Abstract
Objective
18F is the most extensively used radioisotope in current clinical practices of PET imaging. This selection is based on the several criteria of pure PET radioisotopes with an optimum half-life, and low positron energy that contributes to a smaller positron range. In addition to 18F, other radioisotopes such as 68Ga and 124I are currently gained much attention with the increase in interest in new PET tracers entering the clinical trials. This study aims to determine the minimal scan time per bed position (Tmin) for the 124I and 68Ga based on the quantitative differences in PET imaging of 68Ga and 124I relative to 18F.
Methods
The European Association of Nuclear Medicine (EANM) procedure guidelines version 2.0 for FDG-PET tumor imaging has adhered for this purpose. A NEMA2012/IEC2008 phantom was filled with tumor to background ratio of 10:1 with the activity concentration of 30 kBq/ml ± 10 and 3 kBq/ml ± 10% for each radioisotope. The phantom was scanned using different acquisition times per bed position (1, 5, 7, 10 and 15 min) to determine the Tmin. The definition of Tmin was performed using an image coefficient of variations (COV) of 15%.
Results
Tmin obtained for 18F, 68Ga and 124I were 3.08, 3.24 and 32.93 min, respectively. Quantitative analyses among 18F, 68Ga and 124I images were performed. Signal-to-noise ratio (SNR), contrast recovery coefficients (CRC), and visibility (VH) are the image quality parameters analysed in this study. Generally, 68Ga and 18F gave better image quality as compared to 124I for all the parameters studied.
Conclusion
We have defined Tmin for 18F, 68Ga and 124I SPECT CT imaging based on NEMA2012/IEC2008 phantom imaging. Despite the long scanning time suggested by Tmin, improvement in the image quality is acquired especially for 124I. In clinical practice, the long acquisition time, nevertheless, may cause patient discomfort and motion artifact.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent years, the use of 18F-FDG has become a huge success in molecular imaging due to the targeting characteristic of this compound as a marker of glucose metabolism. However, this advantage is not optimal in all types of cancer. 18F-FDG is shown to give low specificity and sensitivity for non-glucose uptake cases. The previously published manuscript stated that 18F-FDG gives a limited role in neuroendocrine tumors (NETs) as the well-differentiated NETs are slow growing and do not avid the 18F [1]. Despite that, the American Thyroid Association (ATA) management guidelines do not recommend the use of 18F-FDG in the evaluation of differentiated thyroid cancer (DTC). This is because the primary lesion of the thyroid cancer might be overlooked [2]. Currently, the limitations of positron emission tomography (PET) imaging with 18F especially in staging and diagnosis of NETs and DTC have been shown to improve with other PET tracers such as 68Ga and 124I.
However, each PET radioisotope consists of different physical properties that give rise to different impacts on PET quantitative imaging as shown in Table 1. For instance, the use of 68Ga might contribute to low spatial resolution and increase of image blurring which is caused by partial volume effect (PVE). Other than that, 68Ga also consists of low positron yield and large positron range in tissue due to its higher positron energy emission. Overall, the PET imaging quantitative and image quality may be disturbed in such ways.
In addition to 68Ga, 124I with a long half-life yet non-pure positron emitters is another isotope becoming relevant for PET imaging. Regardless of its advantage, the presence of prompt gamma emission that falls within the energy window of the scanner (61% of 605 keV single photon emission of 124I) may contribute to the significance effects like inaccurate measurable of photon detection which eventually caused the rate of true coincidence events detection to decrease [3,4,5]. Detections of these prompt gamma emissions could either increase or lower the background uniformity, and thus the noise level. Indirectly, these prompt gamma events also affected the dead time of the detector as well as scanner correction. Previously, a higher noise level is reported in a higher background counts and thus leads to the inconsistent radioactivity distribution in lower activity lesions [4].
Hence, these considerations led to the onset idea of this study. In this work, the quantitative differences in PET imaging of 68Ga and 124I relative to 18F were assessed. The quantitative differences among the three radionuclides were used as a benchmarking in the derivation of the minimal scan time, Tmin for the 124I and 68Ga. The Tmin for the 124I and 68Ga was determined based on the 15% COV recommended for 18F. 18F is considered as the reference for the comparison as it is required for most of the measurements by the National Electrical Manufacturers Associations (NEMA) standards and the most widely used in PET routine quality control. At the end of the study, quantitative analyses of the image were performed to identify the effectiveness of the Tmin.
Materials and methods
All data acquisition and analysis were performed using an integrated PET–CT system with bismuth germanium oxide (BGO) crystal (Discovery ST, GE Medical System, Milwaukee, USA) and PMOD 3.7 medical imaging analysis software.
