Abstract
Purpose of Review
Thrombocytosis is common to all myeloproliferative neoplasms (MPN), including essential thrombocythemia (ET), polycythemia vera (PV), and myelofibrosis. Despite the traditionally held belief amongst many clinicians that thrombocytosis correlates with thrombosis risk, there is little evidence in the literature to support that claim. Herein we critically analyze the literature to better understand the relationship between thrombocytosis and risk of thrombosis in MPN.
Recent Findings
Both retrospective and prospective studies argue against associations between thrombocytosis and risk of thrombosis in patients with ET and PV. Rather, most studies suggest that the presence of extreme thrombocytosis is instead associated with an increased risk of hemorrhagic events, a paradoxical phenomenon with important clinical implications.
Summary
Thrombosis risk has a multifactorial set of etiologies in MPNs. While qualitative abnormalities of the platelets may contribute, associations between platelet quantity and thrombosis risk are weak in MPN patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Case Presentation and Introduction
A 59-year-old female with osteoporosis and incidentally discovered thrombocytosis is urgently referred to hematology clinic by her primary care physician due to concern that she is at imminent risk for a cerebrovascular accident. Apart from mild subjective fatigue, the patient feels well and had recently completed a triathlon. On further questioning, she denies headaches, visual changes, paresthesias, weakness, evidence of erythromelalgia, or history of thrombosis. She does note slight bruising since being started on aspirin by her PCP and is without clinical evidence of splenomegaly on exam.
Laboratory analysis is significant for WBC 6.2 × 109/L, Hgb 13.6 g/dl, and platelets 1185 × 109/L. Her iron studies and inflammatory markers are normal and JAK2 V617F is negative. Her ristocetin activity is 105% and she is ultimately found to have a type 1 CALR mutation and a bone marrow suggestive of essential thrombocythemia. The central question is whether or not her thrombocytosis strongly associates with thrombosis.
The exact definition of thrombocytosis varies in the literature but is generally considered when platelet counts ≥ 400–450 × 109/L. The vast majority (> 90%) of cases of thrombocytosis are reactive or secondary in nature and do not in fact reflect a primary hematologic disorder (primary thrombocytosis). Acute insults may cause transient elevation in platelet counts (i.e., trauma or infection) while more chronic conditions may present with sustained thrombocytosis (i.e., iron deficiency anemia, malignancy, chronic inflammatory conditions). Furthermore, Ruggeri et al. found that ~ 1% of asymptomatic patients in the general population were found to have a platelet count > 400 × 109/L, although platelet counts normalized in > 92% on recheck within 8 months [1]. Although the data is limited, one retrospective study suggested a ~ 1.6% incidence of venous thromboembolic complications in patients with secondary thrombocytosis, although only when in the presence of additional risk factors such as preceding surgery, malignancy, or post-splenectomy. In the absence of additional risk factors, there was no association found between secondary thrombocytosis and thrombosis, regardless of cause [2].
Less than 10% of cases of isolated thrombocytosis actually reflect a primary hematologic condition. The majority of these conditions fall within the spectrum of myeloproliferative neoplasms (MPN) which include essential thrombocythemia (ET), polycythemia vera (PV), and primary myelofibrosis (PMF). These conditions are characterized by clonal proliferation of myeloid stem cells with variable morphologic maturity.
Before analyzing the association between thrombocytosis and thrombosis risk, platelet homeostasis will be briefly reviewed. Platelet production is directly regulated by thrombopoietin (TPO), a hormone predominantly synthesized in the liver. TPO regulates proliferation and differentiation of megakaryocytes in the bone marrow by binding to its receptor, c-Mpl (TPO-R), which is expressed on both the surface of megakaryocytes and circulating platelets. After TPO binds to the extracellular portion of c-Mpl, a signaling cascade is initiated via the JAK-STAT pathway leading to downstream signaling, cell growth, and megakaryopoiesis [3]. Platelet production is thus tightly regulated by the amount of TPO directly delivered to megakaryocytes in the bone marrow. As platelet mass decreases, less TPO is bound to circulating platelets and thus more able to stimulate megakaryocyte proliferation and differentiation in the bone marrow. Conversely, as platelet mass increases, more TPO is sequestered by circulating platelets and less able to stimulate megakaryopoiesis [4].
