Abstract
Conventional MRI protocols are an integral part of routine clinical imaging in pediatric patients. The advent of several newer MRI techniques provides crucial insight into the structural integrity and functional aspects of the developing brain, especially with the introduction of 3T MRI systems in clinical practice. The field of pediatric neuroimaging continues to evolve, with greater emphasis on high spatial resolution, faster scan time, as well as a quest for visualization of the functional aspects of the human brain. MR vendors are increasingly focusing on optimizing MR technology to make it suitable for children, in whom as compared to adults the head size is usually smaller and demonstrates inherent neuroanatomical differences relating to brain development. The eventual goal of these advances would be to evolve as potential biomarkers for predicting neurodevelopment outcomes and prognostication, in addition to their utility in routine diagnostic and therapeutic decision-making. Advanced MR techniques like diffusion tensor imaging, functional MRI, MR perfusion, spectroscopy, volumetric imaging and arterial spin labeling add to our understanding of normal brain development and pathophysiology of various neurological disease processes. This review is primarily focused on outlining advanced MR techniques and their current and potential pediatric neuroimaging applications as well as providing a brief overview of advances in hardware and machine design.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
MR imaging has evolved significantly in the last two decades with advances in hardware design and software capabilities. There has however been a slight lag in the translation of these technical developments for clinical applications, especially in pediatric imaging due to the unique set of challenges in imaging this subset of the population [1]. With growing concerns for radiation exposure with CT scanning, particularly in children, there has been a paradigm shift with increasing scope and focus on newer MR applications for diagnosis, prognosis, treatment monitoring and research in various pediatric neurological diseases.
Conventional MRI
Conventional MRI sequences include T1W, T2W, FLAIR, GRE and diffusion weighted (DW) images. Typically T1weighted images are used for depiction of anatomy and T2 weighted and FLAIR images for depicting tissue pathology. Gradient T2W images are sensitive to the presence of blood products and calcium. Diffusion images reflect changes in the mobility of water molecules within tissues that help characterize pathologies.
Advances in Hardware and Machine Design
Most pediatric academic centers show a trend towards reduced use of CT scans and concomitant shift to MR as a preferred modality for pediatric neuroimaging. This has led to an increase in initiatives to customize hardware designs specifically suited to children. Examples include child-friendly MR suites, smaller head coils for increased resolution, and noise cancellation technology for MRI sequences [2]. In order to improve patient comfort, newer generation MRI scanners are designed with shorter tunnels and wider bores. Parallel advances in software design with faster sequences; better resolution and potential novel solutions like motion detection-correction are extremely useful in clinical pediatric neuroimaging. The use of multichannel data acquisition enables faster structural and functional imaging, for e.g., Echo planar imaging (EPI) with higher temporal resolution and less geometric distortion [3]. Audiovisual aids such as goggles and headphones are now commonly used for improving ‘patient-centric’ scanning experience that can help mitigate anxiety by distracting from the otherwise intimidating environment for a child.
While the above measures have significantly aided imaging older children, additional challenges in imaging neonates and premature babies in the NICU setting include reducing scan time and managing the logistics of transportation. A small footprint neonatal MR system, which can be set up in the NICU is an excellent practical illustration of these advances. There are however significant technical challenges such as compatible incubators, smaller magnet coils and electronic and software modifications needed for such sites [2, 4]. Rapid change in technology allows continuous improvement in safety and imaging quality, with the aim to attain capabilities that would no longer preclude any extremely ill neonate from undergoing an MR examination.
Diffusion Tensor Imaging
Diffusion weighted imaging (DWI) is part of the routine pediatric brain protocol. Diffusion tensor imaging (DTI) is an advanced application of diffusion-weighted imaging that measures the rate of random motion of water molecules in different directions. DTI exploits the correlation between the direction dependent diffusion of water molecules (anisotropy) and thus depicts white matter tract orientation.
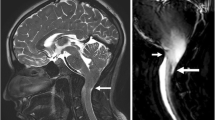
Maximum diffusivity is along the longitudinal course of the fiber tract. DTI can be further characterized by scalar quantities including fractional anisotropy (FA) maps. FA maps are cross sectional representations of directional information that may be represented in grey scale or can be colour coded; FA maps portray diffusivity along white matter tracts [5–9]. Anisotropic (direction dependent) diffusion is represented as bright areas on FA maps and the intensity is proportional to the degree of anisotropy. The diffusion of a water molecule is directional in normal fiber tracts (high FA). With any disruption of the normal anisotropy in affected tracts, the FA decreases (Fig. 1). Mean diffusivity (MD) is another such scalar derivative of DTI, which is predominantly affected by cellular size, contents and integrity. The principle direction of diffusion in a vector is called as an Eigen vector and the representation of the white matter pathway can be processed by visualizing Eigen vectors in adjacent voxels: a technique known as fibre tractography [10] (Fig. 2).
