Abstract
Background
Effects of different sources of medical uncertainty on people’s health-related cognitions, emotions, and decision making have yet to be systematically examined.
Purpose
The aim of this study is to examine how uncertainties arising from different sources are associated with decision making regarding stem cell transplantation in Fanconi anemia, a rare, inherited bone marrow failure syndrome that typically presents during childhood.
Methods
Data were collected through a cross-sectional survey of 178 parents of 126 Fanconi anemia patients.
Results
Two distinct sources of uncertainty were associated with decision outcomes: probability was associated with a lower likelihood of choosing stem cell transplantation, and ambiguity due to conflicting expert opinions was associated with greater decision-making difficulty. Concern about transplantation may mediate these associations.
Conclusions
Different sources of uncertainty have different effects on Fanconi anemia treatment decisions, which may be mediated by parents’ emotional reactions. Further research is needed to elucidate these effects and help Fanconi anemia families cope with uncertainty.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Medicine and healthcare provide numerous situations in which people may experience uncertainty, defined as the subjective perception of ignorance [1]. For example, people may perceive uncertainty when expert opinions regarding cancer screening recommendations conflict, when evidence about a treatment’s efficacy in a clinical trial is limited, or when disease risk estimates provided by online risk calculators, direct-to-consumer genetic testing, or healthcare providers are imprecise. These and other situations necessitate an understanding of how people interpret and respond to uncertain information. This need is particularly salient given the current emphasis on shared and informed decision making in the clinical encounter [2, 3], and people’s exposure to complex, contradictory, or incomplete health-related messages [4–7].
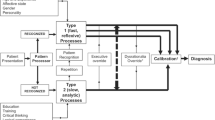
Medical uncertainty can be conceptualized as a multidimensional construct. Scholars have described various views of the construct of uncertainty [8–11]; however, here we focus on a taxonomy recently developed by Han and colleagues [1] for categorizing different types of uncertainty in healthcare. Informed by theoretical and empirical work in disciplines including communication, decision sciences, and psychology, their taxonomy describes three distinct dimensions of uncertainty (see Fig. 1). Source, the dimension of primary interest in the present study, encompasses probability (i.e., first-order or “aleatory” uncertainty about the risk of an event arising from the randomness or indeterminacy of the future), ambiguity (i.e., second-order or “epistemic” uncertainty regarding the strength, validity, consistency, or adequacy of risk information), and complexity (i.e., aspects of an event that make it difficult to comprehend, such as multiple possible causes or outcomes) [1]. Issue, an additional dimension that refers to the substantive content of the uncertainty, includes scientific (i.e., disease-centered, regarding diagnosis, prognosis, and treatment), practical (i.e., healthcare system-centered), and personal (i.e., patient-centered) uncertainty. Finally, locus refers to where uncertainty resides—in the mind of a patient, his/her healthcare provider, both, or neither. With the present study, we focused on several sources of medical uncertainty that are supported by a limited but growing body of empirical research on their psychological effects (described below), and examined these sources while holding the other dimensions constant (issue: scientific and locus: patient).
Sources of uncertainty in healthcare, based on the taxonomy proposed by Han, Klein, and Arora [1]. In the present study, the bolded sources of uncertainty were examined, with the other proposed dimensions of uncertainty, issue and locus, held constant at the levels of scientific and patient, respectively. Figure modified from the original published in [1] published by SAGE Publications, all rights reserved. © 2011, Society for Medical Decision Making
Han and colleagues’ [1] model provides a useful organizational framework for understanding the nature of medical uncertainty but does not explicitly specify how different sources of uncertainty influence people’s cognitions, emotions, and decisions. However, different sources of uncertainty do appear to have distinct effects. For example, probability engenders distinct behavioral responses, such as risk seeking or risk aversion, which vary depending on the magnitude of probability and whether losses or gains are at stake [12]. At the same time, ambiguity has characteristic effects that are distinct from those of probability itself. People have been shown to demonstrate “ambiguity aversion” [13] when presented with risk information that is ambiguous (lacking in reliability, credibility, or adequacy), such that they tend to form pessimistic appraisals of these risks and avoid decision making. Empirical evidence suggests that “ambiguity aversion” influences judgment and decision making in diverse contexts including healthcare. For instance, perceptions of ambiguity regarding cancer screening recommendations are associated with lower perceptions of the preventability of cancer, greater perceptions of cancer risk, and greater worry about cancer [14]. Similarly, perceptions of ambiguity regarding contradictory mammography recommendations have been shown to be associated with lower intentions to use mammography, lower future uptake of mammography, and greater mammography-related worry [15]. Qualitative research has also suggested that ambiguity regarding the benefits and risks of human papillomavirus (HPV) vaccines interferes with Appalachian women’s ability to make vaccination decisions; specifically, women remain in decision-making limbo for extended periods of time [16].
Although ambiguity is a distinct source of medical uncertainty, past research has suggested that ambiguity itself is not a unidimensional construct; rather, different kinds of ambiguity exist and have differential psychological and behavioral effects. Han and colleagues [1] noted that ambiguity can arise from imprecision in the estimates of an action’s benefits or harms, a lack of information (i.e., missing or insufficient information from which to draw conclusions), or conflict (i.e., disagreement or differences in the interpretation of information) in expert opinions or scientific evidence. Ambiguity arising from conflict may have particularly strong effects. Smithson [17] has shown experimentally that people are especially averse to ambiguity when it arises from conflicting expert opinions as opposed to conflicting scientific evidence. This demonstration of “conflict aversion” [17] suggests that ambiguity arising from conflicting expert opinions may exert a more powerful influence on people’s cognitions, emotions, and decisions than other kinds of ambiguity or sources of uncertainty. For example, exposure to conflicting online information from various expert sources about a medical treatment has been associated with a lower likelihood of choosing treatment [18], and conflicting medication information from sources such as physicians and the Internet has been associated with medication non-adherence [19]. However, this possibility has not been systematically examined, and little past research has attempted to isolate the unique psychological effects of different kinds of ambiguity and sources of uncertainty in healthcare. Understanding these influences is important given the frequency with which people are exposed to conflicting or differing medical opinions and messages from the media, healthcare providers, and other informational resources [4–7]. Investigating these effects may inform the development of clinical communication strategies or interventions that promote adaptive psychological and behavioral responses to medical uncertainty.