Philadelphia-negative myeloproliferative neoplasms (MPN), classically including ET, PV, and PMF, are fundamentally characterized by dysregulated myeloid hematopoiesis and increased proliferation of erythroid, megakaryocytic, or granulocytic cells. The molecular pathogenesis of MPN phenotype is most commonly characterized by the presence of a driver mutation in one of the three genes, JAK2, MPL, and CALR. Through differing mechanisms, these mutations lead to constitutive and hyperactive JAK-STAT signaling, ultimately resulting in dysregulated cellular proliferation [5]. The first driver mutation, JAK2-V617F, was first discovered ~ 2005 and occurs in ~ 95% of patients with PV and 50–60% of patients with either ET or PMF [6, 7]. It is characterized by direct overactivation of JAK2 signaling, independent of growth factor, and leads to the development of an MPN phenotype. Activating mutations in MPL occur in 5–8% of patients with ET or PMF and cause TPO-independent activation of c-Mpl due to uninhibited dimerization, constitutive self-activation, and indirect dysregulation of JAK2 signaling [8, 9]. Finally, activating mutations in CALR occur in ~ 25–30% of patients with ET and PMF. Although still unclear, it is thought that pathologic CALR mutations lead to alterations in the structure and charge of calreticulin which specifically activates the TPO receptor and leads to indirect dysregulation of JAK2 signaling. As a result of these mechanisms, any of the MPNs can lead to dysregulated megakaryopoiesis and thrombocytosis.
Essential Thrombocythemia: Examining Correlations Between Thrombocytosis and Thrombosis
Amongst MPNs, essential thrombocythemia (ET) is classically characterized by thrombocytosis, thrombohemorrhagic complications (both venous and arterial), and risk for progressing to myelofibrosis or acute myeloid leukemia (AML) [10••, 11].
The literature reports an incidence rate of thrombosis of 9–22% of patients with ET at time of diagnosis [12,13,14]. Thrombotic manifestations may present clinically as cerebrovascular events, myocardial infarctions, or venous thromboembolic disease and are likely due to qualitative platelet dysfunction.
Despite the nearly universal presence of thrombocytosis in ET, the major risk factors that historically correlate with thrombosis risk are advanced age, history of prior thrombosis, and JAK2 mutational status. Traditionally, the absence or presence of these risk factors helps stratify patients into very low, low, intermediate, or high risk for thrombotic complications and help guide use of cytoreductive therapy with the intent of preventing long-term thrombotic complications.
In current clinical practice, most hematologists aim to reduce platelet counts via cytoreductive therapy in high-risk ET despite multiple observational studies failing to demonstrate a relationship between elevated platelet count and thrombotic risk, either at diagnosis or during follow-up [15]. A prospective multicenter analysis of the PT-1 trial cohort which included 776 patients with essential thrombocythemia found no association between platelet count at diagnosis or follow-up and risk of future thrombotic complications (p = 0.4). Interestingly, the presence of thrombocytosis was instead associated with an increased immediate risk of major hemorrhage (p = 0.001). The authors of this study suggested that cytoreductive therapy should be used to normalize platelet counts but with the goal of minimizing immediate major hemorrhagic complications [15, 16].