While conventional T1 and T2 weighted images are valuable in diagnosing gross abnormalities in a premyelinated brain, DTI provides better anatomic information and quantitative assessment of the white matter microstructure [9, 11]. DTI has been used to assess maturation as well as to quantitatively evaluate milestones in brain development. Diffusion values decrease in the brain during maturation, the changes being most rapid in the first 2 y after birth, with significant reduction in water content [5, 8]. Maturation of the brain is characterized by increased FA [12–14]. Anisotropy of the white matter increases progressively with age in the post natal period [9]. Various mechanisms believed to contribute to this phenomenon include myelination, axonal proliferation and intercellular tortuosity amongst others factors [7, 9]. These changes continue to proceed at a slower rate into adolescence.
DTI provides a window for early detection of the brain injury, which may serve as an early marker reflecting hypoxic ischemic damage. This is particularly critical in the absence of significant findings on conventional MR and in the context of neuro-protective agents and monitoring therapy [7, 15]. DTI in newborns has the potential to evaluate the structural correlate of functional impairment and plasticity in the developing brain [5]. Increase in FA in specific white matter regions in the preterm has been shown to relate to cognitive, fine motor and gross motor outcomes at 2 y of age [16, 17]. Similarly, DTI can also measure white matter changes and associated cognitive dysfunction following mild to moderate traumatic brain injury [18, 19].
The relationship of white matter tracts to space occupying lesions including tumors is crucial in guiding surgical approach and defining the extent of resection. Pre-operative tractography helps prognosticate outcome and predicts potential neurodeficit. Depiction of either infiltration or displacement of white matter tracts by FA and tractography in patients with infiltrating neoplasms (Fig. 3) is important while making pre surgical decisions with regards to the extent of resection [7, 20]. In patients undergoing radiation and chemotherapy, reduction in FA values due to white matter injury has been shown to be associated with poor intellectual outcomes [8, 21].
Demyelinating lesions and normal appearing white matter in multiple sclerosis (MS) patients usually show decreased FA when compared with control subjects. Acute plaques have been reported to demonstrate altered radial diffusivity [22]. Elevated FA has also been documented in brain abscess cavities. This has been correlated with neuro-inflammatory molecules in pus. The reduction in FA following treatment in brain abscess is a potential tool to assess response and surveillance [23].
DTI has also shown utility in evaluating neuroanatomical features in several congenital disorders including holoprosencephaly, corpus callosal agenesis, horizontal gaze palsy with progressive scoliosis and pontine tegmental cap dysplasia [24]. Structural changes such as absence of cortico-spinal tracts in holoprosencephaly, and failed commissural fibers with Probst bundles in agenesis of corpus callosum are well demonstrated with DTI [24]. DTI can also be used to predict outcome in leukodystrophies such as Krabbe’s and X linked adrenoleukodystrophy, in which decreased white matter FA is seen [6].
Abnormal white matter development and persistent degeneration with increasing age has been reported in patients with spina bifida and myelomeningocele [25]. There is a significant decrease in FA value observed in most white matter regions in adolescents with myelomeningocele. DTI shows reduction in structural white matter integrity across major white matter tracts. Reduced anisotropy has also been seen in white matter tracts in patients with temporal lobe epilepsy suggesting disruption of the networks in these patients [26].
Newer high resolution techniques using diffusion tensor imaging aim to understand structural and functional details of the brain network with future prospects of being able to match individual connectomes [27], which will eventually help investigate a broad spectrum of neurological and behavioral disorders.
Functional MR (fMR)
Functional MR (fMR) studies are based on blood oxygen level dependent (BOLD) techniques. fMR has the ability to demonstrate eloquent functional areas with neuro-anatomical localization. The basis of functional MRI is that task driven neuronal activities cause localized change in cerebral blood flow, which results in a decrease in de-oxyhemoglobin and a resultant increase in MR signal in that particular location [28, 29]. Thus fMR is an indirect assessment of neuronal activity with a slight temporal delay [30]. fMR paradigms are usually designed with repeated sampling of brain volume with the subject alternating between an active and a controlled task such as ‘finger tapping’ followed by ‘rest’. Children usually demonstrate widespread activations to a given task [31], which becomes more localized as the brain matures. Two widely used clinical applications of fMR include preoperative assessment of language and memory function prior to surgery for intractable epilepsy (Fig. 4), and presurgical evaluation of potentially eloquent cortex in patients with focal lesions. fMR has an ability to guide tailored tumor resection, with an aim to spare the eloquent cortex [20] (Fig. 5).
