Abstract
To investigate the clinicopathological characteristics and optimal treatment modalities of primary non-Hodgkin lymphoma (NHL) in the small and large intestine. Forty patients with primary NHL in the small and large intestine were studied retrospectively. All cases were reclassified according to the World Health Organization (WHO) classification of lymphoma in 2001. Fourteen patients had primary disease in the small intestine, which were all of B-cell origin with diffuse large B-cell lymphoma (DLBCL) diagnosed in 5 of 14 (35.7%) patients and mucosa-associated lymphoid tissue (MALT) lymphoma in 8 of 14 (57.1%) patients. Ileum was the most commonly involved site (8 of 14 patients, 57.1%), followed by jejunum (2 of 14 patients, 14.3%) and duodenum (1 of 14 patients, 7.1%). Twenty-five patients had primary colorectal lymphoma, with B-cell origin accounting for 92.0% and T-cell origin for 8.0% of these patients. The ileocaecal region has the highest involved rate (13 of 25 patients, 52.0%), followed by colon (7 of 25 patients, 28.0%) and rectum (3 of 25 patients, 12.0%). Compared with surgery alone, post-operation chemotherapy or chemoradiotherapy can significantly improve DLBCL patients’ event-free survival (EFS). However, no post-operation treatment modality can improve OS or EFS for patients with MALT lymphoma. B-cell lymphoma is the most common pathological type of intestinal lymphomas. Chemotherapy-containing treatment modality is an effective way to improve intestinal lymphoma patients’ EFS, especially for those with DLBCL subtype.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Gastrointestinal (GI) tract, accounting for 20∼40% of all extranodal disease, is the most commonly involved site for primary extranodal non-Hodgkin lymphomas (NHL). Almost half of the primary GI lymphomas are in the stomach, which is followed by small intestine with the incidence of 14∼38% [1–4]. Another 10∼20% are in the large intestine [5–9]. Histopathologically, 80∼90% of primary GI lymphomas are of B cell origin. Diffuse large B cell lymphoma (DLBCL) and mucosa-associated lymphoid tissue (MALT) lymphoma topped the rank of the subtypes of NHL that occurred in the GI tract [1, 5, 10–14]. In terms of T-cell lymphoma, there is a discrepancy in the different site of GI tract. Based on the data of a number of studies, the incidence of T-cell lymphoma increases with the site from stomach to colon getting lower, and this discrepancy is more significant among eastern populations [12–17].
Although some studies have shown that chemotherapy could improve the survival chance of intestinal lymphoma patients [18, 19], optimal treatment modality for different NHL subtype is still under-study. Here, we retrospectively analyze the clinical features of 40 intestinal NHL patients and further investigate the survival probability of these patients who were stratified by treatment modalities and pathological subtypes.
2 Patients and methods
From November 1992 to August 2003, 40 patients with primary intestinal NHL were diagnosed and treated at the Department of Medical Oncology, Cancer Institute and Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College (CAMS & PUMC). All specimens were obtained by biopsy or surgical resection and fixed in buffered formalin, embedded in paraffin and stained with hematoxylin-eosin. Antibodies against CD20, CD79a, CD3, CD5 and CD45RO were used for cell-origin analysis. All specimens were reviewed separately by two experienced pathologists (Zou S.M. and Xue L.Y.) and common consensus was reached in all cases. New WHO classification criteria were adopted for diagnosis.
For staging, a modification of the Ann Arbor system for GI lymphoma, proposed by Musshoff, was used. B symptoms were defined as unknown fever (>38°C) for more than 3 days, weight loss more than 10% within 6 months and night sweat. Primary GI NHL was defined according to Lewin et al. [6]. In brief, a patient had to present with GI symptoms of or have predominant lesions in the GI tract. International Workshop criteria were used for response evaluation. Overall survival (OS) was defined as the time from diagnosis to the date of patient’s death for any reason or to the last follow-up. Event-free survival (EFS) was measured from the date of diagnosis to the date that event occurred. Event included disease progression, relapse and patient death for any reason.
2.1 Statistical analysis
SSPS 10.0 software was used for data analysis. For continuous variables, t test or Mann–Whitney U test was employed to analyze the difference between two groups. χ2 test was employed for the analysis of category variables. Survival probability was calculated by Kaplan–Meier method. The log-rank test was used for comparing survival curves. All statistical analysis considered 0.05 as the significance level.