Furthermore, another international collaborative study identified 891patients with ET and analyzed the incidence of major thrombotic complications. After a median follow-up of 6.2 years, ~ 12% of patients had experienced either a major arterial (n = 79) or venous (n = 37) thrombotic event with an overall rate of fatal and nonfatal thrombotic events of 1.9% patient-years. Based on the multivariable analysis, a platelet count of ≥ 1000 × 109/L at diagnosis was not associated with an increased risk of arterial or venous thrombotic events. Instead, the presence of “extreme thrombocytosis” (defined as plt ≥ 1000 × 109/L) was independently associated with a lower risk of arterial thrombosis (HR 0.42, p = 0.007) [17]. This finding may reflect the occurrence of acquired von Willebrand disease (aVWD) observed in patients with thrombocytosis and questions the utility of aggressive antiplatelet therapy in low-risk patients with extreme thrombocytosis.
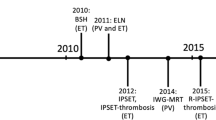
The revised IPSET-thrombosis study reanalyzed retrospective data from 1019 patients with WHO-defined ET initially used to establish International Prognostic Score for Thrombosis in ET (IPSET-thrombosis). This study shifted risk stratification to include age, history of thrombosis, and JAK2 mutation status to identify four risk categories instead of the three-tiered approach in IPSET-thrombosis. These findings were subsequently validated by a retrospective study at Mayo Clinic of 585 patients with WHO-defined ET. Platelet count, yet again, was not found to be an independent risk factor for recurrent thrombosis (HR 1; p = 0.233) [18••, 19••].
In an attempt to limit the potential confounding effects of anti-thrombotic and/or cytoreductive during treatment of Ph-negative MPNs on future thrombotic risk, one study investigated the relationship between prior thrombosis (thrombosis that occurred prior to diagnosis and before treatment; PrTh) and characteristics at diagnosis in 977 thrombocythemic patients with MPN per WHO 2008 criteria. Both univariate and multivariate analyses demonstrated that PrTh rate was significantly related to presence of minor thrombocytosis (defined as plt ≤ 700 × 109/L), leukocytosis (WBC > 10 × 109/L), JAK2 V617F, older age, higher hematocrit (HCT > 45%), and CV risk factors. Interestingly, the highest PrTh rate (33.9%) was associated with the coexistence of minor thrombocytosis and leukocytosis [20•]. More specifically, patients with plt ≤ 700 × 109/L at diagnosis had a prior thrombosis rate of 28% vs 15.8% in those with plt > 700 × 109/L at diagnosis (OR 2.41; p < 0.001). This finding further confirms the hemostatic paradox of thrombocytosis as previously described in the literature, since there was an inverse relationship between thrombosis and thrombocytosis.
Another retrospective study performed univariate and multivariate analyses of thrombosis predictors in 416 ET patients who had been treated with hydroxyurea for at least 12 months. The authors concluded that age and previous thrombosis were independently associated with increased risk of vascular events whereas achievement of complete hematological response per European LeukemiaNet (ELN) did not. In particular, it was noted that rate of major thrombosis in three categories of response per ELN was not related to the achievement of platelet targets less than 400 × 109/L (HR 1.04; p = 0.95) or less than 600 × 109/L (HR 1.05; p = 0.91), indicating that normalization of platelet count did not reduce risk of major vascular events [21].
In accordance with the above findings, another retrospective study evaluated clinically relevant outcomes based on ELN response criteria after treatment with cytoreductive therapy, in this case anagrelide. This study evaluated 154 ET patients treated with anagrelide for a median of 2.9 years. Despite the observation that platelet count at diagnosis was higher in those with a non-complete response vs those who had a complete response (993 × 109/L vs 753 × 109/L respectively; p < 0.001), there was no association of any clinical benefit, including incidence of vascular complications between both groups [22].