Presurgical functional MRI evaluation with motor task in a 13-y-old: Bilateral finger tapping demonstrates anterior displacement of the primary sensory-motor cortex (SM1) by the tumor on the right side. The normal left primary sensory motor cortex and the supplementary motor areas (SMA) are also identified
Language tasks with paradigms using verb generation, semantic decision and story processing for example, engage several language domains and fully define language processing [32, 33]. Language reorganization and plasticity resulting from various neuro-pathological conditions make it imperative to use multiple tasks during fMR studies. Language lateralization in children with epilepsy has been shown to correlate with invasive tests like WADA, making fMR a suitable noninvasive substitute for language lateralization [34, 35].
fMR applications in children are increasingly used for neurobehavioral and cognitive disorders, while language organization and lateralization are major fields of research for understanding brain plasticity [36]. In children, the most critical period for language development is early (6–7 y of life) with more limited development during later years [31, 36]. Anatomical and physiological changes in neuronal development alter the BOLD response in children to a greater extent as compared to that in adults. Neonates and infants may exhibit a negative BOLD response, probably reflecting the inadequate cerebral blood flow (CBF) increase to compensate for O2 metabolism [36].
Resting state fMR has recently emerged as a novel way for investigating development of large-scale functional networks in the brain. The procedure allows for the assessment of resting state connectivity using spontaneous synchronized fluctuations in the bold signal, to determine functional brain network independent of transient task induced correlations [37, 38]. The advantage of resting state fMR is its ability to examine functional organization of the brain, independent of task performance within a short period of time, with minimal cognitive burden, and without sedation [39]. Resting state fMR networks show that children have stronger subcortical connections whereas adults show greater cortical-cortical connectivity [40]. Default mode networks seen on resting state fMR have been shown to develop during the period of rapid growth, in late gestation before acquisition of cognitive competency in childhood [41, 42]. Resting state fMR also demonstrates altered structural and functional under-connectivity between multiple brain regions in individuals with autistic spectrum disorder [43].
MR Perfusion
Dynamic contrast enhanced MR is routinely used to assess tissue vascularity following a bolus of contrast injection. Evaluation of perfusion MR is based on the passage of paramagnetic contrast material through the capillary bed allowing generation of maps of various hemodynamic parameters like cerebral blood volume (CBV), cerebral blood flow (CBF), mean transit time (MTT) and time to peak (TTP) [44, 45]. Dynamic contrast enhanced MR is broadly grouped as dynamic susceptibility contrast (DSC) (T2 weighted) and dynamic contrast enhancement (DCE) (T1 weighted), which is also known as permeability imaging. These techniques have been used in acute and chronic, focal and global processes including tumor imaging, ischemic cerebrovascular disease, moyamoya, vascular malformations, trauma, and vasculopathy to name a few.
MR perfusion helps identify and differentiate tumors, predict grade and anaplastic transformation, guide stereotactic biopsies, and predict therapeutic response and prognosis [7, 46]. Relative cerebral blood volume (rCBV) can distinguish pediatric brain tumors with progression from tumors that are stable [44]. Tumors with higher rCBV values tend to be associated with a higher histopathological grade [47] (Fig. 6).
T1W (a), T2W (b), and MR perfusion CBV maps (c & d) in a child with diffuse intrinsic pontine glioma (white arrows in a). The CBV maps show a focal area of hypervascularity (white arrow in c and d) within the tumor corresponding to the area of contrast enhancement on the T1W image (red arrow in a) suggesting an area of anaplastic transformation
MR perfusion is useful in acute arterial ischemic stroke for defining infarct core, identifying penumbra for viable tissue, and guiding therapeutic decisions. In primary cerebral vasculopathy like moyamoya, perfusion MR is important for evaluating hemodynamics of the collateral circulation and for assessing change in the hemodynamic status of the collateral circulation following a bypass surgery [44].
Amongst the newer perfusion parameters that are increasingly used, volume transfer constant (K trans) is a parameter based on the trans-endothelial transport of the contrast agent by diffusion. Some of these parameters have the potential to evolve as imaging biomarkers of tumor response to therapy [47].