The overarching aim of the present study was to address this gap by exploring a health problem and decision-making context with abundant sources of uncertainty. As an example, we chose Fanconi anemia, a rare, inherited, bone marrow failure syndrome with complex and evolving treatment options. Fanconi anemia has an incidence of approximately 1 per 130,000 births, and is associated with characteristic birth defects, aplastic anemia (bone marrow failure), hematologic malignancies, and solid tumors at early ages [20–22]. The greatest increase in risk of severe bone marrow failure commonly occurs in childhood through age 20, acute myeloid leukemia in the teenage years through age 30, and solid tumors from ages 20 and older [23].
Although no cure exists for Fanconi anemia, several treatment options are available for managing hematologic complications. One treatment considered by many patients, as well as their parents and families given the early age of onset for Fanconi anemia-related complications, is hematopoietic stem cell transplantation. The decision to undergo transplant is extremely complicated and difficult, due in part to uncertain probabilities of its net benefits and harms. Stem cell transplantation can cure the bone marrow failure associated with Fanconi anemia, but is physically and psychologically demanding [24–26]. Stem cell transplantation has a substantial risk of morbidity and mortality, and although transplant protocols have improved in recent years, the toxicity of pre-transplantation conditioning regimens involving radiation and/or chemotherapy as well as the potential post-transplant complications of acute or chronic graft-versus-host disease may increase Fanconi anemia patients’ subsequent risk of developing solid tumors [27–30].
Furthermore, ambiguity exists due to both lack of information and conflicting expert opinions about the appropriate pre-transplantation conditioning regimen and transplantation protocol. There is insufficient evidence to inform these decisions because Fanconi anemia is so rare that the numbers of patients in any given protocol are small [31]. Consequently, there are also no clear-cut guidelines and expert opinion varies regarding the appropriate time to undertake transplant. Rather, a number of factors must be weighed including disease stage (e.g., early aplastic anemia versus myelodysplastic syndrome or acute myeloid leukemia), use of alternative treatments including androgens (which can manage aplastic anemia but are not curative), hematopoietic stem cell source and degree of donor and patient human leukocyte antigen match, patient age, infectious complications, and existing institutional protocols [27, 32]. Patient psychosocial needs must also be considered, as transplantation constitutes a major life disruption in terms of school or work, family functioning, and interactions with peers, and can lead to social isolation, physical changes, interruptions in identity development, and associated late and potentially long-term chronic effects of treatment [32–34]. Thus, the sources of uncertainty that exist in this decision-making context are numerous, ranging from the probabilities of potential harms and benefits of stem cell transplantation, to ambiguity arising from a lack of information and conflicting expert opinions and scientific evidence. These uncertainties are likely to emerge whenever disease treatment options are limited and evolving; therefore, these characteristics make Fanconi anemia an ideal context for exploring effects of different sources of uncertainty on treatment decision making.
The Present Study
The effects of different sources of medical uncertainty on people’s cognitive, emotional, and decision-making outcomes have yet to be systematically examined. The primary objectives of this study were to examine how different uncertainties are associated with treatment decision making in the model disorder of Fanconi anemia, and to identify psychosocial factors that may influence these associations. We investigated responses among parents of Fanconi anemia patients to several sources of uncertainty related to stem cell transplantation: probability, ambiguity due to a lack of information, ambiguity due to conflicting expert opinions, and ambiguity due to conflicting scientific evidence.
Based on previous scientific literature, we predicted that, in general, greater perceptions of uncertainty regarding transplant among parents would be associated with a lower likelihood of choosing transplant, as well as greater difficulty in making this treatment decision. We conducted exploratory analyses to determine whether any significant associations between specific sources of uncertainty and treatment decision-making outcomes could be mediated by other psychological factors including the perceived risk of harms of stem cell transplantation, concern about harms of transplantation, and the perceived necessity of transplantation. Such cognitive (i.e., perceived risk and necessity) and affective (i.e., concern) factors have been shown to independently influence health-related decision-making outcomes [35–37]. Although a cross-sectional study cannot test temporal mediation [38], it allows exploration of new hypotheses, particularly when there is theoretical or empirical justification for these hypotheses [39]. The hypothesized relationships explored in this study are based on theory and evidence on the phenomenon of “ambiguity aversion” which has been demonstrated with both cross-sectional [14] and longitudinal [15] investigations, and the influence of cognitive and affective factors on transplant treatment decisions in Fanconi anemia families [40]. We hypothesized that, in general, greater perceived uncertainty would be associated with lower perceived necessity of transplant and greater perceived risk and concern about harms of transplant (consistent with “ambiguity aversion”), which in turn would be associated with a lower likelihood of choosing transplant as well as with greater difficulty in making this treatment decision.
