Abstract
Objective
Data involved the association between myocardial ischaemia and the outcome for unrevascularized coronary chronic total occlusion (CTO) patients were limited. The purpose of this study was to evaluate the predictive value of ischaemia detected by single photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) for the adverse events in unrevascularized CTO patients. We further explored whether ischaemia generated from CTO vessel can independently predict the outcome.
Methods
Patients with at least one unrevascularized CTO on coronary angiography were enrolled in this study. Exercise stress/rest SPECT MPI was performed in all patients. All patients were then followed by telephone interview and reviewing of medical records.
Results
Patients with ischaemia experienced significantly higher rate of adverse events than non-ischaemia patients (40.7% vs 7.1%, P = 0.002). Ischaemia demonstrated on MPI [odds ratio (OR) = 7.656; 95% confidence interval (CI) 1.598–36.677; P = 0.011] was an independent predictor for adverse events. Moreover, CTO-ischaemia (OR = 5.466; 95% CI 1.015–29.420; P = 0.048), non-CTO ischaemia (OR = 29.174; 95% CI 3.245–262.322; P = 0.003), mixed-ischaemia (OR = 7.130, 95% CI 1.257–40.445; P = 0.027) were all independent predictors for outcome.
Conclusion
Ischaemia demonstrated on MPI, especially CTO-ischaemia were independent predictors for the adverse events. SPECT MPI can aid to identify patients at risk of adverse events, who may benefit from subsequent CTO percutaneous coronary intervention.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary chronic total occlusion (CTO) was defined as complete occlusion of coronary artery for at least 3 months with thrombolysis in myocardial infarction (TIMI) flow 0, which was observed on up to 30% of coronary angiography [1]. In traditional clinical management, CTO was tended to be treated medically or by coronary artery bypass grafting (CABG). A certain proportion of CTO patients were not revascularized due to complex CTO percutaneous coronary intervention (PCI) procedures and higher risk of periprocedural complications [2]. It was reported that only 10–22% of CTO patients received PCI treatment in a large registration study [3]. However, patients with unrevascularized CTO generally had negative prognosis. A previous research showed that the presence of a CTO in non-infarction related artery was independently associated with reduced left cardiac function as well as early and late mortality in patients after acute ST segment elevation infarction [4].
Regardless of well-formed collaterals, most CTO territories are ischaemic, which was evidenced by previous invasive coronary flow study [5]. Myocardial perfusion imaging (MPI) is a widely available non-invasive imaging technique to evaluate myocardial perfusion for detection of myocardial ischaemia [6]. A large number of high-quality research have confirmed that the great prognostic value of myocardial perfusion evaluated by MPI in suspected or known coronary artery disease (CAD) patients [7,8,9]. For example, it has well been established that extent and severity of myocardial ischaemia are important independent predictors of prognosis in patients with suspected CAD [7]. Hachamovitch’s study showed that the annual event rate of cardiac death or myocardial infarction in patients with abnormal MPI scan was much higher than patients with normal scan [8]. However, data involved the association between myocardial ischaemia and prognosis specifically in patients with unrevascularized CTO were limited. Only two studies had investigated the prognostic value of MPI in patients with unrevascularized CTO and showed that ischaemia on MPI can provide significant independent prediction of hard cardiac event, but participants included in these studies were mainly multivessel CAD with non-CTO lesion, the predictive effects of ischaemia for the adverse outcome due to whether CTO or non-CTO vessel were not discriminated [10, 11]. Therefore, purpose of our study was to identify if myocardial ischaemia shown on MPI predicts clinical outcome in patients with unrevascularized CTO, and whether ischaemia attributable to only CTO vessel independently predicts outcomes was analyzed.