3 Results
3.1 Clinical characteristics
The patients included in our study comprised 1.92% (40 of 2,075) of NHL patients and 37% (40 of 108) of primary GI lymphoma patients treated in our hospital during the same period. The median age at diagnosis was 44 (13∼78) years. Sixty-five percent (26 of 40) of patients were males. The male: female ratio was 1.86:1. Fourteen of 40 patients (35%) had their primary site in the small intestine, 25 of 40 (62.5%) in the large intestine, and 1 of 40 (2.5%) in the unclear site of intestine.
Twenty-eight of 40 patients (70.0%) had stage I/II disease, 12 of 40 patients (30.0%) had stage III/IV disease. Sixteen of 40 patients (40.0%) had B symptoms, with fever and weight loss being the most common. Altogether, 25 patients had complete clinical data for international prognosis index (IPI) scoring. Fourteen of 25 (56.0%) patients were in the low-risk group, 3 of 25 (12.0%) in the low intermediate risk group, 4 of 25 (16.0%) in the high intermediate risk group and 4 of 25 (16.0%) in the high risk group. Twenty-four of 40 patients (60.0%) had bulky disease (≥5 cm), including ten patients with maximum diameter of mass, larger than 10 cm (Table 1).
Thirty-three of 40 patients (82.5%) had GI symptoms as their primary clinical presentations. Abdominal pain was the main diagnostic symptom for this population, which was presented in 26 of 33 (78.8%) patients, followed by diarrhea in 7 of 33 (21.2%), bloody stool in 6 of 33 (18.2%), nausea and vomiting in 4 of 33 (12.1%), melena in 3 of 33(9.0%), constipation and change in bowel habits in two each (6.0%). (One or more symptoms may be presented in one patient.)
Pathologically, DLBCL was diagnosed in 17 of 40 (42.5%) patients. Five of 17 patients (29.4%) had their primary disease in the small intestine, and the rest of 12 of 17 (70.6%) in the colorectum. MALT lymphoma was diagnosed in 20 of 40 (50.0%) patients, including 8 of 20 (40.0%) in the small intestine, 11 of 20 (55.0%) in the colorectal region, and 1 of 20 (5.0%) in the unclear site. T cell lymphoma was diagnosed in 2 of 40 (5.0%), including one in the ileocaecal region and one in the transverse colon. One patient had unclear subtype of B-cell NHL (Table 2).
3.2 Treatment and outcomes
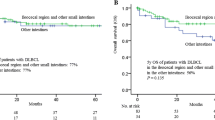
The median time of follow-up was 18 months (ranging from 1 to 103 months) for all patients. The OS and EFS at 2 years were 78.8 and 34.7%, respectively.
Of 40 patients, five were treated with surgical procedure only (radical resection in three stage I patients, exploratory laparotomy in two stage IV patients), four were treated with radiation therapy after operation (All were stage I patients). The other 31 patients were treated with combined chemotherapy after operation, which CHOP-like regimen was employed except one patient treated with cyclophosphamide alone. Furthermore, 7/31 patients received additional radiotherapy when combined chemotherapy had completed (Table 3).
Of those patients treated with surgical procedure only, three relapsed at median time of 4 months (ranged from 3 to 5 months). The other two died within a month because of tumor- and surgery-related complications, respectively. For patients treated with radiotherapy after operation, one died during radiotherapy due to side effects, one relapsed 5 months after diagnosis, the other two survived disease-free for 11 months and 46 months, respectively.
Of 31 patients treated with chemotherapy or chemoradiotherapy, seven had evaluable disease after operation. And complete response was achieved in two patients and partial response in five. The 2-year OS and EFS for patients treated with chemotherapy after operation (n = 24) are 74.0 and 30.6%, respectively. Another seven patients treated with chemoradiotherapy had 2-year OS and EFS of 80.0% and 66.7%, respectively.
Among these four treatment groups (group 1 = surgery only, group 2 = surgery plus radiotherapy, group 3 = surgery plus chemotherapy, group 4 = surgery plus chemoradiotherapy), the difference of OS did not reach the significant level (P = 0.58), while that of EFS did (P = 0.0017) (Figs. 1, 2). Further analysis of EFS has shown that group 3 (P = 0.0015) and group 4 (P = 0.0011) had higher EFS probability compared with group 1, while group 2 did not (data not shown).