Methods
Participants
In November 2007, participants were recruited into the study from family support organizations in the USA (Fanconi Anemia Research Fund) and Canada (Fanconi Canada). These organizations mailed surveys to 905 members of registered families representing 451 individual Fanconi anemia patients. Individuals who did not respond to the first mailing were sent a second survey 2 months later. Self-report surveys were completed separately by mothers, fathers, adult Fanconi anemia patients (18 years or older at the time of the study), and spouses/significant others of adult patients. For the present study, eligibility was restricted to parents of a patient that had been offered stem cell transplantation. This study was approved by the National Cancer Institute Institutional Review Board (NCI protocol 02-C-0052), and is registered in www.clinicaltrials.gov (NCT00027274).
Measures
Sources of perceived uncertainty were assessed with a four-item scale designed for the present study based on a review of the literature and investigator expertise regarding stem cell transplant in Fanconi anemia. Cognitive testing consisting of individual interviews with 18 healthy volunteers was used to evaluate and refine the items to ensure comprehensibility. Each item was designed to assess respondents’ perceptions of a unique source of uncertainty in Fanconi anemia (abbreviated as “FA” in all items): probability (“even if transplant was helpful for most other FA patients, it may not have been helpful for me/my child”), ambiguity due to a lack of information (“at the time, doctors seemed to have enough scientific evidence to recommend transplant for FA patients;” item was reverse-scored), ambiguity due to conflicting expert opinions (“doctors had differing views about whether FA patients with bone marrow failure should undergo transplant”), and ambiguity due to conflicting scientific evidence (“at the time, research findings about the benefits and harms of transplant seemed to be ‘all over the map’”). Responses to each item were made on a four-point scale ranging from 1 = “strongly disagree” to 4 = “strongly agree”; higher values indicate greater perceived uncertainty due to each source. The four-item scale had poor internal consistency (Cronbach’s α = 0.49), confirming the items’ conceptual independence and thus need to analyze each item individually.
Perceived risk of harms of stem cell transplantation was assessed with an 11-item scale designed by study investigators to measure cognitive beliefs regarding the likelihood of various adverse side effects of transplant (e.g., infection, post-transplant cancer). Items were designed to be similar in phrasing to the other scale measures used in this study (e.g., concern about harms of stem cell transplantation), and used a similar response scale. Respondents indicated how likely they thought it was that the patient would experience each of these side effects on a four-point scale ranging from 1 = “very unlikely” to 4 = “very likely.” Items were averaged to produce a mean scale score; higher values indicate greater perceived risk. Exploratory factor analysis supported the unidimensionality of this scale, and it was internally reliable (Cronbach’s α = 0.83).
Concern about harms of stem cell transplantation was assessed with nine items from the ten-item concerns subscale of the Beliefs about Medicines Questionnaire (BMQ; 35), adapted to address emotional worries about potential harms of transplant. Although the original scale included one item assessing concern regarding “uncertainties about the transplant procedure,” this item was omitted to protect against biased estimates of any associations between sources of perceived uncertainty and concern. For each item, respondents indicated how concerned or worried they were about issues such as emotional side effects and long-term medical complications of transplant on a four-point scale ranging from 1 = “not at all” to 4 = “a great deal.” Items were averaged to produce a mean scale score; higher values indicate greater concern (Cronbach’s α = 0.78).
Perceived necessity of stem cell transplantation was assessed with a five-item scale adapted from the perceived necessity subscale of the BMQ [35]. Respondents indicated how much they agreed with beliefs such as that the patient’s future health would depend on undergoing transplant. Responses were made on a four-point scale ranging from 1 = “not at all” to 4 = “a great deal.” Items were averaged to produce a mean scale score; higher values indicate greater perceived necessity (Cronbach’s α = 0.78).
Outcome variables included the decision to undergo stem cell transplantation and decision-making difficulty. Decision to undergo stem cell transplantation was assessed with a single item which asked “did the patient have a transplant?” Responses were coded as 0 = “no” and 1 = “yes.” Decision-making difficulty was assessed with a single item; respondents indicated how much they agreed with the statement “the decision about undergoing transplant was difficult to make” on a four-point scale ranging from 1 = “strongly disagree” to 4 = “strongly agree.”
Demographic and medical variables assessed with the survey were treated as potential covariates and included the patient’s vital status at time of survey completion, gender, country of birth, age at time of Fanconi anemia diagnosis, primary reason for needing transplant, and the number of individuals involved in the transplant decision. For descriptive purposes, data regarding the respondent’s relationship to the patient, identity of the person(s) responsible for making the transplant decision, and patient age at time of transplant were also examined.
Data Analysis
Data were examined for missing values using SPSS 19.0 Missing Values statistical analysis software. Missing values were not differentially related to any theoretically important variables (e.g., patient vital status at time of survey). Surveys with ≥20 % missing items for any component scale variables were excluded from analysis (n = 9). Because the sampling strategy allowed for survey responses from multiple decision-makers per patient (i.e., mother and father), the data were correlated at the family unit level and violated the assumption of independence between cases. In order to include data from each respondent, all analyses and standard error estimates were corrected to account for the correlated data with the use of SPSS 19.0 Complex Samples statistical analysis software, which used Taylor linearization to compute accurate standard errors for statistical testing. This technique allowed for the inclusion of all decision-makers per patient, thereby maximizing the size of the analytic sample while protecting against inaccurate variance estimates that could arise from such a complex sampling design.
Descriptive statistics and bivariate correlations among study variables were computed, and analyses were conducted to test each of the study hypotheses. All analyses were adjusted to correct for the effects of potential confounding demographic and medical variables including patient’s vital status, gender, country of birth, age at Fanconi anemia diagnosis, primary reason for needing transplant, and number of individuals involved in the transplant decision. Multivariable linear regression was used to examine whether each source of perceived uncertainty was associated with transplant decision-making difficulty; multivariable logistic regression was used to determine whether perceived uncertainty was associated with the decision to undergo stem cell transplantation. All statistical tests were two-tailed with α = 0.05.
