Abstract
Background
The degree to which shared vulnerability and protective factors for chronic pain and trauma-related symptoms contribute to pain adjustment in chronic pain patients who have experienced a traumatic event remains unclear.
Purpose
The purpose is to test a hypothetical model of the contribution of experiential avoidance, resilience and pain acceptance to pain adjustment in a sample of 229 chronic back pain patients who experienced a traumatic event before the onset of pain.
Methods
Structural equation modelling was used to test the linear relationships between the variables.
Results
The empirical model shows significant relationships between the variables: resilience on pain acceptance and trauma-related symptoms, experiential avoidance on trauma-related symptoms and experiential avoidance, pain acceptance and trauma-related symptoms on pain adjustment.
Conclusions
This study demonstrates the role of a vulnerability pathway (i.e. experiential avoidance) and a protective pathway (i.e. resilience and pain acceptance) in adaptation to pain after a traumatic event.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
There is a cumulative body of evidence showing an association between being exposed to different kinds of traumatic events and experiencing a chronic pain syndrome [1–5], although it has been argued that the potential mechanism that could at least partly explain this relationship is the presence of posttraumatic stress disorder (PTSD) symptoms [6, 7]. The co-occurrence of chronic pain and PTSD—as a diagnosed disorder—, posttraumatic symptoms—as a subsyndromal PTSD—, as well as trauma-related symptoms—as a predisposing factor for both of them—is well documented, with numerous studies showing that psychological variables play a major role in the increased response to pain among all these patients [6, 8–11].
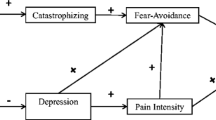
This empirical evidence supports the notion that both disorders involve a specific psychological vulnerability that could be described as a tendency to respond with fear to perceived physical sensations, which in turn leads to avoidance behaviours. In fact, the core of the fear-avoidance model of chronic back pain [12] is how patients interpret pain. When pain is interpreted as threatening, it leads to a dysfunctional behavioural pattern characterized by an excessive fear of pain that gradually extends to a fear of physical movements such that patients will avoid the physical activities that might increase their pain. This being the case, although it is not explicitly stated in the model, experiential avoidance could be considered as a variable that contributes to this tendency to respond with fear. Given that the roots of the fear-avoidance model arise from the cognitive-behavioural treatment of phobia and anxiety disorders, it seems reasonable to consider experiential avoidance as one of the key variables explaining fear-avoidance behaviours.
Experiential avoidance appears as a feature of chronic pain [13, 14] as well as of PTSD [15, 16]. Experiential avoidance is considered to be a process associated with negatively experiencing internal events, in which an affect-related regulatory process takes part that involves unwillingness to endure upsetting private experiences. Therefore, experiential avoidance represents a constant effort to escape and avoid unpleasant emotions, thoughts, memories and other private experiences [17]. Moreover, it is explicitly linked to context and function, as it is placed within the context of valued behaviours and activities that are abandoned because of the unwillingness to be in contact with undesired internal events [18]. In the field of chronic pain research, the role of experiential avoidance in pain adjustment is just beginning to be investigated. Nevertheless, some studies have suggested that this variable plays an undoubted role in pain adjustment. The recent study by Costa and Pinto-Gouveia [19] suggests that chronic pain patients who show lower levels of experiential avoidance report less depression, anxiety and stress. In a previous study [20], these authors found that experiential avoidance partially or fully mediates the effects of coping on depression and distress in chronic pain patients, suggesting that experiential avoidance, and not only pain coping, is involved in the psychopathological profile that characterizes some of these patients. In the study carried out by Esteve et al. [13], experiential avoidance was significantly associated with fear of pain in a sample of chronic back pain patients. Recently, Esteve and Ramírez-Maestre [21] found the same pattern of relationships across three different chronic pain samples: a direct association between experiential avoidance and pain fear avoidance and between pain fear avoidance and negative mood.
In the context of trauma and PTSD, experiential avoidance can be seen as a dysfunctional way of regulating the negative emotions that appear when experiencing a traumatic event. Furthermore, it is has been conceptualized as a toxic self-regulatory diathesis for anxiety-related pathology [18]. In line with this, experiential avoidance is considered to be involved in the aetiology of PTSD [22] and in the maintenance of this disorder [23]. Nevertheless, research on experiential avoidance and trauma, as well as on experiential avoidance and PTSD remains scarce. Taken as a whole, the empirical evidence on this issue leads to the conclusion that experiential avoidance is related to increased PTSD symptom severity and poorer functioning (for a review, see Thompson et al. [24]). In this regard, the results presented by Marx and Sloan [15] showed that experiential avoidance predicted the long-term maintenance of PTSD. Furthermore, a study conducted on a sample of Kosovo War survivors found that experiential avoidance partially mediated the effects of PTSD on quality of life, although it did not mediate the effects of the disorder on global distress [25]. Nevertheless, findings on the association between PTSD and experiential avoidance remain inconclusive as it is still unknown whether this variable is a unique predictor of PTSD symptoms or a predictor of generalized psychological dysfunction among trauma victims [24]. In this sense, in the experimental study carried out by Gómez-Pérez and López-Martínez [26], no differences in experiential avoidance were found between trauma-exposed women with and without PTSD symptoms.
No research has been conducted using samples of patients with trauma-related symptoms, PTSD and chronic pain to identify which variables could decrease experiential avoidance and increase acceptance of those internal events that often elicit painful reactions. Acceptance involves flexible, efficient responses with individuals staying in contact with their emotions and thoughts and attending to the information they provide [27]. Therefore, acceptance and experiential avoidance could be viewed as opposite extremes of a psychological continuum [28]. In fact, acceptance includes viewing psychological events as understandable and transient reactions to external events, rather than viewing internal and private events as eliciting painful reactions that must be avoided [24].