PET–CT imaging using NEMA phantom
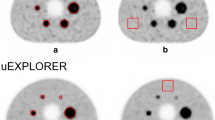
A NEMA2012/IEC2008 phantom containing six fillable spheres and background compartment was used. The large background compartment was filled with an 18F-FDG solution of 3 kBq/mL. Spheres, representing tumors of 0.50, 1.14, 2.75, 5.65, 11.65, and 27.00 ml, were filled with an 18F-FDG solution of 30 kBq/mL giving tumor background ratio (TBR) of 10:1. A similar amount of 68Ga and 124I activity concentration was filled into the phantom’s sphere and background volume. Routine list-mode PET scan time at the one-bed position was implemented in this study. The phantom was placed on the scanner bed with the center of each sphere aligned on the transverse plane and center of the field of view as shown in Fig. 1. Data were acquired for 1, 5, 7, 10 and 15 min acquisition time to determine the Tmin for each radioisotope. Five PET–CT acquisitions are done for each radionuclide and hence a total of 15 acquisitions performed in this study.
The images were reconstructed using a fully 3D ordered subset expectation maximization (OSEM) algorithm. Two iterations and 21 subsets, with the standard Gaussian post-filters with 6.0 mm full width half maximum (FWHM) were used. OSEM is currently the most widely used iterative reconstruction method [6, 7]. This reconstruction scheme provides better image quality due to the incorporation of correction for geometrical response and detector system efficiency, system dead time, random coincidence, scatter and attenuation [8].
Derivation of Tmin
Tmin is used to determine the optimum radioactivity given to the patients using quadratic formulation. Analysis of the coefficient of variations (COV) was used as a platform in the derivation of Tmin. COV is presenting the variability of the data, i.e. the amount of noise present in an image. The most uniform region in the image, specifically the phantom background usually considered for the COV calculation. COV was determined by the ratio between the standard deviation of the counts in the volume of interest (VOIs) of the background (SDB) to the mean counts of backgrounds VOIs (MB) as described in by [9]
In this study, the derivation of Tmin was performed by fitting the measured COV data using the power-law function. COV data as a function of scan time per bed position was plotted and fitted using the concerning function which is presented by COV = aT−b, where T is the scan time per bed position, a and b are the fitting coefficients. As recommended, COV = 15% is considered acceptable to ensure the image quality and quantification accuracy are within tolerance [8]. Therefore, COVmax = 15% was also used as the reference guidelines for 68Ga and 124I in this study. The coefficient determination R2 > 0.9, for all radioisotopes, indicates that the power-law fits the data well. R2 is commonly presented by values ranging from 0 to 1. It shows how well the fitted data presented the actual data set. R2 of 1 means that the actual data set is completely explained by the fitted equation. Based on the fitted function, Tmin can be derived using the following equation:
The AB described in Eq. 2 is the true activity concentration of the radioisotopes in the background compartment of the phantom during the starting time of the phantom scan Ta. Theoretically, the calculated activity concentration should equal to 3 kBq/ml. COVmax of 15% to be used for Tmin calculation has been previously recommended [8].
Image analysis
To quantify the PET image quality, six spheres inside the phantom image were contoured to define the VOIs. The VOI was defined to include the actual size of the sphere and also corrected for the background uptake. The sphere outlining was done manually with the guidance of CT information (Fig. 2). The previous study did suggest 50, 70% or halfway between background and maximum pixel value for the automatic region of interest (ROI) definition [10]. In this study, the manual definition of VOIs is possible due to the small number of images. The definition of the volume allows the whole volume of the sphere to be analysed in a single analysis. The background was defined by five rectangular VOIs of 30.0 ml within the background volume.
The image was analysed based on the following parametric:
Contrast recovery coefficient (CRC)
Mathematically, percentage contrast is presented by Eq. 3 [11]. MS and MB are the mean concentration (kBq/ml) in the sphere and background each, and R is the true sphere to background activity:concentration ratio (10:1). In an ideal case, the CRC must be equal to 100%.
Signal-to-noise ratio (SNR)
SNR is a term used to represent the ratio between signals (meaningful information) to the noise, shown by
Here TS and TB are the total number of counts in sphere VOIs and background VOIs, while SDB is the standard deviation of background [11].
Visibility (VH)
Visibility could be defined as the ability to distinguish a hot spot sphere with respect to the background activity concentration, regardless of the sizes of the sphere. Quantitative evaluation of the sphere’s visibility is represented by
Nvoxels is the number of voxels in the spheres [12].