We also conducted exploratory mediational analyses to test whether the observed associations were consistent with a multiple mediator model (Fig. 2). Consistent with convention [41], paths a 1−3 represent the direct effects of perceived uncertainty on the proposed cognitive and affective mediators, and paths b 1−3 represent the direct effects of the mediators on the decision outcome variables. The total effect of uncertainty on decision outcomes is represented by path c, and path c’ is the direct effect of uncertainty on decision outcomes controlling for the mediators. The indirect effects are exerted through the proposed mediators. Multivariable linear regression was used to derive coefficients for the effects of perceived uncertainty on decision-making difficulty through the proposed mediator variables of perceived risk, concern, and perceived necessity (tested simultaneously). Logistic regression was used to derive coefficients for the effects of perceived uncertainty on the decision to undergo transplant through the proposed mediators (for these analyses, the potential mediators were dichotomized with a median split). These coefficients were used to compute point estimates for the indirect effects (i.e., the effects of uncertainty on decision outcomes through the potential mediators). The Monte Carlo method [42] was used to compute 95 % confidence intervals (CIs) for the indirect effects. The Monte Carlo method involves directly generating sample statistics (i.e., point estimates) based on the joint asymptotic distribution of the component statistics to obtain multiple estimates of the indirect effects. The Monte Carlo method is comparable to other accepted approaches to CI construction (e.g., bootstrapping), and is appropriate for data obtained through a complex sampling design [42]. A web-based Monte Carlo calculator [43] was used with R statistical analysis software to compute the 95 % CIs based on 20,000 simulated draws for the simple indirect effects (i.e., the effect of a source of uncertainty on a decision outcome variable through a single potential mediator) and the total indirect effects (i.e., the effect of a source of uncertainty on a decision outcome variable through all three potential mediators). Significance of the indirect effects is based upon 95 % CIs that exclude zero.
General proposed mediational model for association between sources of perceived uncertainty about stem cell transplantation and transplantation decision outcomes in parents of Fanconi anemia patients. a Sources of perceived uncertainty are hypothesized to be associated with the decision outcome variables. b Sources of perceived uncertainty are hypothesized to exert indirect effects on the decision outcome variables through the cognitive and affective mediators
Results
Surveys were received from 398 individuals (response rate: 44 %). Of these, 200 were from parents of patients who had been offered transplant, and were thus eligible for the present study. A total of 22 cases with substantial missing data for the study variables (inclusive of the 9 cases noted above with missing scale items) were excluded, resulting in an analytic sample of 178 parents who provided complete responses about their decision-making experiences regarding 126 individual Fanconi anemia patients.
Respondent and Fanconi Anemia Patient Characteristics
As shown in Table 1, most survey respondents (88 %) reported that the patient had received a stem cell transplant. The majority of respondents (61 %) were mothers of patients. Mothers (88 %) and fathers (80 %) were most frequently endorsed as a person responsible for making the transplant decision, with patients (10 %) and other individuals (8 %) endorsed as decision makers less frequently. Fanconi anemia patient characteristics are shown in Table 2; there were no significant differences in any medical or demographic characteristics between those patients who chose transplant and those who did not. A majority of patients were alive at the time of the survey (65 %), were born in the USA (83 %), and had been offered transplant due to aplastic anemia (68 %).
Sources of Perceived Uncertainty and Decision-Making Outcomes
Descriptive statistics and bivariate correlations between study variables are shown in Table 3. Respondents endorsed (on scales ranging from 1 to 4) moderate perceptions of: ambiguity due to conflicting scientific evidence about stem cell transplant (M = 2.47, SD = 0.95), the probabilistic effectiveness of transplant (M = 2.21, SD = 1.07), and ambiguity due to conflicting expert opinions about transplant (M = 2.01, SD = 1.01). Respondents perceived somewhat less ambiguity due to a lack of information about transplant (M = 1.64, SD = 0.89).
We hypothesized that for each source of uncertainty, greater perceptions of uncertainty would be associated with both lower likelihood of choosing stem cell transplant, and with greater difficulty in making this treatment decision. Multivariable logistic regression models, adjusting for patient vital status, gender, country of birth, age, reason for needing transplant, and number of individuals involved in the transplant decision showed that respondents’ perceptions of probability were associated with their decision to undergo transplant (adjusted OR = 0.50, 95 % CI = 0.30 to 0.83, p = 0.008). That is, consistent with predictions, greater perceptions of the probabilistic effectiveness of transplant were associated with decreased odds of choosing to undergo transplant. However, there was no significant association between probability and respondents’ decision-making difficulty (adjusted β = 0.13, p = 0.17). Perceived ambiguity due to a lack of information was associated with neither the decision to undergo transplant (adjusted OR = 0.80, 95 % CI = 0.50 to 1.28, p = 0.36), nor respondents’ decision-making difficulty (adjusted β = 0.09, p = 0.42). Respondents’ perceptions of ambiguity due to conflicting expert opinions were not significantly associated with their decision to undergo transplant (adjusted OR = 0.82, 95 % CI =0.55 to 1.22, p = 0.32), although they were significantly associated with greater decision-making difficulty (adjusted β = 0.26, p = 0.002). Perceived ambiguity due to conflicting scientific evidence was not associated with the decision to undergo transplant (adjusted OR = 0.72, 95 % CI = 0.45 to 1.15, p = 0.16), nor with decision-making difficulty (adjusted β = 0.02, p = 0.85).
