major profile causing malignant PE. Some studies suggested that most malignant PE occurs in adenocarcinoma [17]. Malignant PE is an early clinical sign that is generally found in lung adenocarcinoma patients, with a high EGFR mutation level particularly in exon 21 L858R mutation [18].
This study found significant differences in PE fluid between the two groups, especially in glucose and LDH levels. These significant differences might be due to tuberculosis related effusion in most participants in the nonmalignant group. Measurement of pleural fluid glucose levels (< 60 mg/dL) could indicate a diagnosis of parapneumonic PE, malignancy, rheumatoid disease, or tuberculous pleurisy [19]. Malignant PE and tuberculosis-related PE have a similar characteristic of pleural fluid analysis profile that is exudative lymphocytic predominant. In addition, glucose level in tuberculosis-related PE was found to be at a lower level of 4.33 mmol/L compared with malignant PE of 6.22 mmol/L [20]. Lactic acid dehydrogenase is a marker of non-specific inflammation that increases in both tuberculosis and cancer. In cancer, a higher LDH increase generally indicates a wider pleural inflammation process and the presence of blood cells in the pleural cavity [17].
The standard diagnosis of malignant PE is the presence of malignant cells in pleural fluid cytology. The specificity of pleural fluid cytology is generally high, but its sensitivity is reported between 30 and 90% [21]. Therefore, a biomarker is needed to help the diagnosis of malignant PE. In this study, the participants of malignant PE with positive pleural fluid anatomy pathology were 47.06% with cell block examination. This number was higher compared with the results of positive anatomic pathology with pleural fluid cytology examination of 38.23%. Cell block method has a higher sensitivity and can maintain tissue patterns, and the block can be stored for further staining or immunohistochemistry. Shivakumarswamy’s study compared the interpretation of pleural fluid anatomical pathology samples with cytology and cell block smears. The cell block showed cellular features with glandular patterns, cell layers, clusters, and cell balls. On the other hand, the cytology smear method showed the pattern of a spread-out single cell. The cell block method can also maintain the structure of the nucleus, cytoplasm, cell membranes, and chromatin details. Furthermore, it can increase the diagnosis of anatomic pathology by 15% compared with that of pleural fluid cytology. This study found an increase in the diagnosis of pleural fluid anatomy pathology by 9% [22].
In this study, malignant PE had significantly higher VEGF-A pleural fluid level than patients with nonmalignant effusion. Several previous studies stated that VEGF-A levels were consistently and significantly higher in malignant PE than nonmalignant PE. A study conducted by Jia et al. compared the value of VEGF-A serum in lung cancer, gastric cancer, and non-cancerous diseases. The study found that VEGF-A level in lung cancer pleural fluid was 457.54 pg/mL, while nonmalignant PE was 124.48 pg/mL [7]. Kim et al., in their study, compared pleural fluid VEGF levels in PE related to lung cancer and PE related to tuberculosis. The study obtained VEGF level in malignant PE was 2091.47 ± 1624.80 pg/mL; and in tuberculosis group, 1291.05 ± 110.53 pg/mL [17].
The VEGF-A values of participants with positive pleural fluid anatomy pathology were higher than those with negative pleural fluid anatomy pathology, although the difference was not statistically significant (p > 0.05). Patients with various types of lung cancer, especially non-small cell carcinoma (NSCC), generally have elevated VEGF expression in cancer cells. Several local cancer factors such as hypoxia, numerous growth, and hormonal factors can contribute to the induction of VEGF expression in cancer cells. Growth factors include epidermal growth factor, transforming growth factor, and insulin-like growth factor. Increased VEGF in malignant PE can also be related to the interaction of VEGF and VEGFR that stimulates cancer cells and mesothelial cells to secrete VEGF. Increased VEGF-A level in pleural fluid is not only related to the presence of malignant cells in PE, but also related to local cancer factors, mesothelial cells in malignant PE conditions that also secrete VEGF-A, and interactions between VEGF and VEGFR [7, 17, 23].
