Abstract
Background
In chronic total occlusion (CTO), the evidence for revascularization is less robust than for stable angina. A medical therapy strategy is common and often based on distal collateralization, regardless of the presence of ischemia.
Aim
The aim of this study was to examine the correlation between distal collateralization, myocardial perfusion imaging (MPI), and hard cardiac events (HCE) in CTO.
Method
Retrospective analysis of consecutive patients undergoing coronary angiography revealed 21 non-revascularized patients with CTO and MPI, over a 24-month period. Blinded review of patient charts, MPI, and angiography was undertaken. HCE of death, myocardial infarct, and unstable angina were assessed. Mean follow up was 23 months.
Results
Summed difference scores were calculated on a 17-segment model and collaterals graded on the Rentrop scale. 43% of patients had HCE, and 62% had collaterals. Ischemia on MPI accurately predicted HCE in CTO (60% vs 0%, P = .01). Distal collateralization failed to predict freedom from ischemia on MPI (31% vs 25%, P = .53) or HCE (31% vs 62%, P = .15).
Conclusion
MPI in patients with CTO accurately predicted HCE. This allows for accurate triage of patients by MPI for consideration of revascularization. Patients without ischemia can be safely managed with optimal medical therapy. The presence of collateralization did not predict either ischemia or HCE.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
In chronic total occlusion (CTO), the evidence for revascularization is less robust than for stable angina. Current ACC/AHA1 and ESC2 guidelines recommend ischemia-directed revascularization; however, that is largely based on non-occlusive stable coronary disease data. This treatment algorithm is also theoretically supported by previous study demonstrating hemodynamic equivalence of CTO and 90% luminal stenoses.3
Percutaneous coronary intervention (PCI) of CTO is complex with potential risks. Advancements in hardware and PCI techniques are increasing the procedural success rate;4 however, potential lethal complications still exist. Even in the hands of experienced operators, in hospital mortality rates of 0.5% and myocardial infarction (MI) rates of 3% are observed.5 Coronary computed tomography assists in predicting cases where PCI will be technically successful,6 and in others, delineate extraluminal plaque and collateral channels to assist PCI planning,7 but does not identify which patients will clinically benefit from revascularization. While single graft coronary bypass surgery is indicated in non-LAD disease not amenable to PCI in patients with refractory angina,8 it is infrequently undertaken because of the operative risks, recovery time, and lack of demonstrated prognostic benefit.
Despite these guidelines, the management of CTO remains controversial, with no head-to-head trials comparing the relative efficacy of an optimal medical therapy (OMT) strategy vs revascularization. Given the complexity and risk of CTO PCI,5 OMT is common and often based on the demonstration of distal collateralization, regardless of the presence of ischemia.
We aimed to evaluate the correlation between distal collateralization, ischemia demonstrated by myocardial perfusion imaging (MPI), and hard cardiac events (HCE). A changing landscape of pharmacotherapeutics as well as improving PCI techniques have provided the need for a contemporary management strategy, and we aimed to identify an at-risk population who stand to benefit the most from revascularization.
Methods
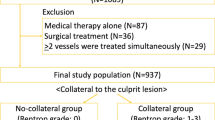
A retrospective analysis of consecutive patients undergoing diagnostic coronary angiography over a 24-month period (September 2008-September 2010) at a single tertiary center was undertaken. CTO, defined as a new estimated luminal stenosis ≥99% with no clinical or biochemical history of MI within the prior 3 months or persistent luminal stenosis ≥99% demonstrated at coronary angiography twice at least 3 months apart, was identified in 90 patients and classified by the initial planned management strategy. 39 underwent CTO PCI, 4 proceeded to single LAD bypass graft surgery, and 47 were managed medically. Of the 47 planned for medical therapy, 21 had undergone MPI as part of their assessment, and blinded chart review of these subjects was performed.
MPI studies were conducted using an exercise protocol where possible (n = 8), with 99mTc-sestamibi scintigraphy conducted at rest, then post stress. Patients unable to exercise or with left bundle branch block were stressed pharmacologically using a dipyridamole protocol (0.568 mg/kg over 4 minutes). Beta blockers and caffeine were withheld for at least 24 hours in all patients. Dipyridamole stress was contraindicated in one patient because of reactive airways disease, and a standardized dobutamine protocol was used. In two patients, the presence of large perfusion defects at rest raised clinical concern regarding the safety of stress, and rest 99mTc-sestamibi/ 24-hour 201-Thallium study was used to demonstrate significant resting ischemia, and hence increased risk of cardiac events.9 All studies were retrospectively analyzed in a blinded, semiquantitative fashion by a nuclear cardiologist. A standard 17-segment model was scored on a five-point scale.10 Summed rest scores (SRS), summed stress scores, and summed difference scores (SDS) were calculated with SDS 0-1 considered normal, SDS 2-4 representing mild ischemia, SDS 5-7 moderate ischemia, and SDS >7 severe ischemia.