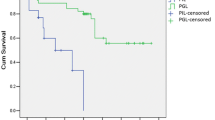
Pathologically, the 2-year OS for DLBCL patients and MALT lymphoma patients were 79.9 and 73.3%, respectively, while 2-year EFS for two subtypes were 39.2 and 31.8%, respectively. The difference of OS and EFS between two subtypes did not reach the significant level (data not shown). However, if the survival probabilities of different treatment groups were compared within the DLBCL population, statistically significant difference could be seen in EFS (P = 0.01) (Fig. 3). Further analysis showed that chemotherapy (group 3, P = 0.006) and chemoradiotherapy (group 4, P = 0.02) after operation could bring EFS benefit to these patients compared with those treated with operation alone. However, the EFS between group 3 and group 4 were comparable with no significant difference shown. As far as MALT lymphoma was concerned, neither OS nor EFS showed significant difference among four treatment groups (Fig. 4).
4 Discussion
The clinical characteristics of our study were similar to those described in previous reports. There is a male predominance, with the maximal incidence in the 40 to 60 years age group [5, 10, 12, 17] and abdominal pain as the most common presentation [5]. Ileum and ileocaecal region were the most commonly involved site for small [10, 13, 20, 21] and large intestine [4–6, 12–17, 19, 22, 23], respectively, probably due to relatively higher proportion of lymphoid tissue in these area. Moreover, higher leocaecal region involvement rate could be seen in western populations [4, 6, 14, 17, 22, 23] compared with that of eastern ones [5, 12, 13, 15, 16, 19]. This discrepancy is similar to the geographic difference of colon tumor between the west and east. Diet habit, which acts as a kind of exposure factor of colon malignancies, may attribute to this, although no such a correlation has been established in lymphoma.
As in other reports, DLBCL and MALT lymphoma were the main subtypes of intestinal NHL, either in the small or large intestine [1, 5, 10–14, 21]. Furthermore, other reports showed that the incidence of DLBCL increased with the site from stomach to colon getting lower. Accordingly, the incidence of MALT was becoming fewer [1, 5, 10, 11, 13–15, 17, 21]. The exact reason is unknown, although the decreasing of MALT component from stomach to colon could partially explain the phenomenon. However, no such a tendency can be seen in our study, probably due to small number of cases.
Many studies have shown that intestinal lymphoma had poorer survival than gastric lymphoma [1, 10, 17]. Probably due to higher proportion of aggressive lymphoma, such as DLBCL, and T-cell lymphoma can be seen in this area [12–17]. However, no studies, including ours, had found survival difference between NHL patients with small intestinal and large intestinal involvement [13].
Survival analysis in our study showed that patients treated with surgery alone had poorer EFS than those treated with chemotherapy-containing strategy. Two patients (one was DLBCL, one was MALT lymphoma) in this group with stage IV disease died soon after operation. The other three patients (two were DLBCL, one was MALT lymphoma), although they had stage I disease, suffered disease progression at a median time of 3 months. As a result, surgery alone did not show any benefit for the survival of these patients. The role of surgery in the treatment of GI lymphoma, either alone or in combination with other modalities, has been a matter of debate for a long time [21, 24–29]. The results of recent studies have shown that the status of surgery had been undermined by conservative management, especially chemotherapy-containing modalities, which could not only improve GI lymphoma patients’ quality of life, but also their survival [17, 19, 30–32]. Thus, many authors recommended that surgery need not be considered for treating of GI lymphomas.
However, compared with nodular lymphoma, it is difficult to obtain tumor tissue for diagnosing GI lymphoma since most patients have their disease inside the abdomen. In addition, the similarity of radiographic features between GI lymphoma and other intestinal cancers makes it hard to quit surgical procedure before the ultimate diagnosis is obtained. After all, surgery is the primary treatment choice for intestinal cancer patients. Furthermore, serious complications such as bleeding, obstruction and perforation often occur during peri-treatment period. This cannot be managed by conservative treatment. Based on these facts, it is reasonable to confine surgery to certain circumstances in the treatment of GI lymphomas.
MALT lymphoma is a kind of indolent lymphoma. Few studies explore the optimal treatment for intestinal MALT lymphomas. Most experience comes from gastric MALT lymphoma, for which non-systematic treatment such as surgery, regional radiotherapy or H. pylori eradiation therapy may be employed [1, 10, 32]. Chemotherapy is mostly confined to advanced diseases. And no definite conclusion can be made regarding which treatment modality is superior [32, 33]. The same situation can be seen in our study that no treatment modalities showed the ability of improving MALT patients’ OS and EFS. Thus, the natural history of these patients is probably still unchanged. Since it is an incurable disease, the treatment should be conservative until some new strategies or new agents such as fludarabine or Rituximab proved to be more effective than the present ones.