Materials and methods
Study subjects
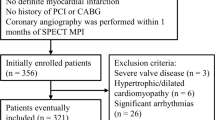
This was a retrospective cohort study. Nuclear medicine database of MPI from January 1, 2014 to December 31, 2017 at Fuwai hospital was retrospectively reviewed. Patients who were diagnosed with CTO accompanied with at least one CTO vessel that was not revascularized were included in the study. All patients underwent stress and rest 99mTc-MIBI single photon emission computer tomography (SPECT) MPI and the diagnosis of CTO was confirmed by coronary angiography. The interval between MPI and coronary angiography was within 12 months. Exclusion criteria were acute coronary syndrome within 90 days after CTO diagnosis, history of CABG, pacemaker or defibrillator implantation, or lost to follow-up. A total of 82 consecutive patients were finally included in the analysis. The study was approved by Fuwai hospital Ethical Committee.
99mTc-MIBI SPECT stress and rest perfusion imaging
A 2-day rest and exercise stress SPECT MPI protocol was applied. Exercise stress test was performed according to Bruce’s protocol on a bicycle ergometer with a 12-lead electrocardiogram. A dose of 740 MBq 99mTc-MIBI was injected intravenously at rest and peak stress, respectively. Sixty to ninety minutes after injection of 99mTc-MIBI, MPI was acquired on a Siemens double-headed SPECT system (e.cam, Siemens Medical Solution USA, Inc, Malvern, PA, USA) or Discovery NM530c SPECT system (GE Healthcare). With a low-energy high resolution parallel collimator (Siemens), projection data were acquired over a 180° anterior arc, from 45° left posterior oblique view to 45° right anterior oblique view, in 64 × 64 matrix, with 32 projections. Myocardial transverse tomograms were reconstructed with a standard filtered back projection algorithm with a three-dimensional Butterworth filter (cut-off frequency, 0.5; order, 5). Using a dedicated Cadmium Zinc Telluride camera with multiple pinhole collimator (GE), there was no detector or collimator motion during data collection. Images were reconstructed using an algorithm of three-dimensional iterative reconstruction (7 iterations and 32 subsets).
Interpretation of myocardial perfusion imaging
The standardized 17-segment model of the American Heart Association was used for left ventricular segmentation. Myocardial segments were assigned to three vascular territories, with seven segments (segment: 1, 2, 7, 8, 13, 14, 17) for the left anterior descending artery (LAD), five (segment: 5, 6, 11, 12, 16) for the left circumflex artery (LCX), and five (segment: 3, 4, 9, 10, 15) for the right coronary artery (RCA). If the LCX was dominant, two inferior segments (segment: 10, 14) were reassigned from RCA to LCX [12].
Myocardial perfusion images were evaluated visually by two experienced nuclear medicine physicians. MPI abnormality was qualitatively diagnosed by radioactivity distribution sparse or defect of at least two consecutive frames on at least two different tomographic images. SPECT-negative was defined as absolutely normal perfusion on stress and rest MPI. SPECT-positive was defined as perfusion defect on stress MPI or reversible or fixed perfusion defect on stress and rest MPI. Extension and severity of the perfusion defects were scored by consensus of two experienced observers. Segmental uptake of 99mTc-MIBI was assessed by a 5-point scoring system (0 = normal, 1 = equivocal, 2 = moderately reduced, 3 = severely decreased uptake, and 4 = absence of detectable tracer uptake). A summed stress score (SSS) was obtained by adding the scores of the 17 segments of the stress 99mTc-MIBI images.
It was further analyzed based on myocardial segments that assigned to three coronary territories, and classified into ischaemia due to CTO or non-CTO. Overall, patients were divided into SPECT-positive and SPECT-negative group based on MPI results. Four subgroups were CTO-ischaemia whose ischaemia presented only in CTO territory, non-CTO ischaemia whose ischaemia presented only in non-CTO territory, mixed-ischaemia whose ischaemia presented in both CTO and non-CTO territory, and SPECT-negative who were with normal MPI results.
Coronary angiography
Coronary angiography was performed using standard techniques as previously described. Two experienced cardiologists who were unaware of the other imaging data assessed the angiograms independently. Discrepancies were resolved by consensus. A CTO lesion was defined as a luminal complete occlusion on coronary angiography for an estimated duration of ≥ 3 months, with TIMI flow grade 0 in one major coronary artery or one of its major branch. Diseased coronary artery was defined as stenosis of an epicardial coronary artery that included 50% or more of the residual luminal or stent diameter.