The protective role of acceptance in the context of chronic pain is well documented and has been demonstrated to be positively associated with lower pain intensity, improved daily functioning and better mood [29–31] and negatively associated with pain avoidance behaviours [32]. Therefore, pain acceptance seems to represent an adaptive form of “pain confrontation” whereby the individual responds to pain-related experiences without attempting to control them and engages in valued activities, as well as reaching personal goals, regardless of these experiences [21, 33]. Hence, pain acceptance could be considered to be a positive pathway to pain adjustment, leading to lower levels of pain intensity, pain disability and emotional distress.
Regarding trauma research, it is well known that the majority of people exposed to a traumatic event maintain stable equilibrium without developing reactive psychopathology [34]. It has been assumed that to successfully process traumatic events, the individual must be willing to be in contact with private events (i.e. emotions, memories, bodily sensations) [35]. In fact, some evidence suggests that acceptance is associated with fewer psychological symptoms and more positive outcomes after exposure to trauma [24]. Furthermore, acceptance has been postulated to be an attitude that may protect trauma survivors from engaging in the chronic avoidance that serves to exacerbate symptomatology which, as a result, would help them to interpret any posttraumatic symptoms as transient. In fact, the majority of people who have experienced a traumatic event do not develop PTSD symptoms. Hence, identifying which factors protect individuals against the development of PTSD is of undoubted interest in the context of trauma exposure. In this sense, it has been demonstrated that people who have experienced a traumatic event without developing PTSD symptomatology present high levels of psychological resilience [34, 36]. Taking all this into account, it might be expected that acceptance and resilience are related constructs. This has been suggested by two studies in the field of chronic pain research. The study by López-Martínez et al. [37] included a sample of heterogeneous chronic pain patients, showing that resilience and pain acceptance were positively related and both predicted active pain coping. In addition, Ramírez-Maestre et al. [38] obtained the same results in a sample of patients with chronic back pain.
As far as we know, only two studies have evaluated resilience and pain acceptance in chronic pain patients with PTSD symptoms [39] and trauma-related symptoms [40], showing that trauma-exposed chronic pain patients without PTSD had higher scores on resilience and pain acceptance than trauma-exposed chronic pain patients with PTSD or with trauma-related symptoms. There is a broad consensus regarding the definition of psychological resilience as a dynamic process that involves overcoming the negative effects of exposure to risk, successfully coping with adverse experiences and avoiding negative trajectories associated with risk [41]. Thus, it is unsurprising that resilience has been shown to moderate the association between PTSD risk factors and the development of PTSD by buffering the effects of the risk factors [34, 36, 42]. It is also worth noting that higher scores on measures of psychological resilience have been shown to be negatively associated with a positive screen for PTSD [34, 43] and positively associated with posttraumatic growth [34].
In summary, the empirical evidence suggests that experiential avoidance could be considered a shared vulnerability factor for chronic pain and PTSD symptoms. In addition, research has begun to highlight resilience and acceptance (as the opposite of experiential avoidance) as protective factors that contribute to better adjustment in both disorders. Despite the well-documented co-occurrence of PTSD and chronic pain, the degree to which all these variables contribute to pain adjustment in chronic pain patients with both trauma-related symptoms and PTSD symptoms remains unclear. Thus, the aim of the present study was to test, via structural equation modelling, a hypothetical model of the contribution of experiential avoidance, resilience and pain acceptance to adjustment to pain in a sample of chronic back pain patients who had been exposed to traumatic events before the onset of pain. We hypothesized that after a traumatic event, resilience would significantly predict increases in pain acceptance and decreases in experiential avoidance and that it would be negatively associated with trauma-related symptoms. We also hypothesized that pain acceptance would be negatively associated with experiential avoidance and that experiential avoidance would be positively associated with trauma-related symptoms. Finally, accordingly to the hypothetical model, a direct effect of pain acceptance, trauma-related symptoms and experiential avoidance on pain adjustment (i.e. pain intensity, pain disability and emotional distress) was predicted.
Methods
Participants
The participants consisted of a consecutive sample of 241 patients with chronic back pain. They had been referred by physicians and physiotherapists from several primary care health centres in Málaga (Spain). The inclusion criteria for the study were the following: back pain of benign origin for at least the last 3 months, pain intensity 3 or above on the Pain Numerical Rating Scale of 10 points [44], continuous or intermittent pain appearing for five or more days per week and exposure to a traumatic event before the onset of pain (12 patients were excluded because pain onset occurred before they were exposed to a traumatic event). The doctors who participated in the study reviewed the patients’ clinical history and if the patients fulfilled the inclusion criteria, their participation was requested. No one refused participation.
Thus, the final sample included 229 patients. The majority of them were female (71.2 %) and were married (66.8 %); 36.7 % had completed secondary education and were employed (48.3 %). Their ages ranged from 18 to 60 years (mean = 45.53, SD = 11.89). All of them had back pain in the following regions: lumbar, sacral and coccygeal (88.6 %); cervical (10.5 %) and thoracic (0.9 %). Participants completed the Davidson Trauma Scale (DTS) [45] only if they endorsed experiencing at least one of the items of the Stressful Life Events Questionnaire Revised (SLEQ-R) [46]. Thus, participants were considered to have a positive history of exposure to traumatic events when they answered Yes to at least one of the Stressful Life Event Screening Questionnaire Revised (SLESQ-R) items. The mean duration of pain was 4.61 years (SD = 3.80). Their mean scores on the DTS was 30.78 (SD = 30.35). Data regarding the clinical traumatic variables is available in the Electronic Supplementary Material (ESM). The most common traumatic events were death of a very close person due to accident, homicide or suicide (45.9 %); emotional abuse (39.7 %); physical abuse (29.3 %) and life-threatening accident (24.5 %). The average number of traumatic situations experienced by participants was 2.51 (SD = 1.76).
Procedure
The research project, of which this study is a part, was approved by the Ethics Committees of the Málaga and Costa del Sol Health Districts (Spain). Prior to data collection, the researchers held a meeting with the participating doctors in which the eligibility criteria were explained and the procedures were decided on.