Diagnostic angiography was blindly reviewed with collateralization assessed according to the validated Rentrop classification scale.11 Collaterals were graded as 0 (no visible filling of any collateral channels); 1 (filling of the distal branches, but not the epicardial portion, of the recipient artery); 2 (partial filling of the recipient epicardial artery); or 3 (complete filling of the recipient epicardial artery) depending on their angiographic appearance. Distal collateralization was then dichotomously divided as present (Rentrop Grade 1, 2, or 3) or absent (Rentrop Grade 0). It is contentious as to whether Grade 1 collaterals should be considered as absent or present collaterals; however, no patients in our study were assessed as Grade 1. The MPI study preceded angiography in 19 of 21 cases, and the findings were available to the treating clinician at the time of procedure, although the decision to medically manage was not necessarily directly related to MPI findings.
Follow up for a mean period of 23 months (13-37 months) was undertaken, assessing for HCE of death, MI, and unstable angina (UA). UA was defined as an acute coronary syndrome without Troponin I elevation, and resultant hospital admission with either revascularization of the CTO or titration of antianginal therapy. Analysis was performed on a patient experiencing HCE basis, rather than a cumulative aggregate involving multiple HCE per patient. Pearsons chi square test was used for statistical analysis, with a P value < .05 considered significant. Kruskal-Wallis testing was used for non-continuous variables. Further statistical and ROC curve analyses were performed using MedCalc for Windows, version 9.5.0.0 (MedCalc Software, Mariakerke, Belgium).
Results
For this study, 21 of 47 patients met the inclusion criteria of a medically managed CTO with a co-existent MPI study. 76% were male. The baseline characteristics of these patients were typical of an ischemic disease population (Table 1). Current guidelines of OMT in ischemic heart disease recommend aspirin, beta blockade, ace inhibition, and statin therapy.12 The medication regimes of all 21 patients were considered optimal, with doses maximized as allowed by heart rate, blood pressure, and symptoms (Table 2) in the absence of justifiable relative contraindications. Only one patient was not on aspirin, with warfarin being used for atrial fibrillation. Two patients were intolerant of statin therapy, but were on alternative anti cholesterol medications with acceptable lipid profiles. Two patients were not on ace inhibition or angiotensin receptor blockade due to renal impairment. One patient was not on beta blocker due to a resting heart rate of 48.
There was general agreement between retrospective reviews of both MPI and angiographic collateral assessment and the initial procedure reports. The median SDS was 5 (0-27), and only one study was reclassified compared with the original MPI report (mild ischemia to normal; SDS 1). As described above, in two patients with significant 99mTc-sestamibi resting perfusion defects (SRS of 21 and 22), 24-hour 201-Thallium redistribution images were performed to document resting ischemia in preference to stress. Scoring of the 201-Thallium scintigraphy using the same 17-segment model produced scores of 15 and 3, respectively. Both these patients were considered to have severe ischemia.
The Rentrop grading of collaterals demonstrated strong agreement with the initial angiographic procedure reports. All the patients retrospectively classified as Rentrop Grade 2 or 3 had collaterals reported at the time of diagnostic angiography; and no Rentrop Grade 0 patients had been reported to have distal collateralization. A total of 62% (13/21) had distal collateralization, but this failed to predict ischemia on MPI (Table 3). 86% (18 of 21) of CTO lesions in our study were in a non-LAD territory (Table 1), most likely reflecting that LAD CTO lesions were revascularized and hence not captured in our analysis. Our observed HCE event rate therefore probably underestimates the true event rate in medically managed CTO, as proximal LAD lesions are more likely to jeopardize a prognostically significant myocardial mass.
43% (9 of 21) patients experienced HCE. There were no deaths, six MI and three UA. All nine patients with HCE underwent repeat angiographic assessment with the known CTO considered the “culprit” lesion in all cases. There was a strong correlation between ischemia on MPI and HCE (Table 4), with an area under the ROC curve of 0.750 (Figure 1; 95% confidence interval 0.516-0.910, P < .01). Distal collateralization failed to significantly predict HCE (31% vs 62%, P = .15).