The VEGF-A value of ≥ 416.60 pg/mL that correctly clarified patients with malignant PE was in fact around 85.29%. On the other hand, the VEGF-A value of < 416.60 pg/mL that confirmed patients with PE instead of tuberculosis, according to the finding was 84.22%. A study by Jia et al. used median levels of VEGF-A level in pleural fluid with a cutoff value of 406.19 pg/mL, followed by survival time analysis, and obtained that patients with pleural fluid VEGF-A level of > 406.19 pg/mL had a relatively shorter survival time rate although not statistically significant (p = 0.066) [7]. In Zhou et al.’s study, the comparison of VEGF pleural fluid in malignant PE and pleural tuberculosis effusion resulted in sensitivity and specificity data of 71% and 61% respectively [24]. The difference in sensitivity and specificity values of this study compared with that of other studies could be caused partly by the differences in the characteristics and number of samples.
This study found that positive predictive value and negative predictive value of VEGF-A level in pleural fluid were 93.55% and 76.19% respectively. These values indicated that the VEGF-A value of ≥ 416.60 pg/mL could correctly predict tuberculosis PE patients at 93.55%, while the VEGF-A value of < 416.60 pg/mL could predict that a person does not suffer from a nonmalignant PE at 76.19%.
The limitation of this study is the diagnosis in the impure nonmalignant pleural effusion group using bacteriological examination results, but non-bacteriological assessment based on clinical symptoms, radiological results, and/or participant pleural fluid analysis. In addition, the grouping of pleural fluid types does not use Light’s criteria [25].
Conclusion
This study found a significant comparison between VEGF-A level in pleural fluid of patients with malignant and nonmalignant PE, where the VEGF-A level was higher in malignant PE than nonmalignant. There were no significant differences in VEGF-A levels in malignant PE patients with positive and negative anatomic pathology results. The sensitivity and specificity of VEGF-A level in pleural fluid for the diagnosis of malignant PE were 85.29% and 84.22% respectively, with a cutoff value of 416.60 pg/mL. The VEGF-A examination in pleural fluid can be considered as a means of supporting the diagnosis of malignant PE.
References
Asamura H (2010) Principles and practice of lung cancer. Lippincott Williams & Wilkins, Philadelphia
Thomas R, Kalomenidis I, Jett J, Lee YC (2016) Textbook of pleural diseases. Taylor & Francis
Haas AR, Sterman DH, Musani AI (2007) Malignant pleural effusions: management options with consideration of coding, billing, and a decision approach. Chest 132(3):1036–1041. https://doi.org/10.1378/chest.06-1757
Shu J, Sun G, Liu H, Liu J (2007) Clinical utility of vascular endothelial growth factor in diagnosing malignant pleural effusions. Acta Oncol 46(7):1004–1011
Spella M, Giannou AD, Stathopoulos GT (2015) Switching off malignant pleural effusion formation-fantasy or future? J Thorac Dis 7(6):1009–1020. https://doi.org/10.3978/j.issn.2072-1439.2015.05.20
Yano S, Shinohara H, Herbst RS, Kuniyasu H, Bucana CD, Ellis LM, Fidler IJ (2000) Production of experimental malignant pleural effusions is dependent on invasion of the pleura and expression of vascular endothelial growth factor/vascular permeability factor by human lung cancer cells. Am J Pathol 157(6):1893–1903. https://doi.org/10.1016/S0002-9440(10)64828-6
Jia L, Du Y, Li T, Lv Y, Wang Y, Zhang Y, Zhou X, Liu W (2015) Differential expression of vascular endothelial growth factor-A, -C and -D for the diagnosis and prognosis of cancer patients with malignant effusions. Oncol Lett 10(2):667–674. https://doi.org/10.3892/ol.2015.3305
Van Der Flier M, Coenjaerts F, Kimpen JL, Hoepelman AM, Geelen SP (2000) Streptococcus pneumoniae induces secretion of vascular endothelial growth factor by human neutrophils. Infect Immun 68(8):4792–4794. https://doi.org/10.1128/iai.68.8.4792-4794.2000
Matsuyama W, Hashiguchi T, Matsumuro K, Iwami F, Hirotsu Y, Kawabata M, Arimura K, Osame M (2000) Increased serum level of vascular endothelial growth factor in pulmonary tuberculosis. Am J Respir Crit Care Med 162(3):1120–1122
