Abstract
Myeloproliferative neoplasms (MPNs), including polycythemia vera and essential thrombocythemia, are frequently associated with thrombotic complications. Prevention of thrombotic events is thus a primary aim of the current treatment for these disorders. Although it is known that microparticles (MPs), which are small vesicles released from cell membranes and circulate in the blood, directly contribute to thrombosis via their procoagulant activity, potential associations between plasma levels of MPs and the risk of thrombotic events in MPNs have not been reported. In the present study, we characterized plasma levels of MPs and assessed their potential association with the occurrence of thrombotic events in 59 patients with MPNs. Plasma levels of procoagulant MPs expressing tissue factor (TF+ MPs) were significantly higher in patients suffering thrombotic events than in patients without such events (median/μl plasma: 33.8 vs 47.2, p = 0.02). Among patients who developed thrombotic events, irrespective of patients’ blood counts, TF+ MP were significantly higher in patients without cytoreductive therapy than in those receiving cytoreductive therapy (101.2 vs. 42.5, p < 0.001). These results suggest that elevated levels of TF+ MP may be considered as a novel surrogate marker for thrombotic events in MPN patients. Further studies are needed to clarify the mechanism involved.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myeloproliferative neoplasms (MPNs) are clonal disorders of hematopoietic stem cells characterized by the proliferation of multiple myeloid lineages [1]. These neoplasms are etiologically linked to a somatic mutation in JAK2 gene (JAK2V617F), which is found in about 90% of patients (pts) with polycythemia vera (PV) and in about 50% of essential thrombocythemia (ET) and primary myelofibrosis (PMF) [1]. Notably, in a large proportion of JAK2V617F-negative PV pts, mutations in exon 12 of JAK2 gene have been also found [2]. Overall, the aberrant activation of the JAK-STAT pathway leads to the cytokine-independent uncontrolled cell proliferation typical of these neoplasms [3]. On the other hand, somatic mutations in the endoplasmic reticulum chaperone gene (CALR) are detectable in a majority of MPN pts with non-mutated JAK2 [4, 5], and in a small proportion of MPN pts, somatic mutations in MPL gene have been also reported [6, 7]. In the majority of pts, these mutations (JAK2, CALR, and MPL) are mutually exclusive, indicating that the aberrant activation of signal pathways associated with the mutated genes is implicated in the pathogenesis of these disorders.
Hemorrhagic events or thrombotic complications, including arterial or venous thromboses, sometimes appearing in unusual sites, are frequently observed in pts with MPNs with these complications being often the initial event leading to the diagnosis of these neoplasms [8]. It is estimated that after diagnosis, the yearly incidence of thrombotic events in MPN pts may range from approximately 1–10% [8]. As a result, the prevention of thrombotic complications, especially in PV and ET pts, constitutes one of the primarily aims of the current therapeutic approaches of MPNs [9]. Therefore, the identification of clinical, laboratory, or genetic biomarkers associated with the development of thrombotic events is clinical relevant in MPN pts.
Various studies have identified clinical features such as age (>60 years), history of thrombosis, and cardiovascular risk factors as predictors of thrombosis in MPN pts [8, 10, 11] and elevated levels of γ-glutamyl transferase associated with splanchnic thrombosis in MPN pts [12]. In addition, the presence of JAK2V617F and its allele burden has been reported to be predictors of thrombotic and hemorrhagic complications in MPN pts [8, 10]. In contrast, neither mutation of MPL nor CALR is associated with an increased risk of thrombosis [13, 14]. Despite recent advances in understanding the factors that may contribute to the development of thrombotic events, the identification of pts at higher risk for developing thrombosis who may benefit from antithrombotic therapy remains a challenge.
Microparticles (MPs) are circulating small vesicles released from the membranes of activated platelets, endothelial cells, leucocytes, and erythrocytes. They mediate cell–cell communication by transferring a cargo of cell surface receptors, mRNAs, and microRNAs from the cell of origin to target cells [15]. In addition, MPs bind and fuse to the plasma membrane of the target cells, thereby being engulfed [16]. MPs play some roles in inflammation and angiogenesis, and contribute to the pathogenesis of the thrombotic phenomena through their procoagulant activities [17, 18]. Although a few studies have reported that elevated levels of MPs are frequently detectable in MPN pts, no studies have tested the clinical relevance of increased MPs levels, particularly their potential association with the risk of coagulability [19, 20], and thus, it is currently unknown whether the serum levels of MPs in MPN pts are, indeed, associated with the occurrence of thrombotic events in MPN pts.
This study, therefore, characterized the circulating MPs in the plasma of MPN pts and analyzed the potential association between MPs levels with the risk of thrombotic events in MPN pts. Our data revealed that plasma levels of procoagulant MPs (PCMPs), particularly those positive for tissue factor (TF+ MPs), were significantly higher in pts who suffered thrombotic events than in pts without thrombotic events, suggesting that plasma MPs may represent a novel risk factor for thrombosis in MPNs.