Polycythemia Vera: Thrombocytosis and Thrombosis
As has been the case with ET, neither retrospective nor prospective studies have consistently reported a significant correlation between platelet number and thrombosis risk [23, 24]. First, the PV Study Group (PVSG) 01, the largest prospective PV cohort prior to the ECLAP cohort, demonstrated that no hematologic parameter, including platelet count, measured prior to a thrombotic event was associated with increased risk of thrombosis [25]. Similarly, the European Collaboration on Low-Dose Aspirin in PV (ECLAP) did not find an association between platelet count and thrombotic events or total mortality. This prospective study demonstrated that major thrombotic events occurred in 8.3% of patients with baseline platelet count > 400 × 109/L vs 9.3% of those with lower platelet counts (p = 0.8). They similarly concluded that neither the currently proposed target of plt < 400 × 109/L nor any other platelet count deciles were predictive of increased thrombosis risk [26].
To the contrary, a high platelet count has been instead associated with an increased risk of hemorrhagic events. Accordingly, a reduction in platelet count with cytoreductive therapy has been shown to reduce risk of bleeding [24, 25]. The association between thrombocytosis and increased risk of hemorrhagic events may once again be explained by the development of acquired von Willebrand factor deficiency [27].
In contrast to prior studies, one study evaluated 261 PV patients (median follow-up ~ 7.2 years) who were treated with hydroxyurea (median duration of treatment ~ 4.4 years). Unexpectedly, they found that lack of response in platelet count, defined as plt < 400 × 109/L, was associated with both an increased risk of thrombosis (p = 0.04) and bleeding (p = 0.009). Interestingly, this study demonstrated that control of hematocrit, defined as Hct < 45%, did not statistically reduce incidence of either thrombosis (p = 0.8) or bleeding (p = 0.8) [28]. This is in contradiction with the randomized CYTO-PV study published in 2013 [29].
Myelofibrosis: Thrombocytosis and Thrombosis
Similar to other Philadelphia-negative MPNs, bleeding and thrombosis are long recognized complications of myelofibrosis. Based on the available literature, the incidence of thrombotic complications in PMF ranges from 6 to 12%, an incidence similar to that in ET but lower than PV [30,31,32]. Furthermore, the pathomorphologic entity of early/prefibrotic PMF may carry an even higher thrombotic risk than either ET or overt (fibrotic) PMF with frequency of thrombotic complications ranging from 15 to 30% [33, 34].
Given the associated morbidity and mortality, multiple studies have attempted to characterize risk factors of thrombosis in patients with PMF. Amongst these, age > 60, JAK2 V617F mutation status, and history of thrombosis have been the most established risk factors of thrombosis in fibrotic PMF [30, 32, 35]. More recently, Guglielmelli et al. reported age ≥ 65 years, leukocytosis, JAK2V617F mutation status, presence of CV risk factors, and high-molecular-risk mutations as independent risk factors of arterial thrombosis in early/prefibrotic PMF while only history of previous thrombosis was predictive of venous events [36]. Another large observational study which included 340 patients with either early/prefibrotic PMF or fibrotic PMF reported that when compared with major thrombocytosis (plt > 700 × 109/L), the presence of minor thrombocytosis (plt ≤ 700 × 109/L) at diagnosis was associated with a higher risk of thrombosis and trend toward lower risk of bleeding [20•]. Despite one study reporting thrombocytosis as an independent risk factor of thrombosis in univariate analysis, other studies have found either no significant association or a paradoxical inverse relationship between thrombotic risk and platelet count [20•, 30, 31, 33].
Furthermore, a contemporary study validated the IPSET-thrombosis score (comprised of age, history of thrombosis, JAK2 mutation, and CV risk factors), originally developed for ET, as the most accurate predictor of thrombotic risk in patients with prefibrotic PMF. It is important to note that thrombocytosis is not included amongst the risk factors for thrombosis in the IPSET-thrombosis score [36].
“Extreme” Thrombocytosis in MPN
The presence of “extreme” thrombocytosis (ExT), defined as a platelet count > 1000–1500 × 109/L, is an important consideration when approaching treatment of patients with MPN [37]. The presence of ExT in ET and PV patients is believed to be associated with increased risk of bleeding diatheses, presumably via mechanism of a platelet count–dependent acquired von Willebrand disease. Its presence is thus an important consideration when using aspirin in patients with low-risk ET or PV due to the increased risk of bleeding complications. When present in this population, some have advised to screen for ristocetin cofactor activity with consideration to withhold aspirin therapy if results show < 30% activity. Equally important, extreme thrombocytosis neither defines high-risk disease nor independently serves as an indication for cytoreductive therapy [38].