A common diagnostic pathway is for patients with positive MPI to proceed to coronary angiography. Within our cohort of positive MPI patients (n = 15), the absence of collaterals correlated with a high HCE event rate of 83% (5 of 6), and was a predictor of poor outcome. The presence of collaterals (with positive MPI) failed to discriminate between patients that suffered HCE and those that did not, with almost half of the patients with collaterals experiencing events (four of nine). In these patients with positive MPI, the presence of collaterals does not assist in predicting HCE.
Discussion
Distal coronary collaterals are frequently present in CTO and are often used to justify OMT, rather than revascularization, driven largely by improved survival and freedom from MI demonstrated in the 1980s,13 as well as low technical success rates of CTO PCI in that period. However, these benefits have not been reproduced in the current era of improved stents, antiplatelet agents and anti-ischemic medications. We observed no significant relationship between visualization of collaterals and HCE suggesting a restricted utility in currently used management algorithms. Angiographic assessment of collaterals’ functional capabilities and ability to predict against cardiac events is limited, with the Rentrop grading system only demonstrating a weak correlation to invasive parameters of function.14 It fails to discriminate the vast majority of patients, who have Grade 3 collaterals. More accurate assessment requires quantitative angiography with multiple invasive pressure measurements, including a pressure distal to the occlusion (which requires crossing the CTO with a pressure wire and increased radiation exposure). This is not practicable in every-day practice, and is only undertaken at the time of revascularization.14 Recent evidence does suggest long-term survival with a well-developed, functional collateral circulation; however, visualization of collaterals at angiography alone cannot predict these patients, or their functional capabilities.15 Our results support this failure to predict functional reserve.
In CTO, ischemia may be caused by inadequate collateral arteries or by coronary steal during exercise or pharmacological stress. Coronary steal is the phenomenon of decreased collateral flow due to microvascular dilatation and has three primary determinants: increased donor artery resistance (with or without a discrete stenosis), non-negligible collateral resistance, and the microvasculature distal to the occlusion lacking vasodilatory reserve as a result of already being maximally dilated.16 The visual appearance of collaterals at angiography under basal resting conditions is not directly influenced by these factors, and therefore struggles to predict coronary steal, particularly in cases without a discrete epicardial donor stenosis. Steal occurs in up to a third of CTO patients. While protecting against resting ischemia, collaterals do not protect against stress-induced perfusion defects, and only 10% of collateral circulations provide an adequate functional response to pharmacological stress.17 Although we observed a slightly higher rate of ischemic protection (31%), the majority of patients with collaterals still had significant perfusion abnormalities.
MPI is backed by robust data to predict ischemia and risk of cardiac events across a broad spectrum of coronary artery disease presentations.18 Our findings support its applicability to the CTO cohort. The demonstration of regional perfusion reduction at the myocyte level allows it to accurately predict ischemia regardless of the anatomy. It provides summative evaluation of the ischemic burden and indirectly assesses the functional capabilities of collateral arteries. This is in contrast to invasive physiological assessment of collaterals, which is limited by anatomy and relies on distal pressure wire placement necessitating crossing of the occlusive disease or traversing the collateral supply. Our demonstration of increased HCE in patients with ischemia on MPI adds to the accumulating knowledge base of CTO, and in particular the importance of recognizing physiological compromise.
There are a number of potential benefits of revascularization in CTO, and intervention should be considered in patients at increased risk of HCE. Patients with CTO and high ischemic burden (>12.5%) have significant reduction in ischemia (>5% reduction) following successful PCI, with demonstrated survival benefit at 12 months.19 These results are in keeping with prior observational findings of mortality benefit with revascularization in stable coronary artery disease and significant ischemia.20 Recanalization of CTO can also reduce ischemia in other vascular territories. A significant fractional flow reserve (FFR < 0.75) within an epicardial donor artery can be rendered nonsignificant by PCI of the CTO which reduces the strain of a collateral circulation.21 Another important consideration is patients presenting with ST elevation MI (STEMI) in a different coronary artery. In STEMI, patients with coexistent CTO in a non-infarct artery experience increased cardiac mortality at 2 years, as well as increased infarct size and impairment of reperfusion markers.22 PCI of CTO (prior to STEMI) can therefore potentially reduce risk in this population at high risk for multi-vessel disease. Improvement in left ventricular function is also observed following PCI of CTO.23
Guideline recommendations for PCI in CTO follow those for non-occlusive obstructive coronary disease.2 Although the COURAGE24 and BARI-2D25 trials recently demonstrated no benefit of revascularization over OMT in stable coronary artery disease, they are not directly applicable to the CTO population. There are two important observations of these trials. First, the COURAGE nuclear substudy showed a significant reduction in ischemic burden with revascularization compared with OMT and that residual ischemic burden was related to survival.26 CTO patients inherently have a high ischemic burden, and survival benefit for those with >5% ischemic burden reduction with revascularization has already been demonstrated.19 Second, in the BARI-2D trial, a statistically significant majority (358 of 577) of patients with CTO were selected for CABG rather than PCI as the revascularization strategy. Although the individual outcomes of these patients are not known, this CABG arm of the trial demonstrated survival benefit with revascularization over OMT.25,27 Also, the patients selected for the CABG arm had a significantly higher myocardial jeopardy index than those recruited for PCI, which is proportional to ischemic burden25 and likely applicable to CTO patients. The significant increase in HCE in patients with CTO and ischemia observed in our study make these patients as ideal targets for revascularization and further randomized evaluation.