At the end of their medical visit, each patient who fulfilled the eligibility criteria was informed by their doctor of the study aims and their participation was requested. The participants were contacted by telephone to make an appointment; none of them refused participation. Each participant completed a battery of questionnaires in the same order in an oral semi-structured interview format with a psychologist lasting 1.5 h. All patients were interviewed at their clinic, while waiting to be seen by their physicians. Informed consent was obtained prior to data collection. Patients were aware that the information collected was confidential.
Measures
Stressful Life Event Screening Questionnaire Revised
This is a dichotomous response self-report measure (Yes/No) assessing previous exposure to 13 specific Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (DSM-IV) PTSD criterion A events for use in a non-treatment-seeking sample [47], which implies that the person experienced, witnessed or was confronted with an event or events that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others. In addition, the person’s response involved intense fear, helplessness or horror. It has a very good test-retest reliability, with a median kappa of 0.73. It also has a good convergent validity, with a median kappa of 0.64, as well as a good discrimination between criterion A and non-criterion A events [47]. The original questionnaire was slightly modified recently [46], with the inclusion of miscarriage, and the way some items were phrased was changed.
As far as we know, no validated instruments are available in Spanish for assessing lifetime exposure to a variety of traumatic events. Thus, the SLESQ-R [47] was translated into Spanish. We employed forward-backward translation to adapt this scale into the final Spanish version. First, the original English version of the SLESQ-R was translated into Spanish by two native Spanish speakers. Both were clinical psychologists familiar with the terminology of the area covered by the instrument and had clinical experience with chronic pain patients. As a result, two Spanish versions were obtained and compared for inconsistencies. These inconsistencies were taken into account, and a new Spanish version was produced based on the corrections made. This Spanish version was then translated into English by a native speaker familiar with the psychological terminology. This English translation was then compared to the original English RS and checked for inconsistencies. The inconsistencies were then corrected in the final Spanish version.
After completing the SLESQ-R, respondents were asked to nominate their most distressing traumatic event (if endorsing more than one) for later PTSD inquiry. Cronbach’s alpha for this questionnaire was 0.70 in the sample of the current study.
Davidson Trauma Scale
The DTS [45] measures the 17 PTSD symptoms described in DSM-IV. Each DTS item is measured on a 0–4 scale of severity and frequency, such that the maximum possible score is 136. Scores on the DTS can differentiate patients with PTSD and partial PTSD from patients without PTSD in the general population. It has a good test-retest reliability (r = 0.86), internal consistency (r = 0.99) and convergent and divergent validities, as well as current validity. It also predicts validity in relation to response to treatment, as well as sensitivity treatment effects [48]. Subjects with a DTS score of 40 or more are considered to have a probable diagnosis of PTSD, whereas scores between 30 and 40 are considered as probable subsyndromal PTSD [49]. The Spanish version was used in this study [50]. The internal consistency of the DTS total score in this sample was 0.92.
Resilience Scale
The original Resilience Scale [51], which was developed for the general population, considered resilience to be a positive personality characteristic that moderates the negative effects of stress and promotes adaptation. The Resilience Scale comprises 25 items scored on a seven-point scale ranging from 1 (Disagree) to 7 (Agree). The Spanish version used in this study was adapted for patients with chronic musculoskeletal pain and comprises 18 items showing a good internal consistency, stability and construct validity [41]. Cronbach’s alpha for this questionnaire was 0.94.
Acceptance and Action Questionnaire
The Acceptance and Action Questionnaire [52] is a nine-item questionnaire designed to measure the tendency to engage in experiential avoidance. Each item is rated on a seven-point scale ranging from 1 (Never) to 7 (Always). Higher scores indicate higher levels of avoidance and immobility. The instrument has good psychometric properties [52]. The Spanish adaptation used in this study [53] has psychometric properties similar to the original one. Cronbach’s alpha for this questionnaire was 0.73.
Chronic Pain Acceptance Questionnaire
This is a 20-item scale assessing acceptance of pain [30]. The items are rated on a scale from 0 (Never true) to 6 (Always true). It has a good internal consistency and concurrent validity. Like the original questionnaire, the Spanish version [54] has a good internal consistency and good criterion validity. Cronbach’s alpha for this questionnaire was 0.83.
Composed Pain Intensity Index
According to the recommendations of Jensen et al. [44], patients were asked to rate their mildest, average and worst pain during the past 2 weeks, as well as their current pain, on a scale ranging from 0 (No pain) to 10 (Extremely painful). A composite pain intensity score was calculated for each subject by calculating the average of the mildest, average, worst and current pain. Composites of the 0–10 ratings are very reliable measures of pain intensity in chronic pain patients [44]. Cronbach’s alpha for this questionnaire was 0.81.
Roland-Morris Disability Questionnaire
This questionnaire consists of 24 items in which the responders are asked to rate the degree to which pain interferes with functioning in different areas of life [55]. Ratings may range from 0 (No disability) to 24 (Maximum disability). The Spanish version of this scale [56] has suitable reliability and validity. Cronbach’s alpha for this questionnaire was 0.87.
Hospital Anxiety and Depression Scale
This self-reporting scale comprises two seven-item scales designed to rate depression and anxiety, respectively [57]. The scores from both scales can be added to produce a total score of emotional distress [58]. Ratings may range from 1 (Almost always) to 4 (Almost never). The Spanish version used in this study [59] has suitable reliability and validity, and the internal consistency of both scales is high. Cronbach’s alpha for this questionnaire was 0.83.
Statistical Analysis
Data were analysed using SPSS (Windows version 19.0, SPSS Inc, Chicago, IL) and AMOS Graphics (version 19.0; Small Waters Corp., Chicago, IL) software.
Univariate and multivariate distributions were examined. Inspection of Mahalanobis d 2 values did not indicate any multivariate outliers in the sample. The multivariate distribution was found to be normal, with a Mardia coefficient of multivariate kurtosis of 0.61. There was no evidence of significant univariate skewness or kurtosis across any of the variables.