Materials and methods
Sample population
In this observation study, we analyzed clinical courses and genetic characteristics of Philadelphia-negative MPN pts who were followed-up at Kindai University Hospital or at Kindai University Nara Hospital from June 2015 to March 2016. The clinical data of 59 pts diagnosed as having PV (n = 17), ET (n = 37), PMF (n = 2), or secondary MF (2nd MF) (n = 3) according to the revised World Health Organization 2008 criteria were collected from the medical records. The pts’ characteristics are presented in Table 1. Genomic DNA and plasma were collected and subjected to assays for genetic mutations and MPs, respectively. Healthy control (CTL) subjects were collected from 8 males and 4 females, aged 26–54 years, without the previous anti-inflammatory or antithrombotic medication (n = 12). This study was approved by the Ethics Committee of Kindai University, and pts provided written informed consent.
Blood sampling and routine laboratory assays
Blood samples were obtained at diagnosis or during their clinical courses. Venous blood was drawn from a large antecubital vein using a 21-gauge needle. First, 3 ml of blood was collected into an EDTA (ethylenediaminetetraacetic acid)-2K Insepack™ II-D tube (Sekisui medical, Tokyo, Japan) for complete blood count (CELL-DYN Sapphire, Abbott Laboratories, Abbott Park, IL, USA). Afterwards, 1.8 ml of blood was collected into 3.2% sodium citrate Insepack™ II-W tube (Sekisui medical) for analysis of MPs and for general laboratory tests of the coagulation and fibrinolysis.
Plasma preparation
Isolation of MPs for flow cytometric analyses was performed as described previously [21]. In brief, platelet poor plasma (PPP) was obtained from sodium citrate-anticoagulated blood by centrifugation at 5000g at 24 °C for 15 min without centrifuge brake. To collect MPs, 600 µl of PPP was centrifuged at 17,000g at 20 °C for 3 min and the supernatant was removed. MP pellet was then resuspended in 900 µl of diluted Annexin V buffer (BD bioscience, Franklin Lakes, NJ, USA).
Quantification and characterization of MPs by flow cytometry
Quantification of MP numbers and their phenotypic characterization were conducted by flow cytometry (FACS CantoII, BD bioscience), as previously described [16]. Briefly, MP size gate was set between 200 and 1000 nm using Megamix® beads (BioCytex, Stago, Asnieres, France). Total amount of MPs were defined as all events falling within the MP gate. To count the numbers of MPs, aliquot of resuspended MP pellet (100 µl) was added to Megamix bead (100 µl), followed by counting up to 2000 of 0.5 µl beads component of Megamix (total absolute count of MP = event in region except beads/2000 event of 500 nm beads). The origin of MPs was determined by flow cytometry using the cell-specific monoclonal antibodies as follows: fluorescein isothiocyanate (FITC)-labeled anti-CD41a (HIP8) for platelets, anti-CD146-FITC (P1H12) for endothelial cells, and anti-CD45-FITC (2D1) for leukocytes (BD bioscience). Annexin V (ANV) and TF on the surface of MPs were detected by allophycocyanin (APC)-labeled annexin V and phycoerythrin (PE)-labeled anti-CD142 antibody (HTF-1), respectively (BD bioscience).
Genetic mutation analysis
Genomic DNA was purified from peripheral blood samples using Wizard® Genomic DNA Purification Kit (Promega, Madison, WI). Mutations in JAK2, MPL, and CALR were detected with a next-generation sequencer (NGS), Ion Torrent PGM™ (Thermo Fisher Scientific, Waltham, MA, USA). The PCR primers were designed using Ion Ampliseq™ designer v.3.4 (Thermo Fisher Scientific). Sequencing of CALR was performed as previously described [4].
Thrombin generation assay
To quantify the procoagulant activity of MPs, we performed thrombin generation assay. The amount of thrombin formed in plasma upon re-calcification was measured using a modified thrombin generation test [22, 23]. In brief, PPP samples were defibrinated using reptilase (ZERIA Pharmaceutical, Tokyo, Japan) followed by incubation for 30 min at 37 °C. The clots were removed by centrifugation. Chromogenic substrate for thrombin S-2238 (Chromogenix, Instrumentation Laboratory, Orangeburg, NY) and CaCl2 were added to defibrinated samples, and then, the change of absorbance at 405 nm was assessed using an Envision plate reader (Wallace, 1420 ARVO MX-2, Turku, Finland). The dynamic optical density was taken to yield a thrombin generation curve. The amount of thrombin generation was calibrated to thrombin activity using thrombin (Wako Pure Chemical Industries, Osaka, Japan).
Statistical analysis
Data analysis was carried out using the EZR software [24]. Quantitative variables were described as range, median, and standard deviation. Qualitative variables were described as number and percent. To compare parametric quantitative variables between two groups, Student’s t test was applied. Spearman’s rank correlation coefficient and multiple regression analysis were employed to assess the relationship between PCMPs and clinical and laboratory variables. Univariate and multivariate analyses of variance with Bonferroni’s correction for multiple comparisons were employed to compare means among groups for normally distributed variables. Receiver-operating characteristic (ROC) curves were prepared by plotting the sensitivity vs. specificity, and the area under the curve (AUC) and the 95% confidence interval (CI) of the AUC for the levels of MPs were calculated. A p value of <0.05 was considered significant in all analyses.