The DECISION CTO (Clinical Trials.gov NCT01078051) trial aims to address the paucity of randomized controlled data comparing revascularization with OMT in CTO. Robust evidence delineates improved long-term cardiac survival of successful vs unsuccessful CTO PCI;28 however, it is possible that unsuccessful PCI may have a higher event rate than OMT alone because of procedure complication and emboli to the microvascular circulation. Regardless of the final outcome of DECISION CTO, our findings suggest that the presence of ischemia is an accurate discriminator of patient’s at high risk of cardiac events. Intuitively, revascularization to reduce the ischemic burden should limit these events, and until these randomized data become available, our results support ischemia-directed revascularization, without consideration of collateralization.
Conclusion
Despite inherent limitations of a small sample size and retrospective, non-randomized review, MPI in patients with CTO accurately predicted HCE, with extremely high sensitivity and negative predictive value. Patients without ischemia can be safely managed with OMT given their exceptionally low rate of HCE. The presence of collateralization did not predict either ischemia or HCE, and even in the positive MPI subgroup, it failed to further risk stratify patients. In the absence of definitive outcome data directly addressing medical therapy and CTO PCI, it is the subgroup of patients at risk of HCE, who may potentially benefit from attempted revascularization. We hypothesize that the accurate prediction of HCE by MPI can identify these patients; and that this cohort deserves further randomized evaluation of outcomes with PCI.
References
Levine G, Bates E, Blankenship J, Bailey S, Bitti J, Cercek B, et al 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: Executive summary: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol 2011;58:e44-122.
Wijns W, Kolh P, Danchin N, Di Mario C, Falk V, Folliquet T, et al. Guidelines on myocardial revascularization. Eur Heart J 2010;31:2501-55.
Flameng W, Schwarz F, Hehrlein F. Intra-operative evaluation of the functional significance of coronary collateral vessels in patients with coronary artery disease. Am J Cardiol 1978;42:187-92.
Jones D, Weerackody R, Rathod K, Behar J, Gallagher S, Knight C, et al. Successful recanalisation of chronic total occlusions is associated with improved long-term survival. JACC Cardiovasc Interv 2012;5:380-8.
Rathore S, Matsuo H, Terashima M, Kinoshita Y, Kimura M, Tsuchikane E, et al. Procedural and in-hospital outcomes after percutaneous coronary intervention for chronic total occlusions of coronary arteries 2002 to 2008: Impact of novel guidewire techniques. JACC Cardiovasc Interv 2009;2:834-42.
Soon K, Cox N, Wong A, Chiatowitz A, Macgregor L, Santos P, et al. CT coronary angiography predicts the outcome of percutaneous coronary intervention of chronic total occlusion. J Interv Cardiol 2007;20:359-66.
Surmely J, Katoh O, Tsuchikane E, Nasu K, Suzuki T. Coronary septal collaterals as an access for the retrograde approach in the percutaneous treatment of coronary chronic total occlusions. Catheter Cardiovasc Interv 2007;69:826-32.
Hillis L, Smith P, Anderson J, Bittl J, Bridges C, Byrne J, et al. ACCF/AHA Guidelines for Coronary Artery Bypass Graft Surgery: A report of the American College of Cardiology Foundation. American Heart Association Task Force of Practice Guidelines. Circulation 2011;124:e652-735.
Kong G, Lichtenstein M, Gunawardana D, Better N, Roysri K, Sivaratnam D. Fixed defects on rest/stress Tc-99m sestamibi study underestimates myocardial ischaemia: Comparison with 24-hour thallium-201 study for short term and intermediate term follow up. Clin Nucl Med 2008;33:168-71.
Hansen C, Goldstein R, Akinboboye O, Berman D, Botvinick E, Churchwell K, et al. ASNC Imaging Guidelines for Nuclear Cardiology Procedures: Myocardial perfusion and function: Single photon emission computed tomography. J Nucl Cardiol 2007;14:e39-60.
