Abstract
Objective
The aim of this prospective pilot study was to investigate the potential of serial FLT-PET/CT compared to FDG-PET/CT to provide an early indication of esophageal cancer response to concurrent neoadjuvant chemoradiation therapy.
Methods
Five patients with biopsy-proven esophageal adenocarcinomas underwent neoadjuvant chemoradiation (Tx) prior to minimally invasive esophagectomy. The presence of residual tumor was classified histologically using the Mandard et al. criteria, categorizing patients as pathologic responders and non-responders. Participants underwent PET/CT imaging 1 h after intravenous administration of FDG and of FLT on two separate days within 48 h of each other. Each patient underwent a total of 3 scan “pairs”: (1) pre-treatment, (2) during treatment, and (3) post-treatment. Image-based response to therapy was measured in terms of changes in SUVmax (ΔSUV) between pre- and post-therapeutic FLT- and FDG-PET scans. The PET imaging findings were correlated with the pathology results after surgery.
Results
All tumors were FDG and FLT avid at baseline. Lesion FLT uptake was lower than with FDG. Neoadjuvant chemoradiation resulted in a reduction of tumor uptake of both radiotracers in pathological responders (n = 3) and non-responders (n = 2). While the difference in the reduction in mean tumor FLT uptake during Tx between responders (ΔSUV = − 55%) and non-responders (ΔSUV = − 29%) was significant (P = 0.007), for FDG it was not, [responders had a mean ΔSUV = − 39 vs. − 31% for non-responders (P = 0.74)]. The difference in the reduction in tumor FLT uptake at the end of treatment between responders (ΔSUV = − 62%) and non-responders (ΔSUV = − 57%) was not significant (P = 0.54), while for FDG there was a trend toward significance [ΔSUV of responders = − 74 vs. − 52% in non-responders (P = 0.06)].
Conclusion
The results of this prospective pilot study suggest that early changes in tumor FLT uptake may be better than FDG in predicting response of esophageal adenocarcinomas to neoadjuvant chemoradiation. These preliminary results support the need to corroborate the value of FLT-PET/CT in a larger cohort.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal cancer is among the ten most common malignancies worldwide and the seventh most common cause of cancer-related deaths in developed countries [1, 2]. Most patients are found to have advanced disease at presentation with an overall 5-year survival of 12% [2]. Preoperative and definitive combined radiation therapies are among the standard treatment options for locally advanced disease [3,4,5].
Patients who respond to neoadjuvant treatment have a better prognosis than those undergoing surgery alone. Responders have a markedly better prognosis after surgery than non-responders [6,7,8,9,10,11]. However, only 40–50% of the patients respond to neoadjuvant therapy and those who do not may be compromised by the toxic side effects of ineffective treatment. Thus, there is a need for a diagnostic test that could accurately predict tumor response non-invasively and early in the course of therapy. In this manner, non-responding patients could be identified early and be treated with a different regimen, or taken to surgery without being subjected to the potential toxicity of a full course of chemoradiation. This approach, using FDG-PET as a measure of response, has been tested in CALGB 80803, with preliminary results suggesting that changing chemotherapy regimens in patients with a poor FDG response to induction chemotherapy may increase the likelihood of achieving a pathologic complete response [12].
Currently, there is no reliable means to assess esophageal cancer response to chemoradiotherapy. Pathologic analysis following esophagectomy remains the most accurate method to determine treatment effect. Response to therapy is currently assessed by using morphologic imaging techniques, such as computed tomography (CT) and endoscopic ultrasonography [13, 14]. When using these techniques response is based on the decrease in tumor size. However, none of these routinely used methods have proven to be accurate enough to differentiate cancerous from non-cancerous tissue after treatment.
Alternative methods capable of interrogating the tumoral functional phenotype are necessary. Functional imaging using positron emission tomography (PET) has facilitated the non-invasive evaluation of tumor pathophysiology and metabolism. The basis for the use of 18F-fluorodeoxyglucose (FDG) is the increased glucose metabolism of cancer cells compared to normal tissues. Several clinical studies using FDG-PET in the neoadjuvant setting of esophageal cancer treatment have shown good correlations between an FDG-PET-based response, histological response and improved overall survival [15,16,17,18,19,20].
FDG-PET imaging is part of today’s routine cancer care, but has fundamental limitations. FDG is not strictly ‘tumor-specific’ and false-positive results may arise secondary to uptake in benign tissue and in treatment-induced inflammatory conditions. In many instances, FDG-PET may fail to distinguish between residual tumor and inflammation [20]. Therefore, there is a need to test more specific molecular imaging probes that may be able to predict and more accurately characterize early tumor response to therapy.