Exploratory Mediation Analyses
The pattern of results regarding how different sources of uncertainty were associated with decision outcomes elucidated specific areas for further investigation through exploratory mediation analyses. We accordingly examined whether the cognitive factors of perceived risk and perceived necessity of stem cell transplantation, and the affective factor of concern about harms of stem cell transplantation could mediate the observed significant associations between: (1) perceived probability and the decision to undergo transplant; and (2) perceived ambiguity due to conflicting expert opinions and decision-making difficulty. The direct paths from these two sources of uncertainty to the proposed mediators and from the mediators to the decision outcomes are shown in Table 4; the Monte Carlo-computed 95 % CIs for the simultaneously tested indirect effects are shown in Table 5.
After adjusting for the effects of demographic and medical variables, results were consistent with the proposed meditational model such that the set of cognitive and affective factors mediated the association between perceived probability and the decision to undergo transplant. The total and direct effects of probability were −0.7010 (p = 0.008), and −0.5170 (p = 0.08), respectively. The total indirect effect through the three mediators was −1.0235, Monte Carlo 95 % CI = −2.2520 to -0.0711 (note that the total indirect effect does not equal the difference between the total and direct effects due to differences in the scales of these values when using logistic regression and a dichotomous outcome variable [41]). When specific indirect effects were examined, only concern about harms of transplant remained a significant mediator after controlling for perceived risk and necessity (point estimate = −0.8620, Monte Carlo 95 % CI = −1.9510 to −0.1020). As predicted, greater perceptions of the probabilistic effectiveness of transplant were associated with increased odds of experiencing high levels of concern, which in turn was associated with decreased odds of choosing to undergo transplant. Additionally, there was a greater odds of choosing to undergo transplant when the patient needed transplant due to aplastic anemia as opposed to other reasons (p = 0.03).
Consistent with the proposed meditational model, adjusted analyses suggested that the set of cognitive and affective factors could also mediate the association between perceived ambiguity due to conflicting expert opinions and decision-making difficulty. The total and direct effects of ambiguity due to conflicting expert opinions on decision-making difficulty were 0.2610, p = 0.002, and 0.1940, p = 0.02, respectively. The difference between the total and direct effects was the total indirect effect through the three mediators (point estimate = 0.0673, Monte Carlo 95 % CI = 0.0055 to 0.1408). When specific indirect effects were examined, only concern about harms of transplant remained a significant mediator after controlling for the other potential mediators (point estimate = 0.0374, Monte Carlo 95 % CI = 0.0020 to 0.0866). Consistent with our predictions, greater perceptions of ambiguity due to conflicting expert opinions about transplant were associated with greater concern about transplant, which in turn was associated with greater decision-making difficulty. Additionally, less decision-making difficulty was reported when the patient was born in the USA and needed the transplant due to aplastic anemia (p ≤ 0.04).
Discussion
The majority of Fanconi anemia patients and their families will face the challenging decision of whether to undergo stem cell transplantation as a means of treating hematologic complications of the disease. The difficulty in making this decision comes from a variety of uncertainties arising from multiple sources. The present study is the first to systematically examine the unique associations of these various uncertainties with Fanconi anemia parents’ decision-making experiences. Results suggest that different uncertainties may have different effects on Fanconi anemia treatment decisions.
As hypothesized, greater perceived probability—the perception of future outcomes as random or indeterminate—was associated with a lower likelihood of choosing transplant; however, it was not associated with decision-making difficulty. The choice of stem cell transplantation requires families to weigh diverse, patient-specific medical, psychosocial, and institutional factors in the face of limited empirical data on the influence of these factors on patient outcomes. This results in substantial uncertainty about the net benefits and harms of transplant for individual Fanconi anemia patients. Our data suggest a preference or bias against intervention when uncertainty arises from probability; however, the mechanisms of this bias favoring the status quo are unclear. On the one hand, it could reflect a pessimistic focus on the unknown, potentially painful, long-term, or lethal complications of transplant. On the other hand, this bias could reflect an optimistic focus on individual characteristics that may lower patients’ risks for adverse health outcomes (thus undermining the need to proceed to transplant) but that are unaccounted for in experts’ prognostic estimates. In these ways, perceived probability may serve to facilitate the influence of either pessimistic or optimistic motivations and appraisals that both promote a preference for the status quo and against intervention. More research is needed to test these and other potential explanations for our findings.
As predicted, greater perceived ambiguity due to conflicting expert opinions was associated with greater difficulty in making the transplant decision. This finding is consistent with reports of the key roles played by medical professionals in this context [40, 44]. Because of the high-stakes nature of the transplant decision, Fanconi anemia families may rely heavily on expert opinion or may even prefer to delegate decision-making authority to clinicians, in spite of efforts aimed at promoting patient participation and shared decision making. If families perceive the opinions of these experts to be in conflict, their decision making may understandably become more difficult—consistent with our finding of an association between perceived ambiguity due to conflicting expert opinions and parents’ transplant decision-making difficulty. This finding is also consistent with research on “conflict aversion” [17], which demonstrates that people are particularly averse to situations where ambiguity arises due to perceived conflict or disagreement among experts. However, perceived ambiguity due to conflicting expert opinions was unrelated to parents’ actual choice of transplant. The reasons are unclear, but may reflect the real or perceived absence of other viable treatment options.