DLBCL is the most common subtype of aggressive lymphoma. And it has been proved that, for nodular DLBCL, chemotherapy is the optimal treatment modality and can improve patients’ long-term survival. In our study, survival analysis found that, although chemotherapy-containing modalities were capable of improving intestinal NHL patients’ EFS, the benefits were restricted only to DLBCL patients. This is consistent with the results from nodular and some gastric DLBCL patients [31, 34]. In addition, MALT lymphoma, an indolent lymphoma, usually has a better survival than aggressive lymphoma such as DLBCL. And the data from some studies supported this point of view, especially those studies concerning GI lymphoma [1, 10]. However, in our study, statistical analysis found no significant difference in the OS and EFS between DLBCL and MALT lymphoma patients. And some other studies showed the same results [11, 13, 21, 35]. Interestingly, we found that those studies in which survival difference was significant had lower proportion of patients treated with chemotherapy (33.6% [1] and 38.8% [10], respectively). While 70–100% patients treated with chemotherapy in those studies in which no significant survival difference was found. As a result, we thought that it was probably chemotherapy, which potentially improved the survival of DLBCL that made the DLBCL patients have the comparable survival with MALT lymphoma patients. For these reasons, chemotherapy-containing strategy may be the optimal choice and should be warranted for intestinal DLBCL patients.
Individual centers see only small numbers of patients with intestinal lymphoma over a long period, and there is therefore a need for a multicenter prospective study in order to create a database large enough for definitive analysis to be made in order to rationalize the treatment of such patients.
References
Nakamura S, Matsumoto T, Iida M, Yao T, Tsuneyoshi M. Primary gastrointestinal lymphoma in Japan: a clinicopathologic analysis of 455 patients with special reference to its time trends. Cancer. 2003;97:2462–73.
Yoshino T, Miyake K, Ichimura K, et al. IIncreased incidence of follicular lymphoma in the duodenum. Am J Surg Pathol. 2000;24:688–93.
Zucca E, Roggero E, Bertoni F, Cavalli F. Primary extranodal non-Hodgkin’s lymphomas. Part 1: Gastrointestinal, cutaneous and genitourinary lymphomas. Ann Oncol. 1997;8:727–37.
Amer M, el-Akkad S. Gastrointestinal lymphoma in adults: clinical features and management of 300 cases. Gastroenterology. 1994;106:846–58.
Wong MT, Eu KW. Primary colorectal lymphomas. Colorectal Dis. 2006;8:586–91.
Lewin KJ, Ranchod M, Dorfman RF. Lymphomas of the gastrointestinal tract: a study of 117 cases presenting with gastrointestinal disease. Cancer. 1978;42:693–707.
Kashimura A, Murakami T. Malignant lymphoma of the large intestine-15-year experience and review of literature. Gastroenterol Jpn. 1976;11:141–7.
Henry CA, Berry RE. Primary lymphoma of the large intestine. Am Surg. 1988;54:262–6.
Dragosics B, Bauer P, Radaszkiewicz T. Primary gastrointestinal non-Hodgkin’s lymphomas: a retrospective clinicopathologic study of 150 cases. Cancer. 1985;55:1060–73.
Nakamura S, Matsumoto T, Takeshita M, et al. clinicopathologic study of primary small intestine lymphoma: prognostic significance of mucosa-associated lymphoid tissue-derived lymphoma. Cancer. 2000;88:286–94.
Koch P, Probst A, Berdel WE, et al. Treatment results in localized primary gastric lymphoma: data of patients registered within the German multicenter study (GIT NHL 02/96). J Clin Oncol. 2005;23:7050–9.
Kim YH, Lee JH, Yang SK, et al. Primary colon lymphoma in Korea: a KASID (Korean Association for the Study of Intestinal Diseases) Study. Dig Dis Sci. 2005;50:2243–7.
kohno S, Ohshima K, Yoneda S, Kodama T, Shirakusa T, Kikuchi M. Clinicopathological analysis of 143 primary malignant lymphomas in the small and large intestines based on the new WHO classification. Histopathology. 2003;43:135–43.
Bairey O, Ruchlemer R, Shpilberg O. Non-Hodgkin’s lymphomas of the colon. Isr Med Assoc J. 2006;8:832–5.
Gan JL, Tang ZJ. Clinical, endoscopic and pathological features of primary colorectal non-Hodgkin lymphoma: 24 cases report. Zhonghua Wei Chang Wai Ke Za Zhi. 2006;9:502–5.
Bai CM, Yang T, Xu Y, et al. Clinical analysis of 32 primary intestinal non-Hodgkin’s lymphoma. Zhonghua Zhong Liu Za Zhi. 2006;28:142–4.