PET imaging with radiotracers of DNA synthesis, such as the thymidine analog 3′-deoxy-3′-18F-fluorothymidine (FLT) may prove to be more specific than FDG-PET to detect early changes in tumor proliferation as a function of treatment. FLT is a surrogate marker of the DNA salvage pathway. It is phosphorylated by thymidine kinase 1, which has increased activity during the S phase of the cell cycle, and it is retained in proliferating cells without being incorporated into DNA [21]. FLT is taken up by the normal proliferating marrow and is glucuronidated in the liver. Early clinical data with FLT imaging demonstrated that its uptake correlates well with in vitro measures of proliferation. In vitro and preclinical in vivo studies have revealed that FLT-PET is an effective molecular imaging modality to study the antiproliferative effects of different therapeutic regimens in different tumor types, including esophageal cancer [22,23,24].
Clinical studies in patients with lymphoma, breast cancer, gliomas, and esophageal squamous cell carcinomas, yielded encouraging results that demonstrated an advantage of FLT over FDG to provide earlier evidence of treatment efficacy [25,26,27,28]. The general consensus of these studies has been that FLT tumor uptake decreases early after the initiation of treatment, suggesting that imaging cell proliferation may play a significant role when monitoring anticancer therapy. However, more clinical studies are still needed to assess the value of FLT-PET to monitor response to chemoradiation in patients with esophageal cancer. Furthermore, to the best of our knowledge, there are no clinical data currently available on the assessment of response using FLT-PET compared to FDG during neoadjuvant chemoradiotherapy for esophageal adenocarcinomas.
The aim of this prospective pilot study was to investigate the potential of serial FLT-PET/CT scans compared to FDG-PET/CT scans to provide an early indication of esophageal adenocarcinoma response to concurrent neoadjuvant chemoradiation therapy.
Methods
Patient population
Inclusion criteria
Patients were considered eligible to participate in the study if they had: (1) histologically or cytologically confirmed adenocarcinoma of the esophagus or gastroesophageal junction. (2) American Joint Commission on Cancer (AJCC) Cancer Staging manual, 7th edition TNM stage T2-4, N0-2, M0 as determined by pretreatment endoscopic ultrasound [29]. T1 tumors were eligible if they were T1, N1, M0. (3) Disease clinically limited to the esophagus or gastroesophageal junction. If the tumor extended below the gastroesophageal junction into the proximal stomach, 50% of the tumor had to involve the distal esophagus or gastroesophageal junction. Adenocarcinomas of the distal esophagus included tumors of the distal esophagus, or Siewert type I, and tumors of the gastroesophageal junction, which involved equally both the distal esophagus and proximal stomach, or Siewert type II [30]. (4) Tumor surgically resectable and with a minimum length of 2 cm [19, 31], and (5) ECOG performance status 0–1 and to be a candidate for combined modality therapy with chemotherapy consisting of carboplatin and paclitaxel and concurrent radiation.
Exclusion criteria
Patients who exhibited any of the following conditions at screening were not considered eligible to participate in the study: (1) prior chemotherapy or radiotherapy. (2) Patients who had major surgery less than 4 weeks before enrollment. (3) Prior malignancies other than basal cell or squamous cell carcinoma of the skin, in situ cervical carcinoma, or superficial transitional cell bladder carcinoma. Any other prior malignancy was permitted only if diagnosed and/or treated more than 3 years before registration and without evidence of recurrence. (4) In situ carcinoma (TIS) and tumors determined to be T1N0 following endoscopic ultrasound. (5) Supraclavicular (for lower esophageal tumors) or celiac (for upper esophageal tumors) lymph node involvement, as determined by EUS, CT, or PET imaging, and confirmed histopathologically as positive for viable tumor. (6) Cervical esophageal tumors, or gastric cancers with minor involvement of the gastroesophageal junction or distal esophagus, (7) patients with tracheo-esophageal fistulas, and (8) evidence of metastatic disease.
Treatment plan
All patients received neoadjuvant chemoradiation therapy prior to surgery. Chemotherapy and radiation for esophageal cancer were delivered per standard practice.
Patients received 5040 cGy of radiation delivered over 5–6 weeks using 6 and/or 15 MV energy beams. Radiation was given over 28 fractions with a fractional dose of 180 cGy. All radiation was delivered in the supine position. All patients underwent a chemotherapy regimen of paclitaxel and carboplatin adhering to our institution’s standard of care for esophageal adenocarcinoma [5]. Administered carboplatin doses were titrated to correlate with an area under the curve (AUC) of 2 mg per milliliter per minute, and administered paclitaxel doses were 50 mg per square meter of body surface area (50 mg/m2). Minimally invasive esophagectomy was performed 5–9 weeks after completion of radiation therapy.