Results
Clinical and laboratory features
The baseline characteristics of 59 MPN pts, including 17 PV pts, 37 ET pts, 2 PMF pts, and 3 2nd MF pts, are summarized in Table 1. MPN pts consisted of 21 men and 38 women with a median age of 68 years ranging from 30 to 97. Hb levels ranged from 7.9 to 22.8 g/dl with median of 15.5 g/dl in PV pts (Hb level 7.9 g/dl was observed in one pt referred to our hospital due to gastrointestinal bleeding). Plt count ranged from 36.7 × 104 to 106.8 × 104/μl with median of 68.8 × 104/µl in ET pts. Among 17 PV pts, phlebotomy was conducted in 6 pts (35.3%), and hydroxyurea (HU) was given into 9 pts (52.9%). Among the 37 pts with ET, 19 pts (51.4%) were treated with HU, 10 pts (27%) were with anagrelide, and 11 pts (29.7%) were not treated. Among the three pts with 2nd MF, one pt was treated with the JAK2 inhibitor, ruxolitinib. The risk of thrombosis in the pts studied was calculated according to the standard risk classification using age ≥60 years and previous thrombosis as criterion. Thus, among the 17 pts with PV, 13 pts (56.4%), two pts (11.8%), and two pts (11.8%) were classified as high, intermediate, and low risks, respectively, while 30 (81.1%), five (13.5%), and two (5.4%) of the 37 pts with ET were identified to have high, intermediate, and low risks, respectively.
Thrombotic and hemorrhagic events
Among the 59 MPN pts studied, 22 pts (37.3%) experienced thrombotic events prior to diagnosis and/or the following observational period (7 pts with PV, 13pts with ET, and 2 pts with 2nd MF) (Table 1). The most frequent type of thrombotic event was cerebral infarction (18.6%), followed by angina pectoris and myocardial infarction (6.8 and 5.1%, respectively). The frequency of each thrombotic event was roughly the same among PV and ET groups. Of note, in PV pts, all thrombotic events occurred prior to or at diagnosis and, therefore, no one was receiving prophylaxis for thrombosis before the events occurred. Among the 13 thrombotic events observed in ET pts, nine events (69.2%) occurred prior to or at diagnosis, while four events (30.8%) occurred after diagnosis (Table 2).
On the other hand, three pts (5.1%) (two with PV and one with ET) experienced hemorrhagic complications in gastrointestinal tract, subcutaneous tissues, or intracranial regions, while none of the pts with PMF or 2nd MF experienced bleeding events (Table 1). Of the two pts with PV complicated with bleeding (UPN 11, 12), one was being treated with aspirin, while the other was not. One pt with ET (UPN 46) accompanied by bleeding was treated with warfarin (Table 2).
Genetic mutations of MPN pts
We next examined JAK2, MPL, and CALR mutations in MPN pts using NGS and direct sequencing. Among the 59 pts studied, JAK2V617F was found in 48 pts (81.4%). According to the MPN subtypes, mutations were observed in 17/17 (100%), 29/37 (78.4%), 1/2 (50%), and 1/3 (33.3%) pts with PV, ET, PMF, and 2nd MF, respectively (Table 3). CALR mutations were detected in 2 ET pts (5.4%; type 1 in 2 pts,) and 2/3 2nd MF pts (66.7%; type 1 in 1 pts; type 2 in 1 pts). There was no MPL mutated pts. Consistent with the previous publications, JAK2 and CALR mutations were mutually exclusive.
Number and phenotypic characterization of microparticles
Next, we analyzed MPs in 59 MPN pts, whose clinical characteristics are summarized in Table 1. As shown in Fig. 1a, there was no significant difference in the total amounts of MPs and ANV+ MPs between MPN pts and healthy CTLs (n = 12). Similarly, no difference was observed in the levels of total MPs among subtypes (PV, ET, PMF, and 2nd MF) of MPN (data not shown). On the other hand, the levels of TF+ MPs in MPN pts were higher than those in CTLs, although this difference was not statistically significant (p = 0.09). Importantly, the levels of total MPs in pts treated with cytoreductive agents [Tx(+)] were not statistically significant than those in pts not treated with cytoreductive therapy [Tx(−)]; however, when comparisons were done based on the levels of specific MP, namely the levels of PCMP, such as ANV+ MPs and TF+ MPs, we observed significant decreases in the levels of PCMP microparticles after cytoreductive treatments (median ANV+ MPs/μl plasma: Tx(−) 4.89 × 102 vs. Tx(+) 2.16 × 102, p < 0.05; median TF+ MPs: Tx(−)/μl plasma 46.3 vs. Tx(+) 37.9, p < 0.05) (Fig. 1a), indicating that cytoreductive therapy may be associated with a decrease in the risk of thrombotic events mediated by PCMPs.