As a first step, partial correlations between all the variables considered in the analyses were examined, while controlling for medication use. Because the measured variables were normally distributed, the maximum likelihood estimation method was used. In line with contemporary guidelines, model fit was evaluated using several fit indices and convergence between findings was assessed [60, 61], namely, the Satorra-Bentler chi-square, the root mean square error approximation (RMSEA), the goodness-of-fit index (GFI), the adjusted goodness-of-fit index (AGFI) and the comparative fit index (CFI). The Satorra-Bentler chi-square is a chi-square fit index that corrects the statistic under distributional violations by determining whether the value of this statistic is less than twice the model’s degrees of freedom [61]. Regarding RMSEA, values less than 0.08 indicate an adequate fit. In respect to GFI and AGFI, the closer the values of these indexes are to 1 the better the fit. The CFI measures the proportional improvement in fit by comparing a hypothesized model with a more restricted baseline model. The CFI indexes also range from 0 (absolute lack of fit) to 1 (perfect fit).
Five latent variables—resilience, pain acceptance, experiential avoidance, PTSD symptoms and pain adjustment—were associated in a hypothetical structural equation model. In order to minimize the number of variables in the analysis, pain adjustment as a latent construct was specified by pain intensity (composite pain intensity index), emotional distress (hospital anxiety emotional distress score) and pain disability (Roland-Morris Disability Questionnaire). The rationale of this decision was based on a previous research that has shown not only that adjustment to chronic pain included measures of negative emotions (i.e. depression and anxiety) and of pain disability [62], but that pain intensity seems to be an important predictor of disability for several domains of life [63]. Hence, seven observable variables or indicators of the latent variables were used. One loading for the latent variable was fixed at 1.0 for setting the metric of the latent construct. Resilience, pain acceptance, experiential avoidance and PTSD symptoms were measured by one variable; thus, the error variance was fixed at 0 and the loading value at 1.
Results
Bivariate Analyses
As a first step in the data analysis, partial correlations—while controlling for medication intake—between resilience, pain acceptance, experiential avoidance, PTSD symptoms and pain adjustment variables (pain intensity, disability and emotional distress) were calculated. Table 1 shows descriptive statistics (means and standard deviations) and partial correlations of the measures used in the structural equation analysis.
Resilience was significantly and positively associated to pain acceptance and significantly and negatively associated to experiential avoidance, trauma-related symptoms, pain intensity, pain disability and emotional distress. Pain acceptance was significantly and negatively associated to experiential avoidance, trauma-related symptoms, pain intensity, pain disability and emotional distress. Experiential avoidance was significantly and positively associated to trauma-related symptoms, pain intensity, pain disability and emotional distress. PTSD symptoms were significantly and positively related to pain intensity, pain disability and emotional distress. Pain intensity, pain disability and emotional distress were significantly and positively inter-correlated.
Measurement Model
Seven observable variables or indicators of the latent variables were used. Pain adjustment as a latent construct was specified by pain intensity (pain intensity index), pain disability (Roland-Morris Disability Questionnaire) and emotional distress (Hospital Anxiety and Depression Scale total score).
The structural equation analysis was used as a preliminary test of the model to determine if the pattern of relationships between the included measures was as expected. The overall pattern of results broadly supported the hypothetical model. The initial evaluation of the model indicated a good fit with the data (see Table 2). However, evaluation of the measurement model showed that the direct path between resilience and experiential avoidance was non-significant (β = 0.03, p = 0.70). The model was therefore altered by eliminating this path, and fit was evaluated again. The results of evaluating the final model are shown in Table 2. Fit indices indicated an excellent fit to the data, with decreases of Satorra-Bentler chi-square and RMSEA values, a closer value of AGFI to 1 and a perfect fit of CFI value.
The final model as well as standardized coefficients and R 2 values are shown in Fig. 1, with R 2 values shown above each endogenous variable.
Empirical model. Standardized path coefficients are presented. RS Resilience Scale, CPAQ Chronic Pain Acceptance Questionnaire, AAQ Action and Acceptance Questionnaire, DTS Davidson Trauma Scale, INDEX composed pain intensity index, RMDQ Roland-Morris Disability Questionnaire; HADS-T Hospital Anxiety and Depression Scale total score. Latent variables are represented by circles and observed variables by squares. All paths are significant at p < 0.05
According to the results, resilience yielded two statistically significant path coefficients. The first one to pain acceptance (explaining 44 % of the variance of this variable) with higher levels of resilience related to higher levels of pain acceptance. The second was to trauma-related symptoms with individuals reporting higher levels of resilience reporting lower levels of trauma-related symptoms. Pain acceptance yielded a statistically significant path coefficient to experiential avoidance (explaining 7 % of the variance) and to pain adjustment. The results indicate that higher levels of pain acceptance were related to lower levels of experiential avoidance, pain intensity, pain disability and emotional distress. Experiential avoidance yielded two statistically significant path coefficients. The first one was to trauma-related symptoms (explaining 42 % of the variance of this variable, in combination to resilience) and the one second was to pain adjustment. According to the data, higher levels of experiential avoidance are associated to higher levels of trauma-related symptoms, pain intensity, pain disability and emotional distress. Trauma-related symptoms yielded a statistically significant path coefficient to pain adjustment, with individuals characterized with more of these symptoms reporting higher levels of pain intensity, pain disability and emotional distress. The variance of pain adjustment (55 % of the explained variance) depended on the combined effects of pain acceptance—which diminished pain intensity, disability and emotional distress—and trauma-related symptoms and experiential avoidance, which increased the aforementioned variables.
Discussion
This study tested a hypothetical model of the contribution of experiential avoidance, resilience and pain acceptance to pain adjustment in a sample of chronic back pain patients who experienced a traumatic event before the onset of pain and had trauma-related symptoms. It was predicted that experiential avoidance would be positively related to trauma-related symptoms, resilience would be negatively related to experiential avoidance and trauma-related symptoms and pain acceptance would be negatively associated with experiential avoidance. The hypothetical model also predicted a direct effect of experiential avoidance, pain acceptance and trauma-related symptoms on adjustment to chronic pain (i.e. pain intensity, pain disability and emotional distress). The findings provide empirical support for the majority of these hypotheses.