The duration of protocol participation was from the time of enrollment until the post-treatment scans were completed, i.e., a maximum of 14 weeks. After surgical resection, patients were followed for survival and patterns of recurrence until removal from study or until death, whichever occurred first.
Pathological analysis
All patients underwent surgical resection following neoadjuvant chemoradiotherapy. The surgical specimens were opened longitudinally from proximal to distal, and when applicable, along the greater curvature of the stomach. Sections of tumor, resection margins, areas of uninvolved esophagus and stomach, and lymph nodes were examined histologically. Tumor grading and staging were based on the AJCC TNM classification [29]. The tumor bed and residual gross lesion was examined with light microscopy. All specimens were evaluated by a gastrointestinal surgical pathologist who was unaware of the clinical and PET/CT results. Each slice containing tumor bed and residual gross lesion was examined for residual tumor, inflammation, fibrosis and necrosis. The final percentages were determined from the average value obtained from all slides.
The presence of residual tumor was classified in accordance with the criteria described by Mandard et al. [32]. Briefly, surgical samples were assigned a tumor regression grade as follows. Grade 1, no residual cancer and considered negative for tumor (based on the presence of fibrosis with or without inflammation or necrosis and absence of viable tumor cells); grade 2, rare residual cancer cells, with microscopic disease (< 10% viable tumor cells); grade 3, fibrosis outgrowing residual cancer, with sub-macroscopic disease (10–50% viable tumor cells); grade 4, residual cancer outgrowing fibrosis, with macroscopic disease (> 50% viable tumor cells), and grade 5, absence of regressive changes. The evaluation also included overall pathological therapeutic response in resected locoregional lymph nodes after therapy. Due to the small sample size, for final analysis the patients were grouped into pathologic responders (tumor regression grades 1–2) and non-responders (tumor regression grades 3–5).
Imaging protocol
After fasting for a period of 6 h, patients underwent PET/CT imaging 1 h after intravenous administration of either 444 MBq of FDG or 370 MBq of FLT. Patients were scanned with both radiotracers on two separate days within 48 h of each other. A total of three scan pairs were acquired per patient for a total of 30 PET/CT exams (15 with FDG and 15 with FLT). The studies were acquired (1) prior to radiotherapy simulation (pre-treatment scan); (2) during the second week of chemoradiation (during-treatment scan), and (3) three to four weeks after the conclusion of therapy (post-treatment scan) (Fig. 1).
Blood glucose levels were monitored prior to the FDG scans as per clinical protocol. The imaging procedure was rescheduled if glucose levels exceeded 200 mg/dL. The imaging protocol used was the same for both radiotracers. Following an uptake phase of 60 ± 10 min post-injection, patients were scanned with a combined PET/CT scanner (Discovery ST; General Electric Healthcare, Waukesha, WI, USA). Scans were acquired in the supine position with the arms placed above their heads when possible, and without any specific breath-holding instructions. Unenhanced CT scans for attenuation correction and anatomic co-registration were performed first, from the patient’s head to the mid-thighs, using the following acquisition parameters: 140kVp, 75–120 mA (varying according to the patient’s weight), 0.5 s per CT rotation, a pitch of 1.375:1, and a reconstructed slice thickness of 3.75 mm. Emission scans were acquired in 3-dimensional mode starting at the mid-thighs toward the head, for 6–7 bed positions of 3 min each. The CT data were reconstructed using a filtered backprojection algorithm. PET data were reconstructed using an ordered-subset expectation maximization iterative algorithm (28 subsets, 2 iterations) yielding a volume of 47 slices.
All patients were followed by their clinical and radiation oncologists. The study protocol was approved by our hospital Institution Review Board (IRB), and all patients gave written informed consent.
Image analysis
The visual and semi-quantitative PET image analyses of the primary lesions and lymph nodes were performed using a dedicated nuclear medicine workstation (Hermes, Stockholm, Sweden). Semi-quantitative analyses of maximum standardized uptake values (SUVmax) at each time point were generated for each lesion corrected for body weight. Circular regions of interest (ROI) of 1.5 cm in diameter were manually placed over all suspected lesions in the slice with maximum FDG and FLT uptake. If no focal uptake was visible in the follow-up scans, the ROI was placed in the same location where the lesion was identified in the baseline scan, using the anatomic landmarks of the CT images as a reference. The evaluation of tumor response to therapy in the PET images was done by quantifying changes in lesion FDG and FLT uptake between baseline and post-therapeutic scans using the following equation:
Due to the small number of subjects included in this pilot study, for final analysis the patients were grouped into responders (CR + PR) and non-responders (SD + PD).