Koch P, del Valle F, Berdel WE, et al. Primary gastrointestinal non-Hodgkin’s lymphoma: I. Anatomic and histologic distribution, clinical features, and survival data of 371 patients registered in the German Multicenter Study GIT NHL 01/92. J Clin Oncol. 2001;19:3861–73.
Ibrahim EM, Ezzat AA, El-Weshi AN, et al. Primary intestinal diffuse large B-cell non-Hodgkin’s lymphoma: clinical features, management, and prognosis of 66 patients. Ann Oncol. 2001;12:53–8.
Fan CW, Changchien CR, Wang JY, et al. Primary colorectal lymphoma. Dis Colon Rectum. 2000;43:1277–82.
Haselkorn T, Whittemore AS, Lilienfeld DE. Incidence of small bowel cancer in the United States and worldwide: geographic, temporal, and racial differences. Cancer Causes Control. 2005;16:781–7.
Morton JE, Leyland MJ, Vaughan Hudson G, et al. Primary gastrointestinal non-Hodgkin’s lymphoma: a review of 175 British National Lymphoma Investigation cases. Br J Cancer. 1993;67:776–82.
Bruneton JN, Thyss A, Bourry J, Bidoli R, Schneider M. Colonic and rectal lymphomas. A report of six cases and review of the literature. Rofo. 1983;138:283–7.
Kajanti M, Karkinen-Jaaskelainen M, Rissanen P. Primary gastrointestinal non-Hodgkin lymphoma. A review of 36 cases. Acta Oncol. 1988;27:51–5.
Brands F, Monig SP, Raab M. Treatment and prognosis of gastric lymphoma. Eur J Surg. 1997;163:803–13.
Crump M, Gospodarowicz M, Shepherd FA. Lymphoma of the gastrointestinal tract. Semin Oncol. 1999;26:324–37.
Fischbach W, Dragosics B, Kolve-Goebeler ME, et al. Primary gastric B-cell lymphoma: results of a prospective multicenter study. The German-Austrian Gastrointestinal Lymphoma Study Group. Gastroenterology. 2000;119:1191–202.
Azab MB, Henry-Amar M, Rougier P, et al. Prognostic factors in primary gastrointestinal non-Hodgkin’s lymphoma. A multivariate analysis, report of 106 cases, and review of the literature. Cancer. 1989;64:1208–17.
Bellesi G, Alterini R, Messori A, et al. Combined surgery and chemotherapy for the treatment of primary gastrointestinal intermediate- or high-grade non-Hodgkin’s lymphomas. Br J Cancer. 1989;60:244–8.
Salles G, Herbrecht R, Tilly H, et al. Aggressive primary gastrointestinal lymphomas: review of 91 patients treated with the LNH-84 regimen. A study of the Groupe d’Etude des Lymphomes Agressifs. Am J Med. 1991;90:77–84.
Schmidt WP, Schmitz N, Sonnen R. Conservative management of gastric lymphoma: the treatment option of choice. Leuk Lymphoma. 2004;45:1847–52.
Aviles A, Nambo MJ, Neri N, et al. The role of surgery in primary gastric lymphoma: results of a controlled clinical trial. Ann Surg. 2004;240:44–50.
Aviles A, Nambo MJ, Neri N, Talavera A, Cleto S. Mucosa-associated lymphoid tissue (MALT) lymphoma of the stomach: results of a controlled clinical trial. Med Oncol. 2005;22:57–62.
Nakamura S, Matsumoto T, Suekane H, et al. Long-term clinical outcome of Helicobacter pylori eradication for gastric mucosa-associated lymphoid tissue lymphoma with a reference to second-line treatment. Cancer. 2005;104:532–40.
Park YH, Lee SH, Kim WS, et al. CHOP followed by involved field radiotherapy for localized primary gastric diffuse large B-cell lymphoma: results of a multi center phase II study and quality of life evaluation. Leuk Lymphoma. 2006;47:1253–9.
Mihaljevic B, Nedeljkov-Jancic R, Vujicic V, Antic D, Jankovic S, Colovic N. Primary extranodal lymphomas of gastrointestinal localizations: a single institution 5-yr experience. Med Oncol. 2006;23:225–35.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Li, B., Shi, Yk., He, Xh. et al. Primary non-Hodgkin lymphomas in the small and large intestine: clinicopathological characteristics and management of 40 patients. Int J Hematol 87, 375–381 (2008). https://doi.org/10.1007/s12185-008-0068-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-008-0068-5