Regarding experiential avoidance, the results of the current study are in line with those obtained in previous studies [13, 20–22] showing that this variable is associated with worse adjustment to pain (with higher levels of pain intensity, pain disability and emotional distress related to higher levels of experiential avoidance). These findings are consistent with the definition of experiential avoidance as a process characterized as a rigid and inflexible emotion regulation strategy that represents the unwillingness to remain in contact with aversive private experiences [17]. These results seem to reflect that when individuals with chronic back pain try to control the negative emotional experiences that are related to experiencing pain, they increase their suffering. This seemingly paradoxical effect probably occurs because the struggle to control pain serves as an experientially avoidant function which represents a maladjusted attempt to manage pain.
In addition, there is a well-documented relationship between experiential avoidance and psychopathology, and it has been argued that it is both a vulnerability and maintaining factor for PTSD [23–25]. Thus, it is unsurprising that the results of this study show a positive link from experiential avoidance to trauma-related symptoms, as predicted. In this regard, the cognitive theory formulated by Ehlers and Clark [64] assumes that people who tend to avoid negative emotions may be more likely to use avoidance-based ways of coping and therefore could be more vulnerable to persistent PTSD symptoms. Taken as a whole, the findings of the current study support the hypothesis that experiential avoidance is a significant predictor not only of psychological functioning, but also of physical functioning. Importantly, these results indicate that when chronic back pain patients attempt to escape and avoid unpleasant emotions, thoughts, memories and other private experiences, not only are trauma-related symptoms exacerbated, but this symptomatology—in combination with the unwillingness to experience undesirable negative private events—is likely to reduce pain adjustment. Moreover, it must be borne in mind that the percentage of explained variance of pain adjustment was 55 %.
Pain acceptance also contributed to this explained variance. Acceptance of pain includes responding to pain-related experiences without attempts at control or avoidance, engaging in valued activities and reaching personal goals regardless of these experiences [65]. In fact, this variable has been recently identified as a relevant element in the psychological treatment of chronic pain patients [66]. Similar to previous studies [65, 67, 68], the findings show that pain acceptance is associated with reports of less pain intensity and enhanced emotional and physical functioning in chronic back pain patients. Pain acceptance has been defined according to two different mechanisms: willingness to experience pain and activity engagement despite experiencing pain [31]. In line with this, pain acceptance has been considered to be the opposite of experiential avoidance [27]. The results of the current study provide empirical support to this assertion, as they show that the higher the level of pain acceptance, the lower the level of experiential avoidance. In contrast to confronting pain by avoidance, the willingness to undergo undesirable psychological experiences is likely to enhance overall functioning. The results support this, as they show that pain acceptance is negatively associated with pain intensity, pain disability and emotional distress. That is, it seems that pain acceptance predicts better adjustment to chronic pain. This is in line with previous research [32, 65], which highlights this variable as a form of pain confrontation that represents a positive pathway to pain adjustment. Thus, it is understandable that acceptance and commitment therapy (ACT) has been recently listed by Division 12 of the American Psychological Association as an empirically validated treatment for chronic pain [69]. In the case of PTSD, there is also increasing evidence that ACT is a potentially effective treatment [24].
A process central to ACT is psychological flexibility, which not only involves acceptance, but the ability to persist and to be guided by one’s own values [70]. This attitude may protect individuals from engaging in emotional and behavioural avoidance that in turn exacerbate symptoms and impairment. Therefore, a resilient attitude may be considered as a salutogenic factor. There is broad consensus that resilience represents the ability to adapt to stressful circumstances. This ability could be considered to be a dynamic process that involves overcoming the negative effects of exposure to risk (i.e. a traumatic event), successfully coping with adverse experiences and avoiding negative trajectories associated with risk. In the specific context of chronic pain, resilience also involves the ability of patients facing a disabling physical illness to maintain relatively stable levels of psychological, emotional and social functioning [41]. The results not only provide empirical support to this, but confirm that resilience buffers the effects of trauma-related symptomatology on pain adjustment [34, 36]. According to the current findings, resilience seems to represent a main factor in adaptation to a chronic back pain condition, not only due to its role in pain adjustment (promoting pain acceptance), but also due to its role regarding the effects of stressful and negative experiences on the experience of chronic pain (reducing the impact of trauma-related symptoms after the occurrence of a traumatic event). Of interest, resilience is clearly negatively associated with trauma-related symptoms (with a large effect size of −0.62). These results are consistent with the proposals and findings of previous studies [34, 36, 42], highlighting resilience as a protective factor that mediates the association between exposure to traumatic events and the development of PTSD symptoms. It is worth noting that the findings of the present study indicate that this symptomatology has a direct effect on adjustment to pain, accounting for a significant proportion of the variance in this outcome variable. Thus, the presence of trauma-related symptoms is positively associated with the intensity of pain, the level of pain disability and emotional distress, with higher levels of trauma-related symptomatology related to higher levels of pain intensity, pain disability and emotional distress. These results are consistent with the findings of previous research [10, 71]. Furthermore, the relationship of both PTSD and chronic pain to increased disability and distress is well documented in the literature [72].
Although we are not aware of any studies that have investigated both variables in samples of either chronic pain or patients with PTSD, it seemed reasonable to consider that resilience may reduce experiential avoidance. Nevertheless, although Pearson’s coefficient correlation was weak although significant (r = −0.15), path analysis did not support this association. Taking into account the measure that was employed for the assessment of resilience in this study, this variable reflects the ability of patients facing chronic pain to maintain relatively stable levels of psychological, emotional and social functioning [41]. Experiential avoidance has been conceptualized as a dysfunctional way of regulating negative emotions that leads to the constant attempt to avoid unpleasant emotions, thoughts and other negative private experiences [17]. Hence, resilience seems to be a process that not only involves an emotional regulatory process, but a way of coping with adversity in which personal competence and acceptance of self and life are important features.