Statistical analysis
Results were expressed as the mean ± SD. Image-based response to therapy was assessed in terms of lesion uptake values and changes in lesion SUVmax between pre- and post-therapeutic images on FLT-PET/CT and on FDG-PET/CT scans. PET findings were correlated with pathology results after surgery. Comparisons of changes in lesion’s metabolic and proliferative activity during and after treatment between responders and non-responders were performed using a two-tailed t test. P < 0.05 was used to define statistical significance.
Results
This prospective pilot study enrolled five consecutive patients that were males with a mean age, 63.4 ± 11 years, with biopsy-proven, resectable adenocarcinoma of the esophagus or the gastroesophageal junction. All patients underwent esophagogastroduodenoscopy with biopsy of the primary lesion within 2 weeks before the PET studies, and had concomitant endoscopic ultrasound (EUS) for staging. Table 1 summarizes the characteristics of the patients enrolled in this pilot study, as well as the results of PET-derived tumoral proliferative and metabolic analyses.
Fifty-two ± fourteen days after the end of neoadjuvant radiochemotherapy all patients underwent Ivor-Lewis esophagectomy with radical lymph node dissection. Pathological analyses of the surgical specimens revealed treatment response in three patients and lack of response in two. Pathological stages before/after therapy were as follows: patient 1, T3N2M0/T3N2/M0; patient 2, T3N2M0/T1aN0M0; patient 3, T3N1M0/T3N1M0; patient 4, T3N1M0/T1aN0M0, and patient 5, T3N2M0/T2N1M0.
All patients underwent FDG and FLT-PET imaging at baseline, during treatment and post-treatment, for a total of 30 imaging sessions. All scans for a given patient and for both radiotracers were acquired using the same scanner. The average time that lapsed between baseline PET/CT imaging and the start of treatment was 13 ± 4 days for FDG and 3 ± 4 days for FLT. During-treatment scans were acquired 18 ± 2 days for FDG, and 16 ± 2 days for FLT, and the post-treatment scans were obtained 30 ± 6 days for FDG, and 30 ± 7 days for FLT.
Pre-treatment analysis
All tumors were FDG (mean SUVmax = 6.9 ± 2.9) and FLT avid (mean SUVmax = 4.7 ± 0.9) at baseline. While lesion FLT uptake was lower than FDG, the difference was not statistically significant. The mean tumor FDG SUVmax of responders before therapy was 4.97 ± 0.05, compared to 10.0 ± 1.79 in non-responders (P = 0.01). The mean tumor FLT SUVmax of responders before treatment was 5.01 ± 1.01, compared to 4.21 ± 0.62 in non-responders (P = 0.08).
Early during treatment analysis
There was good agreement in tumor response to treatment between both radiotracers. Neoadjuvant chemoradiation resulted in a reduction of tumor uptake of both FDG and FLT, which in turn continued to decrease as a function of treatment in both responders (n = 3) and non-responders (n = 2). The mean tumor FDG SUVmax of responders early during treatment was 3.44 ± 0.64, compared to 5.06 ± 1.33 in non-responders (P = 0.25). The mean tumor FLT SUVmax of responders early during treatment was 2.19 ± 0.24, compared to 2.99 ± 0.29 in non-responders (P = 0.08). While there was a significant difference in the reduction of mean tumor FLT uptake during treatment between responders (ΔSUV = − 55 ± 5%) and non-responders (ΔSUV = − 29 ± 4%) (P = 0.007) (Fig. 2), for FDG there was not, with responders having a mean tumor ΔSUV = − 39 ± 26% vs. a ΔSUV = − 31 ± 22% in non-responders (P = 0.74) (Fig. 3).
Post-treatment analysis
The mean tumor FDG SUVmax of responders at the end of treatment was 1.61 ± 0.55, compared to 4.08 ± 2.85 in non-responders (P = 0.08). The mean tumor FLT SUVmax of responders post-treatment was 1.83 ± 0.23, compared to 1.82 ± 0.54 in non-responders (P = 0.98).
The difference in the reduction in mean tumor FLT uptake at the end of treatment between responders (ΔSUV = − 62 ± 9%) and non-responders (ΔSUV = − 57 ± 6%) was no longer significant (P = 0.54) (Fig. 2), while for FDG there was a clear trend toward significance, with responders having a mean tumor ΔSUV = − 74 ± 8% compared to a ΔSUV = − 52 ± 8% in non-responders (P = 0.06) (Fig. 3).