Comparison of plasma MP levels between MPN patients and healthy controls. a Plasma levels or total MPs (left panel) and procoagulant MPs (middle and right panels) in healthy control individuals (n = 12) and MPN patients treated with cytoreductive drugs [Tx(+) n = 37] or not treated with cytoreductive drugs [Tx(−) n = 22] are indicated. Boxes and whiskers indicate median and (interquartile) range. Horizontal lines indicate median levels. p values are according to Student’s t test. CTL healthy control, NS not significant; *p < 0.05. b Plasma levels or total MPs (left panel) and procoagulant MPs (middle and right panels) in ET patients treated with hydroxyurea (n = 15) or with anagrelide (n = 6) are indicated. Boxes and whiskers indicate median and (interquartile) range. Horizontal lines indicate median levels. p values are according to Student’s t test. ANV annexin V, TF tissue factor, HU hydroxyurea, NS not significant
We next assessed the levels of MPs according to the cytoreductive therapy utilized. In treated with either anagrelide or HU (Fig. 1b, left and middle panel), however, pts treated with anagrelide tended to have lower levels of TF+ MPs than those treated with HU, though this difference was not statistically significant (p = 0.06) (Fig. 1b, right panel). Interestingly, plasma levels of total MPs were significantly lower in pts receiving anticoagulant therapy with warfarin (n = 8) in comparison with levels in pts not receiving anticoagulants (n = 51) (p = 0.02), although the impact of these findings is unknown given the small number of pts receiving anticoagulants (8 vs. 51) (Supplementary Fig. 1). The biological and clinical relevance of this finding may be compromised by the fact that the levels of PCMPs (ANV+ and TF+) in pts receiving anticoagulants in comparison with those in pts without anticoagulants were not statistically significant (Supplementary Fig. 1). Therefore, it is currently unknown if anticoagulants are actually capable of reducing the levels of MPs.
Phenotypic characteristics of microparticles
The phenotypic characterization of PCMPs showed that the majority of ANV+ MPs (68.2%) were CD41a+ platelets derived (PDMP) in MPN pts not treated with cytoreductive therapy, while this fraction was less than 30% in CTLs (Fig. 2). Notably, the proportion of ANV+ MPs that were CD41a+ (PDMP) in MPN pts decreased after cytoreductive therapy (44.7%), although these changes were not statistical significant. The rest of ANV+ MPs in both untreated MPN pts and CTLs consisted of leukocyte (positive for CD45) and endothelial cell (positive for CD146)-derived MPs. Because CD146 is also expressed on MPs derived from lymphocytes, we evaluated the expression of CD45 on CD146+ PCMPs. As a result, CD45 and CD146 double positive PCMPs were hardly detected in both MPN cases and CTLs, and hence, the majority of CD146+ PCMPs were thought to be derived from endothelial cells. On the other hand, about 50% of TF+ MPs were of unknown origin (others) in MPN pts, either untreated (46.5%) or treated (49.5%) with cytoreductive therapy; an important proportion of TF+ MPs (41.3%) were EDMP in CTLs, which was almost twice that that observed in MPN pts (Fig. 2). It must be noted that although the cytoreductive therapy significantly reduced the plasma levels of PCMPs in MPN pts (Fig. 1b), the phenotypic characteristic of PCMP was not significantly modified in response to cytoreductive treatment (Fig. 2).
Phenotypic analysis of MPs in MPN patients. Phenotypic characterization of procoagulant MPs in healthy controls (n = 12), MPN patients receiving cytoreduction therapy (n = 37), or untreated patients (n = 22) was performed by flow cytometry analysis. PS phosphatidylserine, TF tissue factor, PDMP platelet-derived MP, LDMP leukocyte-derived MP, EDMP endothelial cell-derived MP
Effect of PCMPs on thrombin generation
To assess the functional procoagulant activity of MP, we quantified thrombin generation by monitoring cleavage kinetics of thrombin chromogenic substrate in 6 pts and 6 healthy CTL plasma samples (Fig. 3A). Before the experiment, we confirmed that defibrination of plasma did not affect the content of MPs in PPP (data not shown). Then, we assessed correlation between the amount of TF+ MPs and (a) lag time, (b) peak value of thrombin generation, (c) endogenous thrombin potential, and (d) time to peaks (Fig. 3B). There was no correlation between plasma levels of total MPs or ANV+ MPs and these indicators (data not shown); however, we observed an apparent correlation between the levels of TF+ MPs with peak value (r = 0.583, p = 0.0468), and a close correlation with time to peak (r = −0.508, p = 0.0918 (Fig. 3C). Although the biological relevance of these observations is unclear, since the analysis may have been skewed by the presence of an outlier sample.