Taken as a whole, the findings of the current investigation provided direct support for the speculation that experiential avoidance may play an important role in the maintenance of psychological difficulties following a traumatic experience. Once the pain occurs, this may then interfere with the processing of pain as a feared stimulus. This motivates the avoidance of internal and external experiences associated with it and a worst adjustment to pain. Conversely, resilient sufferers of traumatic events are more likely to accept the pain without attempting to control it and engage in valued activities, regardless of pain. Hence, pain acceptance could be considered to be a positive pathway to pain adjustment. However, as the work in this area is quite sparse, the findings obtained in this study need to be further explored before advocating any particular therapy model for chronic pain patients with trauma-related symptoms. Yet, ACT seems promising as an intervention in this context as it appears that the strategy of learning how to live with pain may be more functional in the long term than the strategy of attempting to learn how to live without it.
Although the current study is of interest, it has limitations which must be taken into account. First, the analyses were conducted on cross-sectional, self-report data collected at the time of enrolment. It is therefore impossible to determine the exact nature of the associations between the variables studied or to form conclusions on cause-and-effect relationships. Although the inclusion criteria required participants to have experienced trauma prior to the onset of pain symptoms and that it was specified in the SEM that PTSD symptoms predicted pain outcomes, it is possible that the causal pathway could be in the opposite direction. In addition, shared method variance may have contributed to the magnitude of some correlations. Second, the study sample consisted of patients with chronic musculoskeletal pain (specifically, neck and back pains). Thus, the findings of the present study may only be generalizable to patients with specific pain complaints. Third, the possible influence of pain interventions other than medication intake (e.g. physiotherapy, activity-related instructions, counselling) was not controlled. Taking these limitations into account, future studies on the pattern of associations between trauma-related symptoms, PTSD and pain outcomes should be longitudinal and use large samples of patients with different pain disorders.
In spite of these limitations, the results of this study demonstrate the role of a vulnerability pathway (i.e. experiential avoidance) and a protective pathway (i.e. resilience and pain acceptance) in adaptation to pain after a traumatic event. Furthermore, the structural analysis shows that the two pathways are interconnected. Taking this into account, intervention programs for chronic pain patients with trauma-related symptoms as well as PTSD should include therapeutic techniques aimed at affecting both pathways. The promotion of pain acceptance as a protective variable may reduce the potential for psychological vulnerability—that is, experiential avoidance—to both disorders. Identifying patients who have low levels of pretreatment resilience may provide interventions with added benefit, as this could enhance the psychological flexibility needed to achieve greater adjustment to a chronic pain condition by reducing unwillingness to endure upsetting negative private experiences and other forms of avoidance.
References
Casey CY, Greenberg MA, Nicassio PM, Harpin RE, Hubbard D. Transition from acute to chronic pain and disability: A model including cognitive, affective, and trauma factors. Pain. 2008; 134: 69-79.
Jones GT, Power C, McFarlane GJ. Adverse events in childhood and chronic widespread pain in adult life: Results from the 1958 British cohort Study. Pain. 2009; 143: 92-96.
Kindler LL, Jones KD, Perrin N, Bennett RM. Risk factors predicting the development of widespread pain from a chronic back or neck pain. J Pain. 2010; 11: 1320-1328.
Rivara FP, Mackenzie EJ, Jurkovich GJ, et al. Prevalence of pain in patients 1 year alter major trauma. Arch Surv. 2008; 143: 282-287.
Sachs-Ericsson N, Kendall-Tackett K, Hernandez A. Childhood abuse, chronic pain, and depression in the National Comorbidity Survey. Child Abuse Negl. 2007; 31: 531-547.
Otis JD, Keane TM, Kerns RD. An examination of the relationship between chronic pain and posttraumatic stress disorder. J Rehabil Res Dev. 2003; 40: 397-405.
Shipherd JC, Keyes M, Jovanovic T, et al. Veterans seeking treatment for posttraumatic stress disorder: What about comorbid chronic pain? J Rehabil Res Dev. 2007; 44: 153-166.
Asmundson GJG, Coons MJ, Taylor S, Katz J. PTSD and the experience of pain: Research and clinical implications of shared vulnerability and mutual maintenance models. Can J Psychiatry. 2002; 47: 930-937.
Asmundson GJG, Hadjistavropolous HD. Addressing shared vulnerability for comorbid PTSD and chronic pain: A cognitive-behavioral perspective. Cogn Behav Pract. 2006; 13: 8-16.
Martin AL, Halket E, Asmundson GJG, Flora DB, Katz J. Posttraumatic stress symptoms and the diathesis-stress model of chronic pain and disability in patients undergoing major surgery. Clin J Pain. 2010; 26: 518-527.
Sharp TJ, Harvey AG. Chronic pain and posttraumatic stress disorder: Mutual maintenance? Clin Psychol Rev. 2001; 21: 857-877.
Vlaeyen JWS, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain. 2000; 85: 317-332.
Esteve MR, Ramírez-Maestre C, López-Martínez AE. Experiential avoidance and anxiety sensitivity as dispositional variables and their relationship to the adjustment to chronic pain. Eur J Pain. 2012; 16: 718-726.
Zettle RD, Hocker TR, Mick KA, Scofield BE. Differential strategies in coping with pain as a function of level of experiential avoidance. Psychol Rec. 2005; 55: 511-524.
Marx BP, Sloan DM. Peritraumatic dissociation and experiential avoidance as predictors of posttraumatic stress symptomatology. Behav Res Ther. 2005; 43: 569-583.
Tull MT, Gratz KL, Salters K, Roemer L. The role of experiential avoidance in posttraumatic stress symptoms and symptoms of depression, anxiety and somatization. J Nerv Ment Dis. 2004; 192: 754-761.