Management of extreme thrombocytosis is heterogeneous. An international survey of Israeli, Italian, and British MPN groups, Mayo Clinic, and NCCN MPN panel regarding different clinical case scenarios for management of ExT analyzed responses from 90 physicians. Based on this survey, 74% of physicians determined a platelet count ≥ 1500 × 109/L to be an indication for cytoreduction while 11% considered a plt ≥ 2000 × 109/L and 15% would not advise treatment, regardless of platelet count, unless there was presence of an abnormal vWF:RCo. If cytoreduction deemed indicated, target platelet counts varied from normal (53%), ≤ 600 × 109/L (30%), ≤ 1000 109/L (9%), to counts that normalized vWF:RCo [39]. In conclusion, there was no consensus on management of extreme thrombocytosis. This was manifested by variable platelet thresholds for triggering cytoreduction in low-risk ET/PV, variable platelet count targets if cytoreduction indicated, and variable answers regarding vWF:RCo testing prior to aspirin use. Approaches to treatment also varied depending on country of response although there was less variation depending on years of practice and/or experience. The large variation in responses for management ExT under different clinical scenarios emphasizes the need for prospective, randomized trials in patients with ExT.
Conclusion
The vast majority of literature has not found an association between thrombocytosis and risk of thrombosis (Table 1). The presence of thrombocytosis has instead been associated with an increased risk of hemorrhagic events, a paradoxical phenomenon thought to be mediated in some instances but not all, via an acquired VWD. Given that the majority of data was collected from retrospective cohorts, additional prospective studies will further help validate these clinically significant findings.
Furthermore, when cytoreduction is indicated, there is a large paucity of clinical data to help guide platelet goals. As previously discussed, it is even unclear whether complete normalization of platelet count by cytoreduction reduces thrombosis-free survival. In accordance with the aforementioned relationship between thrombocytosis and bleeding, some studies have suggested that normalizing platelet counts may instead reduce the risk of hemorrhagic events.
Finally, even the management of ExT is heterogenous and varies widely depending on geographic location. Interestingly, this variability is less so when clinicians are instead stratified by years of clinical practice and/or experience. This overall large variability in clinical practice emphasizes the need for prospective, randomized trials that would help optimize outcomes for this patient population.
Given the morbidity and mortality associated with both thrombosis and bleeding in MPNs, careful consideration must be made when recommending aspirin therapy for primary and secondary prevention of vascular events. Despite a clear benefit in patients with PV, a meta-analysis of twenty-four observational studies revealed imprecise and inconsistent findings regarding the net benefit of antiplatelet therapy in patients with ET [40•]. Furthermore, another study reported that primary prevention with antiplatelet therapy did not reduce thrombotic risk but significantly increased risk of bleeding in patients with low-risk CALR-mutated ET [41]. Even when aspirin therapy deemed indicated, the ideal dosing is also in question. Recent studies suggest that when compared with daily dosing of low-dose ASA in patients with ET, twice-daily (BID) dosing was associated with improved parameters of platelet inhibition including more consistent inhibition of platelet aggregation and more profound and consistent inhibition of serum thromboxane B2, a validated biomarker of platelet COX-1 activity [42, 43•]. Although these findings suggest that a BID dosing regimen may optimally reduce thrombotic risk in patients with ET, further validation is needed by additional studies assessing for a true reduction in thrombotic risk.
In keeping with the literature reviewed here, the patient in the above vignette was counseled about signs and symptoms of thrombosis, but was not started on cytoreduction, noting distribution in very low-risk thrombosis classification by IPSET-R (younger age, lack of thrombosis history, JAK2 negative). As demonstrated in Fig. 1, our management approach to MPN-associated thrombocytosis is multifaceted and individualized based on disease, risk classification, mutation status, and presence of aVWD or unexplained bleeding.