Follow-up
All patients were followed by telephone interview and reviewing of medical records. The beginning of follow-up was set as date of exercise stress MPI. The endpoint was defined as composite adverse events of cardiac death, acute myocardial infarction, hospital readmission due to deterioration of cardiac function or aggravation of angina pectoris and revascularization. Deterioration of cardiac function was defined that New York Heart Association (NYHA) classification elevates at least one class. Revascularization included PCI for CTO or non-CTO lesion and CABG.
Statistical analysis
Continuous data were described as mean ± standard deviation (SD) or median (interquartile range). Categorical data were described as numbers (percentages %). Unpaired Student t test or Mann–Whitney U test was used for continuous variables. Chi-squared test or Fisher’s exact test was used for categorical variables. To test the association between baseline covariates and the adverse events, univariate logistic regression analysis was performed with results expressed as odds ratio (OR) with 95% confidence intervals (CIs). The variables with P < 0.1 on univariate analysis were allowed to entered in a multivariate logistic regression analysis model. Multivariable logistic regression was performed to determine whether SPECT-positive and CTO-ischaemia were independent predictors for outcome. Multiple categories independent variate regression analysis was applied to detect whether CTO-ischaemia, non-CTO ischaemia, mixed-ischaemia were associated with the adverse events, respectively. Cumulative event-free survival rate for composited end points were estimated by the Kaplan–Meier method and compared using log-rank tests. All statistical analyses were performed with SPSS software, Version 22.0 (IBM Corp, Armonk, NY, USA). P value < 0.05 was considered statistically significant.
Results
Baseline characteristics
Patients' baseline characteristics of 82 patients are summarized in Table 1. The mean age of population in this study was 58.7 ± 10.5 years, 73 (89.0%) patients were male. Although there were significantly statistical differences in left ventricular ejection fraction (LVEF) and left ventricular end diastolic diameter (LVEDD) between two groups, most of patients in our study were NYHA classification I–III, and the two LV functional parameters were within normal range, so the statistical differences in LVEF and LVEDD were considered as no clinical significance.
Coronary angiography
According to the definition of diseased coronary artery, stenosis of an epicardial coronary artery that included 50% or more of the residual luminal or stent diameter, among all 82 patients, 10 had three diseased coronary vessels, 40 had two diseased vessels, and 32 had single diseased vessel. A total of 92 CTO lesions were revealed by angiography among these 82 patients. Most of patients (73/82, 89.0%) had single CTO, eight patients had two CTO lesions, and one patient had three CTO lesions, respectively. A large proportion of CTO lesions (60/92, 65.2%) located in the major coronary artery (10 LAD-CTO, 32 LCX-CTO, 18 RCA-CTO). A small proportion of CTO lesions (32/92, 34.8%) located in major coronary branches (seven in diagonal artery, eight in circumflex obtuse marginal artery, seven in posterior descending artery, ten in posterior lateral artery). There were no significant differences in number of diseased vessels, number and location of CTO lesions between patients in SPECT-positive group and SPECT-negative group.
Myocardial perfusion results
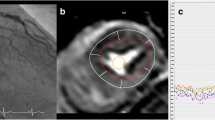
Table 2 shows the MPI results. Myocardial ischaemia detected by MPI was present in 54 patients of the CTO population in our study (54/82, 65.9%). The rest 28 patients showed negative MPI scan [28/82, 34.1%, SSS = 1 (0, 2)]. Of the 54 patients with ischaemia, 47 patients were attributable to CTO lesions [25 CTO-ischaemia, SSS = 9 (4.5, 12.5); 22 mixed-ischaemia, SSS = 15 (8, 21)]. There were 7 patients whose ischaemia were attributable to non-CTO vessels [SSS = 5 (2, 8)]. Figure 1 shows representative SPECT MPI images of patients with CTO-ischaemia, non-CTO ischaemia and mixed-ischaemia.