Hayes SC, Wilson KG, Gifford E, Follette VM, Strosahl KD. Emotional avoidance and behaviour disorders: A functional dimensional approach to diagnosis and treatment. J Consult Clin Psychol. 1996; 64: 1152-1168.
Kashdan TB, Barrios V, Forsyth JP, Steger MF. Experiential avoidance as a generalized psychological vulnerability: Comparisons with coping and emotion regulation strategies. Behav Res Ther. 2006; 44: 1301-1320.
Costa J, Pinto-Gouveia JP. Experiential avoidance and self-compassion in chronic pain. J Appl Soc Psychol. 2013; 43: 1578-1591.
Costa J, Pinto-Gouveia JP. The mediation effect of experiential avoidance between coping and psychopathology in chronic pain. Clin Psychol Psychother. 2011; 18: 34-47.
Esteve R, Ramírez-Maestre C. Pain fear avoidance and pain acceptance: A cross-sectional study comparing their influence on adjustment to chronic pain across three samples of patients. Ann Behav Med. 2013; 46: 169-180.
Orsillo SM, Batten SV. Acceptance and commitment therapy in the treatment of posttraumatic stress disorder. Behav Modif. 2005; 29: 95-129.
Morina N, Stangier U, Risch AK. Experiential avoidance in civilian war survivors with current versus recovered posttraumatic stress disorder: A pilot study. Behav Change. 2008; 25: 15-22.
Thompson RW, Arnkoff DB, Glass CR. Conceptualizing mindfulness and acceptance as components of psychological resilience to trauma. Traum Violence Abuse. 2011; 12: 220-235.
Kashdan TB, Morina N, Priebe S. Post-traumatic stress disorder, social anxiety disorder, and depression in survivors of the Kosovo War: Experiential avoidance as a contributor to distress and quality of life. J Anxiety Disord. 2009; 23: 185-196.
Gómez-Pérez L, López-Martínez AE. Association of trauma, posttraumatic stress disorder and experimental pain response in healthy young women. Clin J Pain. 2013; 29: 425-434.
Kashdan TB, Breen WE. Social anxiety and positive emotions: A prospective examination of a self-regulatory model with tendencies to suppress or express emotions as moderating variables. Behav Ther. 2008; 39: 1-12.
Orsillo SM, Roemer L, Barlow DH. Integrating acceptance and mindfulness into existing cognitive-behavioral treatment for GAD: A case study. Cogn Behav Pract. 2003; 10: 222-230.
McCracken LM. Learning to live with pain: Acceptance of pain predicts adjustment in persons with chronic pain. Pain. 1998; 74: 21-27.
McCracken LM, Vowles KE, Eccleston C. Acceptance of chronic pain: Component analysis and a revised assessment method. Pain. 2004; 107: 159-166.
McCracken LM, Zhao-O’Brien J. General psychological acceptance and chronic pain: There is more to accept than the pain itself. Eur J Pain. 2010; 14: 170-175.
McCracken LM, Samuel VM. The role of avoidance, pacing, and other activity patterns in chronic pain. Pain. 2007; 130: 119-125.
McCracken LM, Eccleston C. A prospective study of acceptance and patient functioning with chronic pain. Pain. 2005; 118: 164-169.
Bensimon M. Elaboration on the association between trauma, PTSD and posttraumatic growth: The role of trait resilience. Personal Individ Differ. 2012; 52: 782-787.
Kashdan TB, Kane JQ. Post-traumatic distress and the presence of post-traumatic growth and meaning in life: Experiential avoidance as moderator. Personal Individ Differ. 2011; 50: 84-89.
Fincham DS, Altes LK, Stein DJ, Seedat S. Posttraumatic stress disorder symptoms in adolescents: Risk factors versus resilience moderation. Compr Psychol. 2009; 50: 193-199.
López-Martínez AE, Ríos-Velasco L, Ruiz-Párraga GT, Esteve R, Sánchez-Reyna A. The role of resilience and acceptance versus catastrophizing and pain-related fear in chronic pain adjustment. Eur J Pain. 2009; 13(supp): 970.
Ramírez-Maestre C, Esteve R, López-Martínez AE. The path to capacity: Resilience and spinal chronic pain. Spine. 2012; 37: E251-E258.
Ruiz-Párraga GT, López-Martínez AE. The contribution of posttraumatic stress disorder to chronic pain adjustment. Health Psychol. 2014. doi:10.1037/hea0000040.
Ruiz-Párraga GT, López-Martínez AE, Gómez-Pérez L, Ramírez-Maestre C, Barranquero I. Traumatic event stories, PTSD symptoms, resilience, pain acceptance, procedural variables and disability in women with chronic pain. Eur J Pain. 2009; 13(supp): S271.
Ruiz-Párraga GT, López-Martínez AE, Gómez-Pérez L. Factor structure and psychometric properties of the Resilience Scale in a chronic musculoskeletal pain sample. J Pain. 2012; 13: 1090-1098.
McFarlane AC, van Hooff M, Goodhew F. Anxiety disorders and PTSD. In: Neria Y, Galea S, Norris FH, eds. Mental Health and Disorders. New York: Cambridge University Publishers; 2009: 47-66.
Whealin JM, Stotzer R, Nelson D, Fengand L, Liu-Tom HT, Pietrzak RH. Evaluating PTSD prevalence and resilience factors in a predominantly Asian American and Pacific Islander sample of Iraq and Afghanistan Veterans. J Affect Dis. 2013; 150: 1062-1068.
Jensen MP, Turner P, Romano JR, Fisher LD. Comparative reliability and validity of chronic pain intensity measures. Pain. 1999; 83: 157-162.
Davidson JRT. Davidson Trauma Scale. Nueva York: Multi-Health Systems, Inc.; 1996.
Green BL, Chung JY, Daroowalla A, Kaltman S, DeBenedictis C. Evaluating the cultural validity of the stressful life events screening questionnaire. Violence Against Women. 2006; 12: 1191-1213.