Contrary to our hypotheses, other sources of uncertainty including ambiguity due to a lack of information and ambiguity due to conflicting scientific evidence were associated with neither decision-making difficulty nor the transplant decision itself. This suggests that uncertainty regarding research evidence—as opposed to expert opinions—may be less relevant to parents’ decision making. This finding may be attributable to the limited nature of the evidence; however, it is also possible that Fanconi anemia families struggle with using existing empirical evidence to inform their transplant decision. Risk communication research confirms that interpreting such evidence, particularly evidence that is numerical in nature, is challenging for many people [45]. Additionally, parents of Fanconi anemia patients are likely to be under a great deal of stress due to the substantial cognitive, emotional, and practical demands of the disease and treatment [44]. These stressors may limit both the ability and opportunities for Fanconi anemia families to interpret research evidence, and may cause them to rely less on the evidence and to be less concerned by its associated ambiguities. Instead, they may rely on the opinions of trusted healthcare providers. These and other possibilities need to be explored.
Our exploratory mediational analyses provide insight into mechanisms that may underlie the observed associations between probability and the transplant decision, and between ambiguity due to conflicting expert opinions and transplant decision-making difficulty. Results suggested that Fanconi anemia parents’ emotional concerns about harms of transplant could significantly mediate both associations. Thus, parents’ emotional reactions to uncertainties regarding transplant, as opposed to their cognitive perceptions of risk or necessity, appear to be a critical factor in their decision-making experiences. This finding is consistent with theoretical and empirical work demonstrating that emotions have greater influence than cognitions on health-related behaviors [46, 47], and that emotions such as fear and anxiety are associated with risk-averse behavioral choices [48, 49]. Our findings suggest that emotional concerns are important in the Fanconi anemia decision-making context; however, several questions remain. It is not clear whether other emotional responses that could occur in this context, such as sadness, frustration, or anger, might also play a role in mediating effects of uncertainties on decision making. Reciprocal relationships between cognitions and emotions may also exist [46], further complicating these processes. Elucidating these relationships and the mechanisms through which various uncertainties affect decisions and behaviors will require future longitudinal investigations of the transplant decision-making process.
Limitations, Strengths, and Future Directions
Several sources of bias may have influenced these results. Participants were recruited from Fanconi anemia support organizations in the USA and Canada, and were likely highly motivated individuals who may not be representative of all Fanconi anemia families (44 % response rate, and no data on non-respondents were available). Furthermore, a minority of our sample chose not to undergo transplant (n = 22 respondents for 18 patients). The frequency with which Fanconi anemia families choose not to undergo transplant is not documented, thus it is not possible to determine to what extent the present sample is the result of selection bias, or to what extent these findings would generalize to other families with Fanconi anemia, or to families with other disorders in which transplant is a treatment option and similar sources of uncertainty exist. In addition, participants provided retrospective reports of their transplant decision-making experiences, which may have been subjected to recall bias. Although analyses were adjusted for the effects of medical and sociodemographic factors that may have influenced participants’ responses (e.g., patient vital status), these variables were limited in scope and derived from self-reported data. Another limitation is the use of single-item measures to assess sources of uncertainty. Such measures lack the statistical reliability of a well-validated scale; however, given that no such scales exist, we developed and refined items through cognitive testing in order to capture uncertainties specific to the Fanconi anemia context. Such single-item measures of psychosocial constructs (e.g., cancer risk, worry) have been shown to be strong predictors of behavioral outcomes in other contexts [47, 50, 51]. Finally, this was a cross-sectional study involving multiple comparisons with a modest sample size; therefore, it is not possible to draw firm conclusions about causal directions and mediating effects. Although our results are consistent with available theory and evidence, further longitudinal and experimental studies are needed to confirm our findings with validated measures perhaps supplemented by patient medical records in larger samples of Fanconi anemia families (to the extent possible given the rarity of this disorder). Thus, our findings are best viewed as preliminary, hypothesis-generating results that provide a valuable foundation for future investigations of Fanconi anemia parents’ treatment decision making, as well as decision-making processes in other disease contexts where treatment options are evolving and uncertainty is abundant.
In spite of these limitations, our study is the first to systematically explore associations between different sources of medical uncertainty and treatment decision making. It adds to the limited body of work on psychosocial aspects of Fanconi anemia, and furthers understanding of the many uncertainties that exist in healthcare [1]. This study is the first, to our knowledge, to use context-specific measures that captured unique sources of uncertainty, concerns about stem cell transplantation, perceptions of risks of transplantation, and perceptions of necessity of transplantation among Fanconi anemia parents in this decision-making context. Finally, these results have important implications for clinical care. Clinicians’ approaches to communicating complex and uncertain medical information can play a critical role in shaping patients’ treatment preferences [52]. These results corroborate the role of clinicians in providing Fanconi anemia families with guidance in the transplant decision, and suggest that conflict in expert recommendations can lead to distress and contribute to the difficulty of the decision. Uncertainty arising from the inability to predict probabilities of benefits and harms of transplant for individual patients compounds the challenges of this choice. These findings are perhaps not surprising; however, they represent empirical evidence that underscores the need for Fanconi anemia clinicians to make their recommendations transparent and consistent to the greatest extent possible, and to reinforce the randomness or indeterminacy of the outcomes of all treatment options—transplant as well as conservative management. These uncertainties cut both ways; from a normative standpoint they do not favor one action or another (transplant versus no transplant). Somehow making this clear to families may be the most—and the best—that clinicians can do in supporting the decisions of Fanconi anemia families. Furthermore, efforts should be taken to help Fanconi anemia families prepare over time for the communication and informational challenges they will face; doing so may allow families and clinicians to effectively work together to make treatment decisions that reflect parental and patient preferences, patient needs, and available medical knowledge [52, 53].