In both the during-treatment and post-treatment images of responders, we consistently observed significant reductions in FLT as well as FDG tumoral uptake while tumor bulk remained on CT images throughout treatment (Figs. 4, 5).
Representative axial PET and PET/CT fused slices of pathologically confirmed responder (71 year-old male with a T3N2M0 esophageal adenocarcinoma at baseline downstaged to T1aN0M0 after therapy) in whom there is a more pronounced reduction (− 60%) of gastro-esophageal tumor FLT uptake during treatment compared to FDG (− 33%) (arrowheads), with FLT providing earlier and more convincing evidence of treatment efficacy. At the end of treatment both tumor FLT and FDG uptake continue to decrease to normal gastroesophageal uptake levels (asterisks) [− 73% for FLT and -80% for FDG from pre-treatment uptake (arrows)]
Pathologically confirmed responder (50 year-old male with a T3N2M0 esophageal adenocarcinoma at baseline downstaged to T2N1M0 after therapy) with a 50 % reduction in esophageal tumor FLT uptake (arrowheads) during treatment compared to baseline (arrows), which continues to further decrease to almost background levels as evidenced in the post-treatment images (asterisks), predicting favorable response. On the other hand FDG tumor uptake decreases only partially during therapy (17%) (arrowheads), most likely due to radiation induced inflammation, to finally decrease to 65% from baseline uptake, but with a persistent small focus of FDG activity after the end of treatment (asterisks). There is no evidence of decrease in tumor bulk during treatment in CT images despite the reduction in proliferative and metabolic activity in the PET images
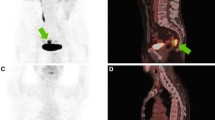
Marked early reduction of FLT uptake in irradiated bone marrow corresponding to the paths of the radiation beams was observed in all patients. There was decreased uptake in irradiated spine, ribs and sternum consistent with decreased cell proliferation in the areas subjected to radiation treatment. In the post-treatment images uptake in the irradiated marrow increased to almost normal levels, consistent with marrow repopulation and reactivation of proliferative activity (Fig. 6). Bone marrow uptake reduction was also observed in the FDG images, but it was not as pronounced as in the FLT scans.
Representative Sagittal FLT-PET images obtained before, during and after treatment. Note the more pronounced decrease in FLT uptake in the irradiated vertebral bone marrow and the sternum corresponding to the paths of the radiation beams, consistent with decreased cell proliferation during treatment. In the post-treatment images uptake in the irradiated marrow increases to almost normal levels consistent with marrow repopulation and reactivation of proliferative activity
Discussion
The primary aim of this prospective pilot study was to evaluate the use of serial FLT-PET/CT as an early biomarker of clinical response to neoadjuvant chemoradiotherapy compared to FDG-PET/CT in patients with esophageal adenocarcinomas.
As indicated previously, while all tumors were FDG and FLT avid at baseline, FLT uptake was lower than FDG. This may be explained by the fact that not all metabolically active tumor cells are proliferating at any given time. It is well known that the intensity of FDG uptake is lower in esophageal adenocarcinomas compared to those of the squamous cell type [33]. Interestingly, it seems like the same might hold true with FLT uptake. In our study, the mean tumor FLT SUVmax of esophageal adenocarcinomas at baseline was 4.7 and lower than that reported for squamous cell carcinomas of the esophagus by other investigators. Yue and colleagues [27] reported a baseline tumor FLT mean SUVmax of 9.7 in their cohort of 21 patients with esophageal squamous cell carcinomas, while in the study by Park et al. [28] the average FLT SUVmax of 13 esophageal squamous cell tumors was 6.7.
Our study showed that neoadjuvant chemoradiation resulted in a reduction of tumor FDG and FLT uptake, with tumor avidity continuing to decrease with increased radiation dose in both responders and non-responders. These reductions in the intensity of FLT and FDG uptake as a function of chemoradiotherapy are consistent with tumoral proliferative and metabolic response to treatment, respectively. The observed differences in the decrease in tumor uptake between FLT (55% in responders versus 29% in non-responders) and FDG (39 vs. 31%, respectively) early during treatment, suggest that chemoradiotherapy might affect tumor cell proliferation faster than their glycolytic metabolic pathway. These results were in fact comparable to those of other investigators studying the value of FLT to monitor response to treatment of esophageal squamous cell carcinomas [28, 34]. Park and colleagues recently published their results of a small study investigating FLT-PET as a biomarker of early response to induction chemotherapy with S-1 and oxaliplatin before radiotherapy and resection of esophageal squamous cell tumors [28]. The authors indicated that they observed a median decrease of 57.1% in tumor FLT uptake in the 8 patients that responded to the first two cycles of chemotherapy, compared to 10.2% in the only patient who did not respond to therapy. The authors concluded that the early decrease in FLT uptake as a function of induction chemotherapy might prove as a useful predictor of treatment response.