Effect of procoagulant MPs on thrombin generation in vitro. A Representative colorimetric curves showing the cleavage kinetics of a thrombin chromogenic substrate (S-2238) in a sample after re-calcification. B Derivative of the colorimetric curve (“thrombograms”) corresponding to date shown in a. Parameters of the thrombogram. a Lag time (min), b peak height (unit), c endogenous thrombin potential (area under the curve) (unit × min), d time to peak (min). The change of thrombin generation that converts to that of thrombin activity (unit) is displayed. C Correlations analysis between total amount of TF+ MPs and thrombogram parameters, peak value (left) and time to peak (right) in PPP of 6 MPN pts (black circle), and 6 healthy controls (black up-pointing triangle). Linear regression analysis was used to test the association between continuous variables. The amount of TF+ MPs is plotted against each thrombogram parameter. Regression parameters (r) and significance values (p) are shown
Correlation between peripheral blood counts and PCMP levels
Next, we evaluated the relationship between common hematological parameters (Hb, WBC, and Plt counts) and total PCMP levels in MPN pts. As shown in Supplementary Fig. 1, there was no a statistically significant relationship between the total PCMP levels and the hematological parameters (Supplementary Fig. 2), suggesting that PCMPs were elevated independently of the excessive blood cells that are typical in MPN pts. In addition, there was no a statistically significant relationship between the PCMP levels and hemostatic and fibrinolytic parameters (e.g., PT, APTT, and vWF activity) (data not shown).
Correlation of PCMP levels with previously reported risk factors for thrombotic events in MPNs
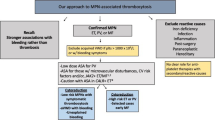
We next examined the impact of ANV+ and TF+ MP levels in MPN pts in association with previously reported risk factors, including age, JAK2 mutation, and thrombosis history [8, 10]. Both plasma levels of ANV+ and TF+ MP were not influenced by age, but levels of these PCMPs were higher in pts with JAK2 mutation, although it was not statistically significant (Fig. 4a, b). Importantly, the levels of TF+ MPs but not those of ANV+ MPs were significantly higher in MPN pts who developed thrombotic events than in those pts who did not have thrombosis (CVE) (n = 59; p = 0.02). These results were more obvious when the analysis was performed in MPN pts not treated with cytoreductive therapy (n = 22, p = 0.01).
Correlation analysis between procoagulant MP values and predictors of thrombosis in MPN patients. The association among plasma levels of procoagulant MP (PCMPs) with age (a), JAK2 mutation status (b), or the development of thrombotic events (CVE) (c) in MPN patients was analyzed by Student’s t test. Boxes and whiskers indicate median and (interquartile) range. Horizontal lines indicate median levels. NS not significant
Next, we tried to determine the cut-off value of MP level that best indicates the risk of thrombosis in accordance with the thrombotic history by ROC analysis. As shown in Fig. 5, in comparison with total MPs and levels of ANV+ MPs, the levels of TF+ MPs correlated better with the pts’ thrombotic history. The determined that a cut-off value of ≥84.7/µl best proposed cut-off value of TF+ MPs accurately predicted thrombosis with a sensitivity 100% and a specificity of 71.4%, and the area under the ROC curve 0.917 with 95% confidence interval from 78.7 to 100%.
Evaluation of the levels of TF+ MPs effectiveness as a potential biomarker for predicting thromboembolism in MPN patients in the practical setting. To determine optimal cut-off values for the levels of MPs, receiver-operating characteristic (ROC) curves were used. ROC analysis of accuracies of levels of TF+ MPs for the presence of thrombotic history. (Asterisk) Indicates cut-off value of each. AUC area under the curve, CI confidence interval
We then assessed the impact of TF+ MPs ≥84.7 on thrombotic events with previously reported risk factors. Univariate analysis demonstrated that a documented cardiovascular risk together with a TF+ MPs ≥84.7 were significant risk factors for thrombosis (n = 43, p = 0.02 and n = 5, p = 0.02, respectively), while none of the other previously reported (classical risk factors) factors such as gender, age ≥60, and JAK2 mutation showed statistical significant association with thrombosis in the practical setting (Table 4). In multivariate analysis, however, TF+ MPs ≥84.7 lost the statistical significance (n = 5, p = 0.12) probably due to the relatively small number of pts included in the analysis. TF+ MPs ≥84.7, however, retained a high hazard ratio (HR 4.37) compared with other risk factors.
Discussion
In this study, we tested the hypothesis that plasma levels of MPs can be a biomarker of thrombosis risk in MPN pts. Although we have investigated a relatively small number of pts (n = 59), our data revealed some findings that we believe are of clinical relevance. The plasma levels of TF+ MP were significantly higher in pts who suffered thrombotic events than in pts without thrombotic events, suggesting that plasma MPs may represent a novel risk factor for thrombosis in MPNs. Notably, in this study, 41.2% of PV and 35.1% of ET pts experienced thrombosis, which are slightly higher rates than those reported by the previous studies (8–38.6 and 8–30.7% in PV and ET, respectively), in western countries [25, 26]. Although the reason for the high frequency of thrombosis in our pts is unknown, it is likely that specific characteristics of some of the pts in this study including various pts that were undiagnosed for a long period of time may have contributed to the increased frequency of thrombotic events.
The prevention of thrombotic and/or bleeding events is a crucial component for the management of PV and ET pts and, therefore, properly classifying pts in the appropriate risk category is of crucial importance for therapeutic purposes [9, 27]. Age and thrombotic history represent the most important risk factors for thrombosis in PV and ET pts [5,6,7,8] and other risk factors such as JAK2V617F status have emerged as novel important risk factors for thrombosis in PV and ET pts. Importantly, all of these markers (age, thrombotic history, and JAK2V617F) are present at the moment of diagnosis and are the factors which we cannot virtually modify by treatment or intervention. Several guidelines recommend to control Ht about 45% in PV pts and number of platelet counts ≤400 × 103/µl in ET pts [28]. In contrast to these guidelines, it was recently reported that the frequency of thrombotic events did not decrease even if platelet counts were reduced to ≤400 × 103/µl in ET pts [29].