Representative images of myocardial perfusion imaging. A A 64-year-old man with CTO-ischaemia experienced deterioration of cardiac function after 13 months. Reversible myocardial perfusion defects (arrows) were found in inferolateral wall. Coronary angiography revealed that CTO lesion located in LCX, the middle and remote RCA was about 60% stenosis. B An 85-year-old man with non-CTO ischaemia experienced acute myocardial infarction after 16 months. Fixed myocardial perfusion defects (arrows) were found in apex, apical anterior wall, basal inferoseptal wall mid and basal inferior wall. Coronary angiography revealed that CTO lesion located in LCX, the proximal, and middle LAD was 50% stenosis, first and second diagonal branch were both 90% stenosis. C A 60-year-old man with CTO and non-CTO ischaemia experienced cardiac death after 63 months. Fixed myocardial perfusion defects (arrows) were found in inferior wall (thin arrow) and inferolateral wall. Coronary angiography revealed that CTO lesion located in LCX, the distal end of LAD stent was 50% stenosis and RCA stent was 95% stenosis
Follow-up results
Patients were followed up for a median duration of 51.8 (39.1, 66.4) months. During follow-up, 24 patients experienced the composite adverse events. Patients in SPECT-positive group experienced significantly higher rate of adverse events (22/54, 40.7%) than those in SPECT-negative group (2/28, 7.1%) (P = 0.002).
Among 22 patients in SPECT-positive group who experienced adverse events, ten patients were admitted to hospital as a result of deterioration of cardiac function and aggravation of angina pectoris, nine patients were treated with revascularization, two patients experienced acute myocardial infarction, one patient died of cardiovascular event. The adverse events of two patients in SPECT-negative group were both non-CTO revascularization.
For subgroup analysis, the adverse events rate in the group of CTO-ischaemia, non-CTO ischaemia, mixed-ischaemia were 32.0% (8/25), 71.4% (5/7), and 40.9% (9/22). Patients in these three ischaemia groups had significantly higher rate of adverse events comparing to those in the SPECT-negative group (7.1%, 2/28) (P = 0.034, P = 0.001, P = 0.006).
Univariate and multivariate logistic regression analyses
Table 3 shows the results of univariate logistic regression analysis. SPECT-positive (OR = 8.937; 95% CI 1.921–41.575; P = 0.005) was revealed as significant predictor for adverse events. Multiple categorical independent variable logistic regression analysis was constructed to detect whether CTO-ischaemia, non-CTO ischaemia, mixed-ischaemia were associated with the adverse events. The results showed that CTO-ischaemia (OR = 6.118; 95% CI 1.157–32.359; P = 0.033), non-CTO ischaemia (OR = 32.500; 95% CI 3.670–287.841; P = 0.002), mixed-ischaemia (OR = 9.000, 95% CI 1.693–47.837; P = 0.010) were all significantly associated with outcome (Table 4).
Two multivariate logistic regression models were constructed based on inclusion of either SPECT-positive or each subgroup of ischaemia to detect the independent predictive value for the adverse events (Table 5). After backward stepwise multivariate analysis, LVEF was not significantly associated with outcome (OR = 0.959; 95% CI 0.877–1.038; P = 0.301) (OR = 0.958; 95% CI 0.881–1.041; P = 0.306) in two models. In model 1, SPECT-positive remained an independent predictor for outcome (OR = 7.656; 95% CI 1.598–36.677; P = 0.011). The Kaplan–Meyer survival curves showed that the adverse event-free survival rate of SPECT-positive patients was significantly lower than SPECT-negative patients (log-rank = 7.850, P < 0.01) (Fig. 2A). In model 2, CTO-ischaemia (OR = 5.466; 95% CI 1.015–29.420; P = 0.048), non-CTO ischaemia (OR = 29.174; 95% CI 3.245–262.322; P = 0.003), mixed-ischaemia (OR = 7.130; 95% CI 1.257–40.445; P = 0.027) were all significant independent predictors for adverse events. The adverse event-free survival rate of patients with CTO-ischaemia (log-rank = 4.574, P < 0.05), non-CTO ischaemia (log-rank = 15.610, P < 0.001), and mixed-ischaemia (log-rank = 6.304, P < 0.05) was all significantly lower than non-ischaemia patients (Fig. 2B). Among three ischaemia subgroups, adverse event-free survival rate of patients with non-CTO ischaemia was significantly lower than patients with CTO-ischaemia (Log-rank = 5.265, P < 0.05), there were no significantly differences between mixed-ischaemia and CTO-ischaemia (Log-rank = 0.148, P > 0.05), non-CTO ischaemia (Log-rank = 3.614, P > 0.05).