Fiorelli A, Vicidomini G, Di Domenico M, Napolitano F, Messina G, Morgillo F, Ciardiello F, Santini M (2011) Vascular endothelial growth factor in pleural fluid for differential diagnosis of benign and malignant origin and its clinical applications. Interact Cardiovasc Thorac Surg 12(3):420–424. https://doi.org/10.1510/icvts.2010.250357
Koniari I, Koletti B, Apostolakis E (2011) Vascular endothelial growth factor with tumour growth factor-beta, endostatin, proteinases or cytokines might be useful for differential diagnosis of pleural effusions. Interact Cardiovasc Thorac Surg 12(3):424–425. https://doi.org/10.1510/icvts.2010.250357A
Merinda V, Soegiarto G, Wulandari L (2020) T790M mutations identified by circulating tumor DNA test in lung adenocarcinoma patients who progressed on first-line epidermal growth factor receptor-tyrosine kinase inhibitors. Lung India 37(1):13–18. https://doi.org/10.4103/lungindia.lungindia_182_19
Wulandari L, Soegiarto G, Febriani A, Fatmawati F, Sahrun (2020) Comparison of detection of epidermal growth factor receptor (EFGR) gene mutation in peripheral blood plasma (liquid biopsy) with cytological specimens in lung adenocarcinoma patients. Indian J Surg Oncol. https://doi.org/10.1007/s13193-020-01046-1
Kalifatidis A, Lazaridis G, Baka S, Mpoukovinas I, Karavasilis V, Kioumis I, Pitsiou G, Papaiwannou A, Karavergou A, Tsakiridis K (2015) Thoracocentesis: from bench to bed. J Thorac Dis 7(1):S1–S4
Cao W, Wang Y, Zhou N, Xu B (2016) Efficacy of ultrasound-guided thoracentesis catheter drainage for pleural effusion. Oncol Lett 12(6):4445–4448
Gupta PK, Prabhakar S, Sharma S, Anand A (2011) Vascular endothelial growth factor-a (VEGF-A) and chemokine ligand-2 (CCL2) in amyotrophic lateral sclerosis (ALS) patients. J Neuroinflammation 8(1):47
Kim H-R, Kim B-R, Park R-K, Yoon K-H, Jeong E-T, Hwang K-E (2017) Diagnostic significance of measuring vascular endothelial growth factor for the differentiation between malignant and tuberculous pleural effusion. Tohoku J Exp Med 242(2):137–142. https://doi.org/10.1620/tjem.242.137
Wu S-G, Yu C-J, Tsai M-F, Liao W-Y, Yang C-H, Jan I-S, Yang P-C, Shih J-Y (2013) Survival of lung adenocarcinoma patients with malignant pleural effusion. Eur Respir J 41(6):1409–1418
Light RW (2007) Pleural diseases. 5 edn. Lippincott Williams & Wilkins
Porcel JM, Vives M (2003) Differentiating tuberculous from malignant pleural effusions: a scoring model. Med Sci Monit 9(5):CR175–CR180
Takahashi S (2011) Vascular endothelial growth factor (VEGF), VEGF receptors and their inhibitors for antiangiogenic tumor therapy. Biol Pharm Bull 34(12):1785–1788. https://doi.org/10.1248/bpb.34.1785
Shivakumarswamy U, Arakeri SU, Karigowdar MH, Yelikar B (2012) Diagnostic utility of the cell block method versus the conventional smear study in pleural fluid cytology. J Cytol 29(1):11–15. https://doi.org/10.4103/0970-9371.93210
Chen Y, Mathy NW, Lu H (2018) The role of VEGF in the diagnosis and treatment of malignant pleural effusion in patients with non-small cell lung cancer (review). Mol Med Rep 17(6):8019–8030. https://doi.org/10.3892/mmr.2018.8922
Zhou WB, Bai M, Jin Y (2009) Diagnostic value of vascular endothelial growth factor and endostatin in malignant pleural effusions. Int J Tuberc Lung Dis 13(3):381–386
Porcel JM (2013) Identifying transudates misclassified by Light’s criteria. Curr Opin Pulm Med 19(4):362–367. https://doi.org/10.1097/MCP.0b013e32836022dc
Acknowledgments
We thank Ms. Rossellini Ngiono B. Sc for her dedicated time to review and proofread our manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed toward data analysis, drafting and revising the paper, gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hariyanto, W., Wulandari, L., Pradjoko, I. et al. Comparison of Vascular Endothelial Growth Factor-A (VEGF-A) Level in Pleural Fluid of Patients with Malignant and Nonmalignant Pleural Effusion. Indian J Surg 83, 132–138 (2021). https://doi.org/10.1007/s12262-020-02204-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-020-02204-z