Our approach to MPN-associated thrombocytosis. Our approach when evaluating suspected MPN-associated thrombocytosis. Once thrombocytosis confirmed to be MPN-associated, indications for antiplatelet and/or cytoreductive therapy are dependent on disease risk classification and presence of acquired VWD or unexplained bleeding. *Retrospective study reported that low-dose ASA did not reduce risk of thrombosis but did increase risk of bleeding in low-risk CALR+ ET [41]. 1Compared with daily dosing of low-dose ASA in patients with ET, twice-daily (BID) dosing associated with improved parameters of platelet inhibition including more consistent inhibition of platelet aggregation and lower and more consistent levels of serum thromboxane B2, a validated biomarker of platelet COX-1 activity; no assessment of true thrombosis risk reduction [42, 43•]. 2 Metanalysis of twenty-four observational studies evaluating aspirin use in adults with ET reported overall inconsistency and imprecision amongst studies and thus high uncertainty regarding net effect of ASA in this patient population [40•]
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ruggeri M, Tosetto A, Frezzato M, Rodeghiero F. The rate of progression to polycythemia vera or essential thrombocythemia in patients with erythrocytosis or thrombocytosis. Ann Intern Med. 2003;139(6):470–5.
Griesshammer M, Bangerter M, Sauer T, Wennauer R, Bergmann L, Heimpel H. Aetiology and clinical significance of thrombocytosis: analysis of 732 patients with an elevated platelet count. J Intern Med. 1999;245(3):295–300.
Varghese LN, et al. The thrombopoietin receptor: structural basis of traffic and activation by ligand, mutations, agonists, and mutated calreticulin. Front Endocrinol (Lausanne). 2017;8:59.
Vannucchi AM, Barbui T. Thrombocytosis and thrombosis. Hematology Am Soc Hematol Educ Program. 2007;2007:363–70.
Skoda RC, Duek A, Grisouard J. Pathogenesis of myeloproliferative neoplasms. Exp Hematol. 2015;43(8):599–608.
James C, Ugo V, le Couédic JP, Staerk J, Delhommeau F, Lacout C, et al. A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature. 2005;434(7037):1144–8.
Pardanani AD, Levine RL, Lasho T, Pikman Y, Mesa RA, Wadleigh M, et al. MPL515 mutations in myeloproliferative and other myeloid disorders: a study of 1182 patients. Blood. 2006;108(10):3472–6.
Pikman Y, Lee BH, Mercher T, McDowell E, Ebert BL, Gozo M, et al. MPLW515L is a novel somatic activating mutation in myelofibrosis with myeloid metaplasia. PLoS Med. 2006;3(7):e270.
Zoi K, Cross NCP. Genomics of myeloproliferative neoplasms. J Clin Oncol. 2017;35(9):947–54.
••Barbui T, et al. Development and validation of an International Prognostic Score of thrombosis in World Health Organization-essential thrombocythemia (IPSET-thrombosis). Blood. 2012;120(26):5128-33; quiz 5252. Practice-changing publication validating IPSET-thrombosis score for risk-stratifying patients with ET into three categories based on thrombotic risk.
Barbui T, Barosi G, Birgegard G, Cervantes F, Finazzi G, Griesshammer M, et al. Philadelphia-negative classical myeloproliferative neoplasms: critical concepts and management recommendations from European LeukemiaNet. J Clin Oncol. 2011;29(6):761–70.
Cortelazzo S, Viero P, Finazzi G, D'Emilio A, Rodeghiero F, Barbui T. Incidence and risk factors for thrombotic complications in a historical cohort of 100 patients with essential thrombocythemia. J Clin Oncol. 1990;8(3):556–62.