As indicated above FLT-PET revealed early therapy-induced changes in tumor proliferation in response to treatment. While the difference in the reduction in tumor FLT uptake during treatment between responders and non-responders was statistically significant, for FDG it was not. This may be explained by the fact that FLT uptake is not affected as much as FDG uptake is by radiation-induced inflammation. In contrast, it is well known that this nonspecific FDG uptake may lead to overestimation of the proportion of viable tumor cells during therapy, making it difficult to differentiate tumors responding to treatment from those that are not (Fig. 5). In fact, in responders with persistent FDG uptake, histopathological analysis demonstrated inflammatory infiltrates with no residual tumor, consistent with esophagitis. This correlates well with our previously published findings [19] and are similar to those reported by Yue and colleagues in esophageal squamous cell carcinomas [27]. These investigators argued that FLT-PET may able to differentiate between inflammation and viable tumor uptake, while confirming chemoradiotherapy treatment efficacy.
The difference in the reduction in tumor FLT uptake at the end of treatment between responders and non-responders was not statistically significant in our cohort (Fig. 2), while for FDG there was a clear trend toward significance (Fig. 3). At the end of treatment FLT uptake might have been influenced by the continuous effect of radiation that reduced the proliferative capacity of viable tumor cells remaining after treatment. The lack of a considerable reduction of inflammatory response at this stage minimized non-specific FDG uptake, and therefore, allowed for a more clear distinction in radiotracer uptake between responders and non-responders.
While no meaningful survival comparisons could be made between responders and non-responders in our small study, the data showed that a reduction in tumor proliferation during treatment correlated well with survival in our patient population. These results are in line with those of Chen et al. who studied 34 patients with esophageal squamous cell cancers and reported that proliferative response early during treatment (4 weeks after the start of radiotherapy or chemoradiotherapy) may carry important prognostic information [34]. They reported very similar ΔSUV changes in terms of reduction in proliferative and metabolic activity as a function of treatment. Patients with an FLT ΔSUV greater than 60% during treatment (interim PET negative group) had a better 2-year progression-free survival (PFS) and loco-regional control (LRC) than the interim PET-positive group (P = 0.046). The FDG-PET/CT scan demonstrated better prediction of PFS and LRC when the reduction in metabolic activity as a function of treatment was 75% or higher in the post-treatment scan (P = 0.016). An SUVmax that decreased more than 75% on the final FDG-PET/CT scan was associated with better clinical outcome (PFS: 73.3 vs. 36.8%, P = 0.022; LRC: 86.7 vs. 52.6%, P = 0.029). The investigators emphasized that these results were most noticeable in the subgroup of patients treated with chemoradiotherapy.
The main limitation of this pilot study is the small number of patients; however, its main strength is that all patients had paired (FLT and FDG) PET studies three times prospectively. We analyzed data from multiple imaging sessions (N = 30) with both radiotracers for each patient, and some clinically important and interesting correlations could be demonstrated. If further studies confirm the FLT uptake phenotype during treatment as an accurate predictor of final tumor response, the early identification of those patients not responding could direct change in the therapy algorithm potentially improving survival and quality of life.
Conclusion
The preliminary results of this prospective pilot study underline the potential of FLT-PET/CT as an indicator of early response of esophageal cancer to neoadjuvant treatment. Changes in tumor FLT uptake early during treatment appear to be better than FDG to predict the effect of concurrent neoadjuvant chemoradiotherapy on esophageal adenocarcinomas. These results support additional studies to build upon our observations and validate the clinical value of FLT-PET/CT in a larger cohort, clarifying the meaning of interim scan findings in the context of prognostic significance.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics 2017. CA: A Cancer J Clin. 2017;67:7–30.
Blot WJ, Devesa SS, Kneller RW, Fraumeni JF Jr. Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA. 1991;265:1287–9.
Sjoquist KM, Burmeister BH, Smithers BM, Zalcberg JR, Simes RJ, Barbour A, Gebski V. Australasian Gastro-Intestinal Trials Group. Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: an updated meta-analysis. Lancet Oncol. 2011;12:681–92.
Ronellenfitsch U, Schwarzbach M, Hofheinz R, Kienle P, Kieser M, Slanger TE, et al. Preoperative chemo(radio)therapy versus primary surgery for gastroesophageal adenocarcinoma: systematic review with meta-analysis combining individual patient and aggregate data. Eur J Cancer. 2013;49:3149 – 3148.