Measures of brain perfusion correlate with brain maturation and increasing perfusion is seen in areas that are myelinating. CBF is typically lower in neonates compared with older children and increases in early childhood with a peak at 7 y; CBF reaches adult values around adolescence [44]. The frontal association cortex is the final area in which cerebral perfusion increases.
Arterial spin labeling (ASL) is a newer technique, which is based on saturation pulses that label blood before it flows into the brain [45]. The major advantage of ASL is that it requires no injection of contrast. In more recent studies using ASL in various types of brain tumors and correlating with tumor grade, relative tumor blood flow is able to distinguish high-grade from low-grade tumors [48, 49]. Use of ASL in perinatal arterial ischemic stroke showed significant abnormalities associated with infarcted areas in the acute and subacute phase [50]. ASL can also provide information on small vessel status in silent sickle cell disease, and can identify patients at a risk of stroke.
MR Spectroscopy
MR spectroscopy (MRS) is a noninvasive MR technique used to demonstrate and quantify cellular metabolites in pediatric neurological diseases. MR spectroscopic studies are usually performed using various techniques including single and multi-voxel MRS.
Common metabolite markers routinely evaluated with MR spectroscopy (MRS) include N-acetylaspartate (NAA) which is a marker reflecting neuronal viability and integrity, choline (Cho) which represents cell membrane turnover and cellular density, and creatine (Cr), a metabolite related to energy metabolism. Additional metabolites like lactate (Lac) which is present in response to anaerobic metabolism, and glutamine/glutamate (Glx) and myoinositol (mI) which represent astrocytic response are also routinely evaluated [51, 52]. The most prominent peak visualized on MRS after brain maturation is NAA at 2.0 ppm. Spectral peaks for choline and creatine are identified at 3.2 ppm and 3.0 ppm respectively. Lactate is typically seen as a doublet at 1.3 ppm while lipids and macromolecules are located at 0.9 ppm and 1.3 ppm on proton spectra. Myoinositol (mI) is better quantified on a short time to echo (TE) at 3.6 ppm (Table 1).
High choline and lower NAA peaks in the neonatal brain reflect a need for high level of substrate early in development and during progressive maturation of the brain [53]. The ratio of these metabolites shows reversal of peaks in the first few months with progressive maturation.
A common clinical application of MRS is in neonatal hypoxic ischemic injury (HIE) where MRS can provide additional information compared to conventional imaging. Elevated lactate may be seen within a few hours of the insult with reduced NAA and elevated glutamine evident after 24 h [54, 55]. The lactate /NAA ratio is one of the potential prognosticators for neonatal HIE with elevated levels associated with worse outcomes [56].
Conventional MR has limited specificity for inborn errors of metabolism, including organic acidemias, disorders of amino-acids metabolism, fatty acid oxidations, mitochondrial dysfunctions and lysosomal and peroxisomal disorders. Few metabolic disorders exhibit characteristic changes on MRS. For example, organic acid disorders like maple syrup urine disease with abnormal branched chain amino acids demonstrate resonance peaks at 0.9 ppm [57]. Urea cycle defects present with elevated glutamine on MRS [52]. MRS is also used in leuko-encephalopathies with the most characteristic signature peak being an NAA peak in Canavan’s disease [58] (Fig. 7). Additionally, other diseases show some specific MRS findings, for example, creatine deficiency shows low creatine peaks (Fig. 8) and non-ketotic hyperglycinemia shows a glycine peak at 3.6 ppm [57].
Single voxel MR spectroscopy with echo time of 144 ms from the left basal ganglia in this 7-y-old child: Structural MR images showed completely normal appearing grey and white matter structures. MR spectroscopy shows creatine deficiency with significant reduction in the creatine metabolite peak on the MR spectra at 3.0 ppm
An abnormal MRS spectrum with a non-specific pattern may be seen in hypomyelinating disorders like Pelizaeus-Merzbacher, metachromatic leukodystrophy, Krabbe’s and X linked adrenoleukodystrophy. Occasionally Pelizaeus-Merzbacher disease may show mild elevations of NAA. Mitochondrial disorders caused by defects of intra-cellular energy metabolism show elevated lactate peaks [57] (Fig. 9). However, the absence of lactate does not exclude the possibility of mitochondrial disorders. In the acute phase of ADEM, there is elevation of choline, lipids and lactate with reduced mI [59].