Results
Table 2 shows the COV calculated for 18F, 124I and 68Ga, acquired at 1, 5, 7, 10 and 15 min. The COV decreases with the increment of acquisition time for all radioisotopes. The lower value of COV indicates that longer acquisition time leads to a lower degree of variation among the data series. In clinical practice, longer acquisition time nevertheless increases the risk for patient movement, especially for pediatric patients. A comparison of the three radioisotopes reveals that the 124I yielded higher COV as compared to the 18F and 68Ga.
In Fig. 3, the COV against the scan times is presented (the experimental data are shown by the solid lines). The data for 18F, 68Ga, and 124I were fitted using the power-law function with two coefficient variables (the fitted data are shown by the dashed lines). In this study, the power-law resulted in COV equal to 24.757 T−0.471, 22.922 T−0.385 and 78.108 T−0.478 for 18F, 68Ga and 124I, respectively. T in these expressions refers to the scanning time. Noted that, the Tmin is derived at COVmax = 15% using the derived power-law functions. Alternatively, the derivation of the Tmin could be performed by interpolation of the fitted COV data [8]. The Tmin obtained by 18F and 68Ga were 3.08 and 3.24 min, respectively. Meanwhile, the Tmin for 124I radioisotope was longer than the 18F and 68Ga radioisotopes. At 15 min of acquisition time, the COVI-124 = 21.2%, which is still greater than the COVmax = 15% as recommended by the previous study [8]. Hence, extrapolation of the data was performed until it reached the COVmax = 15%. Based on the extrapolated data, the Tmin for 124I is 32.93 min.
Image analyses
Contrast recovery coefficient (CRC)
In Fig. 4, the calculated CRC is plotted against the sphere volume. Noted that, the symbols used to represent 18F, 68Ga, and 124I in Figs. 4, 5, and 6 are consistent throughout this article. Hence, for the simplicity of the figures, we thus added the figure legend in sub-figure (a) only. Comparison agrees that the increment of the acquisition time does not improve the image quality for all radioisotopes assessed (maximum standard deviation of 0.07 was calculated). Therefore, the results presented here are limited to 1 and 5 min of acquisition time. The other data are purposely not presented here due to the insignificant difference. While a small relative difference was calculated between 18F and 68Ga, 124I consistently yields lower CRC as compared to 18F and 68Ga. Overall, the analyses of the small sphere gave lower CRC compares to the larger sphere. Imaging of 18F and 68Ga using the suggested Tmin do not significantly affect the CRC of these two radioisotopes, with relative differences of 0.19–0.68 and 0.39–1.76%, respectively. Nevertheless, the implementation of Tmin for 124I leads to significant changes. The CRC obtained from 124I imaging using Tmin acquisition time is approaching CRC obtained by 18F and 68Ga (Fig. 4c, d).
Signal-to-noise ratio (SNR)
In contrast to CRC, an increment of acquisition time leads to a greater increment of the SNR (highest standard deviation of 13.2, 6.8 and 5.0 for the largest sphere of 18F, 68Ga and 124I each). As expected, image noise for 68Ga is higher and 124I consistently resulted in the lowest SNR value. A comparison shows that the SNR obtained for 124I at 15 min acquisition time equivalent to 18F and 68Ga SNR value acquired at 1 min acquisition time (shown by a thick arrow in Fig. 5c, d). Extrapolation of the data suggested that the acquisition of 124I using calculated Tmin able to improve the SNR up to 31.6 for the largest sphere and 9.2 for the smallest sphere.
Visibility (VH)
The ability of PET–CT in visualizing small tumors is undeniable. In this study, all radioisotopes show good visibility even for the smallest sphere and shortest acquisition time. These findings nevertheless are limited to the high TBR (TBR = 10:1) tested in this study. Low accumulation of activity (lower TBR) is most likely to show a lower VH and hence worth being assessed in a future study. According to the Rose criterion, the hot spheres were visible when the VH value is larger than four [12]. The visibility of the sphere was even better with the usage of 18F, whereby VH = 45 was measured at 1 min acquisition time. In general, 68Ga shows higher VH compared to 18F at shorter acquisition time, while contrast findings were observed for acquisition time greater than 7 min (Fig. 6). Again, implementation of the Tmin able to reduce the quantitative difference in the visibility of the sphere especially for the 124I.