Goodman L, Corcoran C, Turner K, Yuan N, Green BL. Assessing traumatic event exposure: General issues and preliminary findings for the Stressful Life Events Screening Questionnaire. J Trauma Stress. 1998; 11: 521-542.
Davidson JRT, Book SW, Colket JT, et al. Assessment of a new self-rating scale for posttraumatic stress disorder. Psychol Med. 1997; 27: 153-160.
Davidson JRT, Tharwani HM, Connor KM. Davidson Trauma Scale (DTS): Normative scores in the general population and effect sizes in placebo-controlled SSRI trials. Depress Anxiety. 2002; 15: 75-78.
Bobes J, Calcedo-Barba A, García M, et al. Evaluación de las propiedades psicométricas de la versión española de cinco cuestionarios para la evaluación del trastorno de estrés postraumático. Actas Esp Psiquiatr. 2000; 28: 207-218.
Wagnild FM, Young HM. Development and psychometric evaluation of the Resilience Scale. J Nurs Meas. 1993; 1: 165-178.
Hayes SC, Strosahl K, Wilson KG, Bissett RT, Pistorello J, Toarmino D. Measuring experiential avoidance: A preliminary test of a working model. Psychol Rec. 2004; 54: 553-578.
Barraca J. Spanish adaptation of the acceptance and action questionnaire. Int J Psychol Psychol Ther. 2004; 4: 505-515.
Bendayan R, Esteve R, Blanca MJ. New empirical evidence of the validity of the Chronic Pain Acceptance Questionnaire: The differential influence of activity engagement and pain willingness on adjustment to chronic pain. Br J Health Psychol. 2012; 17: 314-326.
Roland MO, Morris RW. A study of the natural history of back pain. Part 1: Development of a reliable and sensitive measure of disability in low back pain. Spine. 1983; 8: 141-144.
Kovacs FM, Llobera J, Gil del Real MT, Abraira V, Gestoso M, Fernández C. Validation of the Spanish version of the Roland Morris Questionnaire. Spine. 2002; 2: 149-151.
Zigmond S, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983; 67: 361-370.
Aben I, Verhey F, Lousberg R, Lodder R, Honing G. Validity of the Beck depression inventory, hospital anxiety and depression scale, SCL-90, and Hamilton depression rating scale as screening for depression. Psychosomatics. 2002; 43: 386-393.
Quintana JM, Padierna A, Esteban C, Arostegui I, Bilbao A, Ruiz I. Evaluation of the psychometric characteristics of the Spanish Version of the Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 2003; 107: 216-221.
Byrne BM. Structured Equation Modeling with AMOS. Basic Concepts, Applications, and Programming. 2nd ed. New York: Taylor and Francis; 2010.
Ullman JB. Structural equation modelling. In: Tabachnick BG, Fidell LS, eds. Using Multivariate Statistics. Needham Heights: Allyn and Bacon; 2001: 653-711.
McCracken LM, Eccleston C. Coping or acceptance: What to do about chronic pain? Pain. 2003; 105: 197-204.
Silva AG, Alvarelhão J, Queirós A, Rocha NP. Pain intensity is associated with self-reported disability for several domains of life in a sample of patients with musculoskeletal pain aged 50 or more. Disabil Health J. 2013; 6: 369-376.
Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behav Res Ther. 2000; 38: 319-345.
Esteve MR, Ramírez-Maestre C, López-Martínez AE. The role of pain acceptance, coping strategies and pain-related cognitions. Ann Behav Med. 2007; 33: 179-188.
Wetherell JL, Afari N, Rutledge T. A randomized, controlled trial of acceptance and commitment therapy and cognitive behavioural therapy for chronic pain. Pain. 2011; 152: 2098-2107.
Viane I, Crombez G, Eccleston C, Devulder J, De Corte W. Acceptance of the unpleasant reality of chronic pain: Effects upon attention to pain and engagement with daily activities. Pain. 2004; 112: 282-288.
Vowles KE, McNeil DW, Gross RT, McDaniel ML, Mouse A, Bates M. Effects of pain acceptance and pain control strategies on physical impairment in individuals with chronic low back pain. Behav Ther. 2007; 38: 412-425.
Wicksell RK, Gunnar LO, Hayes SC. Mediators of change in acceptance and commitment therapy for pediatric chronic pain. Pain. 2013; 152: 2792-2801.
Hayes SC, Strosahl KD, Wilson KG. Acceptance and Commitment Therapy: An Experiential Approach to Behavior Change. New York: Guildford Press; 1999.
Katz J, Asmundson GJ, McRae K, Halket E. Emotional numbing and pain intensity predict the development of pain disability up to one year alter lateral thoracotomy. Eur J Pain. 2009; 13: 870-878.
Moeller-Bertram T, Keltner J, Strigo IA. Pain and post traumatic stress disorder-review of clinical and experimental evidence. Neuropharmacology. 2012; 62: 586-597.
Acknowledgments
We thank the physicians of Cruz de Humilladero, Carranque, Puerta Blanca, Teatinos and the Carihuela Primary Health Care Centres, both in Málaga, Spain, for their help in data collection. The authors wish to thank anonymous reviewers whose comments and suggestions aided in the preparation of this article. This work was partly supported by grants from the Andalusian County Council (HUM-566; P07-SEJ-3067) and the Spanish Ministry of Science and Innovation (PSI2008-01803/PSIC). Gema T. Ruiz-Párraga received a grant from the Regional Government of Andalusia (Proyectos Excelencia 2008–2012).
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards
Alicia E. López-Martínez and Gema T. Ruiz Párraga declare that they have no conflict of interest. All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 17 kb)
About this article
Cite this article
Ruiz-Párraga, G.T., López-Martínez, A.E. The Role of Experiential Avoidance, Resilience and Pain Acceptance in the Adjustment of Chronic Back Pain Patients Who Have Experienced a Traumatic Event: a Path Analysis. ann. behav. med. 49, 247–257 (2015). https://doi.org/10.1007/s12160-014-9654-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-014-9654-3