The pathogenic role of TF+ MPs in triggering venous thrombosis is further supported by the fact that phospholipids present on MPs strongly increase their procoagulant activity [30]. Consistent with data from preclinical studies, high levels of MPs have been proposed to be biomarker of vascular injury and a potential predictor of cardiovascular mortality in pts with atherothrombotic diseases [31]. In addition, a prospective analysis recently demonstrated that elevated plasma levels of TF+ MPs were accurately predicted the risk of venous thromboembolism in pts with newly diagnosed pancreatic biliary cancer [32]. Consistent with this notion, our in vitro thrombin generation assay, using pts-derived samples, suggests that increased circulating TF+ MPs may functionally contribute to the procoagulant activity of circulating MPs in MPN pts. The previous studies proposed that phosphatidylserine exposing erythrocytes and platelets, as well as lactadherin+ MPs were crucial factors for the development of thrombotic events in PV pts [33]. Notably, in our study, erythrocytes and platelets counts were not statistically associated with total PCMP levels, suggesting that elevated levels of PCMPs contribute independently to the hypercoagulable status in MPN pts.
In the present study, we quantified circulating MPs with platelet and endothelial markers indicating their activation by flow cytometric analysis, which is a simple and reliable method [19, 20]. As a result, there was no significant difference in the number of total MPs between MPN pts and healthy CTLs. However, we found that PCMP levels were significantly higher in pts without cytoreductive therapy. These findings are largely consistent with a previous study reporting that ET pts had a higher number of MPs with platelet and endothelial markers than healthy subjects and that MPs from ET pts were associated with increased thrombin generation [19]; however, in this study, cytoreductive treatment did not affect the number of TF+ MPs in ET pts. This appears to be in discrepancy with our data showing that cytoreductive therapy resulted in a significant decrease in the levels of circulating PCMPs in MPN pts. Interestingly, we also found that anagrelide-treated pts showed a tendency to have lower levels of TF+ MPs than HU-treated pts, although it was not statistically significant, probably due to the small number of anagrelide-treated pts in this study (n = 6). One may speculate that cytoreductive therapy with HU as monotherapy is ineffective for reducing PCMPs and consequently preventing thrombotic events in PV and ET pts. This speculation appears to be supported by the above described result that platelet count ≤400 × 103/µl mainly by HU was not sufficient to prevent thrombosis in ET pts. Anagrelide is a phosphodiesterase 3 inhibitor originally developed as a drug to inhibit platelet activity. This compound hardly influences general platelet activity at therapeutic doses for ET pts [34] and inhibitory effects on platelet function may lead to a decrease in the levels of TF+ MPs in ET pts. Of note, in our study, two out of six pts treated with anagrelide still showed relatively high levels of TF+ MPs which may suggest the coexistence of other unidentified factors for thrombosis in some MPN pts. Further studies, particularly prospective ones, testing the potential effects of anagrelide on reducing levels of TF+ MPs and in the prevention of thrombotic events in ET pts, are required to generate new therapeutic strategies.
Older age, thrombosis history, cardiovascular risk, and JAK2V617F are largely associated with increased risk for thrombosis in MPN pts and these factors are, therefore, utilized in most risk stratification guidelines. Notably, in a previous report, these risk factors did not affect the TF+ MPs in ET pts [35]. However, in the present study, high levels of TF+ MPs (cut-off value ≥84.74) were identified as a risk factor of thrombosis in MPNs pts by the ROC analysis. Using this cut-off value, we found that only TF+ MPs ≥84.74 and cardiovascular risk were significant risk factors for thrombotic events in MPN pts by univariate analysis, whereas none of the “classical risk factors” (older age, thrombosis history, and JAK2V617F mutation) was an independent risk factor in the practical setting in our model. Because the number of the pts analyzed in this study was relatively small, compared with the previous studies conducted to identify risk factors for thrombosis, we believe that our result does not deny the significance of the “classical risk factors”. This may be supported by the fact that the statistical significance of TF+ MPs ≥84.74 was observed in the univariate analysis but not in the multivariate analysis (p = 0.120). We believe the failure of our multivariate analysis to confirm the relevance of TF+ MPs ≥84.74 as a risk factor for thrombosis was at least in part due to the small number of pts analyzed in this study.
In conclusion, levels of procoagulant TF+ MPs were significantly higher in MPN pts with thrombotic events than in pts without thrombosis. In pts with thrombosis, TF+ MPs were significantly reduced by cytoreduction therapy, especially by anagrelide. Elevated levels of TF+ MPs, (≥84.74), were a risk factor for thrombosis in MPN pts in a univariate analysis, whereas its significance was lost in multivariate analysis probably due to the small number of pts analyzed in this study. Further prospective studies are needed to generate definitive conclusions and thus to elucidate the clinical significance of elevated TF+ MPs in MPN pts.