Discussion
Limited role of 18F-FDG in NETs due to slow growth of well-differentiated NETs, as well as DTC, has been improved with other PET tracers such as 68Ga and 124I. The different physical properties of the radioisotopes may signify the need for explicit imaging protocol for each radioisotope. In our center, 2-min scanning time per bed position is currently implemented and considered satisfactory for 18F and 68Ga PET–CT imaging. Meanwhile, 20 min is implemented for 124I PET–CT imaging to obtain a satisfactory result. Accordingly, in this study, we attempt to define a Tmin for each radioisotope commonly used in imaging at our institution. This definition was made based on the quadratic dose formulation previously proposed by another researcher [8]. It should be noted that all images used for the quantification were reconstructed using a Gaussian filter of the same strength. An optimal smoothing filter based on the noise level for each image was not performed and thus should be regarded as the limitation of this study.
Using the quadratic dose formulation described by Koopman et al. [8], the suggested Tmin for 18F and 68Ga is 3.08 and 3.24 min, respectively. These data show that, instead of administered a higher radioactive dose to the patient (as implemented in linear dose protocol), we can improve the PET–CT image quality by lengthening the scanning time up to the Tmin. For instance, in a linear dose protocol, a 50 kg patient will be administered with 250 MBq of 18F-FDG activity. Rather, an activity as low as 205.2 MBq is appropriate for the same weight of patients when the quadratic dose protocol is implemented [13]. This lower activity will be compensated by longer scanning time as suggested by the Tmin.
Studies have shown that the 124I (T1/2 = 4.18 days) led to longer Tmin as compared to the current practice in our institution. Extrapolation of the data suggested that 32.93 min scanning time is appropriate for optimal 124I imaging. This scanning time is approximately 65% longer than the current protocol. This is apparently due to the lower positron percentage that caused a longer time needed for 124I scanning acquisition. Though the number of photons per unit time of 124I (23%) and 18F (96.7%) is about four times, the Tmin for 124I is almost ten times longer compares to the 18F. For 124I, noted that only 23% positron yields possibly used for imaging. Therefore, the low number of annihilation could be compensated by increasing the scanning time up to Tmin. The possible reason for a longer Tmin of 124I could be due to the less statistical counts and the positron physical property whereby the energy from the 124I is higher than the energy of 18F. The higher energy of 124I leads to a larger positron range of the isotope. Unfortunately, in clinical practice, the long acquisition time may increase the risk for patient discomfort and consequently motion artifact. Nevertheless, the data proved that the longer image acquisition of the 124I using 15% COV would produce an image contrast (CRC) that is comparable to the 18F and 68Ga images (shown in Table 3; Fig. 4c), as measured on 27.00-ml sphere. For the 0.5-ml sphere, the implementation of Tmin able to result in better CRC for 124I compares to 18F and 68Ga imaging. Extrapolation of the 124I data at Tmin gave CRC of 23.0, as tabulated in Table 3. It is worth noted that analyses of the small sphere could be affected by the PVE, whereby underestimation of the uptake value may occur [14]. Meanwhile, appropriate improvement of the SNR (13.8 and 15.9% for 27.00- and 0.5-ml sphere each, as shown in Fig. 5c, d) and visibility (13.8 and 15.8% for 27.00- and 0.5-ml sphere each, Fig. 6c, d) compares to the current image acquisition protocol practices in our institution are noted. Nevertheless, this increase is not as good as 18F as it is limited by the standard deviation of the background. For both SNR and visibility of 18F, improvement of 23.4 and 26.3% was noted for the 27.00- and 0.5-ml sphere, respectively. At early scanning time, the higher standard deviation of the background of 124I due to the less counting is a factor affected the SNR and visibility. SNR, which measures the useful signal with respect to the noise is affected by the uncertainty of the counts. Longer acquisition time leads to more data counted, which eventually reduces the background noise. Higher image noise for 68Ga is apparently due to 0.034% of single photon emission in the range of 350–650 keV and 3% of high-energy photon emission (1077 keV). It should be noted that the data presented here are limited to phantom-based imaging using the BGO-based PET–CT system, whereby the other factors like the patient’s movement are not taken into consideration.
Conclusion
NEMA2012/IEC2008 body phantom imaging was performed to determine the Tmin for the 124I and 68Ga based on the quantitative differences in PET imaging of 68Ga and 124I relative to 18F. It was derived based on the recommendation by Boellard et al. for 18F Tmin calculation, whereby COVmax of 15% was used for the calculation [8]. In this study, the Tmin obtained for 18F, 68Ga and 124I were 3.08, 3.24 and 32.93 min, respectively. Analyses of the images show that imaging of 18F and 68Ga using the suggested Tmin able to yield CRC that is comparable to the CRC yielded by longer acquisition time. In addition to that, the quantitative difference in the visibility of the sphere was reduced, especially for the 124I. Even though a longer acquisition time has been shown able to improve the SNR, the SNR measured on the image acquired using Tmin meets the criteria of good image quality according to recommendations of Fukukita et al. [15]. Despite the long Tmin defined for 124I, extrapolation of the data showed promising improvement in the 124I image quality acquired using the Tmin. The CRC for the 124I was even approaching the CRC calculated for 18F and 68Ga if the imaging is performing using the Tmin. In clinical practice, the long acquisition time, nevertheless, may cause patient discomfort and eventually susceptibility to the motion artifact.