Amongst pediatric neoplasms, taurine at 3.3 ppm has been consistently observed with medulloblastomas and helps differentiate medulloblastoma from other tumors, although desmoplastic variants may show slightly low levels of taurine [60, 61]. Pilocytic astrocytoma, a grade 1 tumor, shows paradoxical elevation of choline, Cho/NAA peaks and low mI [61] with lactate usually present. Ependymoma has variable choline levels with elevated mI as compared to medulloblastomas or pilocytic tumors [52]. In the supratentorial parenchyma, primitive neuroectodermal tumor (PNET) shows elevated choline and taurine levels [62]. Atypical terato-rhabdoid tumors usually demonstrate moderate choline levels [61]. Choroid plexus papillomas have a characteristic mI peak, as against choroid plexus carcinoma that has a prominent choline peak and unremarkable mI [62].
Diffuse infiltrating brainstem glioma (DIBSG) usually depicts high choline (Fig. 10) and citrate on MRS [63]. Amongst gliomas, low-grade astrocytoma typically shows mI that can be used to differentiate from high-grade gliomas [62]. High-grade gliomas show elevated choline (Fig. 11) with prominent lipid peaks. MRS helps grade and differentiate types of tumors, guide stereotactic biopsy and determine response to treatment in brain tumors [51]. Treatment response assessment is an important application of MRS in tumors with increasing choline levels suggesting recurrence [62].
Single voxel MR spectroscopy with voxel placed over the brainstem glioma (a) and over the normal cerebellar parenchyma (b). Elevated choline (red arrow in a) and diminished NAA (white arrow in a) peaks are seen within the tumor compared to the corresponding metabolite peaks within the normal cerebellar parenchyma (b)
MRS is also useful in differentiating tumor mimics like encephalitis which show reduced mI compared to neoplastic processes [52]. Prominent lipid peaks in shaken baby syndrome have been associated with poorer outcomes [55, 58]. Potential applications of MRS include its use as a marker for diffuse white matter injury in perinatal insult. The role of citrate in brain tumors especially in diffuse infiltrative brain stem gliomas and grade 2 and grade 3 astrocytomas is being explored for its potential association with tumor progression [52, 63].
Magnetic Encephalography (MEG)
Magnetic encephalography is a noninvasive functional neurological method that measures electromagnetic neural activity of the brain. MEG is used increasingly for presurgical mapping of eloquent cortex and identification of zones of abnormal interictal activity in patients with seizures.
MEG signal arises from the intracellular postsynaptic current that flows from dendrites to the soma [64]. Sensitive detectors measure magnetic fields associated with neural currents that are exceedingly weak. MEG is sensitive to signals along the walls of sulci that are tangentially oriented and least sensitive to cortical activity from radially oriented cortical surfaces such as crowns of gyri [64]. The activity detected by MEG sensors can be processed by different methods that allow construction of images with functionally relevant neural activity depicted as color overlay on anatomic MR images.
MEG is often used for determining whether an abnormal interictal activity is unifocal or multifocal (Fig. 12) and also helps guide grid placement of intracranial electrodes. It is often used in clinical practice for identification of eloquent functional cortex in relation to structural lesions. Motor mapping for surgical planning, language lateralization, and localization are the other principle applications of MEG [64, 65]. MEG mapping can help in identifying functional eloquent cortex and ictal onset zone in cases where cortical reorganization has occurred. Future applications being studied include autistic disorders, trauma and schizophrenics [64].
Radiogenomics
Recent advances in whole genome sequencing have further helped stratify tumors based on specific genomic alterations. Radiogenomics is an emerging field in cancer imaging which aims to correlate imaging phenotype with cancer gene expression. This is a potentially powerful tool, providing noninvasive insights into molecular subtypes of tumors that could help develop specific tailored therapies. Location and enhancement patterns of pediatric medulloblastomas have been found to be predictive of molecular subgroups [66] and may potentially be used as surrogate markers for genomic expression of these tumors.
Conclusions
Rapidly evolving technology and an ever-expanding understanding of brain development and pathophysiology warrants an integrative approach to investigate structural details and functional aspects of the pediatric brain.
Advanced pediatric neuroimaging techniques, while once, the domain of research are now available in routine clinical practice, making it necessary for clinicians to be familiar with their current applications. The authors have described the most robust of these newer imaging techniques; DTI, fMRI, MR perfusion and MR spectroscopy and their clinical applications with a view to familiarize clinicians to their use in routine clinical practice.