Our study raises intriguing questions and endorses the value of future research on uncertainty in healthcare. Future investigations would benefit from not only a longitudinal design that allows for a deeper analysis of the temporal nature of the treatment decision-making process but also from more nuanced evaluations of medical uncertainty and the various responses it could engender, including emotional responses. Such studies should examine the full spectrum of sources, issues, and loci of uncertainty that exist in healthcare [1], and which may be relevant to the transplant decision in Fanconi anemia. Future studies should also investigate how Fanconi anemia families discuss and develop a shared understanding of medical uncertainty. Past work suggests that open communication has benefits for the adjustment and well-being of families facing transplant decisions [26], yet it is unknown whether this would hold true for types of uncertainty and Fanconi anemia treatment decisions. Future studies should also examine whether the effects of different sources of medical uncertainty differ between Fanconi anemia parents and the patients undergoing treatment. This is an important area of investigation because people’s decision-making preferences and tolerance of risk can differ depending on whether they are choosing for themselves or others [54].
Conclusions
Medical uncertainty abounds in the stem cell transplant decision-making process. Findings of the current study suggest that Fanconi anemia parents’ transplant treatment decisions are differentially influenced by different uncertainties—most notably the probabilistic nature of future outcomes and ambiguity due to conflicting expert opinions. Parents’ emotional reactions to such uncertainties may mediate the effects of these uncertainties on decision-making outcomes. The nature of Fanconi anemia and current state of empirical evidence regarding stem cell transplantation in this context ensures that uncertainty will continue to be a pervasive challenge for both families and their healthcare providers. Further research is needed to better understand how to support decision making and help Fanconi anemia families cope with the many uncertainties they face in dealing with this disease.
References
Han PKJ, Klein WMP, Arora NK. Varieties of uncertainty in health care: A conceptual taxonomy. Med Decis Making. 2011;31(6):828-838.
Barry MJ, Edgman-Levitan S. Shared decision making—The pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780-781.
Woolf SH. The price of false beliefs: Unrealistic expectations as a contributor to the health care crisis. Ann Fam Med. 2012;10(6):491-494.
Nagler R. Adverse outcomes associated with media exposure to contradictory nutrition messages. J Health Commun. 2013; (in press).
Eysenbach G. The impact of the internet on cancer outcomes. CA Cancer J Clin. 2003;53(6):356-371.
Boyle P, Boffetta P, Autier P. Diet, nutrition and cancer: Public, media and scientific confusion. Ann Oncol. 2008;19(10):1665-1667.
Woloshin S, Schwartz LM. Media reporting on research presented at scientific meetings: More caution needed. Med J Aust. 2006;184(11):576-580.
Mishel MH. Uncertainty in chronic illness. Annu Rev Nurs Res. 1999; 17:269–294.
Babrow AS, Kasch CR, Ford LA. The many meanings of uncertainty in illness: Toward a systematic accounting. Heal Commun. 1998;10(1):1-23.
Politi MC, Han PKJ, Col NF. Communicating the uncertainty of harms and benefits of medical interventions. Med Decis Making. 2007;27(5):681-695.
Brashers DE. Communication and uncertainty management. J Commun. 2001;51(3):477-497.
Kahneman D, Tversky A. Prospect theory: An analysis of decision under risk. Econometrica. 1979;47(2):263-291.
Ellsberg D. Risk, ambiguity, and the Savage axioms. Q J Econ. 1961;75(4):643-669.
Han PKJ, Moser RP, Klein WMP. Perceived ambiguity about cancer prevention recommendations: Relationship to perceptions of cancer preventability, risk, and worry. J Health Commun. 2006;11(suppl 1):51-69.
Han PKJ, Kobrin SC, Klein WMP, et al. Perceived ambiguity about screening mammography recommendations: Association with future mammography uptake and perceptions. Cancer Epidemiol Biomarkers Prev. 2007;16(3):458-466.
Hutson SP, Dorgan KA, Duvall KL, Garrett LH. Human papillomavirus infection, vaccination, and cervical cancer communication: The protection dilemma faced by women in southern Appalachia. Women Health. 2011;51(8):795-810.
Smithson M. Conflict aversion: Preference for ambiguity vs conflict in sources and evidence. Organ Behav Hum Decis Process. 1999;79(3):179-198.
Kienhues D, Stadtler M, Bromme R. Dealing with conflicting or consistent medical information on the web: When expert information breeds laypersons’ doubts about experts. Learn Instr. 2011;21(2):193-204.
Carpenter DM, DeVellis RF, Fisher EB, et al. The effect of conflicting medication information and physician support on medication adherence for chronically ill patients. Patient Educ Couns. 2010;81(2):169-176.
Rosenberg PS, Greene MH, Alter BP. Cancer incidence in persons with Fanconi anemia. Blood. 2003;101(3):822-826.
Rosenberg PS, Tamary H, Alter BP. How high are carrier frequencies of rare recessive syndromes? Contemporary estimates for Fanconi anemia in the United States and Israel. Am J Med Genet A. 2011;155A(8):1877-1883.
Shimamura A, Alter BP. Pathophysiology and management of inherited bone marrow failure syndromes. Blood Rev. 2010;24(3):101-122.
Alter BP, Giri N, Savage SA, et al. Malignancies and survival patterns in the National Cancer Institute inherited bone marrow failure syndromes cohort study. Br J Haematol. 2010;150(2):179-188.
Copelan EA. Hematopoietic stem-cell transplantation. N Engl J Med. 2006;354(17):1813-1826.
MacMillan ML, Wagner JE. Haematopoeitic cell transplantation for Fanconi anaemia—When and how? Br J Haematol. 2010;149(1):14-21.
Packman W, Weber S, Wallace J, Bugescu N. Psychological effects of hematopoietic SCT on pediatric patients, siblings and parents: A review. Bone Marrow Transplant. 2010;45(7):1134-1146.