References
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, Bloomfield CD, Cazzola M, Vardiman JW. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–405.
Schnittger S, Bacher U, Haferlach C, Geer T, Müller P, Mittermüller J, Petrides P, Schlag R, Sandner R, Selbach J, et al. Detection of JAK2 exon 12 mutations in 15 patients with JAK2V617F negative polycythemia vera. Haematologica. 2009;94(3):414–8.
Milosevic JD, Kralovics R. Genetic and epigenetic alterations of myeloproliferative disorders. Int J Hematol. 2013;97(2):183–97.
Nangalia J, Massie CE, Baxter EJ, Nice FL, Gundem G, Wedge DC, Avezov E, Li J, Kollmann K, Kent DG, et al. Somatic CALR mutations in myeloproliferative neoplasms with nonmutated JAK2. N Engl J Med. 2013;369(25):2391–405.
Imai M, Araki M, Komatsu N. Somatic mutations of calreticulin in myeloproliferative neoplasms. Int J Hematol. 2017;105(6):743–7.
Ma W, Zhang X, Wang X, Zhang Z, Yeh CH, Uyeji J, Albitar M. MPL mutation profile in JAK2 mutation-negative patients with myeloproliferative disorders. Diagn Mol Pathol. 2011;20(1):34–9.
Kim SY, Im K, Park SN, Kwon J, Kim JA, Lee DS. CALR, JAK2, and MPL mutation profiles in patients with four different subtypes of myeloproliferative neoplasms: primary myelofibrosis, essential thrombocythemia, polycythemia vera, and myeloproliferative neoplasm, unclassifiable. Am J Clin Pathol. 2015;143(5):635–44.
Casini A, Fontana P, Lecompte TP. Thrombotic complications of myeloproliferative neoplasms: risk assessment and risk-guided management. J Thromb Haemost. 2013;11(7):1215–27.
Barbui T. How to manage thrombosis in myeloproliferative neoplasms. Curr Opin Oncol. 2011;23(6):654–8.
Barbui T, Finazzi G, Carobbio A, Thiele J, Passamonti F, Rumi E, Ruggeri M, Rodeghiero F, Randi ML, Bertozzi I, et al. Development and validation of an International Prognostic Score of thrombosis in World Health Organization-essential thrombocythemia (IPSET-thrombosis). Blood. 2012;120(26):5128–33 (quiz 5252).
Carobbio A, Thiele J, Passamonti F, Rumi E, Ruggeri M, Rodeghiero F, Randi ML, Bertozzi I, Vannucchi AM, Antonioli E, et al. Risk factors for arterial and venous thrombosis in WHO-defined essential thrombocythemia: an international study of 891 patients. Blood. 2011;117(22):5857–9.
Görtzen J, Hunka LM, Vonnahme M, Praktiknjo M, Kaifie A, Fimmers R, Jansen C, Heine A, Lehmann J, Goethert JR, et al. γ-Glutamyl transferase is an independent biomarker of splanchnic thrombosis in patients with myeloproliferative neoplasm. Medicine (Baltimore). 2016;95(20):e3355.
Barbui T, Thiele J, Passamonti F, Rumi E, Boveri E, Ruggeri M, Rodeghiero F, d’Amore ES, Randi ML, Bertozzi I, et al. Survival and disease progression in essential thrombocythemia are significantly influenced by accurate morphologic diagnosis: an international study. J Clin Oncol. 2011;29(23):3179–84.
Rumi E, Pietra D, Ferretti V, Klampfl T, Harutyunyan AS, Milosevic JD, Them NC, Berg T, Elena C, Casetti IC, et al. JAK2 or CALR mutation status defines subtypes of essential thrombocythemia with substantially different clinical course and outcomes. Blood. 2014;123(10):1544–51.
Nomura S, Niki M, Nisizawa T, Tamaki T, Shimizu M. Microparticles as Biomarkers of Blood Coagulation in Cancer. Biomark Cancer. 2015;7:51–6.
Geddings JE, Mackman N. Tumor-derived tissue factor-positive microparticles and venous thrombosis in cancer patients. Blood. 2013;122(11):1873–80.
Lacroix R, Dubois C, Leroyer AS, Sabatier F, Dignat-George F. Revisited role of microparticles in arterial and venous thrombosis. J Thromb Haemost. 2013;11(Suppl 1):24–35.
Owens AP, Mackman N. Microparticles in hemostasis and thrombosis. Circ Res. 2011;108(10):1284–97.
Trappenburg MC, van Schilfgaarde M, Marchetti M, Spronk HM, ten Cate H, Leyte A, Terpstra WE, Falanga A. Elevated procoagulant microparticles expressing endothelial and platelet markers in essential thrombocythemia. Haematologica. 2009;94(7):911–8.
Kissova J, Ovesna P, Bulikova A, Zavřelova J, Penka M. Increasing procoagulant activity of circulating microparticles in patients with Philadelphia-negative myeloproliferative neoplasms: a single-centre experience. Blood Coagul Fibrinolysis. 2015;26(4):448–53.