References
Raschle N, Zuk J, Ortiz-Mantilla S, Sliva DD, Franceschi A, Grant PE, et al. Pediatric neuroimaging in early childhood and infancy: challenges and practical guidelines. Ann N Y Acad Sci. 2012;1252:43–50.
Prabhakaran V, Nair VA, Austin BP, La C, Gallagher TA, Wu Y, et al. Current status and future perspectives of magnetic resonance high-field imaging: a summary. Neuroimaging Clin N Am. 2012;22:373–97.
Dahmoush HM, Vossough A, Roberts TPL. Pediatric high-field magnetic resonance imaging. Neuroimaging Clin N Am. 2012;22:297–313.
Sze R. Building the pediatric radiology department of the future. Pediatr Radiol. 2011;41:S247–9.
Hüppi PS, Dubois J. Diffusion tensor imaging of brain development. Semin Fetal Neonatal Med. 2006;11:489–97.
Isaacson J, Provenzale J. Diffusion tensor imaging for evaluation of the childhood brain and pediatric white matter disorders. Neuroimaging Clin N Am. 2011;21:179–89.
Mathur A, Neil J, Inder T. Understanding brain injury and neurodevelopmental disabilities in the preterm infant: the evolving role of advanced MRI. Semin Perinatol. 2010;34:57–66.
Neil J, Miller J, Mukherjee P, Hüppi PS. Diffusion tensor imaging of normal and injured developing human brain - a technical review. NMR Biomed. 2002;15:543–52.
Oishi K, Faria AV, Mori S. Advanced neonatal neuroMRI. Magn Reson Imaging Clin N Am. 2012;20:81–91.
Wycoco V, Shroff M, Sudhakar S, Lee W. White matter anatomy: what the radiologist needs to know. Neuroimaging Clin N Am. 2013;23:197–216.
Englander ZA, Pizoli CE, Batrachenko A, Sun J, Worley G, Mikati MA, et al. Diffuse reduction of white matter connectivity in cerebral palsy with specific vulnerability of long range fiber tracts. Neuroimage Clin. 2013;2:440–7.
Lepomäki VK, Paavilainen TP, Hurme SA, Komu ME, Parkkola RK; PIPARI Study Group. Fractional anisotropy and mean diffusivity parameters of the brain white matter tracts in preterm infants: reproducibility of region-of-interest measurements. Pediatr Radiol. 2012;42:175–82.
Provenzale JM, Liang L, DeLong D, White LE. Diffusion tensor imaging assessment of brain white matter maturation during the first postnatal year. AJR Am J Roentgenol. 2007;189:476–86.
Bartha AL, Yap KRL, Miller SP, Jeremy RJ, Nishimoto M, Vigneron DB, et al. The normal neonatal brain: MR imaging, diffusion tensor imaging, and 3D MR spectroscopy in healthy term neonates. AJNR Am J Neuroradiol. 2007;28:1015–21.
Rodrigues K, Grant PE. Diffusion-weighted imaging in neonates. Neuroimaging Clin N Am. 2011;21:127–51.
Van Kooij BJM, de Vries LS, Ball G, van Haastert IC, Benders MJNL, Groenendaal F, et al. Neonatal tract-based spatial statistics findings and outcome in preterm infants. AJNR Am J Neuroradiol. 2012;33:188–94.
El-Dib M, Massaro AN, Bulas D, Aly H. Neuroimaging and neurodevelopmental outcome of premature infants. Am J Perinatol. 2010;27:803–18.
Wozniak JR, Krach L, Ward E, Mueller BA, Muetzel R, Kiragu A, et al. Neurocognitive and neuroimaging correlates of pediatric traumatic brain injury: a diffusion tensor imaging (DTI) study. Arch Clin Neuropsychol. 2007;22:555–68.
Hulkower MB, Poliak DB, Rosenbaum SB, Zimmerman ME, Lipton ML. A decade of DTI in traumatic brain injury: 10 years and 100 articles later. AJNR Am J Neuroradiol. 2013;34:2064–74.
Young RJ, Brennan N, Fraser JF, Brennan C. Advanced imaging in brain tumor surgery. Neuroimaging Clin N Am. 2010;20:311–35.
Mabbott DJ, Noseworthy MD, Bouffet E, Rockel C, Laughlin S. Diffusion tensor imaging of white matter after cranial radiation in children for medulloblastoma: correlation with IQ. Neuro Oncol. 2006;8:244–52.
Hygino da Cruz LC Jr, Batista RR, Domingues RC. Barkhof F. Diffusion magnetic resonance imaging in multiple sclerosis. Neuroimaging Clin N Am. 2011;21:71–88.