References
Jessica EM, James RH. Imaging in neuroendocrine tumors: an update for the clinician. Int J Endocr Oncol. 2015;2(2):159–68.
Wimmer I, Pichler R. Thyroid cancer: advances in diagnosis and therapy FDG PET in thyroid cancer. London: IntechOpen; 2016.
Conti M, Eriksson L. Physics of pure and non-pure positron emitters for PET: a review and a discussion. EJNMMI Phys. 2016;3(1):8.
Lubberink M, Herzog H. Quantitative imaging of 124I and 86Y with PET. Eur J Nucl Med Mol Imaging. 2011;38(Suppl 1):S10–8.
Disselhorst JA, Brom M, Laverman P, Slump CH, Boerman OC, Oyen WJ, et al. Image-quality assessment for several positron emitters using the NEMA NU 4–2008 standards in the Siemens Inveon small-animal PET scanner. J Nucl Med. 2010;51(4):610–7.
Boellaard R. PET imaging instrumentation and principles of PET protocol optimisation. In: Principles and practice of PET/CT: Part 1. A technologist's guide. European Association of Nuclear Medicine 2010. https://www.eanm.org/publications/technologists-guide/principles-practice-petct-part-1/. Accessed 10 June 2018.
Tong S, Alessio AM, Kinahan PE. Image reconstruction for PET/CT scanners: past achievement and future challenges. Imaging Med. 2010;2(5):529–45.
Koopman D, van Osch JAC, Jager PL, Tenbergen CJA, Knollema S, Slump CH, et al. Technical note: how to determine the FDG activity for tumour PET imaging that satisfies European guidelines. EJNMMI Phys. 2016;3(1):22.
Buvat I, Frey E, Green A, Ljungberg M. Quantitative nuclear medicine imaging: concepts, requirements and methods. Human health reports. Vienna: International Atomic Energy Agency; 2014.
Boellaard R, Krak NC, Hoekstra OS, Lammertsma AA. Effects of noise, image resolution, and ROI definition on the accuracy of standard uptake values: a simulation study. J Nucl Med. 2004;45:1519–27.
Ziegler S, Jakoby BW, Braun H, Paulus DH, Quick HH. NEMA image quality phantom measurements and attenuation correction in integrated PET/MR hybrid imaging. EJNMMI Phys. 2015;2(1):18.
Elschot M, Vermolen BJ, Lam MG, de Keizer B, van den Bosch MA, de Jong HW. Quantitative comparison of PET and Bremsstrahlung SPECT for imaging the in vivo yttrium-90 microsphere distribution after liver radioembolization. PLoS ONE. 2013;8(2):e55742.
Soret M, Bacharach SL, Buvat I. Partial-volume effect in PET tumor imaging. J Nucl Med. 2007;48(6):932–45.
Musarudin M, Muhammad SSH, Said M. Implementation of quadratic dose protocol for 18F-FDG whole-body PET imaging using a BGO-based PET/CT scanner, GE Discovery ST. Iran J Nucl Med. 2019;27(2):73–80.
Fukukita H, Suzuki K, Matsumoto K, Terauchi T, Daisaki H, Ikari Y, et al. Japanese guideline for the oncology FDG-PET/CT data acquisition protocol: synopsis of version 2.0. Ann Nucl Med. 2014;28:693–705.
Acknowledgements
Authors wish to acknowledge the support, succour, and cooperation given by the staff at the Nuclear Medicine Department, Institut Kanser Negara for the data information and also to Universiti Sains Malaysia, Kubang Kerian for supporting this research. This study reference NMRR-19-508-46863 had not funded by any organisation. We would like to thank the Director General of Health Malaysia for his permission to publish this article.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Said, M.A., Musarudin, M. & Zulkaffli, N.F. The quantification of PET–CT radiotracers to determine minimal scan time using quadratic formulation. Ann Nucl Med 34, 884–891 (2020). https://doi.org/10.1007/s12149-020-01543-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-020-01543-x