Rentrop K, Cohen M, Blanke H, Phillips R. Changes in collateral filling after controlled coronary artery occlusion by an angioplasty balloon in human subjects. J Am Coll Cardiol 1985;5:587-92.
Smith S, Blair S, Bonow R, Brass L, Cergueira M, Dracup K, et al. AHA/ACC Guidelines for Preventing Heart Attack and Death in Patients with Atherosclerotic Cardiovascular Disease: 2001 Update. J Am Coll Cardiol 2001;38:1581-3.
Hansen J. Coronary collateral circulation: Clinical significance and influence on survival in patients with coronary artery occlusion. Am Heart J 1989;117:290-5.
Werner G, Ferrari M, Heinke S, Kuethe F, Surber R, Richartz B, et al. Angiographic assessment of collateral connections in comparison with invasively determined collateral function in chronic coronary occlusions. Circulation 2003;107:1972-7.
Seiler C. The human collateral coronary circulation. Eur J Clin Invest 2010;40:465-76.
Werner G, Fritzenwanger M, Prochnau D, Schwarz D, Ferrari M, Aarnoudse W, et al. Determinants of coronary steal in chronic total coronary occlusions. J Am Coll Cardiol 2006;48:51-8.
Aboul-Enein F, Kar S, Hayes S, Sciammarella M, Abidov A, Makkar R, et al. Influence of angiographic collateral circulation on myocardial perfusion in patients with chronic total occlusion of a single coronary artery and no prior myocardial infarction. J Nucl Med 2004;45:950-5.
Klocke F, Baird M, Lorell B, Bateman T, Messer J, Berman D, et al. ACC/AHA/ANSC Guidelines for the use of cardiac radionuclide imaging—Executive summary. Circulation 2003;108:1404-18.
Dafley D, Koshy S, Grantham J, Bybee K, House J, Kennedy K, et al. Changes in myocardial ischaemic burden following percutaneous coronary intervention of chronic total occlusions. Catheter Cardiovasc Interv 2011;78:337-43.
Hachamovitch R, Hayes S, Friedman J, Cohen I, Berman S. Comparison of the short-term survival benefit associated with revascularisation compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 2003;107:2900-7.
Sachdeva R, Uretsky B. The effect of CTO recanalization on FFR of the donor artery. Catheter Cardiovasc Interv 2011;77:367-9.
Lexis C, van der Horst I, Rahel B, Lexis M, Kampinga M, Gu Y, et al. Impact of chronic total occlusions on markers of reperfusion, infarct size and long-term mortality: A substudy from the TAPAS-trial. Catheter Cardiovasc Interv 2011;77:484-91.
Kirschbaum S, Baks T, van der Ent M, Sianos G, Krestin G, Serruys P, et al. Evaluation of left ventricular function three years after percutaneous revascularization of chronic total coronary occlusion. Am J Cardiol 2008;101:179-85.
Boden W, O’Rourke R, Teo K, Hartigan P, Maron D, Kostuk W, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007;356:1503-16.
Frye R, August P, Brooks M, Hardison R, Kelsey S, Macgregor J, et al. A randomized trial of therapies for Type 2 diabetes and coronary artery disease. N Engl J Med 2009;360:2503-15.
Shaw L, Berman D, Maron D, Mancini G, Hayes S, Hartigan P, et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: Results from the clinical outcomes utilizing revascularization and aggressive drug evaluation (COURAGE) trial nuclear substudy. Circulation 2008;117:1283-91.
Kim L, King S, Kent K, Brooks M, Kip K, Abbott J, et al. Factors related to the Selection of surgical versus percutaneous revascularisation in diabetic patients with multi-vessel coronary artery disease in the BARI 2D (Bypass Angioplasty Revascularization Investigation in Type 2 Diabetes) trial. JACC Cardiovasc Interv 2009;2:384-92.
Joyal D, Afilalo J, Rinfret S. Effectiveness of recanalisation of chronic total occlusions: A systematic review and meta-analysis. Am Heart J 2010;160:179-87.
Author information
Authors and Affiliations
Corresponding author
Additional information
See related editorial, doi:10.1007/s12350-013-9704-4
Rights and permissions
About this article
Cite this article
Wright, S., Lichtenstein, M., Grigg, L. et al. Myocardial perfusion imaging (MPI) is superior to the demonstration of distal collaterals in predicting cardiac events in chronic total occlusion (CTO). J. Nucl. Cardiol. 20, 563–568 (2013). https://doi.org/10.1007/s12350-013-9678-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-013-9678-2