Oppedijk V, van der Gaast A, van Lanschot JJ, van Hagen P, van Os R, van Rij CM, et al. Patterns of recurrence after surgery alone versus preoperative chemoradiotherapy and surgery in the CROSS trials. J Clin Oncol. 2014;32:385–91.
Davies AR, Gossage JA, Zylstra J, Mattsson F, Lagergren J, Maisey N, et al. Tumor stage after neoadjuvant chemotherapy determines survival after surgery for adenocarcinoma of the esophagus and esophagogastric junction. J Clin Oncol. 2014;32:2983–90.
Schmidt T, Sicic L, Blank S, Becker K, Weichert W, Bruckner T, et al. Prognostic value of histopathological regression in 850 neoadjuvantly treated oesophagogastric adenocarcinomas. Br J Cancer. 2014;110:1712–20.
Ancona E, Ruol A, Santi S, Merigliano S, Sileni VC, Koussis H, Zaninotto G, et al. Only pathologic complete response to neoadjuvant chemotherapy improves significantly the long term survival of patients with resectable esophageal squamous cell carcinoma: final report of a randomized, controlled trial of preoperative chemotherapy versus surgery alone. Cancer. 2001;91:2165–74.
Le Prise E, Etienne PL, Meunier B, Maddern G, Ben Hassel M, Gedouin D, et al. A randomized study of chemotherapy, radiation therapy, and surgery versus surgery for localized squamous cell carcinoma of the esophagus. Cancer. 1994;73:1779–84.
Walsh TN, Noonan N, Hollywood D, Kelly A, Keeling N, Hennessy TP. A comparison of multimodal therapy and surgery for esophageal adenocarcinoma. N Engl J Med. 1996;335:462–7.
Urba SG, Orringer MB, Turrisi A, Iannettoni M, Forastiere A, Strawderman M. Randomized trial of preoperative chemoradiation versus surgery alone in patients with locoregional esophageal carcinoma. J Clin Oncol. 2001;19:305–13.
Goodman KA, Niedzwiecki D, Hall N, et al. Initial results of CALGB 80803 (Alliance): a randomized phase II trial of PET scan-directed combined modality therapy for esophageal cancer. Presented at: 2017 Gastrointestinal Cancers Symposium. January 19–21, 2017; San Francisco, California; Abstract 1.
Zuccaro G Jr, Rice TW, Goldblum J, Medendorp SV, Becker M, Pimentel R, et al. Endoscopic ultrasound cannot determine suitability for esophagectomy after aggressive chemoradiotherapy for esophageal cancer. Am J Gastroenterol. 1999;94:906–12.
Jones DR, Parker LA Jr, Detterbeck FC, Egan TM. Inadequacy of computed tomography in assessing patients with esophageal carcinoma after induction chemoradiotherapy. Cancer. 1999;85:1026–32.
Swisher SG, Erasmus J, Maish M, Correa AM, Macapinlac H, Ajani JA, et al. 2-Fluoro-2-deoxy-D-glucose positron emission tomography imaging is predictive of pathologic response and survival after preoperative chemoradiation in patients with esophageal carcinoma. Cancer. 2004;101:1776–85.
Flamen P, Van Cutsem E, Lerut A, Cambier JP, Haustermans K, Bormans G, et al. Positron emission tomography for assessment of the response to induction radiochemotherapy in locally advanced oesophageal cancer. Ann Oncol. 2002;13:361–8.
Wieder HA, Brücher BL, Zimmermann F, Becker K, Lordick F, Beer A, et al. Time course of tumor metabolic activity during chemoradiotherapy of esophageal squamous cell carcinoma and response to treatment. J Clin Oncol. 2004;22:900–8.
Brücher BL, Weber W, Bauer M, Fink U, Avril N, Stein HJ, et al. Neoadjuvant therapy of esophageal squamous cell carcinoma: response evaluation by positron emission tomography. Ann Surg. 2001;233:300–9.
Mamede M, Abreu-E-Lima P, Oliva MR, Nosé V, Mamon H, Gerbaudo VH. FDG-PET/CT tumor segmentation-derived indices of metabolic activity to assess response to neoadjuvant therapy and progression-free survival in esophageal cancer: correlation with histopathology results. Am J Clin Oncol. 2007;30:377–88.
Lordick F, Ott K, Krause BJ, Weber WA, Becker K, Stein HJ, et al. PET to assess early metabolic response and to guide treatment of adenocarcinoma of the oesophagogastric junction: the MUNICON phase II trial. Lancet Oncol. 2007;8:797–805.