Colombi M, Radaelli F, Zocchi L, Maiolo AT. Thrombotic and hemorrhagic complications in essential thrombocythemia. A retrospective study of 103 patients. Cancer. 1991;67(11):2926–30.
Bellucci S, Janvier M, Tobelem G, Flandrin G, Charpak Y, Berger R, et al. Essential thrombocythemias. Clinical evolutionary and biological data. Cancer. 1986;58(11):2440–7.
Campbell PJ, MacLean C, Beer PA, Buck G, Wheatley K, Kiladjian JJ, et al. Correlation of blood counts with vascular complications in essential thrombocythemia: analysis of the prospective PT1 cohort. Blood. 2012;120(7):1409–11.
Harrison CN. Management of essential thrombocythemia: implications of the medical research council primary thrombocythemia 1 trial. Semin Thromb Hemost. 2006;32(3):283–8.
Carobbio A, Thiele J, Passamonti F, Rumi E, Ruggeri M, Rodeghiero F, et al. Risk factors for arterial and venous thrombosis in WHO-defined essential thrombocythemia: an international study of 891 patients. Blood. 2011;117(22):5857–9.
••Barbui T, et al. Practice-relevant revision of IPSET-thrombosis based on 1019 patients with WHO-defined essential thrombocythemia. Blood Cancer J. 2015;5:e369 Practice-changing revision of well-established IPSET-thrombosis score used for thrombotic risk stratification in patients with ET.
••Haider M, et al. Validation of the revised International Prognostic Score of Thrombosis for Essential Thrombocythemia (IPSET-thrombosis) in 585 Mayo Clinic patients. Am J Hematol. 2016;91(4):390–4 External validation for revised IPSET-thrombosis score for patients with ET which is currently used in clinical practice.
•Gugliotta L, et al. Unbiased pro-thrombotic features at diagnosis in 977 thrombocythemic patients with Philadelphia-negative chronic myeloproliferative neoplasms. Leuk Res. 2016;46:18–25 Large cohort study assessing thrombotic risk factors, including platelet count, amongst Ph negative MPNs.
Carobbio A, Finazzi G, Antonioli E, Vannucchi AM, Barosi G, Ruggeri M, et al. Hydroxyurea in essential thrombocythemia: rate and clinical relevance of responses by European LeukemiaNet criteria. Blood. 2010;116(7):1051–5.
Hernandez-Boluda JC, et al. Clinical evaluation of the European LeukemiaNet response criteria in patients with essential thrombocythemia treated with anagrelide. Ann Hematol. 2013;92(6):771–5.
Spivak JL. Polycythemia vera: myths, mechanisms, and management. Blood. 2002;100(13):4272–90.
Schafer AI. Molecular basis of the diagnosis and treatment of polycythemia vera and essential thrombocythemia. Blood. 2006;107(11):4214–22.
Berk PD, Goldberg JD, Donovan PB, Fruchtman SM, Berlin NI, Wasserman LR. Therapeutic recommendations in polycythemia vera based on Polycythemia Vera Study Group protocols. Semin Hematol. 1986;23(2):132–43.
Di Nisio M, et al. The haematocrit and platelet target in polycythemia vera. Br J Haematol. 2007;136(2):249–59.
Falanga A, Marchetti M. Thrombosis in myeloproliferative neoplasms. Semin Thromb Hemost. 2014;40(3):348–58.
Alvarez-Larran A, et al. Assessment and prognostic value of the European LeukemiaNet criteria for clinicohematologic response, resistance, and intolerance to hydroxyurea in polycythemia vera. Blood. 2012;119(6):1363–9.
Marchioli R, Finazzi G, Specchia G, Cacciola R, Cavazzina R, Cilloni D, et al. Cardiovascular events and intensity of treatment in polycythemia vera. N Engl J Med. 2013;368(1):22–33.