Discussion
The main findings of this study are as follows: (1) myocardial ischaemia was present in the majority of patients with unrevascularized CTO. (2) The risk of adverse events in patients with myocardial ischaemia was significantly higher than patients with normal perfusion, and myocardial ischaemia detected by MPI was an independent predictor for adverse events. (3) Ischaemia only attributable to CTO vessel was a predictor for adverse events after adjustment.
We observed that majority of the patients (65.9%, 54/82) showed perfusion abnormalities on MPI. The proportion of ischaemia in our study was similar to that in Wright’s study (71.4%) [10], but lower than other previous studies (93.3–93.6%) [11, 13]. Possibly, this is because not only CTO lesions located in the major coronary arteries but also in major branches were included in Wright’s study and ours. Nearly one third of patients in our study showed occlusions of only major branches but not the major coronary arteries on angiography. Thus, it is reasonable that other studies studying only patients with major coronary arteries CTO had higher ischaemia rate. Although collateral circulation played a protective role for the injured myocardial subtended by CTO [14], it was not adequate to sustain stress myocardial blood flow evidenced by previous physiological examinations and clinical imaging research [5, 15, 16]. Given the large proportion of myocardial ischaemia existing in this population, it is necessary to further study the prognostic value of myocardial ischaemia.
To our best, only two studies explored the association between ischaemia evaluated by MPI and prognosis in patients with unrevascularized CTO. 40.7% (22/54) of patients experienced adverse events in our study, which was lower than that in the study by Wright’s [10] (60%, 9/15) and higher than Galassi’s [11] (26.3%, 31/118). This discrepancy can be explained by differences in follow-up duration and definition of study endpoint. In Wright’s study, relatively broader definition of study endpoint including unstable angina without Troponin I elevation was used, which resulted more adverse events recorded. In Galassi’s study, the median follow-up time was 44-month, which is relatively shorter that in our study (51.8 months). Longer follow-up may lead to more adverse events. In SPECT-negative group, two patients (2/28, 7.1%) experienced adverse events (revascularization of non-CTO vessels) during an average follow-up time of 4.27 years. It can be speculated that the annual adverse event rate of this group of patients would be less than 2%, which was close to previous reports [8, 17].
Previous studies showed that patients with CTO had significantly higher rate of death than those without CTO lesions [18]. With the progress of technique and equipment, the rate of successful CTO-PCI reached above 90% [19]. However, optimal treatment for CTO is controversial [20]. Whether revascularization of CTO is beneficial requires more evidence. Successful CTO-PCI reduced myocardial ischaemic burden [21, 22] and patients with greater decrease in ischaemic burden following CTO-PCI experienced fewer clinical events [21]. It suggested that the benefit of revascularization may depend on the degree of myocardial ischaemia. It is critical to identify patients at high risk and those who may benefit most from revascularization. In our study, a group of patients with unrevascularized CTO were studied and the results demonstrated that myocardial ischaemia detected by MPI was an independently predictor for the adverse events in CTO patients. The rate of adverse events was significantly higher in patients with ischaemia than those with normal stress perfusion. SPECT MPI, which is widely used for evaluating myocardial ischaemia to assist prognostic assessment and risk stratification of patients with CAD [6], was proven utility for patients with CTO in our study.