Toyohara J, Waki A, Takamatsu S, Yonekura Y, Magata Y, Fujibayashi Y. Basis of FLT as a cell proliferation marker: comparative uptake studies with [3H]thymidine and [3H]arabinothymidine, and cell analysis in 22 asynchronously growing tumor cell lines. Nucl Med Biol. 2002;29:281–7.
Dittmann H, Dohmen BM, Kehlbach R, Bartusek G, Pritzkow M, Sarbia M, et al. Early changes in [18F]FLT uptake after chemotherapy: an experimental study. Eur J Nucl Med Mol Imaging. 2002;29:1462–9.
Perumal M, Pillai RG, Barthel H, Leyton J, Latigo JR, Forster M, et al. Redistribution of nucleoside transporters to the cell membrane provides a novel approach for imaging thymidylate synthase inhibition by positron emission tomography. Cancer Res. 2006;66:8558–64.
Apisarnthanarax S, Alauddin MM, Mourtada F, Ariga H, Raju U, Mawlawi O, et al. Early detection of chemoradioresponse in esophageal carcinoma by 3′-deoxy-3′-3H-fluorothymidine using preclinical tumor models. Clin Cancer Res. 2006;12:4590–7.
Pio BS, Park CK, Pietras R, Hsueh WA, Satyamurthy N, Pegram MD, et al. Usefulness of 3′-[F-18]fluoro-3′-deoxythymidine with positron emission tomography in predicting breast cancer response to therapy. Mol Imaging Biol. 2006;8:36–42.
Herrmann K, Wieder HA, Buck AK, Schöffel M, Krause BJ, Fend F, et al. Early response assessment using 3′-deoxy-3′[18F]fluorothymidine-positron emission tomography in high-grade non-Hodgkin’s lymphoma. Clin Cancer Res. 2007;13:3552–8.
Yue J, Chen L, Cabrera AR, Sun X, Zhao S, Zheng F, et al. Measuring tumor cell proliferation with 18F-FLT PET during radiotherapy of esophageal squamous cell carcinoma: a pilot clinical study. J Nucl Med. 2010;51:528–34.
Park SH, Ryu JS, Oh SJ, Park SI, Kim YH, Jung HY, et al. The feasibility of (18)F-Fluorothymidine PET for prediction of tumor response after induction chemotherapy followed by chemoradiotherapy with S-1/oxaliplatin in patients with resectable esophageal cancer. Nucl Med Mol Imaging. 2012;46:57–64.
Edge SB, Byrd DR, Compton CC et al, editors Esophagus and esophagogastric junction. AJCC Cancer Staging Manual. 7th ed. New York: Springer; 2010: pp. 103–15.
Siewert JR, Stein HJ. Classification of adenocarcinoma of the oesophagogastric junction. Br J Surg. 1998;85:1457–9.
Mamede M, El Fakhri G, Abreu-e-Lima P, Gandler W, Nosé V, Gerbaudo VH. Pre-operative estimation of esophageal tumor metabolic length in FDG-PET images with surgical pathology confirmation. Ann Nucl Med. 2007;21:553–62.
Mandard AM, Dalibard F, Mandard JC, Marnay J, Henry-Amar M, Petiot JF, et al. Pathologic assessment of tumor regression after preoperative chemoradiotherapy of esophageal carcinoma. Clinicopathologic correlations. Cancer. 1994;73:2680–6.
Brown RS, Leung JY, Kison PV, Zasadny KR, Flint A, Wahl RL. Glucose transporters and FDG uptake in untreated primary human non-small cell lung cancer. J Nucl Med. 1999;40:556–65.
Chen H, Li Y, Wu H, Sun L, Lin Q, Zhao L. 3′-deoxy-3′-[18F]-fluorothymidine PET/CT in early determination of prognosis in patients with esophageal squamous cell cancer: comparison with [18F]-FDG PET/CT. Strahlenther Onkol. 2015;191:141–52.
Funding
Technology and Innovation Grant from the Kaye Scholar Award at Brigham and Women’s Hospital, Boston, MA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No potential conflicts of interest were disclosed.
Rights and permissions
About this article
Cite this article
Gerbaudo, V.H., Killoran, J.H., Kim, C.K. et al. Pilot study of serial FLT and FDG-PET/CT imaging to monitor response to neoadjuvant chemoradiotherapy of esophageal adenocarcinoma: correlation with histopathologic response. Ann Nucl Med 32, 165–174 (2018). https://doi.org/10.1007/s12149-018-1229-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-018-1229-0