Rath TJ, Hughes M, Arabi M, Shah GV. Imaging of cerebritis, encephalitis, and brain abscess. Neuroimaging Clin N Am. 2012;22:585–607.
Wahl M, Barkovich AJ, Mukherjee P. Diffusion imaging and tractography of congenital brain malformations. Pediatr Radiol. 2010;40:59–67.
Ou X, Glasier CM, Snow JH. Diffusion tensor imaging evaluation of white matter in adolescents with myelomeningocele and Chiari II malformation. Pediatr Radiol. 2011;41:1407–15.
Liu M, Concha L, Lebel C, Beaulieu C, Gross DW. Mesial temporal sclerosis is linked with more widespread white matter changes in temporal lobe epilepsy. Neuroimage Clin. 2012;1:99–105.
Fernandez-Miranda JC, Pathak S, Engh J, Jarbo K, Verstynen T, Yeh F-C, et al. High-definition fiber tractography of the human brain: neuroanatomical validation and neurosurgical applications. Neurosurgery. 2012;71:430–53.
Ogawa S, Lee TM, Nayak AS, Glynn P. Oxygenation-sensitive contrast in magnetic resonance image of rodent brain at high magnetic fields. Magn Reson Med. 1990;14:68–78.
Kwong KK, Belliveau JW, Chesler DA, Goldberg IE, Weisskoff RM, Poncelet BP, et al. Dynamic magnetic resonance imaging of human brain activity during primary sensory stimulation. Proc Natl Acad Sci. 1992;89:5675–9.
Belyaev AS, Peck KK, Brennan NMP, Holodny AI. Clinical applications of functional MR imaging. Magn Reson Imaging Clin N Am. 2013;21:269–78.
O’Shaughnessy ES, Berl MM, Moore EN, Gaillard WD. Pediatric functional magnetic resonance imaging (fMRI): issues and applications. J Child Neurol. 2008;23:791–801.
Provenzale JM. Advances in pediatric neuroradiology: highlights of the recent medical literature. AJR Am J Roentgenol. 2009;192:19–25.
Gaillard WD, Balsamo L, Xu B, McKinney C, Papero PH, Weinstein S, et al. fMRI language task panel improves determination of language dominance. Neurology. 2004;63:1403–8.
Medina LS, Bernal B, Ruiz J. Role of functional MR in determining language dominance in epilepsy and nonepilepsy populations: a bayesian analysis. Radiology. 2007;242:94–100.
Kesavadas C, Thomas B, Sujesh S, Ashalata R, Abraham M, Gupta AK, et al. Real-time functional MR imaging (fMRI) for presurgical evaluation of paediatric epilepsy. Pediatr Radiol. 2007;37:964–74.
Leach JL, Holland SK. Functional MRI in children: clinical and research applications. Pediatr Radiol. 2010;40:31–49.
Lee MH, Smyser CD, Shimony JS. Resting-state fMRI: a review of methods and clinical applications. AJNR Am J Neuroradiol. 2013;34:1866–72.
Raichle ME, Snyder AZ. A default mode of brain function: a brief history of an evolving idea. Neuroimage. 2007;37:1083–90.
Uddin LQ. Resting-state FMRI and developmental systems neuroscience. Front Neurosci. 2011;5:14.
Supekar K, Musen M, Menon V. Development of large-scale functional brain networks in children. PLoS Biol. 2009;7:e1000157.
Doria V, Beckmann CF, Arichi T, Merchant N, Groppo M, Turkheimer FE, et al. Emergence of resting state networks in the preterm human brain. Proc Natl Acad Sci U S A. 2010;107:20015–20.
Rubia K. Functional brain imaging across development. Eur Child Adolesc Psychiatry. 2013;22:719–31.
Rudie JD, Brown JA, Beck-Pancer D, Hernandez LM, Dennis EL, Thompson PM, et al. Altered functional and structural brain network organization in autism. Neuroimage Clin. 2013;2:79–94.
Huisman T, Sorensen A. Perfusion-weighted magnetic resonance imaging of the brain: techniques and application in children. Eur Radiol. 2004;14:59–72.
Wang J, Licht DJ. Pediatric perfusion MR imaging using arterial spin labeling. Neuroimaging Clin N Am. 2006;16:149–67.
Panigrahy A, Blüml S. Neuroimaging of pediatric brain tumors: from basic to advanced magnetic resonance imaging (MRI). J Child Neurol. 2009;24:1343–65.