Barbui T, Carobbio A, Cervantes F, Vannucchi AM, Guglielmelli P, Antonioli E, et al. Thrombosis in primary myelofibrosis: incidence and risk factors. Blood. 2010;115(4):778–82.
Cervantes F, Alvarez-Larrán A, Arellano-Rodrigo E, Granell M, Domingo A, Montserrat E. Frequency and risk factors for thrombosis in idiopathic myelofibrosis: analysis in a series of 155 patients from a single institution. Leukemia. 2006;20(1):55–60.
Elliott MA, Pardanani A, Lasho TL, Schwager SM, Tefferi A. Thrombosis in myelofibrosis: prior thrombosis is the only predictive factor and most venous events are provoked. Haematologica. 2010;95(10):1788–91.
Buxhofer-Ausch V, Gisslinger H, Thiele J, Gisslinger B, Kvasnicka HM, Müllauer L, et al. Leukocytosis as an important risk factor for arterial thrombosis in WHO-defined early/prefibrotic myelofibrosis: an international study of 264 patients. Am J Hematol. 2012;87(7):669–72.
Barosi G, Rosti V, Bonetti E, Campanelli R, Carolei A, Catarsi P, et al. Evidence that prefibrotic myelofibrosis is aligned along a clinical and biological continuum featuring primary myelofibrosis. PLoS One. 2012;7(4):e35631.
Kc D, Falchi L, Verstovsek S. The underappreciated risk of thrombosis and bleeding in patients with myelofibrosis: a review. Ann Hematol. 2017;96(10):1595–604.
Guglielmelli P, Carobbio A, Rumi E, de Stefano V, Mannelli L, Mannelli F, et al. Validation of the IPSET score for thrombosis in patients with prefibrotic myelofibrosis. Blood Cancer J. 2020;10(2):21.
Finazzi G, Carobbio A, Thiele J, Passamonti F, Rumi E, Ruggeri M, et al. Incidence and risk factors for bleeding in 1104 patients with essential thrombocythemia or prefibrotic myelofibrosis diagnosed according to the 2008 WHO criteria. Leukemia. 2012;26(4):716–9.
Tefferi A, Barbui T. Polycythemia vera and essential thrombocythemia: 2017 update on diagnosis, risk-stratification, and management. Am J Hematol. 2017;92(1):94–108.
Koren-Michowitz M, Lavi N, Ellis MH, Vannucchi AM, Mesa R, Harrison CN. Management of extreme thrombocytosis in myeloproliferative neoplasms: an international physician survey. Ann Hematol. 2017;96(1):87–92.
•Chu DK, et al. Benefits and risks of antithrombotic therapy in essential thrombocythemia: a systematic review. Ann Intern Med. 2017;167(3):170–80 A recent meta-analysis suggesting unclear net benefit of antiplatelet therapy in patients with ET.
Alvarez-Larran A, Pereira A, Guglielmelli P, Hernandez-Boluda JC, Arellano-Rodrigo E, Ferrer-Marin F, et al. Antiplatelet therapy versus observation in low-risk essential thrombocythemia with a CALR mutation. Haematologica. 2016;101(8):926–31.
Larsen ML, Pedersen OH, Hvas AM, Niekerk PBK, Bønløkke S, Kristensen SD, et al. Once- versus twice-daily aspirin treatment in patients with essential thrombocytosis. Platelets. 2019;30(3):322–8.
•Roccsa B, et al. A randomized, double-blind trial of three aspirin regimens to optimize antiplatelet therapy in essential thrombocythemia. Blood. 2020; https://doi.org/10.1182/blood.2019004596. Important recent randomized study evaluating efficacy of different aspirin regimens in patients with ET.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Myeloproliferative Neoplasms
Rights and permissions
About this article
Cite this article
Galvez, C., Stein, B.L. Thrombocytosis and Thrombosis: Is There Really a Correlation?. Curr Hematol Malig Rep 15, 261–267 (2020). https://doi.org/10.1007/s11899-020-00588-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11899-020-00588-z