Dey-Hazra E, Hertel B, Kirsch T, Woywodt A, Lovric S, Haller H, Haubitz M, Erdbruegger U. Detection of circulating microparticles by flow cytometry: influence of centrifugation, filtration of buffer, and freezing. Vasc Health Risk Manag. 2010;6:1125–33.
Hemker HC, Al Dieri R, De Smedt E, Béguin S. Thrombin generation, a function test of the haemostatic-thrombotic system. Thromb Haemost. 2006;96(5):553–61.
Zubairova LD, Nabiullina RM, Nagaswami C, Zuev YF, Mustafin IG, Litvinov RI, Weisel JW. Circulating microparticles alter formation, structure, and properties of fibrin clots. Sci Rep. 2015;5:17611.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48(3):452–8.
Price GL, Davis KL, Karve S, Pohl G, Walgren RA. Survival patterns in United States (US) medicare enrollees with non-CML myeloproliferative neoplasms (MPN). PLoS One 2014;9(3):e90299.
Hultcrantz M, Wilkes SR, Kristinsson SY, Andersson TM, Derolf Å, Eloranta S, Samuelsson J, Landgren O, Dickman PW, Lambert PC et al. Risk and Cause of Death in Patients Diagnosed With Myeloproliferative Neoplasms in Sweden Between 1973 and 2005: A Population-Based Study. J Clin Oncol. 2015;33(20):2288–95.
Borowczyk M, Wojtaszewska M, Lewandowski K, Gil L, Lewandowska M, Lehmann-Kopydłowska A, Kroll-Balcerzak R, Balcerzak A, Iwoła M, Michalak M et al. The JAK2 V617F mutational status and allele burden may be related with the risk of venous thromboembolic events in patients with Philadelphia-negative myeloproliferative neoplasms. Thromb Res. 2015;135(2):272–80.
Tefferi A. Myeloproliferative neoplasms: a decade of discoveries and treatment advances. Am J Hematol. 2016;91(1):50–8.
Falchi L, Bose P, Newberry KJ, et al. Approach to patients with essential thrombocythaemia and very high platelet counts: what is the evidence for treatment? Br J Haematol. 2017;176(3):352–64.
Mallat Z, Benamer H, Hugel B, Benessiano J, Steg PG, Freyssinet JM, Tedgui A. Elevated levels of shed membrane microparticles with procoagulant potential in the peripheral circulating blood of patients with acute coronary syndromes. Circulation 2000;101(8):841–43.
Morel O, Hugel B, Jesel L, Lanza F, Douchet MP, Zupan M, Chauvin M, Cazenave JP, Freyssinet JM, Toti F. Sustained elevated amounts of circulating procoagulant membrane microparticles and soluble GPV after acute myocardial infarction in diabetes mellitus. Thromb Haemost. 2004; 91(2):345–53.
Bharthuar A, Khorana AA, Hutson A, Wang JG, Key NS, Mackman N, Iyer RV. Circulating microparticle tissue factor, thromboembolism and survival in pancreaticobiliary cancers. Thromb Res. 2013;132(2):180–4.
Tan X, Shi J, Fu Y, Gao C, Yang X, Li J, Wang W, Hou J, Li H, Zhou J. Role of erythrocytes and platelets in the hypercoagulable status in polycythemia vera through phosphatidylserine exposure and microparticle generation. Thromb Haemost. 2013;109(6):1025–32.
Bellucci S, Legrand C, Boval B, Drouet L, Caen J. Studies of platelet volume, chemistry and function in patients with essential thrombocythaemia treated with Anagrelide. Br J Haematol. 1999;104(4):886–92.
Cacciola RR, Francesco ED, Giustolisi R, Cacciola E. Effects of anagrelide on platelet factor 4 and vascular endothelial growth factor levels in patients with essential thrombocythemia. Br J Haematol. 2004;126(6):885–6.
Acknowledgements
This work was supported by the Osaka Medical Research Foundation for Intractable Diseases, Osaka, Japan (Grant number 2-20). We thank Ms. Keiko Furukawa (Kindai University) for the excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no relevant conflicts of interest to disclose in this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12185_2017_2302_MOESM1_ESM.pdf
Supplemental Fig. 1 Effects of anticoagulant therapy on plasma MP levels in MPN patients. The association among plasma levels of MP with anticoagulant therapy in MPN patients was analyzed by Student’s t test. Boxes and whiskers indicate median and (interquartile) range. Horizontal lines indicate median levels. NS, not significant. Supplemental Fig. 2 Correlations analysis between procoagulant MP values and blood cell counts in MPN patients. Linear regression analysis was used to test the association between continuous variables. No. of MPs is plotted against each blood cell count. Regression parameters (r) and significance values (p) are shown (PDF 486 kb)
About this article
Cite this article
Taniguchi, Y., Tanaka, H., Luis, E.J. et al. Elevated plasma levels of procoagulant microparticles are a novel risk factor for thrombosis in patients with myeloproliferative neoplasms. Int J Hematol 106, 691–703 (2017). https://doi.org/10.1007/s12185-017-2302-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-017-2302-5