Thompson G, Mills SJ, Stivaros SM, Jackson A. Imaging of brain tumors: perfusion/permeability. Neuroimaging Clin N Am. 2010;20:337–53.
Järnum H, Steffensen EG, Knutsson L, Fründ E-T, Simonsen CW, Lundbye-Christensen S, et al. Perfusion MRI of brain tumours: a comparative study of pseudo-continuous arterial spin labelling and dynamic susceptibility contrast imaging. Neuroradiology. 2010;52:307–17.
Yeom KW, Mitchell LA, Lober RM, Barnes PD, Vogel H, Fisher PG, et al. Arterial spin-labeled perfusion of pediatric brain tumors. AJNR Am J Neuroradiol. 2014;35:395–401.
Wintermark P, Warfield SK. New insights in perinatal arterial ischemic stroke by assessing brain perfusion. Transl Stroke Res. 2012;3:255–62.
Horská A, Barker PB. Imaging of brain tumors: MR spectroscopy and metabolic imaging. Neuroimaging Clin N Am. 2010;20:293–310.
Panigrahy A, Nelson MD Jr, Blüml S. Magnetic resonance spectroscopy in pediatric neuroradiology: clinical and research applications. Pediatr Radiol. 2010;40:3–30.
Kocak M. Advanced imaging in pediatric neuroradiology. Pediatr Radiol. 2009;39:456–63.
Barkovich AJ, Baranski K, Vigneron D, Partridge JC, Hallam DK, Hajnal BL, et al. Proton MR spectroscopy for the evaluation of brain injury in asphyxiated, term neonates. AJNR Am J Neuroradiol. 1999;20:1399–405.
Cecil KM, Jones BV. Magnetic resonance spectroscopy of the pediatric brain. Top Magn Reson Imaging. 2001;12:435–52.
Barkovich AJ, Miller SP, Bartha A, Newton N, Hamrick SEG, Glenn OA, et al. MR imaging, MR spectroscopy, and diffusion tensor imaging of sequential studies in neonates with encephalopathy. AJNR Am J Neuroradiol. 2006;27:533–47.
Rossi A, Biancheri R. Magnetic resonance spectroscopy in metabolic disorders. Neuroimaging Clin N Am. 2013;23:425–48.
Cecil KM, Kos RS. Magnetic resonance spectroscopy and metabolic imaging in white matter diseases and pediatric disorders. Top Magn Reson Imaging. 2006;17:275–93.
Küker W, Ruff J, Gaertner S, Mehnert F, Mader I, Nägele T. Modern MRI tools for the characterization of acute demyelinating lesions: value of chemical shift and diffusion-weighted imaging. Neuroradiology. 2004;46:421–6.
Tong Z, Yamaki T, Harada K, Houkin K. In vivo quantification of the metabolites in normal brain and brain tumors by proton MR spectroscopy using water as an internal standard. Magn Reson Imaging. 2004;22:1017–24.
Plaza MJ, Borja MJ, Altman N, Saigal G. Conventional and advanced MRI features of pediatric intracranial tumors: posterior fossa and suprasellar tumors. AJR Am J Roentgenol. 2013;200:1115–24.
Borja MJ, Plaza MJ, Altman N, Saigal G. Conventional and advanced MRI features of pediatric intracranial tumors: supratentorial tumors. AJR Am J Roentgenol. 2013;200:W483–503.
Seymour ZA, Panigrahy A, Finlay JL, Nelson MD, Blüml S. Citrate in pediatric CNS tumors? AJNR Am J Neuroradiol. 2008;29:1006–11.
Schwartz ES, Edgar JC, Gaetz WC, Roberts TPL. Magnetoencephalography. Pediatr Radiol. 2010;40:50–8.
Schwartz ES, Dlugos DJ, Storm PB, Dell J, Magee R, Flynn TP, et al. Magnetoencephalography for pediatric epilepsy: how we do it. AJNR Am J Neuroradiol. 2008;29:832–7.
Perreault S, Ramaswamy V, Achrol AS, Chao K, Liu TT, Shih D, et al. MRI surrogates for molecular subgroups of medulloblastoma. AJNR Am J Neuroradiol. 2014;35:1263–9.
Conflict of Interest
None.
Source of Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krishnan, P., Muthusami, P., Heyn, C. et al. Advances in Pediatric Neuroimaging. Indian J Pediatr 82, 154–165 (2015). https://doi.org/10.1007/s12098-014-1657-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-014-1657-3