CTO tended to have a strong relationship with multivessel CAD [23]. In previous studies, whether ischaemia was generated from CTO or non-CTO vessels was not discriminated and the respective predictive effect proportion of CTO-ischaemia and non-CTO ischaemia was obscure. More than 60% of CTO patients in our study were multivessel CAD. Therefore, the predictive value of ischaemia attributed to CTO, non-CTO or both were separately compared. The rate of adverse events in CTO-ischaemia subgroup, non-CTO ischaemia subgroup, mixed-ischaemia subgroup was all significantly higher than normal perfusion subgroup. Ischaemia attributed to different vessels were all independent predictors for outcome. The results indicated that ischaemia in the territory of unrevascularized CTO and non-CTO were both associated with adverse events independently.
Noticeably, the odds ratio of non-CTO ischaemia was higher than CTO-ischaemia. In those who experienced events, patients with non-CTO ischaemia received more revascularization, while patients with CTO-ischaemia presented with more deterioration of cardiac function and aggravation of angina pectoris. It can be explained that patients with CTO-ischaemia may be progressed because of lower rate of attempting in CTO-PCI, while patients with non-CTO ischaemia received interventional therapy for the non-CTO lesion. It is reasonable to speculate the severity of ischaemia was associated with adverse outcome. In our study, SSS for non-CTO ischaemia group was less than that for CTO-ischaemia and mixed-ischaemia groups, indicating patients with non-CTO ischaemia did not have more severe ischaemia. Limited sample size in each group may lead to bias of the result.
Limitation
Our study has several limitations. It is a retrospective observational analysis. In addition, follow-up was performed by telephone, which may lead to recall bias. Our study merely assessed the predictive value of the presence of myocardial ischaemia. Association between the extent and severity of ischaemia evaluated by absolute myocardial blood flow using quantitative PET or SPECT imaging in CTO patients and prognosis should be investigated in future.
Conclusion
Ischaemia demonstrated on MPI, especially CTO-ischaemia were independent predictors for the adverse events. SPECT MPI was useful to identify patients at risk of adverse events, who may benefit from subsequent CTO-PCI. Moreover, patients with unrevascularized CTO who had normal stress MPI were at low risk, revascularization may not be urgent for those patients.
References
Stone GW, Kandzari DE, Mehran R, Colombo A, Schwartz RS, Bailey S, et al. Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: part I. Circulation. 2005;112(15):2364–72.
Patel VG, Brayton KM, Tamayo A, Mogabgab O, Michael TT, Lo N, et al. Angiographic success and procedural complications in patients undergoing percutaneous coronary chronic total occlusion interventions: a weighted meta-analysis of 18,061 patients from 65 studies. JACC Cardiovasc Interv. 2013;6(2):128–36.
Fefer P, Knudtson ML, Cheema AN, Galbraith PD, Osherov AB, Yalonetsky S, et al. Current perspectives on coronary chronic total occlusions: the Canadian Multicenter Chronic Total Occlusions Registry. J Am Coll Cardiol. 2012;59(11):991–7.
Claessen BE, van der Schaaf RJ, Verouden NJ, Stegenga NK, Engstrom AE, Sjauw KD, et al. Evaluation of the effect of a concurrent chronic total occlusion on long-term mortality and left ventricular function in patients after primary percutaneous coronary intervention. JACC Cardiovasc Interv. 2009;2(11):1128–34.
Werner GS, Surber R, Ferrari M, Fritzenwanger M, Figulla HR. The functional reserve of collaterals supplying long-term chronic total coronary occlusions in patients without prior myocardial infarction. Eur Heart J. 2006;27(20):2406–12.
Underwood SR, Anagnostopoulos C, Cerqueira M, Ell PJ, Flint EJ, Harbinson M, et al. Myocardial perfusion scintigraphy: the evidence. Eur J Nucl Med Mol Imaging. 2004;31(2):261–91.
Ladenheim ML, Pollock BH, Rozanski A, Berman DS, Staniloff HM, Forrester JS, et al. Extent and severity of myocardial hypoperfusion as predictors of prognosis in patients with suspected coronary artery disease. J Am Coll Cardiol. 1986;7(3):464–71.