Green AM, Kupfer GM. Fanconi anemia. Hematol Oncol Clin North Am. 2009;23(2):193-214.
Guardiola P, Socie G, Li X, et al. Acute graft-versus-host disease in patients with Fanconi anemia or acquired aplastic anemia undergoing bone marrow transplantation from HLA-identical sibling donors: Risk factors and influence on outcome. Blood. 2004;103(1):73-77.
Rosenberg PS, Socie G, Alter BP, Gluckman E. Risk of head and neck squamous cell cancer and death in patients with Fanconi anemia who did and did not receive transplants. Blood. 2005;105(1):67-73.
Wagner JE, Eapen M, MacMillan ML, et al. Unrelated donor bone marrow transplantation for the treatment of Fanconi anemia. Blood. 2007;109(5):2256-2262.
Rosenberg PS, Alter BP, Socie G, Gluckman E. Secular trends in outcomes for Fanconi anemia patients who receive transplants: Implications for future studies. Biol Blood Marrow Transplant. 2005;11(9):672-679.
Fanconi Anemia Research Fund. Fanconi anemia: Guidelines for diagnosis and management (3rd). Eugene: FARF Inc.; 2008.
Tremolada M, Bonichini S, Pillon M, Messina C, Carli M. Quality of life and psychosocial sequelae in children undergoing hematopoietic stem-cell transplantation: A review. Pediatr Transplant. 2009;13(8):955-970.
Clarke SA, Eiser C, Skinner R. Health-related quality of life in survivors of BMT for paediatric malignancy: A systematic review of the literature. Bone Marrow Transplant. 2008;42(2):73-82.
Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: The development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14(1):1-24.
Klein WMP, Stefanek ME. Cancer risk elicitation and communication: Lessons from the psychology of risk perception. CA Cancer J Clin. 2007;57(3):147-167.
Moser RP, McCaul K, Peters E, Nelson W, Marcus SE. Associations of perceived risk and worry with cancer health-protective actions: Data from the Health Information National Trends Survey (HINTS). J Health Psychol. 2007;12(1):53-65.
Kraemer HC, Kiernan M, Essex M, Kupfer DJ. How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychol. 2008;27(2, Suppl):S101-S108.
MacKinnon DP, Luecken LJ. How and for whom? Mediation and moderation in health psychology. Health Psychol. 2008;27(2, Suppl):S99-S100.
Hutson SP, Han PKJ, Hamilton JG, et al. The use of hematopoietic stem cell transplantation in Fanconi anemia patients: A survey of decision-making among families in the United States and Canada. Health Expect. 2013; (in press).
Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879-891.
Preacher KJ, Selig JP. Advantages of monte carlo confidence intervals for indirect effects. Commun Methods Meas. 2012;6(2):77-98.
Selig JP, Preacher KJ. Monte Carlo method for assessing medation: An interactive tool for creating confidence intervals for indirect effects. [Computer software]. 2008. http://quantpsy.org/. Accessed 24 April 2012.
Zierhut H, Bartels D. Waiting for the next shoe to drop: The experience of parents of children with Fanconi anemia. J Genet Couns. 2012;21(1):45-58.
Reyna VF, Nelson WL, Han PK, Dieckmann NF. How numeracy influences risk comprehension and medical decision making. Psychol Bull. 2009;135(6):943-973.
Loewenstein GF, Hsee CK, Weber EU, Welch N. Risk as feelings. Psychol Bull. 2001;127(2):267-286.
Diefenbach MA, Miller SM, Daly MB. Specific worry about breast cancer predicts mammography use in women at risk for breast and ovarian cancer. Health Psychol. 1999;18(5):532-536.
Lerner JS, Keltner D. Beyond valence: Toward a model of emotion-specific influences on judgement and choice. Cogn Emot. 2000;14(4):473-493.
Lerner JS, Keltner D. Fear, anger, and risk. J Pers Soc Psychol. 2001;81(1):146-159.
Lipkus IM, Iden D, Terrenoire J, Feaganes JR. Relationships among breast cancer concern, risk perceptions, and interest in genetic testing for breast cancer susceptibility among African-American women with and without a family history of breast cancer. Cancer Epidemiol Biomarkers Prev. 1999;8(6):533-539.
Stefanek ME, Wilcox P. First degree relatives of breast cancer patients: Screening practices and provision of risk information. Cancer Detect Prev. 1991;15(5):379-384.
Epstein RM, Peters E. Beyond information: Exploring patients’ preferences. JAMA. 2009;302(2):195-197.
Mishel MH, Germino BB, Lin L, et al. Managing uncertainty about treatment decision making in early stage prostate cancer: A randomized clinical trial. Patient Educ Couns. 2009;77(3):349-359.
Zikmund-Fisher BJ, Sarr B, Fagerlin A, Ubel PA. A matter of perspective: Choosing for others differs from choosing for yourself in making treatment decisions. J Gen Intern Med. 2006;21(6):618-622.
Acknowledgments
This research was supported in part by the Intramural Research Program of the National Institutes of Health and the National Cancer Institute in Rockville, MD, USA (SPH, PKJH, BPA). We thank Drs. Andrew Hayes and Kristopher Preacher for analytic guidance. We are extremely grateful to the Fanconi Anemia Research Fund and Fanconi Canada for mailing questionnaires, and to all participating families.
Conflict of Interest
The authors have no conflicts of interests or financial interests to disclose.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Hamilton, J.G., Hutson, S.P., Moser, R.P. et al. Sources of Uncertainty and Their Association with Medical Decision Making: Exploring Mechanisms in Fanconi Anemia. ann. behav. med. 46, 204–216 (2013). https://doi.org/10.1007/s12160-013-9507-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-013-9507-5