Hachamovitch R, Berman DS, Shaw LJ, Kiat H, Cohen I, Cabico JA, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation. 1998;97(6):535–43.
Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation. 2003;107(23):2900–7.
Wright S, Lichtenstein M, Grigg L, Sivaratnam D. Myocardial perfusion imaging (MPI) is superior to the demonstration of distal collaterals in predicting cardiac events in chronic total occlusion (CTO). J Nucl Cardiol. 2013;20(4):563–8.
Galassi AR, Werner GS, Tomasello SD, Azzarelli S, Capodanno D, Barrano G, et al. Prognostic value of exercise myocardial scintigraphy in patients with coronary chronic total occlusions. J Interv Cardiol. 2010;23(2):139–48.
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. American Heart Association Writing Group on Myocardial Segmentation and Registration for Cardiac Imaging. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105(4):539–42.
Sun XX, Li S, Fang W, Tian YQ, Shen R, Wei H, et al. Preserved myocardial viability in patients with chronic total occlusion of a single coronary artery. J Nucl Cardiol. 2020. https://doi.org/10.1007/s12350-020-02134-z (Epub ahead of print).
Kocaman SA, Arslan U, Tavil Y, Okuyan H, Abaci A, Cengel A. Increased circulating monocyte count is related to good collateral development in coronary artery disease. Atherosclerosis. 2008;197(2):753–6.
Aboul-Enein F, Kar S, Hayes SW, Sciammarella M, Abidov A, Makkar R, et al. Influence of angiographic collateral circulation on myocardial perfusion in patients with chronic total occlusion of a single coronary artery and no prior myocardial infarction. J Nucl Med. 2004;45(6):950–5.
Stuijfzand WJ, Driessen RS, Raijmakers PG, Rijnierse MT, Maeremans J, Hollander MR, et al. Prevalence of ischaemia in patients with a chronic total occlusion and preserved left ventricular ejection fraction. Eur Heart J Cardiovasc Imaging. 2017;18(9):1025–33.
Galassi AR, Grasso C, Azzarelli S, Ussia G, Moshiri S, Tamburino C. Usefulness of exercise myocardial scintigraphy in multivessel coronary disease after incomplete revascularization with coronary stenting. Am J Cardiol. 2006;97(2):207–15.
Farooq V, Serruys PW, Garcia-Garcia HM, Zhang Y, Bourantas CV, Holmes DR, et al. The negative impact of incomplete angiographic revascularization on clinical outcomes and its association with total occlusions: the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial. J Am Coll Cardiol. 2013;61(3):282–94.
Wilson WM, Walsh SJ, Yan AT, Hanratty CG, Bagnall AJ, Egred M, et al. Hybrid approach improves success of chronic total occlusion angioplasty. Heart. 2016;102(18):1486–93.
Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization [published correction appears in Eur Heart J. 2019 Oct 1;40(37):3096]. Eur Heart J. 2019;40(2):87–165.
Safley DM, Koshy S, Grantham JA, Bybee KA, House JA, Kennedy KF, et al. Changes in myocardial ischaemic burden following percutaneous coronary intervention of chronic total occlusions. Catheter Cardiovasc Interv. 2011;78(3):337–43.
Schumacher SP, Kockx M, Stuijfzand WJ, Driessen RS, van Diemen PA, Bom MJ, et al. Ischaemic burden and changes in absolute myocardial perfusion after chronic total occlusion percutaneous coronary intervention. EuroIntervention. 2020;16(6):e462–71.
Hannan EL, Wu C, Walford G, Holmes DR, Jones RH, et al. Incomplete revascularization in the era of drug-eluting stents: impact on adverse outcomes. JACC Cardiovasc Interv. 2009;2(1):17–25.
Acknowledgements
No potential conflicts of interest were disclosed.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ma, X., Guo, L., Zhang, H. et al. Predictive value of SPECT myocardial perfusion imaging in patients with unrevascularized coronary chronic total occlusion. Ann Nucl Med 36, 191–199 (2022). https://doi.org/10.1007/s12149-021-01692-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-021-01692-7